Abstract
BACKGROUND
Specific patterns of allergic sensitization as well as quantification of the in vitro IgE response in early life may provide relevant clinical insight into future rhinitis and asthma risk.
OBJECTIVE
To define relationships among established sensitization to particular aeroallergens, quantitative analyses of allergen-specific IgE levels, pet exposure and sensitization, and asthma and rhinitis risk.
METHODS
Children at high-risk for the development of asthma and allergic diseases were enrolled at birth into the Childhood Origins of ASThma (COAST) study. Allergen-specific IgE was assessed at ages 1, 3, 6, and 9 years by fluoroenzyme immunoassay (Unicap® 100, Pharmacia Diagnostics). Current asthma and rhinitis were diagnosed at age 6 and 8 years.
RESULTS
Sensitization to dog was strongly associated with increased asthma risk (p < 0.0001). Sensitization to perennial compared to seasonal allergens was more strongly associated with asthma risk, while sensitization to seasonal allergens was more closely associated with rhinitis risk. Increased levels of specific IgE to perennial allergens were associated with an increased asthma risk (p = 0.05), while any detectable level of IgE to seasonal allergens was associated with increased rhinitis risk (p = 0.0009). While dog and cat sensitization were both independently associated with increased asthma and rhinitis risk, dog exposure at birth was associated with a reduced risk of asthma, regardless of dog sensitization status during the first 6 years of life (p = 0.05).
CONCLUSIONS & CLINICAL RELEVANCE
Analyzing specific patterns of an individual’s allergic sensitization profile reveals additional relevant associations with asthma and rhinitis risk as opposed to the information gained from characterizing an individual as “atopic” by the presence of any demonstrable sensitization alone. Further, protective mechanisms of dog exposure with regards to asthma risk appear to be unrelated to the prevention of sensitization.
Keywords: asthma, rhinitis, children, IgE, allergic sensitization, pet exposure
INTRODUCTION
Atopy, defined as the genetic predisposition to develop specific IgE to common allergens, is widely accepted as a major risk factor for developing asthma later in life [1]. Recently, it has been suggested that viewing allergic sensitization as a simple dichotomous variable may be an oversimplification that fails to entirely capture its underlying associations with disease [2]. This redefined view of atopy suggests that multiple atopic phenotypes may differ greatly with regards to their relationship with asthma. As such, it may not simply be the presence or absence of allergic sensitization, but rather the specific pattern of the response (age at onset and development, as well as the type and number of specific allergens involved) that plays a role in the development of asthma [3].
Multiple studies have reported significant associations between sensitization to inhalant aeroallergens and asthma development [4-8], and Custovic and colleagues have additionally shown a quantitative relationship between specific serum IgE levels to common inhalant allergens and the presence and persistence of childhood wheezing and reduced lung function [2]. This concept has also been extended to the development of rhinitis in a study conducted by the same group, which suggested that progressively increasing specific IgE to grass pollen was associated with a significantly greater risk of current rhinitis at 5 years of age [9]. Similarly, other studies have reported that sensitization to specific seasonal allergens such as grass and birch pollen significantly increases the association with rhinitis risk [4, 10, 11].
With specific patterns of allergic sensitization being shown to have important implications in asthma and rhinitis risk, it is also logical to examine the effects of exposure to these allergens on the subsequent risk of developing asthma and rhinitis. A controversial topic regarding exposure and allergy is the impact of domestic pet exposure, which has led to conflicting recommendations concerning pet avoidance [12]. We have previously reported that dog exposure at birth was associated with a reduced risk of wheezing in the third year of life [13]. Two other birth cohort studies have observed similar findings [14, 15], yet others have not [16-19]. Additionally, findings assessing the influence of exposure to dog on the development of allergic rhinitis have been inconsistent [18, 19]. Interestingly, multiple birth cohort studies have reported that dog ownership seems to have a protective effect on the development of sensitization to mixed aeroallergens, especially mixed outdoor aeroallergens [15, 16, 18, 20]. With regards to cat exposure, the effect on asthma and rhinitis development is even less clear, as a majority of birth cohort studies have found no association between cat exposure in early life and the development of wheezing symptoms [12].
Based on these findings, we assessed the relationships between the development of asthma and rhinitis and the following characteristics of atopy: (1) the presence or absence of sensitization to specific aeroallergens, (2) the degree of aeroallergen sensitization by quantitative analysis of specific serum IgE antibody levels, and (3) patterns of pet exposure and sensitization.
METHODS
Study Population
289 newborns at high-risk for the development of asthma and allergic disease were recruited from November 1998 through May 2000 into the Childhood Origins of ASThma (COAST) study. Details of the study population and design have been described previously [21]. To qualify for the study, at least 1 parent was required to have respiratory allergies (defined as one or more positive aeroallergen skin tests) and/or a history of physician-diagnosed asthma. Of these children, 285 (98.6%) were followed prospectively for at least 1 year, 275 (95.2%) were followed through 3 years, 259 (90.9%) were followed through 6 years, and 238 were followed through 9 years (82.4%). Informed consent was obtained from the parents, and the Human Subjects Committee at the University of Wisconsin-Madison approved the study (IRB approval number H-2007-0044).
Measuring Allergen-Specific IgE
Peripheral blood samples were collected from the children annually. Allergen-specific IgE was measured in serum by fluoroenzyme immunoassay (FEIA) (UniCAP® 100, Pharmacia Diagnostics AB, Uppsala, Sweden) as previously described [22]. Serum concentrations of specific IgE antibodies for five common inhalant allergens (Dermatophagoides farinae, Dermatophagoides pteronyssinus, cat, dog, and Alternaria alternata) were determined at ages 1, 3, 6, and 9 years. Additionally, allergen-specific IgE to ragweed, silver birch, timothy grass and cockroach were measured at ages 6 and 9 years. The detection limit of the assay with regards to specific IgE was 0.35 kUA/L, and a positive test was defined as ≥0.35 kUA/L.
Clinical Definitions
Using a previously published clinical definition [23], current asthma was diagnosed at 6 and 8 years of age based on the documented presence of one or more of the following during the previous year: (1) physician diagnosis of asthma, (2) use of albuterol for coughing or wheezing episodes (prescribed by physician), (3) use of a daily controller medication, (4) use of a step-up plan including use of albuterol or short-term use of inhaled corticosteroids during illness, and (5) use of prednisone for asthma exacerbation. Rhinitis was defined as routinely or seasonally having frequent sneezes and/or itchy/runny nose, and was ascertained by parental report on historical questionnaires as reported previously [24]. The presence or absence of a dog or cat at home was determined by questionnaires on a yearly basis as previously described [13].
Statistical Analysis
Dichotomous outcomes of allergic sensitization were summarized using rates within the COAST cohort. Relationships between asthma, rhinitis, and allergic sensitization were evaluated using logistic regression models. These relationships were summarized using odds ratios (OR) with 95% confidence intervals (CI). To assess whether the level of specific IgE response beyond detectability was associated with asthma or rhinitis risk, generalized additive models (GAM) were fit with a covariate for detectability and a smooth term covariate for specific IgE quantity. Both asthma and rhinitis and their relationships with pet ownership and sensitization to pets were examined using multivariate logistic regression models with pet ownership and sensitization as covariates. For all statistical analyses, a two-sided p-value of < 0.05 was regarded as statistically significant.
RESULTS
Study Population
Of the 289 children originally enrolled in the COAST study, 259 were followed to at least 6 years of age and had aeroallergen specific IgE measured by FEIA at least once during this time period. At 6 years of age, 73 of 259 (28%) children had current asthma, 116 of 252 (46%) had current rhinitis, and 41 of 252 (16%) had both current asthma and rhinitis. There was no participation bias for obtaining in vitro IgE measurements at 6 years of age with regards to gender, older siblings, parental asthma or allergies, or current asthma at 6 years of age. There was a slightly higher rate of in vitro IgE measurements at 6 years of age in children with current rhinitis (p = 0.03).
Timing and Rates of Sensitization
An analysis of the incidence of IgE sensitization was completed to track the longitudinal trends of allergic sensitization to specific aeroallergens throughout early childhood (Table 1). The prevalence of aeroallergen sensitization rose from 13.5% at 1 year of age to 53% at 9 years of age (Table 1). Mono-sensitization was more common than poly-sensitization at age 1 year; however, at ages 3 years and beyond, poly-sensitization was far more common than mono-sensitization (Table 1).
TABLE 1.
Rates of allergic sensitization to specific aeroallergens throughout early childhood within the COAST cohort.
| Age 1 | Age 3 | Age 6 | Age 9 | |
|---|---|---|---|---|
| Any Aeroallergen | 34/252(13.5%) | 64/231 (27.7%) | 90/201 (44.8%) | 89/168 (53 0%) |
| Only 1 Aeroallergen | 23/252 (9.1%) | 27/231 (11.7%) | 20/201 (10.0%) | 26/168 (15 5%) |
| 2+ Aeroallergens | 11/252 (4 4%) | 37/231 (16 0%) | 70/201 (34.8%) | 63/168 (37 5%) |
| Cat | 15/256(5 9%) | 31/231 (13 4%) | 28/201 (13.9%) | 33/169(19 5%) |
| Dog | 14/252 (5.6%) | 26/231 (11.3%) | 35/202 (17.3%) | 40/169 (23 7%) |
| Dust Mite (DP) | 7/256 (2.7%) | 22/231 (9.5%) | 33/201 (16.4%) | 35/169 (20.7%) |
| Dust Mite (DF) | 6/256 (2.3%) | 16/231 (6.9%) | 35/201 (17.4%) | 34/169 (20 1%) |
| EITHER DM | 8/256 (3.1%) | 22/231 (9.5%) | 36/201 (17.9%) | 38/169 (22.5%) |
| A. Alternata | 6/256 (2.3%) | 29/231 (12.6%) | 52/201 (25.9%) | 54/169 (32.0%) |
| Cockroach | N/A | N/A | 10/201 (5.0%) | 9/169 (5.3%) |
| Ragweed | N/A | N/A | 36/201 (17.9%) | 39/169 (23.1%) |
| Silver Birch | N/A | N/A | 25/201 (12.4%) | 32/169 (18.9%) |
| Timothy Grass | N/A | N/A | 21/201 (10.4%) | 27/168 (16.1%) |
(DM = dust mite, DP = Dermatophagoides pteronyssinus, DF = Dermatophagoides farinae, A. alternata = Alternaria alternata)
Pets (dog and cat) were the most common allergens infants were sensitized to by age 1 year. Rates of sensitization to dog and cat steadily increased to age 9 years (Table 1). Sensitization rates for both species of dust mite showed similar upward trends as age increased: D. pteronyssinus had a sensitization rate of 2.7% at 1 year and increased to 20.7% by 9 years of age, while D. farinae had a sensitization rate of 2.3% at year 1 that increased to 20.1% by 9 years of age.
Of all tested allergens, sensitization to A. alternata showed the largest increase between 1 and 9 years of age. At 1 year, only 2.3% of children were sensitized, but this number grew dramatically to a prevalence rate of 25.9% by 6 years of age and 32% by 9 years of age. In contrast, cockroach sensitization was less common in the COAST cohort. Prevalence rates remained rather low at both 6 years (5%) and 9 years (5.3%). Of seasonal allergens, sensitization to ragweed was the most common, with a prevalence of 17.9% at 6 years of age and 23.1% at 9 years of age. Silver birch and timothy grass showed similar increases in prevalence from age 6 years to age 9 years (Table 1).
Associations between allergen-specific sensitization and asthma
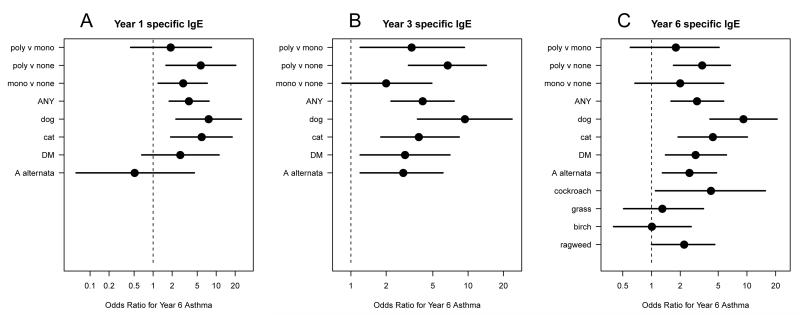
To investigate the relationships between allergen-specific sensitization and asthma development, we compared allergen-specific serum IgE concentrations at 1, 3, and 6 years with the presence of asthma at age 6 years (Fig. 1). Of all allergens tested, sensitization to dog consistently had the strongest association with asthma development. Allergen-specific IgE to dog and cat at 1 year were the only aeroallergens significantly associated with asthma risk [(dog: OR, 7.6; 95% CI, 2.3, 25.1), (cat: OR, 5.9; 95% CI, 1.9, 17.9)] (Fig. 1A). At 3 years of age, all perennial allergens tested were significantly associated with asthma at age 6 years, while dog sensitization (OR, 9.4; 95% CI, 3.7, 23.7) maintained the strongest association with future asthma risk, followed by cat (OR, 3.8; 95% CI, 1.8, 8.4), DM (OR, 2.9; 95% CI, 1.2, 7.0), and A. alternata (OR, 2.8; 95% CI, 1.2, 6.1) (Fig. 1B). Similarly, at 6 years of age, sensitization to any perennial allergen was significantly associated with concurrent asthma. The strongest association was sensitization to dog (OR, 9.2; 95% CI, 4.1, 20.7), followed by cat (OR, 4.4; 95% CI, 1.9, 10.1), cockroach (OR, 4.2; 95% CI, 1.1, 15.6), DM (OR, 2.9; 95% CI, 1.4, 6.1) and A. alternata (OR, 2.5; 95% CI, 1.3, 4.8) (Fig. 1C).
FIGURE 1A-C.
Relationships between allergen-specific sensitization at 1 (A), 3 (B), and 6 (C) years of age and asthma at 6 years of age. Dots represent the odds ratios (OR) and horizontal lines correspond to the 95% confidence intervals (CIs). (poly = poly-sensitization, mono = mono-sensitization, none = no sensitization, ANY = sensitization to any aeroallergen, DM = dust mite, A alternata = Alternaria alternata)
Relationships between pollen sensitization and asthma at age 6 were less consistent. Asthma was associated with sensitization to ragweed (OR, 2.2; 95% CI, 1.0, 4.6), but not silver birch or timothy grass (Fig. 1C). Poly-sensitization to aeroallergens was significantly associated with asthma when compared to absence of sensitization to allergens at age 1, 3, and 6 years [(OR, 5.7; 95% CI, 1.6, 20.4), (OR, 6.7; 95% CI, 3.1, 14.3), (OR, 3.4; 95% CI, 1.7, 6.7), respectively] (Fig. 1A-C). When poly-sensitization was compared directly with mono-sensitization with regards to asthma risk, the only statistically significant distinction between the two was observed at 3 years (OR, 3.3; 95% CI, 1.2, 9.3) (Fig. 1B). Similar relationships were seen between aeroallergen sensitization in early life and asthma at age 8 years (Supplementary Figure 1A-C).
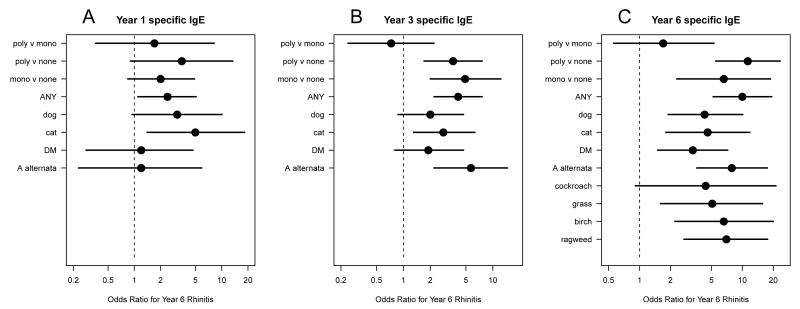
Associations between allergen-specific sensitization and rhinitis
We next evaluated relationships between allergen-specific sensitization and rhinitis at age 6 years (Fig. 2). At 1 year, sensitization to cat (OR, 5.0; 95% CI, 1.4, 18.3) was the only aeroallergen associated with an increased risk of rhinitis at age 6 years (Fig. 2A). By age 3 years, sensitization to both A. alternata (OR, 5.7; 95% CI, 2.2, 14.6) and cat (OR, 2.8; 95% CI, 1.3, 6.3) were associated with increased rhinitis risk (Fig. 2B). At age 6 years, sensitization to all allergens tested except cockroach was associated with concurrent rhinitis. Most notably, sensitization to A. alternata (OR, 7.9; 95% CI, 3.6, 17.5), ragweed (OR, 7.0; 95% CI, 2.7, 17.6), birch pollen (OR, 6.6; 95% CI, 2.2, 20.0), and timothy grass (OR, 5.1; 95% CI, 1.6, 15.7) had the strongest associations with rhinitis (Fig. 2C). These allergens were observed to have even stronger associations with rhinitis at 8 years of age, especially sensitization to birch pollen (OR, 26; 95% CI, 3.4, 197) (Supplementary Figure 2A-C)).
FIGURE 2A-CRelationships between allergen-specific sensitization at 1 (A), 3 (B), and 6 (C) years of age and rhinitis at 6 years of age. Dots represent the odds ratios (OR) and horizontal lines correspond to the 95% confidence intervals (CIs). (poly = poly-sensitization, mono = mono-sensitization, none = no sensitization, ANY = sensitization to any aeroallergen, DM = dust mite, A alternata = Alternaria alternata)
Poly-sensitization to aeroallergens was significantly associated with rhinitis when compared to absence of sensitization to allergens at age 3 and 6 years [(OR, 3.6; 95% CI, 1.7, 7.6 vs. OR, 11.3; 95% CI, 5.5, 23.3)] (Fig. 2B-C). However, no significant distinctions in associations with rhinitis were observed between children with poly-sensitization versus mono-sensitization at age 1, 3, or 6 years. (Fig. 2A-C).
Effect of degree of sensitization
We next sought to determine if the magnitude of allergen-specific IgE provides additional prognostic information beyond that provided by a positive response alone. In a generalized additive model for each allergen as a continuous variable, degree of sensitization at 1, 3, and 6 years was not associated with asthma or rhinitis prevalence at 6 years of age (data not shown).
Due to limited power to detect differences in the initial analysis, we next quantified the magnitude of an IgE response by grouping allergens into those with perennial (cat, dog, cockroach, A. alternata, D. pteronyssinus, D. farinae) and seasonal (ragweed, silver birch, timothy grass) patterns of exposure. The magnitude of a positive IgE response was separated into different levels of specific IgE concentration and compared with asthma and rhinitis at age 6. Greater levels of allergen specific IgE for perennial allergens at age 6 years were positively associated with concurrent asthma (Table 2). In contrast, greater levels of sensitization to seasonal allergens were not significantly associated with concurrent asthma (Table 2).
TABLE 2.
Relationships between the degree of sensitization to perennial and seasonal allergens at 6 years of age and asthma and rhinitis at 6 years of age.
| P-value |
||||||||
|---|---|---|---|---|---|---|---|---|
| Year 6 Perennial Allergens* (kUA/L) | n | asthma year 6 | vs 0 | vs 1 | vs 2 | vs 3 | vs 4 | |
| 0 | All IgE below detecdon | 121 | 17% | -- | -- | -- | -- | -- |
| 1 | All IgE < 1.7 but at least one IgE detectable | 18 | 44% | 0.01 | -- | -- | -- | -- |
| 2 | All IgE < 10 but at least one IgE ≥ 1.7 | 22 | 27% | 0.20 | 0.20 | -- | -- | -- |
| 3 | All IgE < 20 but at least one IgE ≥ 10 | 13 | 23% | 0.61 | 0.23 | 0.78 | -- | -- |
| 4 | All IgE < 50 but at least one IgE ≥ 20 | 10 | 50% | 0.005 | 0.75 | 0.16 | 0.15 | -- |
| 5 | At least one IgE ≥ 50 | 11 | 91% | 0.0003 | 0.03 | 0.004 | 0.005 | 0.05 |
|
| ||||||||
| P-value |
||||||||
| Year 6 Perennial Allergens* (kUA/L) | n | rhinitis year 6 | vs 0 | vs1 | vs 2 | vs 3 | vs 4 | |
|
| ||||||||
| 0 | All IgE below detection | 121 | 31% | -- | -- | -- | -- | -- |
| 1 | All IgE < 1.7 but at least one IgE detectable | 18 | 67% | 0.006 | -- | -- | -- | -- |
| 2 | All IgE < 1.7 but at least one IgE ≥ 1.7 | 22 | 68% | 0.002 | 0.02 | -- | -- | -- |
| 3 | All IgE < 20 but at least one IgE ≥ 10 | 13 | 100% | <0.0001 | 0.03 | 0.03 | -- | -- |
| 4 | All IgE < 50 but at least one IgE ≥ 20 | 16 | 81% | 0.0003 | 0.34 | 0 .37 | 0.23 | -- |
| 5 | At least one IgE ≥ 50 | 11 | 73% | 0.010 | 0.73 | 0.70 | 0.03 | 0.60 |
| P-value |
||||||
| Year 6 Seasonal Allergens** (kUA/L) | n | asthma year 6 | vs 0 | vs 1 | vs 2 | |
|
| ||||||
| 0 | All IgE below detection | 158 | 24% | -- | -- | -- |
| 1 | All IgE < 1.7 but at least one IgE detectable | 20 | 55% | 0.006 | -- | -- |
| 2 | All IgE < 10 but at least one IgE ≥ 1.7 | 14 | 29% | 0.71 | 0.13 | -- |
| 3 | At least one IgE ≥ 10 | 9 | 33% | 0.53 | 0.29 | 0.81 |
|
| ||||||
| P-value |
||||||
|
| ||||||
| Year 6 Seasonal Allergens** (kUA/L) | n | rhinitis year 6 | vs 0 | vs1 | vs 2 | |
| 0 | All IgE below detection | 158 | 40% | -- | -- | -- |
| 1 | All IgE < 1.7 but at least one IgE detectable | 20 | 85% | 0.0009 | -- | -- |
| 2 | All IgE < 10 but at least one IgE ≥ 1.7 | 14 | 79% | 0.01 | 0.03 | -- |
| 3 | At least one IgE ≥ 10 | 9 | 89% | 0.02 | 0.78 | 0.53 |
cat, dog, cockroach, Dermatophagoides farinae, Dermatophagoides pteronyssinus, Alternaria alternata
ragweed, silver birch, timothy grass)
Any level of sensitization to seasonal allergens was associated with concurrent rhinitis, while higher levels of perennial allergen-specific IgE were needed before a significant positive association with concurrent rhinitis was observed (Table 2).
Pet sensitization/exposure and asthma/rhinitis outcome at 6 years
We have previously reported within the COAST cohort that dog exposure at birth was associated with a reduced risk of wheezing and a reduced cumulative prevalence of atopic dermatitis in the third year of life [13]. Due to this finding, as well as observing strong associations between dog and cat sensitization during early life and subsequent asthma risk, we next compared relationships between pet exposure at birth and pet sensitization at any point during the first 6 years of life with asthma and rhinitis prevalence at 6 years of age (Table 3).
TABLE 3.
Relationships between pet exposure at birth and pet sensitization at any point during the first 6 years of life with asthma and rhinitis prevalence at 6 years of age.
| P-value | |||||
|---|---|---|---|---|---|
| dog in home at birth |
sensitized to dog, first 6 years of life |
n | asthma year 6 |
dog in home |
sensitization to dog |
| No | No | 134 | 24% | ||
| Yes | No | 78 | 15% | 0.05 † | <0.0001 * |
| No | Yes | 33 | 70% | ||
| Yes | Yes | 13 | 46% | ||
| P-value | |||||
| dog in home at birth |
sensitized to dog, first 6 years of life |
n | rhinitis year 6 |
dog in home |
sensitization to dog |
|
| |||||
| No | No | 131 | 47% | ||
| Yes | No | 76 | 29% | 0.03 ‡ | 0.0003 ** |
| No | Yes | 33 | 70% | ||
| Yes | Yes | 13 | 77% | ||
| P-value | |||||
| cat in home at birth |
sensitized to cat, first 6 years of life |
n | asthma year 6 | cat in home | sensitization to cat |
|
| |||||
| No | No | 153 | 23% | ||
| Yes | No | 59 | 20% | 0.64 | <0.0001* |
| No | Yes | 30 | 57% | ||
| Yes | Yes | 17 | 53% | ||
| P-value | |||||
| cat in home at birth |
sensitized to cat, first 6 years of life |
n | rhinitis year 6 |
cat in home | sensitization to cat |
|
| |||||
| No | No | 149 | 41% | ||
| Yes | No | 57 | 39% | 0.73 | 0.0003** |
| No | Yes | 31 | 71% | ||
| Yes | Yes | 16 | 69% | ||
Associated with increased asthma
associated with decreased asthma
associated with increased rhinitis
associated with decreased rhinitis
Sensitization to dog during the first 6 years of life was independently associated with increased asthma risk, regardless of whether there was a dog in the home at birth or not [dog present: (46% vs. 15%), dog absent: (70% vs. 24%); (p<0.0001, Table 3)]. Interestingly, dog exposure at birth was associated with a reduced risk of asthma, regardless of dog sensitization during the first 6 years of life. Sensitization to dog at any point during the first 6 years of life was also independently associated with increased rhinitis risk, regardless of a dog being present or absent at birth (p=0.0003, Table 3). Dog exposure at birth was associated with a reduced risk of rhinitis in children who did not become sensitized to dog during the first 6 years of life, but was not associated with reduced rhinitis risk in children who did become sensitized to dog (p=0.03, Table 3).
Sensitization to cat during the first 6 years of life was also independently associated with increased asthma risk, regardless of whether a cat was present in the home at birth or not [cat present: (53% vs. 20%), cat absent: (57% vs. 23%); (p<0.0001, Table 3)]. In contrast to dog ownership, cat exposure at birth was not associated with a significantly reduced risk of asthma. Rhinitis risk was significantly increased with sensitization to cat, regardless of a cat being present or absent at birth [cat present: (69% vs. 39%), cat absent: (71% vs. 41%); (p=0.0003, Table 3)]. Cat exposure at birth did not alter asthma or rhinitis risk.
DISCUSSION
In this prospective birth cohort study, we have conducted three sets of analyses that examine the relationships among allergen sensitization and exposure and asthma and rhinitis outcomes at 6 and 8 years of age. These analyses include the presence or absence of sensitization to particular aeroallergens, the quantitative degree of allergic sensitization, and early life pet exposure. By analyzing patterns of allergen-specific sensitization, we have demonstrated that sensitization to specific aeroallergens differentially impacts subsequent asthma and rhinitis risk. Specifically, sensitization to perennial allergens, to dog in particular, was associated with the highest asthma risk. Furthermore, poly-sensitization at all ages was greatly associated with an increased asthma risk. For rhinitis, seasonal allergens were more closely associated with increased risk. These findings suggest that sensitization to perennial allergens is more closely linked to asthma development, while sensitization to seasonal allergens is more strongly associated with rhinitis development, potentially implicating differential mechanisms regarding both the process of sensitization and the pattern of disease expression in the upper and lower airways. A larger study population and inclusion of a wider panel of allergens may provide further insight into differential effects of specific allergens on asthma and rhinitis risk.
Our data analyzing the magnitude of allergen-specific IgE antibody formation demonstrate that increased levels of specific IgE to perennial allergens was associated with an increased asthma risk, while any detectable level of IgE to seasonal allergens was associated with increased rhinitis risk. These results confirm previous observations that absolute specific IgE antibody levels offer additional information in relation to asthma risk compared to the presence or absence of specific IgE alone [2, 3]. However, we have extended these findings by identifying two separate groups of aeroallergens (perennial and seasonal) that display different associations between the magnitude of their absolute specific IgE levels and the risk of asthma and rhinitis development. Previous results generated by Custovic and colleagues reported that when using specific IgE levels at 5 years of age as a continuous variable, the risk of current wheeze increased significantly with increasing specific IgE to mite, cat, and dog [2]. This risk was the greatest when the levels of specific IgE to mite, cat, and dog were summed. We have extended these associations by clearly showing that an increase in the magnitude of the IgE response to perennial aeroallergens is linked with not only current wheeze, but also asthma. Additionally, the same group reported that when using specific IgE as a continuous variable, the risk of current rhinitis at 5 years of age increased significantly with increasing specific IgE to grass pollen [9]. Though our results are congruent with the fact that high levels of specific IgE to seasonal allergens are associated with an increased rhinitis risk, they contrast this finding by showing that rhinitis risk seems to increase significantly upon reaching the threshold of any detectable specific IgE to seasonal allergens.
Within the COAST cohort, dog and cat sensitization during the first 6 years of life were both independently associated with increased asthma and rhinitis risk, regardless of the respective exposure at birth. Additionally, dog exposure at birth was associated with a reduced risk of asthma, regardless of sensitization status to dog during the first 6 years of life. However, no such relationship was observed with cat exposure at birth. The association of dog exposure and reduced asthma risk, even in children who later become sensitized to dog, is intriguing and suggests that protective mechanisms of dog exposure are unrelated to the prevention of sensitization. Recent work has suggested that dogs may enrich the microbial communities of homes in ways that could influence the developmental pattern of innate immune responses [25]. Defining potential mechanisms underlying these observations is of interest for future study.
The strengths of this study include the prospective design, the high retention rate (90.9%) through age 6 years, and a diverse panel of specific aeroallergens tested at multiple time points in development. One limitation of the COAST study is that the study participants all have a parental history of atopy or asthma. It has been suggested that dog exposure is associated with stronger protective effects in children with atopic parents due to selective dog avoidance [26], though this is controversial [14]. Additionally, the COAST cohort is comprised of a relatively restricted population in regard to demographics such as ethnicity and socioeconomic status. It is possible that the results described may differ in other populations based upon effects of different allergen exposure frequencies and varying practices such as pet keeping that may impact patterns of sensitization [27-31].
In conclusion, our data suggest that increased levels of specific IgE to perennial allergens during early life are associated with an increased asthma risk at school age, while any detectable level of IgE to seasonal allergens is associated with increased rhinitis risk. These observational findings raise the question: why do increasing levels of allergen-specific IgE lead to greater asthma risk, and why is that outcome potentially different from rhinitis in terms of the target organ response? Additional studies are needed to resolve and understand the underlying immunological and physiological mechanisms behind these associations. Our findings, which expand the dichotomous phenotypic characteristic of “atopy” by examining specific patterns of an individual’s allergic sensitization response, could have potential ramifications in clinical practice by allowing clinicians to discern additional relevant associations with asthma and rhinitis risk as opposed to relying on the limited information gained from characterizing an individual as “atopic” by the presence or absence of demonstrable sensitization alone. Clinicians can obtain this additional information by quantifying allergic sensitization, as well as evaluating the type and number of specific allergens involved.
SUPPLEMENTARY FIGURE 1A-C. Relationships between allergen-specific sensitization at 1 (A), 3 (B), and 6 (C) years of age and asthma at 8 years of age. Dots represent the odds ratios (OR) and horizontal lines correspond to the 95% confidence intervals (CIs). (poly = poly-sensitization, mono = mono-sensitization, none = no sensitization, ANY = sensitization to any aeroallergen, DM = dust mite, A alternata = Alternaria alternata)
SUPPLEMENTARY FIGURE 2A-C. Relationships between allergen-specific sensitization at 1 (A), 3 (B), and 6 (C) years of age and rhinitis at 8 years of age. Dots represent the odds ratios (OR) and horizontal lines correspond to the 95% confidence intervals (CIs). (poly = poly-sensitization, mono = mono-sensitization, none = no sensitization, ANY = sensitization to any aeroallergen, DM = dust mite, A alternata = Alternaria alternata)
Supplementary Material
SUPPLEMENTARY FIGURE 1A-C. Relationships between allergen-specific sensitization at 1 (A), 3 (B), and 6 (C) years of age and asthma at 8 years of age. Dots represent the odds ratios (OR) and horizontal lines correspond to the 95% confidence intervals (CIs). (poly = poly-sensitization, mono = mono-sensitization, none = no sensitization, ANY = sensitization to any aeroallergen, DM = dust mite, A alternata = Alternaria alternata)
SUPPLEMENTARY FIGURE 2A-C. Relationships between allergen-specific sensitization at 1 (A), 3 (B), and 6 (C) years of age and rhinitis at 8 years of age. Dots represent the odds ratios (OR) and horizontal lines correspond to the 95% confidence intervals (CIs). (poly = poly-sensitization, mono = mono-sensitization, none = no sensitization, ANY = sensitization to any aeroallergen, DM = dust mite, A alternata = Alternaria alternata)
Acknowledgments
Funding:
Supported, National Institutes of Health (NIH) and by National Institutes of Health grants R01 HL61879, P01 HL70831, T32 AI007635, M01 RR03186, and by the Clinical and Translational Science Award (CTSA) program previously through the National Center for Research Resources (NCRR) grant UL1RR025011, and now by the National Center for Advancing Translational Sciences (NCATS), grant UL1TR000427.
Abbreviations
- COAST
Childhood Origins of ASThma, immunoglobulin E (IgE)
- FEIA
fluoroenzyme immunoassay
- DM
dust mite
- D. farinae
Dermatophagoides farinae
- D. pteronyssinus
Dermatophagoides pteronyssinus
- A. alternata
Alternaria alternata
- OR
odds ratio
- 95% CI
95% confidence interval
Footnotes
Conflict of Interest Statement:
D.J.S. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. D.J.J. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. M.D.E. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. R.E.G. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. C.J.T. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. J.E.G. was an investigator on research grants to the University of Wisconsin from GlaxoSmithKline and Astra Zeneca, and was a consultant to Boehringer Ingelheim. R.F.L. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript.
References
- 1.Sly PD, Boner AL, Björksten B, Bush A, Custovic A, Eigenmann PA, Gern JE, Gerritsen J, Hamelmann E, Helms PJ, Lemanske RF, Martinez F, Pedersen S, Renz H, Sampson H, von Mutius E, Wahn U, Holt PG. Early identification of atopy in the prediction of persistent asthma in children. Lancet. 2008;372:1100–6. doi: 10.1016/S0140-6736(08)61451-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Simpson A, Soderstrom L, Ahlstedt S, Murray CS, Woodcock A, Custovic A. IgE antibody quantification and the probability of wheeze in preschool children. J Allergy Clin Immunol. 2005;116:744–9. doi: 10.1016/j.jaci.2005.06.032. [DOI] [PubMed] [Google Scholar]
- 3.Simpson A, Tan VY, Winn J, Svensén M, Bishop CM, Heckerman DE, Buchan I, Custovic A. Beyond atopy: multiple patterns of sensitization in relation to asthma in a birth cohort study. Am J Respir Crit Care Med. 2010;181:1200–6. doi: 10.1164/rccm.200907-1101OC. [DOI] [PubMed] [Google Scholar]
- 4.Brockow I, Zutavern A, Hoffmann U, Grübl A, von Berg A, Koletzko S, Filipiak B, Bauer CP, Wichmann HE, Reinhardt D, Berdel D, Krämer U, Heinrich J, Group GS. Early allergic sensitizations and their relevance to atopic diseases in children aged 6 years: results of the GINI study. J Investig Allergol Clin Immunol. 2009;19:180–7. [PubMed] [Google Scholar]
- 5.Sporik R, Holgate ST, Platts-Mills TA, Cogswell JJ. Exposure to house-dust mite allergen (Der p I) and the development of asthma in childhood. A prospective study. N Engl J Med. 1990;323:502–7. doi: 10.1056/NEJM199008233230802. [DOI] [PubMed] [Google Scholar]
- 6.Gaffin JM, Phipatanakul W. The role of indoor allergens in the development of asthma. Curr Opin Allergy Clin Immunol. 2009;9:128–35. doi: 10.1097/aci.0b013e32832678b0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Illi S, von Mutius E, Lau S, Niggemann B, Grüber C, Wahn U, group MASM. Perennial allergen sensitisation early in life and chronic asthma in children: a birth cohort study. Lancet. 2006;368:763–70. doi: 10.1016/S0140-6736(06)69286-6. [DOI] [PubMed] [Google Scholar]
- 8.Kusel MM, de Klerk NH, Kebadze T, Vohma V, Holt PG, Johnston SL, Sly PD. Early-life respiratory viral infections, atopic sensitization, and risk of subsequent development of persistent asthma. J Allergy Clin Immunol. 2007;119:1105–10. doi: 10.1016/j.jaci.2006.12.669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marinho S, Simpson A, Söderström L, Woodcock A, Ahlstedt S, Custovic A. Quantification of atopy and the probability of rhinitis in preschool children: a population-based birth cohort study. Allergy. 2007;62:1379–86. doi: 10.1111/j.1398-9995.2007.01502.x. [DOI] [PubMed] [Google Scholar]
- 10.Ghunaim N, Wickman M, Almqvist C, Söderström L, Ahlstedt S, van Hage M. Sensitization to different pollens and allergic disease in 4-year-old Swedish children. Clin Exp Allergy. 2006;36:722–7. doi: 10.1111/j.1365-2222.2006.02489.x. [DOI] [PubMed] [Google Scholar]
- 11.Arshad SH, Tariq SM, Matthews S, Hakim E. Sensitization to common allergens and its association with allergic disorders at age 4 years: a whole population birth cohort study. Pediatrics. 2001;108:E33. doi: 10.1542/peds.108.2.e33. [DOI] [PubMed] [Google Scholar]
- 12.Chen CM, Tischer C, Schnappinger M, Heinrich J. The role of cats and dogs in asthma and allergy--a systematic review. Int J Hyg Environ Health. 2010;213:1–31. doi: 10.1016/j.ijheh.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 13.Bufford JD, Reardon CL, Li Z, Roberg KA, DaSilva D, Eggleston PA, Liu AH, Milton D, Alwis U, Gangnon R, Lemanske RF, Gern JE. Effects of dog ownership in early childhood on immune development and atopic diseases. Clin Exp Allergy. 2008;38:1635–43. doi: 10.1111/j.1365-2222.2008.03018.x. [DOI] [PubMed] [Google Scholar]
- 14.Remes ST, Castro-Rodriguez JA, Holberg CJ, Martinez FD, Wright AL. Dog exposure in infancy decreases the subsequent risk of frequent wheeze but not of atopy. J Allergy Clin Immunol. 2001;108:509–15. doi: 10.1067/mai.2001.117797. [DOI] [PubMed] [Google Scholar]
- 15.Sandin A, Björkstén B, Bråbäck L. Development of atopy and wheezing symptoms in relation to heredity and early pet keeping in a Swedish birth cohort. Pediatr Allergy Immunol. 2004;15:316–22. doi: 10.1111/j.1399-3038.2004.00166.x. [DOI] [PubMed] [Google Scholar]
- 16.Almqvist C, Egmar AC, Hedlin G, Lundqvist M, Nordvall SL, Pershagen G, Svartengren M, van Hage-Hamsten M, Wickman M. Direct and indirect exposure to pets - risk of sensitization and asthma at 4 years in a birth cohort. Clin Exp Allergy. 2003;33:1190–7. doi: 10.1046/j.1365-2222.2003.01764.x. [DOI] [PubMed] [Google Scholar]
- 17.Brussee JE, Smit HA, van Strien RT, Corver K, Kerkhof M, Wijga AH, Aalberse RC, Postma D, Gerritsen J, Grobbee DE, de Jongste JC, Brunekreef B. Allergen exposure in infancy and the development of sensitization, wheeze, and asthma at 4 years. J Allergy Clin Immunol. 2005;115:946–52. doi: 10.1016/j.jaci.2005.02.035. [DOI] [PubMed] [Google Scholar]
- 18.Chen CM, Morgenstern V, Bischof W, Herbarth O, Borte M, Behrendt H, Krämer U, von Berg A, Berdel D, Bauer CP, Koletzko S, Wichmann HE, Heinrich J. Group IoLRFotHISaDoAiCLS, Group GINIPGS, Dog ownership and contact during childhood and later allergy development. Eur Respir J. 2008;31:963–73. doi: 10.1183/09031936.00092807. [DOI] [PubMed] [Google Scholar]
- 19.Nafstad P, Magnus P, Gaarder PI, Jaakkola JJ. Exposure to pets and atopy-related diseases in the first 4 years of life. Allergy. 2001;56:307–12. doi: 10.1034/j.1398-9995.2001.00881.x. [DOI] [PubMed] [Google Scholar]
- 20.Ownby DR, Johnson CC, Peterson EL. Exposure to dogs and cats in the first year of life and risk of allergic sensitization at 6 to 7 years of age. JAMA. 2002;288:963–72. doi: 10.1001/jama.288.8.963. [DOI] [PubMed] [Google Scholar]
- 21.Lemanske RF. The childhood origins of asthma (COAST) study. Pediatr Allergy Immunol. 2002;13(Suppl 15):38–43. doi: 10.1034/j.1399-3038.13.s.15.8.x. [DOI] [PubMed] [Google Scholar]
- 22.Neaville WA, Tisler C, Bhattacharya A, Anklam K, Gilbertson-White S, Hamilton R, Adler K, Dasilva DF, Roberg KA, Carlson-Dakes KT, Anderson E, Yoshihara D, Gangnon R, Mikus LD, Rosenthal LA, Gern JE, Lemanske RF. Developmental cytokine response profiles and the clinical and immunologic expression of atopy during the first year of life. J Allergy Clin Immunol. 2003;112:740–6. doi: 10.1016/s0091-6749(03)01868-2. [DOI] [PubMed] [Google Scholar]
- 23.Jackson DJ, Gangnon RE, Evans MD, Roberg KA, Anderson EL, Pappas TE, Printz MC, Lee WM, Shult PA, Reisdorf E, Carlson-Dakes KT, Salazar LP, DaSilva DF, Tisler CJ, Gern JE, Lemanske RF. Wheezing rhinovirus illnesses in early life predict asthma development in high-risk children. Am J Respir Crit Care Med. 2008;178:667–72. doi: 10.1164/rccm.200802-309OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jackson DJ, Virnig CM, Gangnon RE, Evans MD, Roberg KA, Anderson EL, Burton RM, Salazar LP, DaSilva DF, Shanovich KM, Tisler CJ, Gern JE, Lemanske RF. Fractional exhaled nitric oxide measurements are most closely associated with allergic sensitization in school-age children. J Allergy Clin Immunol. 2009;124:949–53. doi: 10.1016/j.jaci.2009.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fujimura KE, Johnson CC, Ownby DR, Cox MJ, Brodie EL, Havstad SL, Zoratti EM, Woodcroft KJ, Bobbitt KR, Wegienka G, Boushey HA, Lynch SV. Man's best friend? The effect of pet ownership on house dust microbial communities. J Allergy Clin Immunol. 2010;126:410–2. doi: 10.1016/j.jaci.2010.05.042. 12. e1-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hölscher B, Frye C, Wichmann HE, Heinrich J. Exposure to pets and allergies in children. Pediatr Allergy Immunol. 2002;13:334–41. doi: 10.1034/j.1399-3038.2002.02063.x. [DOI] [PubMed] [Google Scholar]
- 27.Eggleston PA, Rosenstreich D, Lynn H, Gergen P, Baker D, Kattan M, Mortimer KM, Mitchell H, Ownby D, Slavin R, Malveaux F. Relationship of indoor allergen exposure to skin test sensitivity in inner-city children with asthma. J Allergy Clin Immunol. 1998;102:563–70. doi: 10.1016/s0091-6749(98)70272-6. [DOI] [PubMed] [Google Scholar]
- 28.Huss K, Adkinson NF, Eggleston PA, Dawson C, Van Natta ML, Hamilton RG. House dust mite and cockroach exposure are strong risk factors for positive allergy skin test responses in the Childhood Asthma Management Program. J Allergy Clin Immunol. 2001;107:48–54. doi: 10.1067/mai.2001.111146. [DOI] [PubMed] [Google Scholar]
- 29.Matsui EC, Wood RA, Rand C, Kanchanaraksa S, Swartz L, Curtin-Brosnan J, Eggleston PA. Cockroach allergen exposure and sensitization in suburban middle-class children with asthma. J Allergy Clin Immunol. 2003;112:87–92. doi: 10.1067/mai.2003.1588. [DOI] [PubMed] [Google Scholar]
- 30.Matsui EC, Wood RA, Rand C, Kanchanaraksa S, Swartz L, Eggleston PA. Mouse allergen exposure and mouse skin test sensitivity in suburban, middle-class children with asthma. J Allergy Clin Immunol. 2004;113:910–5. doi: 10.1016/j.jaci.2004.02.034. [DOI] [PubMed] [Google Scholar]
- 31.Chew GL, Perzanowski MS, Canfield SM, Goldstein IF, Mellins RB, Hoepner LA, Ashby-Thompson M, Jacobson JS. Cockroach allergen levels and associations with cockroach-specific IgE. J Allergy Clin Immunol. 2008;121:240–5. doi: 10.1016/j.jaci.2007.08.024. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
SUPPLEMENTARY FIGURE 1A-C. Relationships between allergen-specific sensitization at 1 (A), 3 (B), and 6 (C) years of age and asthma at 8 years of age. Dots represent the odds ratios (OR) and horizontal lines correspond to the 95% confidence intervals (CIs). (poly = poly-sensitization, mono = mono-sensitization, none = no sensitization, ANY = sensitization to any aeroallergen, DM = dust mite, A alternata = Alternaria alternata)
SUPPLEMENTARY FIGURE 2A-C. Relationships between allergen-specific sensitization at 1 (A), 3 (B), and 6 (C) years of age and rhinitis at 8 years of age. Dots represent the odds ratios (OR) and horizontal lines correspond to the 95% confidence intervals (CIs). (poly = poly-sensitization, mono = mono-sensitization, none = no sensitization, ANY = sensitization to any aeroallergen, DM = dust mite, A alternata = Alternaria alternata)