Abstract
Background
Researchers have linked bipolar disorder to elevations in reward sensitivity and positive affect. Little is known, however, about how people with bipolar disorder respond to rewards and positive affect and how these tendencies relate to functioning or quality of life.
Methods
Persons diagnosed with bipolar I disorder and matched controls completed the Response to Positive Affect (RPA) measure and the Brief Quality of Life in Bipolar Disorder scale. Bipolar participants also completed the Reward Responses Inventory, which we designed to assess the extent to which participants avoid rewarding activities to prevent mania. A subsample of participants with bipolar disorder completed a positive mood induction procedure to examine the validity of the Response to Positive Affect scale.
Results
The majority of bipolar participants reported avoiding at least one rewarding activity as a means of preventing mania. In addition, people with bipolar I disorder reported more dampening responses to positive affect than did control participants. Dampening positive emotions was related to lower quality of life.
Limitations
This study does not address whether responses to affect and reward are related to the longitudinal course of symptoms.
Conclusions
These findings suggest that people with bipolar I disorder seem to be aware of the potential of goal achievements to trigger mania, and many people with bipolar disorder seem to take steps to avoid positive emotion and reward.
Keywords: Bipolar Disorder, Responses to Positive Affect, Reward Sensitivity, Positive Emotion
Persons diagnosed with bipolar I disorder face a dilemma when trying to prevent manic episodes. Mania is characterized in part by intense positive emotion, and in the past two decades, research has revealed the role of goal pursuit and achievement in the onset of mania, as we review below. These facts highlight the predicament faced by those who suffer from bipolar disorder: while seeking the same positive experiences and achievements that we all pursue, people with bipolar disorder must simultaneously view these experiences as signs that they may be headed into a manic episode. On one hand is the possibility of mania, which will disrupt many aspects of their lives. But the alternative is also unpleasant – disengagement from the positive emotions and goal pursuits that people value so highly.
The study reported here was designed to examine how people with bipolar I disorder respond to positive emotions and rewarding activities. We begin by briefly reviewing research on two topics: The first is the roles of reward sensitivity and positive emotionality in mania. The second is mania prevention strategies among persons with bipolar I disorder.
Prior studies have found that reward sensitivity is stably elevated through periods of remission in bipolar I disorder (Meyer et al., 2001) and in college students at risk for hypomania (Meyer et al., 1999). This elevation in reward sensitivity has been found to be a trait-like feature of persons with bipolar disorders (Meyer et al., 2001). However, changes in the activity of this system, such as temporarily increased goal pursuit, can facilitate the onset of manic symptoms (Johnson, 2005). For example, life events that involve goal attainment precede the onset of manic symptoms in bipolar I disorder (Johnson et al., 2000; Johnson et al., 2008b) and bipolar spectrum disorders (Nusslock et al., 2007). Increased involvement in the pursuit of goals prospectively relates to longitudinal increases in manic symptoms (Lozano & Johnson, 2001), and has been used as a prodromal sign of an impending manic episode (Lam & Wong, 1997; Molnar et al., 1988). Trait-like elevations in positive emotionality are also associated with a more severe course of mania (Gruber et al., 2008; Gruber et al., 2009) and have been used on screening scales for manic temperament (Akiskal et al., 2005). Further, people with bipolar I disorder commonly report short-term increases in positive affect as early signs of mania (Molnar et al., 1988; Smith & Tarrier, 1992).
People diagnosed with bipolar disorder report responding in diverse ways when experiencing early signs of mania. Lam and colleagues (2001) classified the responses into three broad categories: Modifying Excessive Behavior (e.g., reducing the number of tasks to a more realistic amount), Early Medical Intervention (e.g., seeing a doctor), and Stimulating Strategies (e.g., enjoying the feeling of high). At 18-month follow-up, Modifying Excessive Behavior was related to decreases in manic symptoms, whereas engaging in Stimulating Strategies was related to increases in manic symptoms.
These studies focused on coping responses after symptoms emerged. The current study extends this work by asking about responses to reward and positive affect in general, not just after symptoms have emerged. Given the evidence that increases in goal engagement and positive mood states during remission can precede the development of manic symptoms, how do people with bipolar disorder respond to these states?
Research outside bipolar disorder has suggested that there are strong individual differences in propensities to amplify or diminish positive emotion. Emotion-amplifying responses (e.g., thinking about how happy one feels) are aimed at maintaining or enhancing the experience of positive emotion (cf. Bryant, 1989; Feldman et al., 2008). In contrast, dampening responses (e.g., thinking “this will never last”) act to diminish positive emotion (Quoidbach et al., 2010; Wood et al., 2003). In normal samples, use of positive-emotion amplifying responses relates to higher well-being, and dampening responses correlate with low self-esteem, depression, and poorer well-being (Quoidbach et al., 2010).
Researchers have begun to examine these responses among people with bipolar spectrum disorders. Although people at risk for and diagnosed with bipolar spectrum disorder have reported frequent use of emotion-amplifying strategies in comparisons with control participants (Feldman et al., 2008; Johnson et al., 2008a; Raes et al., 2010), the available studies have been limited in that researchers have not included participants with bipolar I disorder, and only bipolar I disorder is defined by impairment as a consequence of high moods. People suffering from bipolar I disorder may have an incentive to reduce positive affect compared to those diagnosed with milder forms of disorder. This may lead to a different pattern of responses.
Moreover, beyond responses to positive affect, we noted above that goal engagement predicts increases in manic symptoms and is often described as one of the early signs of mania. Thus, persons at risk for mania may have an incentive to avoid rewarding activities in order to prevent mania. To examine this possibility, we developed a new questionnaire, the Reward Responses Inventory (RRI), to assess the extent to which persons with a history of mania view goal accomplishments as potential triggers of mania and report avoiding rewarding activities in an effort to prevent mania.
If people with bipolar disorder avoid rewarding activities and dampen positive emotion, it is important to consider how these behaviors relate to quality of life among people with bipolar disorder. On one hand, it is possible that down-regulation of positive emotion is associated with lower well-being in people with bipolar disorder just as it is in people without the disorder (Quoidbach et al., 2010). On the other hand, if these strategies prevent mania, their use may be associated with increased quality of life. Understanding variation in quality of life is a particularly important goal in the study of bipolar disorder, which is associated with lower average quality of life and general functioning but also with a great deal of variation in quality of life (Hammen, Gitlin, & Altshuler, 2000; Harrow, Goldberg, Grossman, & Meltzer, 1990).
This study examined self-reports of avoidance of rewarding activities and dampening of positive emotions. We hypothesize that bipolar I disorder will be related to high levels of both avoidance of rewarding activities and dampening of positive emotions. We also examined whether reward avoidance and dampening would help explain lower quality of life observed in bipolar disorder in the context of individual differences in severity of illness history and neuroticism.
Method
Participants
The participants were 90 persons who met criteria for bipolar I disorder, as assessed by the Structured Clinical Interview for DSM-IV (SCID) for axis I disorders, and 72 control participants. Participants were community members from the Miami and Palo Alto areas recruited through advertisements placed in newspapers, flyers, online, and in public transportation sites.
Participants in the bipolar group met diagnostic criteria for bipolar I disorder, and those in the control group did not meet lifetime or current criteria for any mood disorder (including bipolar I disorder, bipolar II disorder, cyclothymia, bipolar disorder NOS, major depressive disorder, or depressive disorder NOS). All participants were native English speakers between 18 and 65 years of age. Participants were excluded if they met diagnostic criteria for substance abuse or dependence in the past year, primary psychotic disorder, a general medical condition of the central nervous system, vascular disease, degenerative disorder, a history of serious head injury, or any developmental disability or language problems that could interfere with understanding of the informed consent procedure or the study tasks and measures. Because traditional antipsychotics blunt reward sensitivity and positive affect (Abler et al., 2007), participants who were prescribed traditional antipsychotic medications were excluded. Bipolar I and control participants were matched on age and gender.
Participants completed written informed consent procedures and received compensation for their participation. All measures and procedures were approved by the institutional review boards at the University of Miami and Stanford University.
Potential participants who contacted study staff were screened by phone to determine possible diagnosis of bipolar I disorder and review demographic and medical exclusion criteria. After potential eligibility was determined, participants were invited to the University of Miami or Stanford University for a more detailed diagnostic interview. Once diagnostic measures were completed, participants completed symptom severity interviews. Bipolar participants were assessed only after achieving symptom remission. If participants with bipolar disorder achieved scores reflecting moderate symptoms (7 or higher on the Modified Hamilton Rating Scale for Depression or 6 on the Bech Rafaelsen Mania Scale), they were scheduled for monthly interviews to track symptom remission. Symptom severity interviews were repeated within two days of the questionnaire battery to ensure that symptoms remained in remission.
Materials
SCID
The Structured Clinical Interview for DSM-IV (SCID) is a commonly used and well-validated measure of DSM-IV-TR lifetime and current psychiatric diagnoses (First, Spitzer, Gibbon, & Williams, 2002). Before administering the SCID, research assistants and graduate students in clinical psychology received extensive training from the principal investigator (Johnson), including completion of didactic training, extensive role play, and establishment of reliability with a set of gold standard interviews. Inter-rater reliability was assessed by rating 10 randomly selected audio interviews. Inter-rater reliability was 1.0 for both the mania and depression modules. Course parameters such as the number of previous manic and depressive episodes and years since mania and depression onset were coded as well.
Somatotherapy Index
The Somatotherapy Index (Bauer et al., 1997) was used to obtain information about the prescribed dose, nonadherence levels, and blood serum levels for anti-depressants, anticonvulsants, lithium, and traditional and atypical neuroleptics. Dose equivalence levels were computed for each class of medication. An overall index of mood stabilizer adequacy was calculated by summing the reported dosages of lithium, valproate, carbamazepine, and atypical neuroleptics divided by their maximum recommended dosages.
Bech-Rafaelson Mania Scale (BRMS)
The BRMS (Bech et al., 1979) was used to assess the severity of manic symptoms. This 11-item interview-based measure detects changes in clinical status and has strong psychometric properties. The BRMS includes manic symptoms such as elevated mood, decreased need for sleep, increased verbal activity, increased motor activity, flight of thoughts, and increased sexual interest. Responses are scored using a 5-point rating scale, with higher scores indicating higher symptom severity. The BRMS is a unidimensional measure, with scores of 15 or below indicating hypomania, scores between 16 and 27 indicating moderate mania and scores of 28 or above indicating severe mania. The scale distinguishes between persons with and without current mania and is highly correlated with other measures of current mania (Bech, 2008). We used a set of standardized probes and obtained high inter-rater reliability (intraclass correlation = .84 based on review of 14 recordings) and acceptable internal consistency (α = .77).
Modified Hamilton Rating Scale for Depression (MHRSD)
The MHRSD (Miller et al., 1985) was used to assess the severity of depressive symptoms. This modification of the widely used Hamilton Rating Scale for Depression includes standardized probes for the interview and behavioral anchors for each rating point, to enhance the reliability of ratings compared to the original version (Hamilton, 1967). Scores for each item range from 0 to 4 or 0 to 2, with a possible total score of 52. Scores below 7 indicate recovery, whereas scores 18 and over indicate depressive relapse (Bech, 2008). This scale has excellent inter-rater reliability (intra-class correlation is .93 in published articles and among our research team members based on review of 14 recordings) and strong internal consistency (in the current sample, α = .82). The MHRSD is sensitive to changes in clinical status and is highly correlated with other measures of current depression (Miller et al., 1985). The scale has been validated as a measure of bipolar depression ((Johnson, 2008; Johnson et al., 2011).
Altman Self-Rating Mania Scale (ASRM)
The Altman Self-Rating Mania Scale (ASRM; Altman, Hedeker, Peterson, & Davis, 1997, 2001) was used to assess manic symptoms before and after the positive mood induction. The ASRM has been used for this purpose in several studies (e.g. Bopp et al., 2010; Johnson & Fulford, 2009). It includes five items measuring common manic symptoms of increased happiness, self-confidence, talkativeness, and activity, and decreased sleep. Three adjustments to this measure were required for this study. First, the item covering sleep was removed, as changes in sleep patterns would be impossible within a laboratory session. Second, the item covering “being more active” was worded as “excited,” as changes in activity level (e.g. socially, sexually) would also be unlikely during the session. Third, the response format was simplified from a wordy five-option multiple-choice format to a seven-point Likert scale ranging from “not at all” to “extremely.” This change was made due to time pressure within the session, as the effects of mood induction procedures can fade within just a few minutes (e.g. Frost & Green, 1982). The result was a very brief, 4-item measure that was administered twice; Cronbach’s alpha was .80 before the mood induction, and .84 afterward.
Responses to Positive Affect (RPA)
The RPA (Feldman et al., 2008) is a 17-item scale that was designed to assess cognitive responses to positive affect. The scale was modeled after the widely used and well-validated Ruminative Responses Scale (RRS; Treynor et al., 1991), which measures cognitive responses to negative affect. Respondents are instructed to indicate on a scale ranging from 1 (“Almost Never”) to 4 (“Almost Always”) the frequency with which they tend to respond in specific ways when feeling happy, excited, or enthused. The RPA comprises three factor-analytically derived subscales. The Dampening subscale includes 8 items that assess the tendency to respond to positive affective states with thoughts that are likely to dampen these states (e.g., “…think ‘my streak of luck is going to end’” or “…think ‘I don’t deserve this’”). In previous research scores on the Dampening scale were found to be related to more severe depression scores both cross-sectionally (Feldman et al., 2008) and prospectively (Raes, Smets, Nelis, & Schoofs et al., 2012). The Self-Focused subscale includes 4 items that assess the tendency to respond to positive affective states with thoughts about positive aspects of one’s self and goals (e.g., “…think ‘I am achieving everything’” or “…think ‘I am living up to my potential’”). The Emotion-Focused subscale includes 5 items that assess the tendency to respond to positive affective states with thoughts about that positive state (e.g., “…think about how happy you feel” or “think about how you feel up to doing everything”). Cronbach’s alphas for this sample were .85 (Dampening subscale), .78 (Self-Focused subscale), and .81 (Emotion-Focused subscale).
Because the RPA has not yet been behaviorally validated, we were interested in testing whether the RPA predicted response to a mood induction. For this validation procedure, we focused on bipolar participants because they are more likely to endorse high Dampening scores. A subset of 34 bipolar participants returned for a follow-up session at which they completed the ASRM, a positive mood induction, and then a second ASRM. The mood induction was aimed at creating a high-arousal positive affect state. Participants were instructed to think in detail about a dream coming true while upbeat music played in the background for 5 minutes. (A choice of classical or Latin music pieces, tested in pilot work, was provided.) Partial correlations were computed between the RPA subscales and the post-induction ASRM score, controlling for pre-induction ASRM score. Reported use of Self-Focused, partial r(31) = .45, p = .008, and Emotion-Focused positive affect amplification strategies, partial r(31) = .40, p = .02 were related to greater responses to the positive mood induction. Reported Dampening of positive affect was related to less response to the positive mood induction, though this result fell short of significance, partial r(31) = -.32, p = .07.
Reward Responses Inventory (RRI)
Several experts in bipolar disorder and reward sensitivity generated 21 items to capture responses to reward-related stimuli. The RRI has two subscales. The means, standard deviations, and internal consistencies are displayed in Table 1. The Reward-Triggered Mania subscale assesses whether respondents report experiencing mania after achieving important goals. The Reward Avoidance subscale assesses whether participants avoid or limit goal pursuit in social, romantic, family, educational, occupational, and creative domains as a way of preventing mania. Participants were asked to rate each item on a four-point rating scale from 1 “very false for me” to 4 “very true for me.” Because the RRI items focus specifically on experiences of mania, this scale was not administered to the control participants. Because the RRI was developed during the course of the study, only 60 participants completed it. This sample is not large enough to allow factor analytic examination of these scales. We do not expect any one person to have experienced mania after all the listed events or to have employed all the strategies, and it is possible that the sets of experiences and strategies listed will not cohere. We view the scales as multiple-act criteria (Fishbein & Ajzen, 1974), lists of behaviors that reflect the superordinate construct but are not necessarily correlated. Further psychometric work in larger samples is warranted.
Table 1.
RRI Scale Items, Internal Consistency Estimates, Means, and Standard Deviations
| Subscales and Items | α | M | SD |
|---|---|---|---|
| Reward-Triggered Mania | 0.82 | 2.5 | 0.68 |
| I have experienced mania after: | |||
| Life became too exciting. | |||
| My confidence got higher. | |||
| My work life started going well. | |||
| My social or romantic started going well. | |||
| I fell in love. | |||
| I had success in school. | |||
| I had a child. | |||
| I got engaged or married. | |||
| I had a creative accomplishment (poetry, music, etc.). | |||
| I got a promotion. | |||
| I started pursuing new goals, hopes, or dreams. | |||
| My work load or activities increased. | |||
| Reward Avoidance | 0.81 | 2.0 | 0.67 |
| To protect myself against mania, I have: | |||
| Tried to limit my social life so it is not too exciting (e.g., not seeing friends, limiting how much I go out, avoiding new people). |
|||
| Tried to limit my romantic life so it is not too exciting (e.g., not starting new relationships, limiting physical involvement, monitoring time or intensity of a new relationship). |
|||
| Tried to limit my work life so it is not too exciting (e.g., not taking on certain jobs, promotions or duties). |
|||
| Tried to limit my creative pursuits. | |||
| Tried to avoid hobbies or other fun activities. | |||
| Tried to avoid being involved in political activities or groups. | |||
| Decided not to have a child. | |||
| Did not start a new school program. |
Note. N=60.
RPA and RRI subscales appeared to index separable constructs. Correlations between the RRI and RPA subscales are shown in Table 2.
Table 2.
Correlations Among RRI and RPA Subscales among Participants with Bipolar I Disorder
| Responses to Reward and Positive Affect |
Reward- Triggered Mania |
Reward Avoidance |
Dampening | Self-Focused Emotion Amplification |
|---|---|---|---|---|
| Reward-Triggered Mania | 1.0 | - | - | - |
| Reward Avoidance | .30* | 1.0 | - | - |
| Dampening | .05 | .28* | 1.0 | |
| Self-Focused | .24 | .27* | .20 | 1.0 |
| Emotion-Focused | .17 | .09 | .12 | .73** |
Note. N=59-60 for columns 1-2, N=89 for columns 3-4
p<0.05
p<0.01.
Brief Quality of Life in Bipolar Disorder (BQOL-BD)
The BQOL-BD (Michalak, Murray, & CREST-BD, 2010) is a 12-item self-report measure designed to assess quality of life over the preceding week. This measure was designed to capture domains covered by traditional quality of life measures, but content was supplemented for bipolar-disorder-relevant concerns based on extensive input from focus groups and from an international group of researchers focused on bipolar disorder. The BQOL-BD score is the sum of 12 items designed to cover quality of life in the following domains: physical health, sleep, mood, cognitive, leisure, social, spirituality, finances, household, self-esteem, independence, and identity. The items were rated on a 5-point scale, with 1 being “Strongly disagree” and 5 “Strongly agree.” Internal consistency for BQOL-BD was 0.82 in this sample. Because the BQOL-BD became available during the course of the study, not all participants completed it.
NEO-FFI-Neuroticism Scale
To examine whether avoiding reward and dampening of positive affect were more common among persons prone to neuroticism, we used the NEO Five-Factor Inventory Neuroticism Scale (NEO-FFI; Costa & McCrae, 1992), a widely used and well-validated 12-item scale. Participants were asked to rate how much they agreed with each statement on a 5-point scale. In our sample, internal consistency was 0.90.
Results
Preliminary Analyses
Matching procedures were effective in that the bipolar and control groups did not differ in age, gender, or education level (see Table 2). Though the bipolar and control groups did not differ in terms of depressive symptoms, the bipolar I group reported more mania symptoms. As shown in Table 2, the bipolar I group reported a fairly severe illness history.
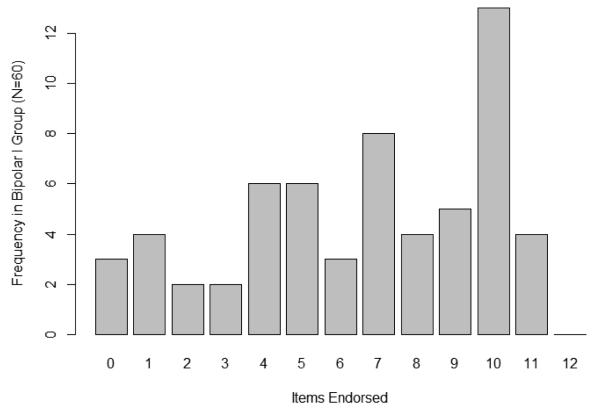
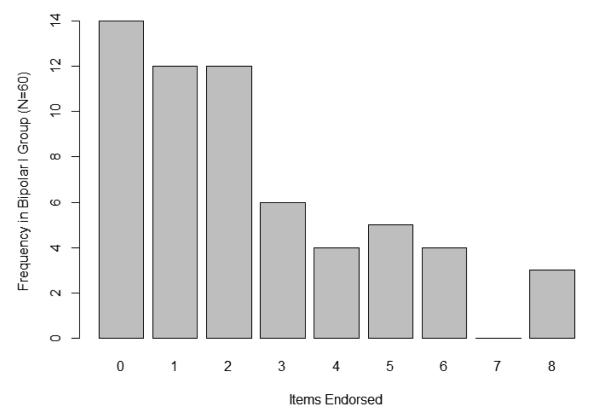
Descriptive Analyses of the Reward Responses Inventory
Almost all bipolar participants reported experiencing mania triggered by one of the events on the Reward-Triggered Mania subscale (57/60 responded “somewhat true” or “very true” to at least one event; 47/60 responded “very true” to at least one event). Most also reported engaging in at least one of the reward-limiting mania prevention strategies on the Reward Avoidance subscale (46/60 responded “somewhat true” or “very true” to at least one strategy; 28/60 responded “very true” to at least one strategy). Figures 1 and 2 show the frequency distribution of participants endorsing items as “somewhat true” or “very true” for each scale.
Figure 1.
Bar Plot of Number of Reward-Triggered Mania Items Endorsed in the Bipolar I Group
Figure 2.
Bar Plot of Number of Reward Avoidance Items Endorsed in the Bipolar I Group
Comparisons between the Bipolar and Control Groups
Bipolar I disorder participants reported more Dampening of positive feelings on the RPA (M = 16.3, SD = 5.3) than did controls (M = 12.5, SD = 3.4), t(152.4) = 5.5, p < 0.001, d = 0.83. Bipolar I disorder and control participants did not differ in their reported use of either Self-Focused, t(159) = 0.52, p = 0.60, or Emotion-Focused emotion amplifying strategies, t(159) = 1.1, p = 0.27. As noted previously, we did not administer RRI scales to the control group because the item content was not relevant to them.
Relationship of Dampening and Reward Avoidance with Quality of Life within Bipolar Disorder
We examined whether self-reported Dampening of positive affect and Reward Avoidance were correlated with self-reported quality of life (BQOL-BD) within the bipolar group. The correlation between Reward Avoidance and BQOL-BD fell short of significance, r(54) = -.24, p = .07, but Dampening was correlated with BQOL-BD, r(69) = -.40, p = .001.
We considered potential confounds that could explain the relationship between Dampening and BQOL-BD within the bipolar group, including demographics (age, gender, and years of education), disease course (BRMS scores, MHRSD scores, number of previous manic and depressive episodes, years since mania and depression onset, and presence of comorbid anxiety or substance-related disorder), treatment (antidepressant dose and total mood stabilizer adequacy), and personality (NEO Neuroticism). Of these variables, Dampening was correlated with antidepressant dosage, r(89) = .26, p = .02, comorbid anxiety disorder, r(89) = .28, p = .01, and Neuroticism, r(89) = .43, p < .001. The correlation between Dampening and BQOL-BD withstood control for antidepressant dosage and comorbid anxiety, partial r(66) = -.31, p = .01, but not for Neuroticism, partial r(64) = -.15, p = .24.
Discussion
This study was designed to examine how persons with bipolar disorder respond to positive emotion and reward. Several major findings emerged. First, almost all of the participants with bipolar I disorder reported experiencing mania shortly after achieving an important success. The present findings extend previous evidence that mania is more likely to occur after goal achievement events (Johnson et al., 2000; Johnson et al., 2008b) by showing that persons with bipolar I disorder seem to be aware of this potential trigger. Second, most persons with bipolar disorder report avoiding rewarding activities in an effort to prevent mania, and they also reported dampening positive emotions more frequently than controls. Third, dampening positive emotions was related to lower self-reported quality of life. These findings also provide support for the RPA scale, in that self-rated responses to positive affect were related to responses to a positive mood induction among persons with bipolar disorder.
It should be noted that this pattern of RPA results differs from that obtained in previous studies, in which undergraduates at risk for mania (Feldman et al., 2008; Raes et al., 2010) or who met criteria for bipolar spectrum disorders (Johnson et al., 2008a) reported more frequent emotion-amplifying responses than controls with no difference in dampening responses. It is noteworthy that those studies examined individuals at risk for mania or with bipolar spectrum disorders. The present study is the first to examine people with bipolar I disorder—other studies have not examined these responses in a sample that has experienced functional impairment as a consequence of manic symptoms.
Notwithstanding the potential clinical importance of the current findings, it is important to note several limitations. Dampening was no longer significantly correlated with Quality of Life after accounting for Neuroticism. It is likely that other personality variables, lifetime experiences related to the disorder, and broader social and individual factors shape these responses. Future research is needed, preferably employing longitudinal designs across the course of illness onset and adaptation, to understand the factors that lead some people to choose these responses to affect and reward and to determine whether the underlying vulnerabilities, as opposed to the use of these strategies, leads to lower quality of life. Future studies of Dampening, Reward Avoidance, and Neuroticism should try to address questions such as: Are these strategies effective for mania prevention? If so, what are the benefits to quality of life associated with their mania-protective effects? What are the costs associated with employing these strategies, and to what extent do the strategies causally affect quality of life? Though previous research has suggested that dampening is related to low self-esteem, depression, and poorer well-being (Feldman et al., 2008; Quoidbach et al., 2010). and that avoiding over-stimulating activities is longitudinally related to lower levels of mania over time (Lam et al., 2001), it is unknown whether use of the specific strategies studied here is related to subsequent symptoms of depression or mania. Subsequent studies can build on this one by employing prospective, longitudinal designs, by examining use of these strategies as they occur, and by experimental short-term manipulations of Dampening and Reward Avoidance.
In sum, people with bipolar disorder report avoiding some of life’s most rewarding pursuits, and they also report dampening joy and happiness. Although these regulatory responses may be intuitive based on an understanding of mania, current data suggests that they may be associated with lower quality of life. Thus, clinicians who consider advising patients about behavioral strategies for mania prevention should consider whether their interventions might affect quality of life. Psychoeducation about the relations among goal pursuit, positive emotions, and mania should be accompanied by a careful consideration of the delicate balance to be struck. Those with bipolar I disorder are obliged to navigate a narrow passage, and clinicians and researchers should be careful to ensure that due attention to preventing mania does not interfere with ongoing engagement in key domains of life and affective experience.
Table 3.
Descriptive Data
| Demographic and Disease Course Variables |
Bipolar I Mean (SD) (N=90) |
Control Mean (SD) (N=72) |
Group Difference |
|---|---|---|---|
| Age | 37.9 (11.7) | 34.6 (11.8) | t(160) = 1.8, p = 0.08 |
| Sex (% female) | 61 | 53 | χ2(1) = 0.8, p = 0.36 |
| Years Education | 14.7 (2.0) | 14.5 (2.1) | t(160) = 0.7, p = 0.51 |
| BRMS (BP-I N = 75, Control N = 55) |
2.5 (2.7) | 1.0 (1.4) | t(118.4) = 4.0, p < 0.001, d = .65 |
| MHRSD (BP-I N = 75, Control N = 55) |
3.3 (4.4) | 2.1 (3.2) | t(128) = 0.1.8, p = 0.08 |
| Previous MDEs (N = 76) | 11.1 (11.6) | ||
| Previous Hospitalizations for MDE (N = 89) |
1.2 (2.3) | ||
| Age of MDE Onset (N = 73) | 18.3 (8.8) | ||
| Previous Manic Episodes (N = 79) |
9.4 (10.4) | ||
| Previous Hospitalizations for Mania |
1.7 (3.1) | ||
| Age of Mania Onset (N = 89) | 22.1 (9.1) |
Note. BRMS = Bech Rafaelsen Mania Scale, MHRSD = Modified Hamilton Rating Scale for Depression, MDE = Major Depressive Episode per SCID interview.
Acknowledgements
We thank Lori Eisner, Daniel Fulford, Terrence Ketter, Christopher Miller, Jennifer Nam, Bailey Smith, Sarah Victor, and Esmé Weijun Wang for their assistance in conducting this study.
Footnotes
Conflicts of Interest. All authors declare that they have no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors Authors Johnson and Carver designed the study and wrote the measure items. Author Johnson was the principal investigator and Carver was the co-principal investigator. Author Marquinez coordinated data collection in Miami and helped write items. Author Gotlib supervised data collection, staff, and recruitment at Stanford. Author Miller designed and conducted the study relating scores on the Responses to Positive Affect (RPA) scale to reactivity to positive mood induction reported as a validation of the RPA. Author Edge analyzed the data and wrote the first draft of the manuscript with support from author Muhtadie and Marquinez. Authors Johnson and Carver contributed to the writing and editing of the manuscript. All authors contributed to and have approved the final manuscript.
References
- Abler B, Erk S, Walter H. Human reward system activation is modulated by a single dose of olanzapine in healthy subjects in an event-related, double-blind, placebo-controlled fMRI study. Psychopharmacology. 2007;191(3):823–833. doi: 10.1007/s00213-006-0690-y. [DOI] [PubMed] [Google Scholar]
- Akiskal HS, Mendlowicz MV, Girardin J-L, Rapaport MH, Kelsoe JR, Gillin JC, Smith TL. TEMPS-A: validation of a short version of a self-rated instrument designed to measure variations in temperament. J Affect Disord. 2005;85:45–52. doi: 10.1016/j.jad.2003.10.012. [DOI] [PubMed] [Google Scholar]
- Altman EG, Hedeker D, Peterson JL, Davis JM. The Altman Self-Rating Mania Scale. Biol Psychiatry. 1997;42:948–955. doi: 10.1016/S0006-3223(96)00548-3. [DOI] [PubMed] [Google Scholar]
- Altman EG, Hedeker D, Peterson JL, Davis JM. A comparative evaluation of three self-rating scales for acute mania. Biol Psychiatry. 2001;50:468–471. doi: 10.1016/s0006-3223(01)01065-4. [DOI] [PubMed] [Google Scholar]
- Bauer M, McBride L, Shea N, Gavin C, Holden F, Kendall S. Impact of an easy-access VA clinic-based program for patients with bipolar disorder. Psychiatr Serv. 1997;48(4):491–496. doi: 10.1176/ps.48.4.491. [DOI] [PubMed] [Google Scholar]
- Bech P. Use of rating scales in affective disorders. Eur Psychiat Rev. 2008;1:6–10. [Google Scholar]
- Bech P, Bolwig TG, Kramp P, Rafaelsen OJ. The Bech-Rafaelsen Mania Scale and the Hamilton Depression Scale: Evaluation of homogeneity and inter-observer reliability. Acta Psychiat Scand. 1979;59(4):420–430. doi: 10.1111/j.1600-0447.1979.tb04484.x. [DOI] [PubMed] [Google Scholar]
- Bopp JM, Milowitz DJ, Goodwin GM, Stevens W, Rendell JM, Geddes JR. The longitudinal course of bipolar disorder as revealed through weekly text messaging: a feasibility study. Bipol Dis. 2010;12(3):327–334. doi: 10.1111/j.1399-5618.2010.00807.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant FB. A four-factor model of perceived control: Avoiding, coping, obtaining, and savoring. J Pers. 1989;57(4):773–797. [Google Scholar]
- Costa PT, McCrae RR. Revised NEO Personality Inventory (NEO PI-R) and NEO Five-Factor Inventory (NEO-FFI) professional manual. Psychological Assessment Resources; Odessa, FL: 1992. [Google Scholar]
- Feldman G, Joormann J, Johnson S. Responses to positive affect: A self-report measure of rumination and Dampening. Cognitive Ther Res. 2008;32(4):507–525. doi: 10.1007/s10608-006-9083-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV-TR Axis I Disorders, Research Version. Patient Edition (SCID-I/P) Biometrics Research, New York State Psychiatric Institute; NY: 2002. [Google Scholar]
- Fishbein M, Ajzen I. Attitudes towards objects as predictors of single and multiple behavioral criteria. Psychol Rev. 1974;81(1):59–74. [Google Scholar]
- Frost RO, Green ML. Velten Mood Induction Procedure Effects: Duration and Postexperimental Removal. Pers Soc Psychol Bull. 1982;8(2):341–347. [Google Scholar]
- Gruber J, Culver JL, Johnson SL, Nam JY, Keller KL, Ketter TA. Do positive emotions predict symptomatic change in bipolar disorder? Bipol Dis. 2009;11(3):330–336. doi: 10.1111/j.1399-5618.2009.00679.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruber J, Johnson SL, Oveis C, Keltner D. Risk for mania and positive emotional responding: Too much of a good thing? Emotion. 2008;8(1):23–33. doi: 10.1037/1528-3542.8.1.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton M. Development of a rating scale for primary depressive illness. Br J Clin Psychol. 1967;6:278–296. doi: 10.1111/j.2044-8260.1967.tb00530.x. [DOI] [PubMed] [Google Scholar]
- Hammen C, Gitlin M, Altshuler L. Predictors of work adjustment in bipolar I patients: A naturalistic longitudinal follow-up. J Consult Clin Psych. 2000;68:220–225. doi: 10.1037//0022-006x.68.2.220. [DOI] [PubMed] [Google Scholar]
- Harrow M, Goldberg JF, Grossman LS, Meltzer HY. Outcome in manic disorders: A naturalistic follow-up study. Arch Gen Psychiatry. 1990;47:665–671. doi: 10.1001/archpsyc.1990.01810190065009. [DOI] [PubMed] [Google Scholar]
- Johnson SL. Mania and dysregulation in goal pursuit: A review. Clin Psychol Rev. 2005;25(2):241–262. doi: 10.1016/j.cpr.2004.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson SL, Cueller AK, Ruggero C, Winett-Perlman C, Goodnick P, White R, et al. Life events as predictors of mania and depression in bipolar I disorder. J Abnorm Psychol. 2008b;117(2):268–277. doi: 10.1037/0021-843X.117.2.268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson SL, Fulford D. Preventing mania: A preliminary examination of the GOALS Program. Behav Ther. 2009;40:103–113. doi: 10.1016/j.beth.2008.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson S, McKenzie G, McMurrich S. Ruminative responses to negative and positive affect among students diagnosed with bipolar disorder and major depressive disorder. Cognitive Ther Res. 2008a;32(5):702–713. doi: 10.1007/s10608-007-9158-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson SL, Morriss R, Scott J, Paykel E, Kinderman P, Kolamunnage-Dona R, Bentall RP. Depressive and manic symptoms are not opposite poles in bipolar disorder. Acta Psychiatr Scand. 2011;123(3):206–210. doi: 10.1111/j.1600-0447.2010.01602.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson SL, Sandrow D, Meyer B, Winters R, Miller I, Solomon D, et al. Increases in manic symptoms after life events involving goal attainment. J Abnorm Psychol. 2000;109(4):721–727. doi: 10.1037//0021-843x.109.4.721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lam D, Wong G, Sham P. Prodromes, coping strategies and course of illness in bipolar affective disorder – a naturalistic study. Psychol Med. 2001;31(08):1397. doi: 10.1017/s003329170100472x. [DOI] [PubMed] [Google Scholar]
- Lam D, Wong G. Prodromes, coping strategies, insight and social functioning in bipolar affective disorders. Psychol Med. 1997;27(05):1091. doi: 10.1017/s0033291797005540. [DOI] [PubMed] [Google Scholar]
- Lozano BE, Johnson SL. Can personality traits predict increases in manic and depressive symptoms? J Affect Disord. 2001;63(1-3):103–111. doi: 10.1016/s0165-0327(00)00191-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer B, Johnson SL, Carver CS. Exploring behavioral activation and inhibition sensitivities among college students at risk for bipolar spectrum symptomatology. Journal of Psychopathology& Behavioral Assessment. 1999;21:275–292. doi: 10.1023/A:1022119414440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer B, Johnson S, Winters R. Responsiveness to threat and incentive in bipolar disorder: Relations of the BIS/BAS scales with symptoms. J Psychopathol Behav. 2001;23(3):133–143. doi: 10.1023/A:1010929402770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michalak EE, Murray G, Crest BD. Development of the QoL.BD: A disorder-specific scale to assess quality of life in bipolar disorder. Bipolar Disord. 2010;12(7):727–740. doi: 10.1111/j.1399-5618.2010.00865.x. [DOI] [PubMed] [Google Scholar]
- Miller IW, Bishop SB, Norman WH, Maddever H. The Modified Hamilton Rating Scale for Depression: Reliability and validity. Psychiat Res. 1985;14(2):131–142. doi: 10.1016/0165-1781(85)90057-5. [DOI] [PubMed] [Google Scholar]
- Molnar G, Feeney M, Fava G. Duration and symptoms of bipolar prodromes. A J Psychiat. 1988;145(12):1576–1578. doi: 10.1176/ajp.145.12.1576. [DOI] [PubMed] [Google Scholar]
- Nusslock R, Abramson LY, Harmon-Jones E, Alloy LB, Hogan ME. A goal-striving life event and the onset of hypomanic and depressive episodes and symptoms: Perspective from the behavioral approach system (BAS) dysregulation theory. J Abnorm Psychol. 2007;116(1):105–115. doi: 10.1037/0021-843X.116.1.105. [DOI] [PubMed] [Google Scholar]
- Quoidbach J, Berry EV, Hansenne M, Mikolajczak M. Positive emotion regulation and well-being: Comparing the impact of eight savoring and Dampening strategies. Pers Indiv Differ. 2010;49(5):368–373. [Google Scholar]
- Raes F, Daems K, Feldman GC, Johnson SL, Van Gucht D. A psychometric evaluation of the Dutch version of the responses to positive affect questionnaire. Psychol Belg. 2010;49(4):293–310. [Google Scholar]
- Raes F, Smets J, Nelis S, Schoofs H. Dampening of positive affect prospectively predicts depressive symptoms in non-clinical samples. Cognition Emotion. 2012;26(1):75–82. doi: 10.1080/02699931.2011.555474. [DOI] [PubMed] [Google Scholar]
- Smith JA, Tarrier N. Prodromal symptoms in manic depressive psychosis. Soc Psych Psych Epid. 1992;27(5):245–248. doi: 10.1007/BF00788937. [DOI] [PubMed] [Google Scholar]
- Treynor W, Gonzalez R, Nolen-Hoeksema S. Rumination Reconsidered: A Psychometric Analysis. Cognitive Ther Res. 2003;27(3):247–59. [Google Scholar]
- Wood JV, Heimpel SA, Michela JL. Savoring versus Dampening: Self-esteem differences in regulating positive affect. J Pers Soc Psychol. 2003;85(3):566–580. doi: 10.1037/0022-3514.85.3.566. [DOI] [PubMed] [Google Scholar]