Abstract
Hydrocele of the canal of Nuck (cyst of the canal of Nuck) is the female homologue of hydrocele of the spermatic cord in males and is a rarely encountered entity, mostly diagnosed on the operating table at the time of suspected inguinal hernia surgery, as the clinical presentation usually is subtle and inconclusive. Diagnosis is mainly by ultrasound and has shown varied presentation of the same over the years. We discuss the sonographic findings of a case of hydrocele of the canal of Nuck.
Keywords: Hydrocele, Canal of Nuck, Sonography, Cyst
CASE REPORT
A 35 year old female presented to the surgical outpatient department with complaints of painful swelling in her right groin for a period of two weeks. Swelling was sudden in onset and the patient reported a slight increase in the size of the swelling since its occurrence. There was no history of vomiting, bowel and bladder dysfunction. On examination an oval, approximately 4×3 cm in size, tender, cystic and fluctuant swelling was present in the region of the right inguinal canal. Transillumination test was negative. Swelling was irreducible against manual pressure. There was no expansible cough impulse, peristaltic activity or abnormal vascularity associated with the swelling. Signs of inflammation were absent. Lymphnodal examination was normal.
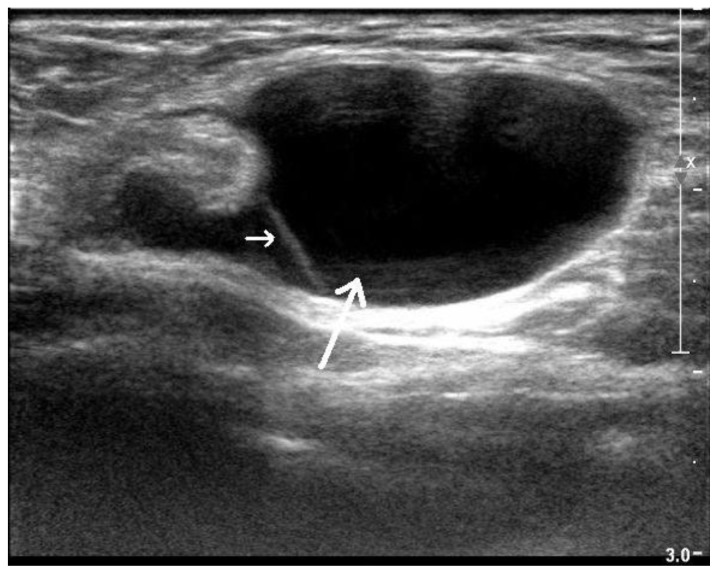
Sonographic examination, using high frequency linear transducer (5 to 17MHz), in longitudinal and transverse planes revealed a well defined, oval, anechoic cystic swelling within the inguinal canal measuring 4.3 × 2.6 cm, with a cranially directed tail measuring 1.6 × 0.7 cm (FIG. 1, FIG. 2), deep to the external oblique fascia. The cyst showed thickened echogenic wall with single septation. Color Doppler showed an avascular cystic structure (FIG. 3). The patient underwent right herniotomy with excision of the hernial sac under general anesthesia. The inguinal region was explored similar to a hernia excision. Fascia was separated and external oblique was opened. Round ligament was identified along with the hydrocele of the canal of Nuck. Hydrocele was separated from the round ligament and excision of the hydrocele was carried out. Hernia was ruled out, external oblique muscle layer and fascia were closed and abdomen sealed. Post-operative period was uneventful and patient recovered satisfactorily. Pathologic examination confirmed our suspicion of Hydrocoele of canal of Nuck. On follow up, once after fifteen days and second after two months, the patient did not report of any symptoms. Thereafter the patient was lost to follow up.
Figure 1.
35 year old female diagnosed with right sided hydrocele of the canal of Nuck. Transverse ultrasonographic image using high frequency linear transducer (L17-5MHz), showing anechoic cystic structure measuring 4.3 × 2.6 cms in size (long arrow) in the right inguinal canal with a septa within (short arrow).
Figure 2.
35 year old female diagnosed with right sided hydrocele of the canal of Nuck. Longitudinal ultrasonographic image using high frequency linear transducer (L17-5MHz) showing patent and partially compressed canal of Nuck (arrow) with an anechoic cystic structure measuring 4.3 × 2.6 cms in size.
Figure 3.
35 year old female diagnosed with right sided hydrocele of the canal of Nuck. Transverse colour Doppler ultrasonographic image using high frequency linear transducer (L17-5MHz) showing an avascular, anechoic cystic structure measuring 4.3 × 2.6 cms in size in the right inguinal canal.
DISCUSSION
Owing to its rarity and the unawareness among clinicians, due to the lack of literature in surgical and gynecological textbooks, Hydrocele of the canal of Nuck is a seldom encountered entity in clinical practice and is commonly mistaken for inguinal hernia as one third of the cases of the former are concomitantly present with the latter [1, 2, 3]. Hydrocele of canal of Nuck is an important differential diagnosis for an irreducible hernia in female patients. Clinically these hydroceles may mimic both inguinal and femoral hernia, and may even strangulate. They can also be mistaken for Bartholin’s cyst of labium majus, which is more common. If infected, it can present as an abscess or tender adenopathy. Although mostly reported in children population, its presence in adults has been documented [4, 5]. Other possible differential diagnoses include lymphadenopathy, bartholin’s cyst, abscess, arterial and venous aneurysms and malignant and benign tumors [1].
In females the evagination of the parietal peritoneum along with the round ligament through the inguinal ring into the inguinal canal forms the canal of Nuck, by 6 months of gestation, which is the female counterpart of processus vaginalis in males [6]. Complete obliteration of the canal of Nuck usually occurs by the first year of life [7]. However, partial patency with peritoneal communication, allowing only fluid collection, may result in hydrocele of the canal of Nuck [1, 6, 7]. Hydrocele of the canal of Nuck is the result of fluid collection within the processus vaginalis counterpart in females either due to physiological seepage of intraperitoneal fluid or hypersecretion or underabsorption in the lining epithelium of the distal segment. Various etiologies in support include idiopathic nature, inflammation, trauma, impairment of lymphatic drainage, endometriosis and rarely as a complication of ventriculoperitoneal shunt and meconium hydrocele [1, 8, 9]. Patent processus vaginalis can either contain fluid, omentum or bowel if it is communicating with the peritoneal cavity or else it can only have fluid or form a loculated cyst in the form of hydrocele of canal of Nuck.
Clinically, hydrocele of the canal of Nuck may present as a painless, translucent, fluctuating, nonreducible swelling in the inguinal area and labium majus [1, 6, 7, 10, 11]. However the overlying external oblique fascia may hinder transillumination in some cases. Cysts are usually small measuring about 3 cm in length and 0.3–0.5 cm in diameter, however, giant hydrocele of canal of Nuck is also reported [2, 12].
The importance of high resolution real time sonography in the diagnosis of hydrocele of canal of Nuck has been mentioned in previous literatures and thus serves as a successful, efficient, accurate and the principal diagnostic modality for differentiating hydrocele of the canal of Nuck from other entities [1, 7, 13]. Several authors have documented varied ultrasound and MR [magnetic resonance] findings for the same. Sonographic appearance of hydrocele of the canal of Nuck shows a thin walled, well defined, hypo echoic or echo free, cystic structure which may vary from an anechoic, tubular, sausage, dumbbell or comma-shaped, “cyst within a cyst” appearance to a multicystic hydrocele [1, 6, 7, 13, 14, 15]. Inguinal or Femoral hernias, on the other hand, mostly have a hyper echoic component protruding out of the hernial orifice into the sac (omentum or intestine) and vary with valsalva manoeuvre. The colour Doppler does not show any vascularity in cases of hydrocoele of canal of Nuck. Data reporting MRI [magnetic resonance imaging] features is still scarce as it is considered to be less superior and cost ineffective as compared to ultrasound [7, 10]. On MRI, the hydrocele appears as a simple cyst characterized as hypointense on T1-weighted images and hyperintense on T2-weighted images [5]. General consensus on the treatment proposes surgical excision of the hydrocele and ligation of the neck of processus vaginalis at the deep ring (FIG. 4, FIG. 5). Aspiration of the cyst can be performed in patients refusing to undergo surgery, however in such cases recurrence is a possibility.
Figure 4.
35 year old female diagnosed with right sided hydrocele of the canal of Nuck. This intra operative image shows the hydrocele being held up by the surgeon.
Figure 5.
35 year old female diagnosed with right sided hydrocele of the canal of Nuck. This intra operative image shows the hydrocele of the canal of Nuck separated from the round ligament.
TEACHING POINT
Although rarely reported, hydrocele of the canal of Nuck should be taken into consideration while listing the differentials for groin swelling in a female. Radiologists should be aware of the sonographic findings of hydrocele of the canal of Nuck to diagnose this entity with precision preoperatively.
Table 1.
Summary table for hydrocele of the Canal of Nuck
| Etiology | Complete or partially patent Processus vaginalis; Imbalance in absorption and secretion of the lining epithelium. |
| Incidence | Unknown. Only 400 cases reported so far. |
| Gender Ratio | Confined to female population. |
| Age Predilection | Mostly in children. Adult cases have been documented. |
| Risk Factors | Idiopathic, Inflammatory, Trauma, Lymphatic blockage, Endometriosis, Complication of ventriculoperitoneal shunt, Meconium hydrocele |
| Treatment | Surgical excision and ligation of the neck of processus vaginalis at the deep ring. |
| Prognosis | Good |
| Findings on imaging |
High resolution sonography: Thin walled, well defined, echo free, cystic structure varying from an anechoic, tubular, sausage, dumbbell or comma-shaped, “cyst within a cyst” to a multicystic appearance. MRI: Thin-walled cystic mass in inguinal area. |
Table 2.
Differential diagnosis table for hydrocele of the Canal of Nuck
| Sonography | MRI | Color Doppler | |
|---|---|---|---|
| Hydrocele of the Canal of Nuck | Thin walled, well defined, hypo echoic or anechoic, single or multicystic structure with or without septations. | Thin-walled cystic mass, hypointense on T1-weighted and hyperintense on T2-weighted images. No enhancement seen. | No vascularity observed |
| Inguinal/Femoral Hernia | Solid, mostly hyper echoic component protruding out of the hernial orifice into the sac (omentum or intestine). Shows response to valsalva and augmentation. | ||
| Saphena varix | Sac-like collection forming part of a column of blood extending to the femoral vein down the leg which lls from below. Best demonstrated on colour Doppler. | ||
| Lymphomas | Hypoechoic mass | Abundant vascularity | |
| Psoas abscess | Irregular hypo echoic wall and echogenic debris or gas bubbles | ||
| Inguinal lymph node | Solid to cystic mass (if necrosis present) Usually multiple |
Solid to cystic mass Hypointense on T1W and hyperintense on T2W sequences Usually multiple |
Internal vascularity present |
ABBREVIATIONS
- MR
Magnetic Resonance
- MRI
Magnetic Resonance Imaging
REFERENCES
- 1.Stickel WH, Manner M. Female hydrocele (cyst of the canal of Nuck). Sonographic appearance of a rare and little-known disorder. J Ultrasound Med. 2004;23:429–432. doi: 10.7863/jum.2004.23.3.429. [DOI] [PubMed] [Google Scholar]
- 2.Block RE. Hydrocele of the canal of Nuck: a report of five cases. Obstet Gynecol. 1975;45:464–466. [PubMed] [Google Scholar]
- 3.Schneider CA, Festa S, Spillert CR, Bruce CJ, Lazaro EJ. Hydrocele of the canal of Nuck. NJ Med. 1994;91:37–38. [PubMed] [Google Scholar]
- 4.Wei BPC, Castles L, Stewart KA. Hydroceles of the canal of Nuck. A N Z J Surg. 2002;72:603–606. doi: 10.1046/j.1445-2197.2002.02466.x. [DOI] [PubMed] [Google Scholar]
- 5.Safak AA, Erdogmus B, Yazici B, Gokgoz AT. Hydrocele of the canal of Nuck: sonographic and MRI appearances. J Clin Ultrasound. 2007;35(9):531–2. doi: 10.1002/jcu.20329. [DOI] [PubMed] [Google Scholar]
- 6.Anderson CC, Broadie TA, Mackey JE, Kopecky KK. Hydrocele of the canal Nuck: ultrasound appearance. Am Surg. 1995;61:959. [PubMed] [Google Scholar]
- 7.Park SJ, Lee HK, Hong HS, et al. Hydrocele of the canal of Nuck in a girl: ultrasound and MR appearance. Br J Radiol. 2004;77:243–244. doi: 10.1259/bjr/51474597. [DOI] [PubMed] [Google Scholar]
- 8.Sharma S, Gangopadhyay AN. Meconium hydrocele presenting as a labial mass. Indian Pediatr. 2005;42:1060–1062. [PubMed] [Google Scholar]
- 9.Yuksel KZ, Senoglu M, Yuksel M, Ozkan KU. Hydrocele of the canal of Nuck as a result of a rare ventriculoperitoneal shunt complication. Pediatr Neurosurg. 2006;42:193–196. doi: 10.1159/000091867. [DOI] [PubMed] [Google Scholar]
- 10.Yigit H, Tuncbilek I, Fitoz S, Yigit N, Kosar U, Karabulut B. Cyst of the canal of Nuck with demonstration of the proximal canal. The role of the compression technique in sonographic diagnosis. J Ultrasound Med. 2006;25:123–125. doi: 10.7863/jum.2006.25.1.123. [DOI] [PubMed] [Google Scholar]
- 11.Collins S, Ortenberg J, Collins S. Hydrocoele and hernia in children. 2002. [Accessed May 18, 2011.]. Available at: http://www.emedicine.com/ped/topic1037.htm.
- 12.Dawam D, Kanu P. Giant hydrocele of the canal of Nuck. Br J Urol. 1998;81(4):636. doi: 10.1046/j.1464-410x.1998.00406.x. [DOI] [PubMed] [Google Scholar]
- 13.Miklos JR, Karram MM, Silver E, Reid R. Ultrasound and hookwire needle placement for localization of a hydrocele of the canal of Nuck. Obstet Gynecol. 1995;85:884. doi: 10.1016/0029-7844(94)00439-k. [DOI] [PubMed] [Google Scholar]
- 14.Chandrasekharan LV, Rajagopal AS. The hydrocele of the canal of Nuck: an ultrasound diagnosis. [Accessed May 18, 2011];Internet J Pathol. 2006 4(2) Available at: http://www.ispub.com/ostia/index.php?xmlFilePath=journals/ijra/vol4n2/Nuck.xml. [Google Scholar]
- 15.Khanna PC, Ponsky T, Zagol B, Lukish JR, Markle BM. Sonographic appearance of canal of Nuck hydrocele. Pediatr Radiol. 2007;37:603–606. doi: 10.1007/s00247-007-0481-6. [DOI] [PubMed] [Google Scholar]