Abstract
Objective
To assess rehabilitation inpatient risk of return to primary service in bone marrow transplant patients.
Design
Retrospective review.
Setting
Inpatient rehabilitation unit within a tertiary referral based cancer center
Participants
All bone marrow transplant patients (131) who were admitted a total of 147 times to inpatient rehabilitation between January 1, 2002, and April 30, 2010.
Interventions
None.
Main Outcome Measures
We analyzed return to primary service and demographic information, cancer characteristics, medications, hospital admission characteristics, and laboratory values.
Results
41% (61/147) of bone marrow transplant admissions were transferred from the inpatient rehabilitation unit back to the primary service. Of those transferred back, 38% (23/61) died after being transferred back to the primary service. Significant or near significant relationships were found for a platelet count < 43,000 per microliter (p<.01), a creatinine level > 0.9 milligrams/deciliter (p<.01), the presence of an antiviral agent (p=.0501), the presence of an antibacterial agent (p=.0519), the presence of an antifungal agent (p<.05) and leukemia, lymphoma or multiple myeloma diagnosis (p<.05). Using five of these factors the Return to Primary-Bone Marrow Transplant (RTP-BMT) index was formulated to determine the likelihood of return to the primary team.
Conclusion
Bone marrow transplant patients have a high rate of transfer from the inpatient rehabilitation unit back to the primary service. The RTP-BMT score can be a useful tool to help clinicians predict the likelihood of return to the primary acute care service.
Keywords: Bone marrow transplant, Rehabilitation, Cancer
Chemotherapy, anemia, thrombocytopenia, steroid myopathy, peripheral neuropathy, immobility syndrome, and infections can lead to asthenia, deconditioning, and fatigue in hematopoietic stem cell transplant patients.1 Mean peak aerobic capacity and muscular strength are reduced after stem cell transplantation.2 Fatigue is the most common and persistent symptom in cancer patients and has been identified as more important than pain.3 It has been found that 87% of inpatient cancer patients have rehabilitation needs.4
While the need for rehabilitation in cancer patients has been established, caring for these patients in an inpatient rehabilitation unit can be challenging given the acuity of their medical conditions. Unfortunately, transfers back to the primary acute care service during inpatient rehabilitation can occur and are usually unplanned. Typically, although not always, the goal of inpatient rehabilitation is discharge home. Medical stability is to preferred to insure an uninterrupted inpatient rehabilitation stay and consistent therapy participation. Several previous studies have identified risk factors for return to primary in different patient populations.5–8 Alam et al. reported a transfer rate of 21% for cancer patients on inpatient rehabilitation (compared to 9.7% for matched non-cancer controls).9 Guo et al. found that 35% of all cancer patients in acute inpatient rehabilitation were transferred back to the primary service.10
We have anecdotally observed a particularly high rate of transfer from inpatient rehabilitation back to the primary service among hematopoietic stem cell transplant patients. To our knowledge, no prior analysis of risk factors associated with return to primary service from inpatient rehabilitation among hematopoietic stem cell patients has been performed. The purpose of this study was to identify risk factors which are associated with a higher frequency of transfers to the primary acute care service.
METHODS
Subjects
This retrospective study included all patients with a history of hematopoietic stem cell transplantation who were admitted to the inpatient rehabilitation unit at a referral-based tertiary care cancer center between January 1, 2002 and April 30, 2010. 131 patients were found. Sixteen patients were admitted to the inpatient rehabilitation unit on two separate occasions, resulting in 147 total admissions. The age of the patients ranged from 21 to 77 years.
Procedure
Approval for this study was obtained from the institutional review board (IRB). A waiver of informed consent was granted by the IRB in compliance with federal and institutional guidelines. Experienced clinicians collected data from medical records and discharge summaries. Charts were reviewed for medical and demographic information. The records for the hospitalization of the patient’s inpatient rehabilitation stay were reviewed from admission to discharge. Data were collected from several categories: demographic information, transplant characteristics, medications, hospital admission characteristics, and laboratory values. Demographic information on rehabilitation transfer day included age, gender, race, marital status, insurance type and date of death (if applicable). Transplant characteristics obtained included type of primary cancer, type of bone marrow transplant, date of last bone marrow transplant, documented pathology reports of graft versus host disease (GVHD) since the last transplant, number of bone marrow transplants, last bone marrow leukocyte blast count, last peripheral leukocyte blast count and if the patient had relapsed. Medication data collected included the presence on the rehabilitation transfer day of antibacterial agents, antiviral agents, antifungal agents, steroid immunosuppresants, non-steroid immunosuppresants (e.g. tacrolimus) and erythropoietic agents. Hospital admission characteristics included the patient’s location prior to admission, reason for hospitalization, reason for transfer to inpatient rehabilitation, if the patient had returned to the primary acute care service and reason for transfer back to the primary service (if applicable). Laboratory values included peripheral white blood cell count, hemoglobin, platelet count, creatinine, prealbumin, albumin, and peripheral blast count on the day of transfer to inpatient rehabilitation.
Analyses included several steps. First, frequencies for 22 categorical variables were examined. Next, nonparametric statistical tests were completed on these variables to detect proportional differences among the categories, as well as their relationship to the study dependent variable, ‘return to primary acute care service.’ Variables selected for further analytical inclusion had to exhibit statistical association and be associated with the outcome in a nontrivial way (i.e. each variable had to contribute clinically useful information. For example, we would not include the date of return to primary although it was significantly related). Using logistic regression analysis, we were then able to identify variables for an indexing tool that is based on medically related variables and the probability of transplant patients’ return to their primary acute care team. The resulting model was termed the Return to Primary – Bone Marrow Transplant Index or RTP-BMT Index.
RESULTS
Table 1 lists selected demographic characteristics of our study population. The study subjects were primarily white (76.87%) and male (59.86%). The mean length of stay was 9.69 days (median, 9 days). The mean length of stay in the hospital before admission to inpatient rehabilitation was 33.19 days (median, 22 days). The types of bone marrow transplant were somewhat evenly divided among autologous (auto; 31.97%), matched related donor (MRD; 34.01%), and matched unrelated donor (MUD; 34.01%). Also shown in Table 1 are frequencies for these categories and subjects’ return to the primary acute care medical team. In total, 61 of the 147 inpatient rehabilitation admissions (41.50%) returned to the primary service. Of those returning to the primary service, 25 (40.98%) were discharged directly home, 23 (37.70%) died in the hospital, 5 (8.20%) were discharged to hospice, 5 (8.20%) were readmitted to inpatient rehabilitation, 2 (3.28%) were transferred to an outside acute hospital and 1 (1.64%) was transferred to a long term acute care facility.
Table 1.
Overall Frequencies and Proportional Differences in the Return to the Primary Acute Care Medical Service by Study Subjects’ Race, Sex, Type of Transplant, and Graft-versus-Host Disease
| Characteristic* | Total (n = 147) | Return to Primary Acute Care Medical Service
|
|||||
|---|---|---|---|---|---|---|---|
| No (n = 86) | Yes (n = 61) | ||||||
|
| |||||||
| Freq. | % | Freq. | % | Freq. | % | Chi-square | |
| Race | χ2(1, N = 147) = 0.002, p = 0.965 | ||||||
| White | 113 | 76.87 | 66 | 76.74 | 47 | 77.05 | |
| Hispanic | 18 | 12.22 | 8 | 9.30 | 10 | 16.39 | |
| Black | 13 | 8.84 | 10 | 11.63 | 3 | 4.92 | |
| Asian | 3 | 2.04 | 2 | 2.33 | 1 | 1.64 | |
| Sex | χ2(1, N = 147) = 1.415, p = 0.234 | ||||||
| Male | 88 | 59.86 | 48 | 55.81 | 40 | 65.57 | |
| Female | 59 | 40.14 | 38 | 44.19 | 21 | 34.43 | |
| Type of bone marrow transplant | χ2(2, N = 147) = 3.272, p = 0.195 | ||||||
| Auto | 47 | 31.97 | 32 | 37.21 | 15 | 24.59 | |
| MRD | 50 | 34.01 | 25 | 29.07 | 25 | 40.98 | |
| MUD | 50 | 34.01 | 29 | 33.72 | 21 | 34.43 | |
| GVHD | χ2(1, N = 147) = 0.545, p = 0.460 | ||||||
| No | 80 | 54.42 | 49 | 56.98 | 31 | 50.82 | |
| Yes | 67 | 45.58 | 37 | 43.02 | 30 | 49.18 | |
Characteristic abbreviations: auto, autologous; MRD, matched related donor; MUD, matched unrelated donor; GVHD, graft-versus-host disease
We examined over 20 categorical variables to identify statistically significant proportional associations between demographic variables by return to the acute care service. Table 1 presents the results of the chi-square tests (p<.05) for the selected demographic characteristics shown. None of these categorical variables—race (white or nonwhite), sex (male or female), type of bone marrow transplant (auto, MRD, or MUD) and GVHD (yes or no) were disproportionately associated with return to the acute care medical team (p>.05). As well, age, marital status, insurance type, number of bone marrow transplants, patient relapse, steroid immunosuppresants, non-steroid immunosuppresants, erythropoietic agents, peripheral white blood cell count, prealbumin, and albumin levels were all distributed proportionally by patients’ return to the acute care medical team (p>.05). Variables with significant (p<.05) deviations among categories by patients’ return to the acute care medical team were antifungal agents (χ2 (1, N = 147) = 7.175, p = 0.0074), antibacterial agents (χ2 (1, N = 147) = 5.143, p = 0.0233), antiviral agents (χ2 (1, N = 147) = 3.984, p = 0.0459), platelet counts (χ2(1, N = 147) = 14.1967, p = 0.0002), creatinine levels (χ2(1, N = 147) = 6.1338, p = 0.0133), and type of primary cancer (χ2(1, N = 147) = 8.713, p = 0.0096).
Forty-eight percent of the admissions in the study (n=70) were alive at the time of data collection. Among the transplant admissions that had died (n=77), we observed patterns of longevity with return to primary service (days until death after BMT and whether patients returned to primary service). Patients that returned to primary service (n=36) lived a median of 76 days post-BMT (95% CI [40,135]). The median post-BMT survival days for patients not returning to primary service (n=41) was 190 days (95% CI [64–266]). Therefore, of the deceased patients, those who returned to primary did not live as long.
Table 2 presents the primary cancer diagnoses for the study sample. The three predominant cancer types were leukemia, lymphoma, and multiple myeloma. These three cancer types comprised more than 98% of the patients who returned to acute care. There were no returns to acute care for patients with Waldenstrom macroglobulinemia, breast, germinoma, renal or testicular cancer.
Table 2.
Primary Cancer Diagnosis at the Time of Bone Marrow Transplant by Return to the Primary Acute Care Service
| Diagnosis* | Total (n = 147) | Return to Primary Acute Care Service
|
||||
|---|---|---|---|---|---|---|
| No (n = 86) | Yes (n = 61) | |||||
| Freq. | % | Freq. | % | Freq. | % | |
|
|
||||||
| Breast | 3 | 2.04 | 3 | 3.49 | 0 | 0.00 |
| Germinoma | 1 | 0.68 | 1 | 1.16 | 0 | 0.00 |
| Leukemia | 66 | 44.90 | 31 | 36.05 | 35 | 57.38 |
| Lymphoma | 45 | 30.61 | 29 | 33.72 | 16 | 26.23 |
| MDS/aplastic anemia | 4 | 2.72 | 3 | 3.49 | 1 | 1.64 |
| Multiple myeloma | 23 | 15.65 | 14 | 16.28 | 9 | 14.75 |
| Renal | 1 | 0.68 | 1 | 1.16 | 0 | 0.00 |
| Testicular | 2 | 1.36 | 2 | 2.33 | 0 | 0.00 |
| Waldenstrom macroglobulinemia | 2 | 1.36 | 2 | 2.33 | 0 | 0.00 |
Diagnosis abbreviations: MDS, myelodysplastic syndrome
Table 3 shows the reasons indicated on the patients’ medical records for the study subjects’ return to their acute care medical team. Of the 19 total reasons, infection (17/61; 27.87%) and functional decline/unable to tolerate therapy (11/61; 18.03%) were the most common reasons for return to the primary acute care team. The remaining 17 documented reasons comprised 54% of the returns.
Table 3.
Reasons for Return to Primary Acute Care Service
| Reason | Frequency | % |
|---|---|---|
| Brain hemorrhage | 2 | 3.28 |
| Cardiac | 6 | 9.83 |
| Completed rehab but not medically ready for discharge | 3 | 4.92 |
| Dyspnea | 1 | 1.64 |
| Functional decline/unable to tolerate therapy | 11 | 18.03 |
| Gastrointestinal bleed | 4 | 6.56 |
| Hematologic | 1 | 1.64 |
| Increased stool | 1 | 1.64 |
| Infection | 17 | 27.87 |
| Insurance | 1 | 1.64 |
| Leukemia | 2 | 3.28 |
| Mental status changes/syncope | 6 | 9.83 |
| Palliative care | 1 | 1.64 |
| Planned procedure | 1 | 1.64 |
| Pulmonary | 1 | 1.64 |
| Pulmonary embolism | 1 | 1.64 |
| Renal | 1 | 1.64 |
| Unknown | 1 | 1.64 |
| Total | 61 | 100.00 |
In order to predict which factors influence patients’ return to the primary acute care medical team, we used logistic regression analysis and the previously identified significant (p<0.05) categorical variables. As previously mentioned, the variables meeting this standard included antifungal agents, antibacterial agents, antiviral agents, platelet counts, creatinine levels, and primary cancer of either leukemia, lymphoma, or multiple myeloma. Table 4 presents the results of the logistic regression using these six independent variables and their association with bone marrow transplant patients’ return to primary service. Also shown in Table 4 are the clinical cut points used in classifying patients into categories. Cut points were set at the median clinical value of the entire population of patients. Median values are commonly used for setting cut points in clinical data but it should be noted that median values may be unstable as they are influenced by the addition of extreme values in either end of the range. As shown by the Wald (χ2) values, all of the variables used in the model retained their statistical associations with the dependent variable, although two variables (the presence of antiviral and antibacterial agents) were slightly above statistical standards (p>.05).
Table 4.
Significant Logistic Regression Predictor Variable Frequencies and Chi-square Values for Bone Marrow Transplant Patients’ Return to Primary Acute Care Service
| Factor | Frequency* | % | β | SE | Wald (χ2) | p | OR [95% CI] |
|---|---|---|---|---|---|---|---|
| Antiviral | .441 | .225 | 3.84 | 0.0501 | |||
| No | 31 | 21.08 | 0.413 [0.16, 0.966] | ||||
| Yes | 116 | 78.91 | 2.318 [1.03, 6.17] | ||||
| Antifungal | .633 | .246 | 6.61 | 0.0101 | |||
| No | 30 | 20.41 | 0.281 [0.09, 0.70] | ||||
| Yesv | 117 | 79.59 | 3.54 [1.42, 10.15] | ||||
| Antibacterial | 1.03 | .531 | 3.78 | 0.0519 | |||
| No | 11 | 7.48 | 0.12 [0.01, 0.68] | ||||
| Yes | 136 | 92.52 | 7.89 [0.01, 146.86] | ||||
| Platelet | .660 | .176 | 13.98 | 0.0002 | |||
| ≥43 K/ uL | 78 | 53.06 | 0.267 [0.13, 0.52] | ||||
| < 43 K/uL | 69 | 46.94 | 3.74 [1.89, 7.59] | ||||
| Creatinine | .663 | .198 | 11.166 | 0.0008 | |||
| ≤.9 mg/dL | 50 | 34.01 | 0.26 [0.11, 0.56] | ||||
| > .9 mg/dL | 97 | 65.99 | 3.77 [1.77, 8.52] | ||||
| Primary Cancer | 1.13 | .527 | 4.65 | 0.0311 | |||
| Other | 13 | 8.84 | 0.10 [0.00, 0.54] | ||||
| Leukemia, lymphoma, or multiple myeloma | 134 | 91.16 | 9.72 [1.83, 179.70] |
Clinical cut points (median clinical value of the entire population) used in classifying patients into categories: K/uL, thousand per microliter; mg/dL, milligram per deciliter
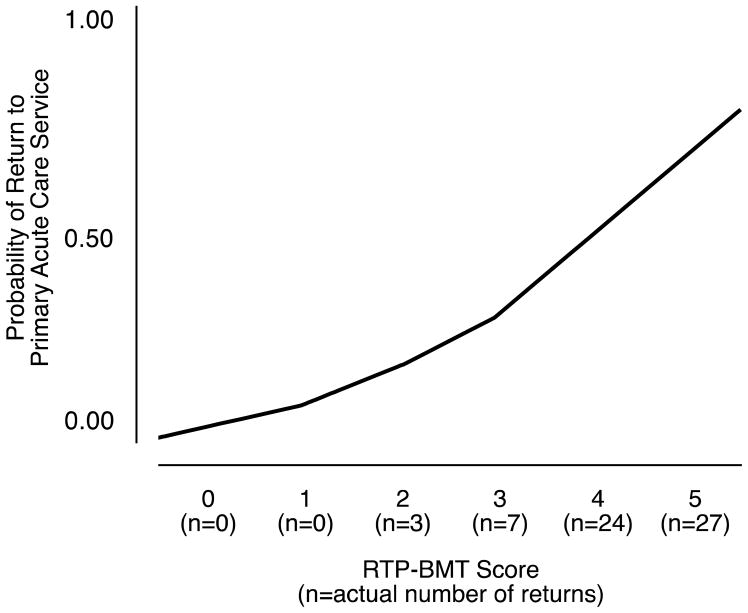
Table 5 applies five of these variables into a scoring system called the RTP-BMT Index.11 A sixth statistically significant variable (primary cancer type being leukemia, lymphoma, or multiple myeloma) was not included because over 91% of patients had one of these primary cancers and it was thus deemed to be extraneous. The five remaining clinical variables were dichotomized into 0 (no, not present) or 1 (yes, present) and return to primary acute care service status (yes, no). The frequency of each patient’s return to acute primary care service was then calculated (0, 1, 2, 3, 4, or 5). From these data, Index probabilities were generated. As shown in the table, RTP-BMT Index scores from 0 to 1 represented patients with low probabilities for return to primary acute care service (4%). An RTP-BMT Index of 2 and 3 represented patients with a medium probability of return (20%). Patients with an Index of 4 or 5 had a high probability of return to primary acute care service (56%). In fact, the latter group had almost three times the probability of return to primary acute care service than patients with an RTP-BMT Index of 2 or 3 and more than 13 times the probability of returning than patients with an Index of 0 or 1. Figure 1 shows the logistic curve of the regression analysis and return probabilities across the entire range.
Table 5.
RTP-BMT Index Cumulative Values Based on Cut Points for Five Factors and the Percentage and Relative Risk Grouping of Bone Marrow Transplant Rehabilitation Patients’ Return to Primary Acute Care Service.*
| Did patient return to primary acute care service? | Probability of return to primary acute care service | Probability of return to primary acute care service by BMT-RTP Index Group | |||
|---|---|---|---|---|---|
| RTP-BMT Index** | No | Yes | % | ||
| 0 | 3 | 0 | 0.0225 |
|
0.0438 |
| 1 | 6 | 0 | 0.0537 | ||
| 2 | 13 | 3 | 0.1230 |
|
0.1960 |
| 3 | 24 | 7 | 0.2573 | ||
| 4 | 27 | 24 | 0.4611 |
|
0.5648 |
| 5 | 13 | 27 | 0.6788 | ||
Wald test for the overall model = 20.627 (p = <.0001); Unit Odds Ratios (per unit change in regressor) = 0.404, CI [0.266, 0.583]
Antiviral present = 1; not present = 0
Antifungal present = 1; not present = 0
Antibacterial present = 1; not present = 0
Platelet count LESS than 43,000 per microliter (uL) = 1; 43 K/uL or GREATER = 0
Creatinine GREATER than .9 (milligram/deciliter, mg/dL)= 1; .9 mg/dL or LESS = 0
Abbreviations: RTP-BMT, Return to Primary – Bone Marrow Transplant Index
Figure 1.
Logistic Regression Curve for the RTP-BMT Index Range (0–5) and Patients’ Return to the Primary Acute Care Service
DISCUSSION
This is the first study to specifically look at risk factors for return to acute care of hematopoietic stem cell transplant rehabilitation patients. The results of our study illustrate the challenges in caring for this patient population in inpatient rehabilitation. Our study identified a number of factors that significantly influenced the likelihood for this group of individuals to return to their primary acute care service, with a clear trajectory of increased probability with the addition of each the identified factors. The results of this study may be useful to consulting physiatrists in planning for the care of a bone marrow transplant patient transferred to inpatient rehabilitation. For example, based on the index score, the physiatry consultant may consider the need for additional help managing these patients during inpatient rehabilitation.
There have been a number of studies that have identified risk factors for return to the primary acute care service from inpatient rehabilitation for a variety of cancer populations.5–8 Guo et al.10 studied of all cancer rehabilitation inpatients and found that the significant factors associated with transfer back were low albumin, elevated creatinine levels and complications from tube feeding or a Foley catheter. Other studies have also identified that albumin and creatinine predict cancer patient outcomes.12–13 Our study confirms that an elevated creatinine is a risk factor for transfer back to acute care in the population evaluated in this study. The absence of an association with a low albumin in the present study in contrast to that of Guo may be due to the characteristics of our more specific study population. Our population was only hematopoietic stem cell transplant patients and were predominantly leukemia, lymphoma, and multiple myeloma. We did not assess the presence of foley catheters and tube feedings as risk factors and thus whether these interventions confer risk in the hematopoetic stem cell patient requires further study.
Co-morbid conditions such as deconditioning and drug toxicities, including steroid myopathy, are common symptoms in patients who are experiencing a complicated posttransplant course and would be expected to increase the need for rehabilitation care. Bone marrow 1-year posttransplant survival at our institution is about 55%, comparable to an overall survival of 53% at a median 37-month follow-up in the literature.14–15 The rate of return to the primary acute care team (41%) and the rate of death in the hospital (38%) among the patients in our study appears to be quite high. However, it is likely that the physiatry service is consulted on lower-functioning bone marrow transplant patients and these are the patients more likely to be transferred to inpatient rehabilitation. Research suggests that functional status may have an impact on hematopoietic stem cell transplant survival.16–21 Thus BMT patients requiring transfer to inpatient rehabilitation patients could have a poorer survival rate compared all patients undergoing BMT.
Despite the identified complication rates, the benefits of exercise and rehabilitation in cancer patients are clear. The challenge is to create a system that balances the complex medical nature of these patients with their rehabilitation needs. Ideally, avoidance of prolonged hospitalization should be the goal. At our institution, we created a physiatric mobile team consisting of a physiatrist, physical therapist, and occupational therapist several years ago. When consulted, the mobile team therapists address issues under the supervision of the physiatrist in acute care. Issues often include family training, better calibrating patient therapy tolerance, or addressing specific obstacles to discharge. The patients can receive up to 2 hours of therapy (1 hour of physical therapy and 1 hour occupational therapy) daily. The mobile team has helped to allow a number of patients (including post-bone marrow transplant) to receive more intense therapies while under the primary medical team’s care, avoiding transfer to the inpatient rehabilitation unit. The primary acute care team can address medical issues while the physiatric mobile team can address their rehabilitation simultaneously. Such coordination between physiatric and medical services clearly is needed in rehabilitation as well due to the high acute care transfer rate of these patients.
If an inpatient rehabilitation transfer is necessary, one also may want to consider whether the rehabilitation hospital can provide the necessary medical services for this group of individuals, including oncologic oversight. Infection was the most common reason for return to acute care. The presence of an antibiotic, antifungal or antiviral agent and the increased likelihood of return to primary acute care hospital team could be a result of a recent infection, or lower white blood cell counts and required these agents prophylactically. At our institution, the bone marrow transplant service follows the patients at least every other day on the rehabilitation unit and is easily reached by pager if medical complications were to arise. Despite this practice, medical complications requiring transfer still occurred frequently. We have found frequent transfusions or neutropenia may be barriers to transfer to other rehabilitation hospitals unable to provide this care. Skilled nursing facilities may also not provide the necessary oversight to identify medical complications early.
Study limitations
The BMT-RTP was formulated from retrospective data and thus validation studies of the RTP-BMT index in which variables were identified and followed prospectively would be useful. The presence of an antimicrobial agent, a statistically significant factor in our study, may be influenced by institution-specific medical care protocols. Multicenter studies would minimize the possible influence of hospital specific care practices. Finally, no Functional Independence Measure (FIM) scores were analyzed in our study. Though an attempt was made to analyze FIM scores, it was found that too few of the patients had a complete FIM score record collected. Future research should be conducted with appropriate measurement of functional change since it is not only a outcome of rehabilitation but may be a predictor of return to acute care.
CONCLUSIONS
The results of this study highlight the challenging medical fragility of hemopoetic stem cell transplant patients in inpatient rehabilitation. The RTP-BMT Index may be useful in planning for the care of these patients during rehabilitation, since this may predict who are more likely to require transfer back to acute care. The vast majority of prior studies evaluating factors in hematopoietic stem cell transplant were understandably focused on pre-transplantation issues. Our study, although limited in scope in that it studied a select group undergoing inpatient rehabilitation, sheds some light on possible post-transplantation factors that predict a more complex medical course.
Acknowledgments
Preliminary data from this study was published as an abstract (Poster 87) from the 2009 Annual Conference of the American College of Physical Medicine & Rehabilitation. There was no financial support for this research.
Abbreviations
- MRD
- MUD
- GVHD
- FIM
- AML
- BMT
- RTP
- IRB
- RR
Footnotes
Disclosures:
We certify that no party having a direct interest in the results of the research supporting this article has or will confer a benefit on us or on any organization with which we are associated AND, if applicable, we certify that all financial and material support for this research (eg, NIH or NHS grants) and work are clearly identified in the title page of the manuscript. Supported in part by the M.D. Anderson Cancer Center support grant # CA 016672 Eduardo Bruera is supported in part by National Institutes of Health grant numbers: RO1NRO10162-01A1, RO1CA122292-01, RO1CA124481-01 And in part by the MD Anderson Cancer Center support grant # CA016672
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Gillis TA, Donovan ES. Rehabilitation following bone marrow transplantation. Cancer. 2001 Aug 15;92(4 Suppl):998–1007. doi: 10.1002/1097-0142(20010815)92:4+<998::aid-cncr1412>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 2.Hayes SC, Davies PS, Parker TW, Bashford J, Green A. Role of a mixed type, moderate intensity exercise programme after peripheral blood stem cell transplantation. Br J Sports Med. 2004 Jun;38(3):304–309. doi: 10.1136/bjsm.2002.003632. discussion 309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Butt Z, Rosenbloom SK, Abernethy AP, et al. Fatigue is the most important symptom for advanced cancer patients who have had chemotherapy. J Natl Compr Canc Netw. 2008 May;6(5):448–455. doi: 10.6004/jnccn.2008.0036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Movsas SB, Chang VT, Tunkel RS, Shah VV, Ryan LS, Millis SR. Rehabilitation needs of an inpatient medical oncology unit. Arch Phys Med Rehabil. 2003 Nov;84(11):1642–1646. doi: 10.1053/s0003-9993(03)00345-9. [DOI] [PubMed] [Google Scholar]
- 5.Carney ML, Ullrich P, Esselman P. Early unplanned transfers from inpatient rehabilitation. Am J Phys Med Rehabil. 2006 May;85(5):453–460. doi: 10.1097/01.phm.0000214279.04759.45. quiz 461–453. [DOI] [PubMed] [Google Scholar]
- 6.Deshpande AA, Millis SR, Zafonte RD, Hammond FM, Wood DL. Risk factors for acute care transfer among traumatic brain injury patients. Arch Phys Med Rehabil. 1997 Apr;78(4):350–352. doi: 10.1016/s0003-9993(97)90224-0. [DOI] [PubMed] [Google Scholar]
- 7.Stineman MG, Ross R, Maislin G, Fiedler RC, Granger CV. Risks of acute hospital transfer and mortality during stroke rehabilitation. Arch Phys Med Rehabil. 2003 May;84(5):712–718. doi: 10.1016/s0003-9993(02)04850-5. [DOI] [PubMed] [Google Scholar]
- 8.Hung JW, Tsay TH, Chang HW, Leong CP, Lau YC. Incidence and risk factors of medical complications during inpatient stroke rehabilitation. Chang Gung Med J. 2005 Jan;28(1):31–38. [PubMed] [Google Scholar]
- 9.Alam E, Wilson RD, Vargo MM. Inpatient cancer rehabilitation: a retrospective comparison of transfer back to acute care between patients with neoplasm and other rehabilitation patients. Arch Phys Med Rehabil. 2008 Jul;89(7):1284–1289. doi: 10.1016/j.apmr.2008.01.014. [DOI] [PubMed] [Google Scholar]
- 10.Guo Y, Persyn L, Palmer JL, Bruera E. Incidence of and risk factors for transferring cancer patients from rehabilitation to acute care units. Am J Phys Med Rehabil. 2008 Aug;87(8):647–653. doi: 10.1097/PHM.0b013e31817fb94e. [DOI] [PubMed] [Google Scholar]
- 11.Gardner MJ, Altman DG. Statistics with confidence. BMJ publications. 1994:51–52. [Google Scholar]
- 12.Kim JEYC, Lee DH, Kim SW, Lee JS, Suh C. Serum albumin level is a significant prognostic factor reflecting disease severity in symptomatic multiple myeloma. Ann Hematol. 2010;89:391–397. doi: 10.1007/s00277-009-0841-4. [DOI] [PubMed] [Google Scholar]
- 13.Durie BG, Salmon SE. A clinical staging system for multiple myeloma. Correlation of measured myeloma cell mass with presenting clinical features, response to treatment, and survival. Cancer. 1975 Sep;36(3):842–854. doi: 10.1002/1097-0142(197509)36:3<842::aid-cncr2820360303>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 14.Be the Match. National Donor Program. 2010 Nov 1; Retrieved from http://marrow.org.
- 15.Boehm A, Sperr WR, Leitner G, et al. Comorbidity predicts survival in myelodysplastic syndromes or secondary acute myeloid leukaemia after allogeneic stem cell transplantation. Eur J Clin Invest. 2008 Dec;38(12):945–952. doi: 10.1111/j.1365-2362.2008.02041.x. [DOI] [PubMed] [Google Scholar]
- 16.Hahn T, McCarthy PL, Jr, Zhang MJ, et al. Risk factors for acute graft-versus-host disease after human leukocyte antigen-identical sibling transplants for adults with leukemia. J Clin Oncol. 2008 Dec 10;26(35):5728–5734. doi: 10.1200/JCO.2008.17.6545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Terwey TH, Hemmati PG, Martus P, et al. A modified EBMT risk score and the hematopoietic cell transplantation-specific comorbidity index for pre-transplant risk assessment in adult acute lymphoblastic leukemia. Haematologica. May;95(5):810–818. doi: 10.3324/haematol.2009.011809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rotta M, Storer BE, Sahebi F, et al. Long-term outcome of patients with multiple myeloma after autologous hematopoietic cell transplantation and nonmyeloablative allografting. Blood. 2009 Apr 2;113(14):3383–3391. doi: 10.1182/blood-2008-07-170746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guilfoyle R, Demers A, Bredeson C, et al. Performance status, but not the hematopoietic cell transplantation comorbidity index (HCT-CI), predicts mortality at a Canadian transplant center. Bone Marrow Transplant. 2009 Jan;43(2):133–139. doi: 10.1038/bmt.2008.300. [DOI] [PubMed] [Google Scholar]
- 20.Sorror M, Storer B, Sandmaier BM, et al. Hematopoietic cell transplantation-comorbidity index and Karnofsky performance status are independent predictors of morbidity and mortality after allogeneic nonmyeloablative hematopoietic cell transplantation. Cancer. 2008 May 1;112(9):1992–2001. doi: 10.1002/cncr.23375. [DOI] [PubMed] [Google Scholar]
- 21.Artz AS, Pollyea DA, Kocherginsky M, et al. Performance status and comorbidity predict transplant-related mortality after allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2006 Sep;12(9):954–964. doi: 10.1016/j.bbmt.2006.05.015. [DOI] [PubMed] [Google Scholar]