Abstract
Poverty is positively associated with poor health; thus, some healthcare commissioners in the UK have pioneered the introduction of advice services in health service locations. Previous systematic reviews have found little direct evidence for a causal relationship between the provision of advice and physical health and limited evidence for mental health improvement. This paper reports a study using a broader range of types of research evidence to construct a conceptual (logic) model of the wider evidence underpinning potential (rather than only proven) causal pathways between the provision of advice services and improvements in health. Data and discussion from 87 documents were used to construct a model describing interventions, primary outcomes, secondary and tertiary outcomes following advice interventions. The model portrays complex causal pathways between the intervention and various health outcomes; it also indicates the level of evidence for each pathway. It can be used to inform the development of research designed to evaluate the pathways between interventions and health outcomes, which will determine the impact on health outcomes and may explain inconsistencies in previous research findings. It may also be useful to commissioners and practitioners in making decisions regarding development and commissioning of advice services.
Keywords: health inequalities, logic model, poverty, primary care, social determinants of health, welfare benefits
What is known about this topic
Poverty is positively associated with poor health.
Research to date has reported that advice services lead to financial gain, but no direct evidence of physical health improvements and limited evidence of mental health improvements.
What this paper adds
A causal pathway between welfare interventions and health and well-being improvements can be constructed from the available evidence. By identifying key elements in a causal pathway via a logic model, research can be used to identify plausible ways in which an intervention improves health and also where the gaps in evidence lie.
Logic models can be used to help illuminate complex pathways from interventions to outcomes, which may be of benefit to both service planners and researchers.
Introduction
In the UK, some commissioners of local health services have pioneered the provision of advice services as part of community and primary care. These advice initiatives have been funded in the expectation that such social interventions might be expected to improve recipients’ health. The literature supports this reasoning, research clearly indicating that poverty is associated with ill-health. A recent report commissioned by the UK Government amassed evidence of a social gradient in health, with those with the lowest socioeconomic status having poorest health and a gradient to those at the highest socioeconomic status having the best health (Marmot 2010). It might be thought therefore that improvements in individual income would be associated with improved health. However, reviews of evidence (e.g. Adams et al. 2006) found no measured effect on physical health from improved welfare benefit income (which is almost always delivered to those with lower socioeconomic status). Authors of these reviews emphasise that this is an absence of evidence for the effect, rather than evidence for absence of effect. This lack of evidence may be the result of complexity, with significant challenges in establishing a clear causal pathway between intervention and health outcome.
Logic models (also known as impact or conceptual models) originate from the field of programme evaluation, and are typically diagrams or flow charts that convey relationships between contextual factors, inputs, processes and outcomes (Joly et al. 2007, Anderson et al. 2011). They are designed to read from left to right illustrating pathways between inputs, strategies, outputs, and short-term, intermediate and longer-term outcomes. Logic models can provide a visual means of examining complex chains of reasoning and can be valuable in providing a ‘roadmap’ to illustrate influential relationships and components between inputs and outcomes (Schmitz 1999, Kellog Foundation 2004). Most models described in the literature are developed via consultation exercises with experts in the field and are thus open to criticisms of being unsystematic and biased. Recent work by the team has, however, demonstrated the possibility for models to be constructed drawing on systematic review techniques (Baxter et al. 2010). The study reported here aimed to use these methods to explore available evidence regarding the potential impact of advice interventions on health outcomes.
Methods
This work used an innovative combination of logic model methods synthesising data collected using the underlying principles of the systematic review process. The research question for the review was: what are the elements in a causal pathway between advice interventions and health outcomes?
Inclusion criteria
The review searched for published peer-reviewed international papers and grey literature from the UK, with broad study design inclusion criteria to maximise the range of work encompassed in the synthesis and to underpin development of the logic model. Research published in English up to February 2010 was eligible for inclusion; the start date was set de facto by the time span of the databases searched. Designs included were intervention studies, quantitative work reporting associations, qualitative studies, systematic reviews, literature reviews and discussion papers. Papers describing links between any type of advice intervention delivered in any setting, to any population, and including all forms of outcome measures and evaluation were considered. In addition to the peer-reviewed and grey literature, we sourced local and Welsh and English data from UK Citizens Advice; no Scottish data were available.
Search strategy
For the first wave of the process, relevant published literature was identified via searching of the Medline, Embase, HMIC PscyINFO, SCI and SSCI, CINAHL, ASSIA, LISA, Sociological Abstracts, Cochrane Library, EPPI Centre and Google Scholar electronic databases. Search terms used were variants of citizens advice, advice and citizens advice bureau (the CAB does not use an apostrophe for the term ‘Citizens’).
Selection of studies for review
The initial searches retrieved 995 citations, which were screened at title and abstract level. One hundred and twenty-eight citations appeared relevant and were retrieved as full papers. The sifting and selection of papers for inclusion were carried out by two members of the research team. In addition to database searching, the reference lists of included papers were examined; there was citation searching of key papers, and experts in the field were contacted to suggest any further references. Figure 1 provides an illustration of the identification process.
Figure 1.
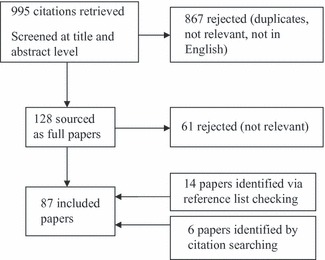
Flow chart illustrating the process of inclusion and exclusion.
Data extraction and synthesis
Papers meeting the inclusion criteria were read and data extracted using a standardised extraction form encompassing author/date, details of any intervention, measures used, reported outcomes linked to health and/or well-being, and links to other non-health impacts. See online Appendix S1 for a summary of individual studies. Following extraction, data from each column were examined by the research team and the logic model was built column by column underpinned by the evidence (Figure 2). So, for example, the first column (the intervention) was expanded by synthesising elements of interventions described across the set of papers. The second column (primary outcomes) was developed by synthesising reported study measures and outcomes, and so on. The primary outcomes were the direct aims of the intervention, such as obtaining unclaimed benefits. We defined secondary outcomes as those (i) with evidence of causal links to the intervention via the primary outcomes reported in the literature and (ii) with already established links to health or well-being.
Figure 2.
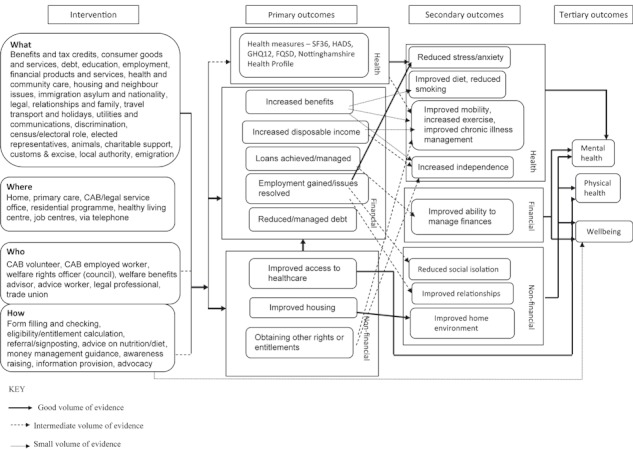
Potential links between advice interventions and health outcomes.
Quality appraisal
In contrast to standard systematic review methods, we set no quality standards on the papers reviewed other than their publication in peer-reviewed journals. We did, however, account for volume of evidence in our logic model. This has three standards, shown by differences in line thickness. The thick line indicates the greatest volume of evidence, for example, quantitative evidence from large-scale epidemiological studies. The thicker dotted line indicates less volume of evidence, for example, from before-and-after data. The thinnest dotted line indicates a low level of evidence, for example, from one or two small-scale qualitative studies.
Results
Our searches identified 87 documents that met the criteria for inclusion. Table 1 categorises the documents reviewed by study design. Data from the included documents were used to construct the logic model, describing components of an advice intervention, the short-term or primary directly measured outcomes, the secondary or more indirect benefits following the intervention, and finally potential links between these outcomes and long-term improvement in health and well-being (see Figure 2). Some examples of the evidence underpinning each component of the logic model are outlined below; detailed information is in the online Appendix S1 (Summary Table).
Table 1.
Summary of the included literature by study design
Components of an advice intervention
In the model, we have divided the intervention into four components: who delivers it, where it is delivered, what is delivered (the content of the intervention) and how (methods/format of delivery).
Primary outcomes
Short-term (primary) outcomes described in the included papers related to (i) health measures, (ii) financial gain and (iii) non-financial benefits.
Health
Fifteen papers used validated tools to assess whether there was a measurable impact of advice services on health (Memel & Gubbay 1999, Abbott & Hobby 2000, 2002, 2003, Greasley 2003, Langley et al. 2004, Powell et al. 2004, Abbott et al. 2005, Caiels & Thurston 2005, Mackintosh et al. 2006, Campbell et al. 2007, Pleasence & Balmer 2007, 2009, Jones 2009, Taylor et al. 2009). Only one paper (a review of evaluations of small UK-based debt advice initiatives) reported evidence of physical health gains; this related to the avoidance of stress-related problems (Williams 2004). No difference was found in the use of NHS services following the intervention (Abbott & Davidson 2000, Abbott & Hobby 2002). In contrast to the lack of quantitative evidence regarding direct physical health benefits, some qualitative data showed that recipients perceived that their physical health improved as a result of receiving additional income (for example, Clarke et al. 2001, Greasley 2003, Borland & Owens 2004, Greasley & Small 2005a,b, Moffatt et al. 2006a, 2010, Doncaster 2008, Moffatt & Scambler 2008).
In relation to mental health and emotional well-being, the most recent review (Adams et al. 2006) reported a statistically significant improvement in mental health measures, particularly depression, although one controlled trial did not find a positive mental health effect from debt advice (Pleasence & Balmer 2007).
Financial
The most commonly reported financial benefits arose from unclaimed benefit income and from help with managing debt. A 2006 systematic review found that the usual financial outcome was a lump sum followed by an increase in recurring benefits (Adams et al. 2006).
Non-financial
Five papers reported non-financial effects following an advice intervention (Reading et al. 2002, Ambrose & Stone 2003, Moffatt et al. 2004, Mackintosh et al. 2006, Doncaster 2008). Material benefits included free prescriptions and dental treatment, council tax exemption, respite care, meals-on-wheels, disabled parking permits, aids and adaptations around the home, help with energy use and a Community Care Alarm scheme. Wider problems addressed fell into categories of housing, employment and relationships.
Secondary/indirect outcomes
We defined secondary outcomes as those (i) with evidence of causal links to the intervention via the primary outcomes reported in the literature and (ii) with already established links to health or well-being. For example, if data show that provision of a parking permit results in increased mobility for recipients, we recorded this as a secondary outcome. The secondary outcomes of interest in our model were those that either constituted or plausibly contributed to health and well-being. As with primary outcomes, we have used the categories: health, financial and non-financial.
Health
The literature widely discusses links between financial difficulties, stress and illness (e.g. Jacoby 2002) and hence interventions to tackle these problems might be expected to reduce financial stress and improve health. An additional indirect impact may be due to a counselling effect, that people felt their health improved as a result of being listened to (Veitch & Terry 1993, Lishman-Peat 2002, Moffatt & Mackintosh 2009).
A number of papers provided data reporting what recipients said they did with increased income and some of these changes in spending may be linked to health benefits (Paris & Player 1993, Moffatt et al. 2004, Nosowska 2004, Adams et al. 2006, Levy & Payne 2006, Moffatt & Higgs 2007, Turley & White 2007, Doncaster 2008, Andersen 2009, Moffatt & Mackintosh 2009). Craig et al. (2003) categorised these uses as increased spending on essentials such as food; spending to increase mobility, such as taxis; the provision of additional goods and services such as gardeners; spending on large household items such as fridges; and spending on personal items such as presents for grandchildren. Improved mobility was also reported as an outcome of some of the other non-financial benefits such as disabled parking permits and adaptations to the house (Paris & Player 1993, Abbott & Hobby 2003, Greasley 2003, Toeg 2003, Caiels & Thurston 2005, Moffatt & Scambler 2008, Moffatt & Mackintosh 2009, Moffatt et al. 2010). Provision of meals-on-wheels services, for example, may have potential to improve diet (Craig et al. 2003).
Financial outcomes
Taylor et al. (2009) showed a strong association between what they term ‘financial capability’ (the ability of an individual to manage his/her money) and psychological well-being, such that changes in the former directly correlate with changes in the latter. Greater incapability is associated with stress and increased reporting of mental health problems, particularly depression. If an intervention can improve individuals’ financial capability, it is likely that mental health benefits will follow.
Non-financial outcomes
Other outcomes secondary to the direct impacts of advice services include reduction in social isolation (Moffatt et al. 2004), improvement in family and other relationships (Dobbie & Gillespie 2010) and improved home environment (Connor et al. 1999, Abbott 2002).
Health and well-being
Following construction of the first three columns of the logic model from the included data, we further examined the papers for evidence of links from reported outcomes to long-term health and well-being benefits. We were unable to find evidence underpinning these plausible chains of reasoning in these papers and therefore conducted further searching across the wider literature, using search terms relating to debt, employment, disposable income, housing, health-care, mental health, physical health and well-being to identify further evidence for this final step in the causal pathway between intervention and health outcomes.
This additional searching was able to locate papers that supported associations between many of the intermediate outcomes identified in the advice literature and longer term impacts on health and well-being. Studies linked improved housing and mental health benefits (Rymill & Hart 1992, Hopton & Hunt 1996, Glover 1999, Blackman & Harvey 2001, Peace & Kell 2001, Migita et al. 2005, Ho et al. 2007, Egan et al. 2010, Liddel & Morris 2009). Also, evidence was found supporting a relationship between improved housing and physical health gains (Willis 2007, Roman et al. 2009, Bambra 2010).
Discussion
The logic model synthesises evidence of plausible routes to link welfare interventions to health benefits. Previous systematic reviews have been unable to demonstrate evidence of clear health gain. One explanation may be that the research thus far has been of limited quality. Our search of the literature confirms that there has been little empirical work that is controlled or longitudinal. The lack of studies with long-term follow-up is important as physical health benefits might take time to emerge following an intervention and thus be unreported in available work. Another potential explanation for lack of evidence of effect may be that the tools used have not been sufficiently sensitive to detect change or may not be measuring outcomes of importance (Moffatt et al. 2006b, Moffatt & Mackintosh 2009). In the papers included in this review, the quantitative measures used were largely unable to detect any change in health status. Many of the qualitative studies, however, suggested that people believed that their health had improved, which may significantly impact an individual’s well-being.
A further obstacle to demonstrating a positive impact on health relates to countervailing forces in the population, such as a steeper than average trajectory of decline for the group entitled to advice (Abbott & Hobby 2000, 2002, 2003, Turley & White 2007). Therefore, the demonstration of significant positive effects using standard baseline and outcome measures presents considerable challenges.
A further possible reason for the failure to find an effect is conceptual. RCTs and other trial designs focus on input and output. This has been termed a ‘black box’ view of mechanisms (Williams 2003, Connelly et al. 2007). This often works well with closed systems, such as human bodies and drugs; however, it is problematic with open systems, such as societies. Logic models, in contrast, take a systems approach and are able to portray elements and relationships within a system (Andersen 2009). The model developed here identifies how the intermediate outcomes set in train by advice services can lead towards improved health for its recipients. For example, there is evidence that financial benefits, such as disability allowance, added to non-financial benefits, such as disabled parking permits, improve people’s mobility. From other sources, we know that improved mobility improves physical and mental health. Linking these factors in a model conceptually, we can describe the pathway from financial benefits to improved mobility and to a positive effect on well-being.
The largest proportion of the evidence we identified related to positive financial outcomes following advice interventions. This primary outcome was then most commonly linked to the secondary outcome of an improvement in mental health. In particular, the literature reported a strong link between a reduction in debt and reduced stress or anxiety. We explored the potential to differentiate strength of evidence by using different thickness (or weighting) of the connecting arrows, using study design type or quantity of evidence as indicators of strength. The model we have developed includes these arrows; however, we have concerns that this may indicate only where links may be more feasible to demonstrate in empirical work, rather than representing true strength of relationships. The further development of methods for differentiating evidence in logic models is an area worth exploring in future studies.
This work may be criticised for departing from standard systematic review methods in a number of ways relating to quality appraisal by including diverse sources of evidence, treating study designs as equal and not carrying out a critical evaluation of included papers. A standard review would have excluded much of the literature sourced here. We would argue that while quality criteria and likelihood of bias in study design are key aspects to consider, the building of the logic model was strengthened by drawing on all available literature (cf. Dorwick et al. 2009). As described above, questions of quality were considered in development of the model linkages. The type of included evidence must be considered, however, in drawing conclusions from this review. In terms of the review itself, our use of terms related to ‘advice’ might have resulted in the exclusion of relevant material from countries in which this term does not have the welfare implications it evidently has in Anglo-American contexts.
This evidence-based logic model provides a framework to inform both researchers and practitioners. The model illuminates the complexity of elements at all phases of a causal pathway from intervention to long-term impacts on health and well-being.
For practitioners, the model has at least three uses. First, it provides a graphic representation of where evidence has been reported for associations between elements. This is useful to support decisions regarding service provision. Second, it may be used to inform decisions regarding the type of provision to fund. Third, it may help practitioners to identify and develop linkages within existing services. The finding of some indications that those with fewer financial concerns might smoke less, for example, might encourage practitioners to combine the offer of a welfare benefits check-up with a stop-smoking service.
For researchers, the model indicates where research might be directed to test the causal chain. Currently, the link between advice and financial outcomes is well demonstrated, with further work required to investigate other relationships in the proposed model. An economic modelling approach to examine financial outcomes in relation to intervention costs would, however, be helpful. We believe that the model identifies the range of variables and potential outcomes that should be considered in any studies, and provides a framework for future research.
Acknowledgments
We acknowledge Jo Abbott, Wendy Baird, Jo Cooke, Paolo Gardois, Melanie Gee, Geoff Green, Julie Hirst, Anthony Kessel, Steve Minter, Suzanne Moffatt, Sarah Salway, Deborah Shields, Rupert Suckling, Angela Tod, Guy Weston and Jane Woodford. Thanks to the two anonymous referees for this journal for their advice.
Source of funding
Work was funded by Derbyshire County Primary Care Trust and NIHR and is an NIHR CLAHRC South Yorkshire project. NIHR CLAHRC for South Yorkshire acknowledges funding from the National Institute of Health Research. The views and opinions expressed are those of the authors, and not necessarily those of the NHS, the NIHR or the Department of Health. CLAHRC SY would also like to acknowledge the participation and resources of their partner organisations, particularly Rotherham NHS. Further details can be found at http://www.clahrc-sy.nihr.ac.uk.
Conflict of interest
Gerard Crofton-Martin is National Development Officer for Citizens Advice, which is one of the main UK organisations that provide advice services of the type examined in this paper. His contribution to this paper was in providing data from Citizens Advice and in discussion of report drafts.
Appendix S1 Summary table [for publication on web].
References
- Abbott B. Workplace and employment characteristics of Citizens’ Advice Bureau (CAB) clients. Employee Relations. 2007;29(3):262–279. [Google Scholar]
- Abbott S. Prescribing welfare benefits advice in primary care: is it a health intervention, and if so, what sort? Journal of Public Health. 2002;24(4):307–312. doi: 10.1093/pubmed/24.4.307. URL http://jpubhealth.oxfordjournals.org/cgi/content/abstract/24/4/307. [DOI] [PubMed] [Google Scholar]
- Abbott S, Davidson L. Easing the burden on primary care in deprived urban areas: a service model. Primary Health Care Research and Development. 2000;1(04):201–206. [Google Scholar]
- Abbott S, Hobby L. Welfare benefits advice in primary care: evidence of improvements in health. Health and Social Care in the Community. 2000;11:168–174. doi: 10.1046/j.1365-2524.2003.00414.x. [DOI] [PubMed] [Google Scholar]
- Abbott S, Hobby L. What is the Impact on Individual Health of Services in Primary Health Care Settings Which Offer Welfare Benefits Advice. Health and Community Care Research Unit, University of Liverpool; 2002. , Liverpool, UK. [DOI] [PubMed] [Google Scholar]
- Abbott S, Hobby L. Who uses welfare benefits advice services in primary care. Health & Social Care in the Community. 2003;11(2):168–174. doi: 10.1046/j.1365-2524.2003.00414.x. [DOI] [PubMed] [Google Scholar]
- Abbott S, Hobby L, Cotter S. What is the impact on individual health of services in general practice settings which offer welfare benefits advice? Health & Social Care in the Community. 2005;14(1):1–8. doi: 10.1111/j.1365-2524.2005.00582.x. [DOI] [PubMed] [Google Scholar]
- Adams J, White M, Moffatt S, Howel D, Mackintosh J. A systematic review of the health, social and financial impacts of welfare rights advice delivered in healthcare settings. BMC Public Health. 2006;6:81. doi: 10.1186/1471-2458-6-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ambrose P, Stone J. Eleven plus to one. Social Policy. 2003;11(2):1–2. [Google Scholar]
- Andersen SH. Unemployment and subjective well-being a question of class? Work and Occupations. 2009;36(1):3–25. [Google Scholar]
- Anderson L, Petticrew M, Rehfuess E, Armstong R, Ueffing E, Baker P, Francis D, Tugwel P. Using logic models to capture complexity in systematic reviews. Research Synthesis Methods. 2011;2:33–42. doi: 10.1002/jrsm.32. [DOI] [PubMed] [Google Scholar]
- Atkinson A, McKay S, Kempson E, Collard S. Levels of financial capability in the UK: results of a baseline survey. Public Money & Management. 2006;47:29–36. [Google Scholar]
- Anyadike-Danes M. What is the problem, exactly? The distribution of Incapacity Benefit claimants’ conditions across British regions. Policy Studies. 2010;31:187–202. [Google Scholar]
- Anyadike-Danes M, McVicar D. Has the boom in incapacity benefit claimant numbers passed its peak? Fiscal Studies. 2008;29:415–434. [Google Scholar]
- Bambra C, Gibson M, Amanda S, Wright K, Whitehead M, Petticrew M. Tackling the wider social determinants of health and health inequalities: evidence from systematic reviews. Journal of Epidemiology and Community Health. 2010;64(4):284–291. doi: 10.1136/jech.2008.082743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bambra C, Givson M, Sowden A, Wright K, Whitehead M, Petticrew M. Tackling the wider social determinants of health and health inequalities: evidence from systematic reviews. Journal of Epidemiology and Community health. 2010;64:284–291. doi: 10.1136/jech.2008.082743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baxter S, Killoran A, Kelly MP, Goyder E. Synthesizing diverse evidence: the use of primary qualitative data analysis methods and logic models in public health reviews. Public Health. 2010;124(2):99–106. doi: 10.1016/j.puhe.2010.01.002. [DOI] [PubMed] [Google Scholar]
- Beer SF, Marcella R, Baxter G. Rural citizens’ information needs: a survey undertaken on behalf of the Shetland Islands Citizens Advice Bureau. Journal of Librarianship and Information Science. 1998;30(4):223–240. [Google Scholar]
- Blackman T, Harvey J. Housing renewal and mental health: a case study. [References] Journal of Mental Health. 2001;10(5):571–583. [Google Scholar]
- Borland J, Owens D. Welfare Advice in General Practice: The Better Advice, Better Health Project in Wales. Citizens Advice Cymru; 2004. , Bangor. [Google Scholar]
- Buck A, Pleasence P, Balmer N. Do citizens know how to deal with legal issues? Some empirical insights. Journal of Social Policy. 2008;37:661–681. [Google Scholar]
- Burns T, Catty J, Becker T, et al. The effectiveness of supported employment for people with severe mental illness: a randomised controlled trial. Lancet. 2007;370:1146–1152. doi: 10.1016/S0140-6736(07)61516-5. [DOI] [PubMed] [Google Scholar]
- Caiels J, Thurston M. Evaluation of the Warrington District CAB GP Outreach Project. Chester, UK: Chester College of Higher Education - Centre for Public Health Research; 2005. [Google Scholar]
- Campbell J, Winder R, Richards SH, Hobart J. Exploring the relationships between provision of welfare benefits advice and the health of elderly people: a longitudinal observational study and discussion of methodological issues. Health & Social Care in the Community. 2007;15(5):454–463. doi: 10.1111/j.1365-2524.2007.00704.x. [DOI] [PubMed] [Google Scholar]
- Citizens Advice Bureau Outcomes of advice. 2010. [WWW document]. URL http://www.citizensadvice.org.uk/index/aboutus/outcomes_of_advice.htm (accessed on 20/8/2012)
- Clarke K, Sarre S, Glendinning C. FWA’s well family service evaluation report. 2001. [WWW document]. URL https://www.escholar.manchester.ac.uk/uk-ac-man-scw:4b277 (accessed on 29/5/2012)
- Connelly JB, Duaso MJ, Butler G. A systematic review of controlled trials of interventions to prevent childhood obesity and overweight: a realistic synthesis of the evidence. Public Health. 2007;121(7):510–517. doi: 10.1016/j.puhe.2006.11.015. [DOI] [PubMed] [Google Scholar]
- Connor J, Rodgers A, Priest P. Randomised studies of income supplementation: a lost opportunity to assess health outcomes. Journal of Epidemiology and Community Health. 1999;53(11):725–730. doi: 10.1136/jech.53.11.725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coppel DH, Packham CJ, Varnam MA. Providing welfare rights advice in primary care. Public Health. 1999;113(3):131–135. doi: 10.1016/s0033-3506(99)00137-7. [DOI] [PubMed] [Google Scholar]
- Craig G, Dornan P, Bradshaw J, Garbutt S, Mumtaz S, Syed A, Ward A. Underwriting citizenship for older people. Benefits. 2003;11(3):187–192. [Google Scholar]
- Cullen L. Out of the picture: CAB evidence on mental health and social exclusion. 2004. [WWW document]. URL http://www.citizensadvice.org.uk/outofthepicture.pdf (accessed on 28/5/2012)
- Day L, Collard S, Hay C. Money Advice Outreach Evaluation: Qualitative Outcomes for Clients. London, UK: LSRC; 2008. URL http://www.justice.gov.uk/downloads/publications/research-and-analysis/lsrc/2008/DebtOutreachOutcomesClients.pdf (accessed on 28/5/2012) [Google Scholar]
- DeSouza M, Sycamore M, Little S, Kirker S. The Pappworth Early Rehabilitation Programme: vocational outcomes. Disability and Rehabilitation. 2007;29(8):671–677. doi: 10.1080/09638280600926538. [DOI] [PubMed] [Google Scholar]
- Dobbie L, Gillespie M. 2010. The health benefits of financial inclusion: a literature review report for NHS greater glasgow and clyde louise dobbie and morag gillespie scottish poverty information unit May 2010 [WWW document]. URL http://www.equalitiesinhealth.org/documents/HealthBenefitsofFIfinalreport.pdf (accessed on 28/5/2012)
- Doncaster PCT. Final Monitoring Report (GM08) Doncaster, UK: Doncaster PCT (Grey Literature); 2008. [Google Scholar]
- Dowrick C, Gask L, Edwards S, et al. Researching the mental health needs of hard-to-reach groups: managing multiple sources of evidence. BMC Health Services Research. 2009;9:226. doi: 10.1186/1472-6963-9-226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dowling S, Joughin C, Logan S, Laing G, Roberts H. Financial benefits and child health. 2003. [WWW document]. URL http://www.barnardos.org.uk/incomestudy27_01.pdf (accessed on 28/5/2012)
- Egan M, Kearns A, Mason P, et al. Protocol for a mixed methods study investigating the impact of investment in housing, regeneration and neighbourhood renewal on the health and wellbeing of residents: the GoWell programme. BMC Medical Research Methodology. 2010;10:41. doi: 10.1186/1471-2288-10-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ennals S. Providing citizens’ advice in general practice. British Medical Journal. 1993;306:1494. doi: 10.1136/bmj.306.6891.1494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finch J, Patel B, Nacra A. Citizens’ advice bureaux. British Journal General Practice. 1993;43:481–482. [Google Scholar]
- Fruin C, Pitt PI. Welfare benefit promotion within a district general hospital rheumatology centre: a joint project with the local Citizens Advice Bureau. Musculoskeletal Care. 2008;6(4):211–219. doi: 10.1002/msc.133. [DOI] [PubMed] [Google Scholar]
- Galvin K, Sharples A. Citizens Advice Bureaux in general practice: an illuminative evaluation. Health and Social Care in the Community. 2000;8(4):277–282. doi: 10.1046/j.1365-2524.2000.00249.x. [DOI] [PubMed] [Google Scholar]
- Gillespie M, Dobbie L, Mulvey G, Gallacher Y. Money Advice for Vulnerable Groups: Final Evaluation Report. Glasgow, UK: Scottish Executive; 2007. URL http://www.scotland.gov.uk/Publications/2007/03/22115958/0 (accessed on 28/5/2012) [Google Scholar]
- Glover N. Mental health and housing: a crisis on the streets? Journal of Social Welfare and Family Law. 1999;21(4):327–337. [Google Scholar]
- Greasley P. The Health Plus Project: Advice Workers in Primary Care in Inner City Bradford: Evaluation Report. Bradford, UK: Department of Community and Primary Care, School of Health Studies, University of Bradford; 2003. URL http://www.phn-bradford.nhs.uk/NR/rdonlyres/078B7453-4EAA-4B5C-93B1-C58E5A91C868/0/TheHealthPlusProject20012003.pdf (accessed on 28/5/2012) [Google Scholar]
- Greasley P, Small N. Welfare Advice in Primary Care. School of Health Studies, University of Bradford; 2002. URL http://www.judithemanuel.co.uk/docs/welfare.pdf (accessed on 28/5/2012) [Google Scholar]
- Greasley P, Small N. Providing welfare advice in general practice: referrals, issues and outcomes. Health & Social Care in the Community. 2005a;13(3):249–258. doi: 10.1111/j.1365-2524.2005.00557.x. [DOI] [PubMed] [Google Scholar]
- Greasley P, Small N. Establishing a welfare advice service in family practices: views of advice workers and primary care staff. Family Practice. 2005b;22(5):513–519. doi: 10.1093/fampra/cmi047. [DOI] [PubMed] [Google Scholar]
- Hanratty B, Jacoby A, Whitehead M. Socioeconomic differences in service use, payment and receipt of illness-related benefits in the last year of life: findings from the British Household Panel Survey. Palliative Medicine. 2008;22(3):248–255. doi: 10.1177/0269216307087140. [DOI] [PubMed] [Google Scholar]
- Harding R, Sherr L, Sherr A, Moorhead R, Singh S. Evaluation of welfare rights advice in primary care: the general practice perspective. Health Social Care Community. 2002;10(4):417–422. doi: 10.1046/j.1365-2524.2002.00393.x. [DOI] [PubMed] [Google Scholar]
- Harding R, Sherr L, Sherr A, Moorhead R, Singh S. Welfare rights advice in primary care: prevalence, processes and specialist provision. Family Practice. 2003;20(1):48–53. doi: 10.1093/fampra/20.1.48. [DOI] [PubMed] [Google Scholar]
- Ho PS, Kroll T, Kehn M, Anderson P, et al. Health and housing among low-income adults with physical disabilities. Journal of Health Care for the Poor and Underserved. 2007;18(4):902–915. doi: 10.1353/hpu.2007.0098. [DOI] [PubMed] [Google Scholar]
- Hobby L. More lolly, more jolly... strong association between low income and ill-health A. S. Health Service Journal. 1999;109(5671):26. [PubMed] [Google Scholar]
- Hobby L, Emanuel J. Citizen’s Advice Bureaux in Primary Care in England and Wales A Review of Available Information. Liverpool, UK: Health and Community Care Research Unit; 1998. [Google Scholar]
- Hopton JL, Hunt SM. Housing conditions and mental health in a disadvantaged area in Scotland. Journal of Epidemiology & Community Health. 1996;50(1):56–61. doi: 10.1136/jech.50.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoskins R, Cater D. Welfare benefits’ screening and referral: a new direction for community nurses? Health Social Care Community. 2000;8:390–397. doi: 10.1046/j.1365-2524.2000.00264.x. [DOI] [PubMed] [Google Scholar]
- Hoskins RAJ, Smith LN. Nurse-led welfare benefits screening in a General Practice located in a deprived area. Public Health. 2002;116(4):214–220. doi: 10.1038/sj.ph.1900848. [DOI] [PubMed] [Google Scholar]
- Hoskins R, Tobin J, McMaster K, Quinn T. Roll-out of a nurse-led welfare benefits screening service throughout the largest Local Health Care Co-operative in Glasgow: An evaluation study. Public Health. 2005;119(10):853–861. doi: 10.1016/j.puhe.2005.03.012. [DOI] [PubMed] [Google Scholar]
- Jacoby M. Does indebtedness influence health? A preliminary inquiry. The Journal of Law, Medicine & Amp; Ethics. 2002;30:560–571. doi: 10.1111/j.1748-720x.2002.tb00426.x. [DOI] [PubMed] [Google Scholar]
- Jenkins R, Bebbington P, Brugha T, Bhugra D, Coid J, Singleton N, Meltzer H. Mental disorder in people with debt in the general population. Psychological Medicine. 2008;38:1485–1493. doi: 10.1017/S0033291707002516. [DOI] [PubMed] [Google Scholar]
- Joly BM, Polyak G, Davis M, Brewster J, Tremain B, Raevsky C, Beitsch L. Linking accreditation and public health outcomes: a logic model approach. Journal of Public Health Management and Practice. 2007;13(4):349–356. doi: 10.1097/01.PHH.0000278027.56820.7e. [DOI] [PubMed] [Google Scholar]
- Jones K, Shiell A. Outcomes of a longitudinal study of citizens advice service clients in wales. 2009. [WWW document] URL http://www.citizensadvice.org.uk/index/policy/study_<of_cab_clients_in_wales.htm (accessed on 28/5/2012)
- Kellog Foundation . The Logic Model Development Guide. Kellog Foundation; 2004. [WWW document]URL http://www.exinfm.com/training/pdfiles/logicModel.pdf (accessed 28/5/2012) [Google Scholar]
- Langley C, et al. Using the Health Assessment Questionnaire and welfare benefits advice to help people disabled through arthritis to access financial support. Rheumatology. 2004;43(7):863–868. doi: 10.1093/rheumatology/keh184. [DOI] [PubMed] [Google Scholar]
- Levy J, Payne M. Welfare rights advocacy in a specialist health and social care setting: a service audit. British Journal of Social Work. 2006;36(2):323–331. [Google Scholar]
- Liddell C, Morris C. Tackling fuel poverty and impacts on human health: a review of recent evidence. Energy Policy. 2009;38:2987–2997. [Google Scholar]
- Lishman-Peat GJB. Welfare benefits take-up project in primary care in Wakefield. Benefits. 2002;10:45–48. [Google Scholar]
- Lucas PJ, McIntosh K, Petticrew M, Roberts H, Shiell A. Financial benefits for child health and well-being in low income or socially disadvantaged families in developed world countries. Cochrane Database of Systematic Reviews (Online) 2008 doi: 10.1002/14651858.CD006358.pub2. Issue 2. Art. No: CD006358. URL http://search.ebscohost.com/login.aspx?direct=true&db=cmedm&AN=18425950&site=ehost-live (accessed on 28/5/2012) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackintosh J, White M, Howel D, Chadwick T, Moffatt S, Deverill M, Sandell A. Randomised controlled trial of welfare rights accessed via primary health care: pilot study. BMC Public Health. 2006;6 doi: 10.1186/1471-2458-6-162. pp. 162. doi: 10.1186/1471-2458-6-162. URL http://www.biomedcentral.com/1471-2458/6/162 (accessed on 28/5/2012) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcella R, Baxter G. Citizenship information service provision in the United Kingdom: a study of 27 case agencies. Journal of Librarianship and Information Science. 2000;32(1):9–25. [Google Scholar]
- Marmot M. Fair Society, Healthy Lives: Strategic Review of Health Inequalities in England Post 2010. London, UK: Department of Health; 2010. URL http://www.instituteofhealthequity.org/projects/fair-society-healthy-lives-the-marmot-review (accessed on 28/5/2012) [Google Scholar]
- Memel D, Gubbay D. Welfare benefits advice in primary care. British Journal of General Practice. 1999;49(449):1032–1033. [Google Scholar]
- Middleton H, Maunder B, Vanes J, et al. Citizens’ advice in general practice. British Medical Journal. 1993;307:504. doi: 10.1136/bmj.307.6902.504-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Migita R, Yanagi H, Tomura S. Factors affecting the mental health of residents in a communal-housing project for seniors in Japan. Archives of Gerontology & Geriatrics. 2005;41(1):1–14. doi: 10.1016/j.archger.2004.10.007. [DOI] [PubMed] [Google Scholar]
- Moffatt S, Higgs P. Charity or entitlement? Generational habitus and the welfare state among older people in North-east England. Social Policy & Administration. 2007;41(5):449–464. [Google Scholar]
- Moffatt S, Mackintosh J. Older people’s experience of proactive welfare rights advice: qualitative study of a South Asian community. Ethnicity & Health. 2009;14(1):5–25. doi: 10.1080/13557850802056455. [DOI] [PubMed] [Google Scholar]
- Moffatt S, Scambler G. Can welfare-rights advice targeted at older people reduce social exclusion? Ageing and Society. 2008;28(6):875–899. [Google Scholar]
- Moffatt M, Stacy R, Downey D, Hudson ESW. The impact of welfare advice in primary care: a qualitative study. Critical Public Health. 2004;14(3):295–319. [Google Scholar]
- Moffatt S, Mackintosh J, White M, Howel D, Sandell A. The acceptability and impact of a randomised controlled trial of welfare rights advice accessed via primary health care: qualitative study. BMC Public Health. 2006a;6:163. doi: 10.1186/1471-2458-6-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moffatt S, White M, Mackintosh J, Howel D. Using quantitative and qualitative data in health services research – what happens when mixed method findings conflict? BMC Health Services Research. 2006b;6:28. doi: 10.1186/1472-6963-6-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moffatt S, Noble E, Exley C. “Done more for me in a fortnight than anybody done in all me life.” How welfare rights advice can help people with cancer. BMC Health Services Research. 2010;10:259. doi: 10.1186/1472-6963-10-259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nosowska G. A delay they can ill afford: delays in obtaining Attendance Allowance for older, terminally ill cancer patients, and the role of health and social care professionals in reducing them. Health & Social Care in the Community. 2004;12(4):283–287. doi: 10.1111/j.1365-2524.2004.00496.x. [DOI] [PubMed] [Google Scholar]
- Paris JA, Player D. Citizens’ advice in general practice. BMJ: British Medical Journal. 1993;306(6891):1518–1520. doi: 10.1136/bmj.306.6891.1518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peace R, Kell S. Mental health and housing research: housing needs and sustainable independent living. Social Policy Journal of New Zealand/Te Puna Whakaaro. 2001;(Issue 17):101–123. [Google Scholar]
- Pleasence P, Balmer N. Changing fortunes: results from a randomized trial of the offer of debt advice in England and Wales. Journal of Empirical Legal Studies. 2007;4(3):651–673. [Google Scholar]
- Pleasence P, Balmer NJ. Mental health and the experience of social problems involving rights: findings from the United Kingdom and New Zealand. Psychiatry, Psychology and Law. 2009;16(1):123–140. [Google Scholar]
- Pleasence P, Balmer N, Buck A. Health Professionals as Rights Advisers: Rights Advice and Primary Healthcare Services. Legal Services Research Centre, Legal Services Commission; 2007. [WWW document]. URL http://lsrc.org.uk/publications/doctors.pdf (accessed on 28/5/2012) [Google Scholar]
- Popay J, Kowarzik U, Mallinson S, Mackian S, Barker J. Social problems, primary care and pathways to help and support: addressing health inequalities at the individual level. Part I: the GP perspective. Journal of Epidemiology and Community Health. 2007;61(11):966–971. doi: 10.1136/jech.2007.061937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Popay J, Kowarzik U, Mallinson S, Mackian S, Barker J. Social problems, primary care and pathways to help and support: addressing health inequalities at the individual level. Part II: lay perspectives. Journal of Epidemiology and Community Health. 2007;61(11):972–977. doi: 10.1136/jech.2007.061945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porter H. Prescribing citizen’s advice. The Health Summary (The Fundholding Summary) 1998. 1998;XV(2):9–10. [Google Scholar]
- Powell J, Langley C, Kirwan J, Gubbay D, Memel D, Pollock J, Means R, Hewlett S. Welfare rights services for people disabled with arthritis integrated in primary care and hospital settings: set-up costs and monetary benefits. Rheumatology. 2004;43(9):1167–1172. doi: 10.1093/rheumatology/keh278. [DOI] [PubMed] [Google Scholar]
- Reading R, Steel S, Reynolds S. Citizens advice in primary care for families with young children. Child Health Care and Development. 2002;28(1):39–45. doi: 10.1046/j.1365-2214.2002.00241.x. [DOI] [PubMed] [Google Scholar]
- Roman CG, Knight CR, Chalfin A, Popkin SJ. The relation of the perceived environment to fear, physical activity, and health in public housing developments: evidence from Chicago. Journal of Public Health Policy. 2009;30:S286–S308. doi: 10.1057/jphp.2008.62. [DOI] [PubMed] [Google Scholar]
- Rymill A, Hart T. Breaking new ground: shared supported housing for people with mental health related difficulties. Australian Social Work. 1992;45(4):21–26. [Google Scholar]
- Sanderson D, Mahon J. An Interim Evaluation on the “Primary Care as a Community Resource” Project Final Report. [Grey Literature] Doncaster, UK: University of York; 2003. [Google Scholar]
- Schmitz C. Everything you Wanted to Know About Logic Models but were Afraid to Ask. Kellog Foundation; 1999. [WWW document] URL http://www.insites.org/documents/logmod.htm (accessed on 28/5/2012) [Google Scholar]
- Sherr L, Hardy R, Singh S, Sherr A, Moorhead R. A Stitch in Time-Accessing and Funding Welfare Rights Through Health Service Primary Care. 2002. [WWW document] URL http://www.lho.org.uk/viewResource.aspx?id=8763 (accessed on 28/5/2012) [Google Scholar]
- Sherratt M, Jones K, Middleton P. A citizens’ advice service in primary care: improving patient access to benefits. Primary Health Care Research and Development. 2000;1:139–146. [Google Scholar]
- Smith M, Patel A. Money advice outreach evaluation: cost and effectiveness of the outreach pilots. 2008. [WWW document]. URL http://www.justice.gov.uk/downloads/publications/research-and-analysis/lsrc/DebtOutreachCostEffectiveness.pdf (accessed on 28/5/2012)
- Taylor M, Jenkins S, Sacker A. Financial capability and wellbeing. Evidence from the BHPS. 2009. [WWW document]. URL http://www.fsa.gov.uk/pubs/occpapers/op34.pdf (accessed on 28/5/2012)
- Toeg D. Proactive, targeted benefits advice for older people in general practice: a feasibility study. Health & Social Care in the Community. 2003;11(2):124–128. doi: 10.1046/j.1365-2524.2003.00412.x. [DOI] [PubMed] [Google Scholar]
- Turley C, White C. Assessing the Impact of Advice for People with Debt Problems. London, UK: Legal Services Commission; 2007. [Google Scholar]
- Veitch T, Terry A. Citizens’ advice in general practice. Patients benefit from advice. British Medical Journal. 1993;307:262. doi: 10.1136/bmj.307.6898.261-b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiggan J, Talbot C. The Benefits of Welfare Rights Advice: A Review of the Literature. 2006. [WWW document] URL http://nawra.org.uk/Documents/Benefitsofwelfarerightsadvicelitreview.pdf (accessed on 28/5/2012) [Google Scholar]
- Williams GH. The determinants of health: structure, context and agency. Sociology of Health & Illness. 2003;25(3):131–154. [PubMed] [Google Scholar]
- Williams TOM. Review of research into the impact of debt advice. 2004. [WWW document] URL http://www.justice.gov.uk/downloads/publications/research-and-analysis/lsrc/2005/impactlitrev.pdf (accessed on 28/5/2012)
- Willis L. Housing Subsidy and Self Perception of Well-Being: Does Type of Housing Subsidy make a Difference in Residents’ Perceptions of Mental and Physical Health? Columbia, SC: University of Missouri; 2007. URL https://mospace.umsystem.edu/xmlui/handle/10355/4734 (accessed on 28/5/2012) [Google Scholar]
- Winder R, Richards SH, Wyatt K, Campbell J. Receiving specialist welfare benefit advice within Social Services: a qualitative interview study of older people and their carers. Research, Policy and Planning. 2008;26(1):33–43. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


