Abstract
Esophageal lipomas are rare tumors, making up 0.4% of all digestive tract benign neoplasms. Most of these lesions are clinically silent as a result of their small size, however, the majority of lesions over 4 cm have been reported to cause dysphagia, regurgitation and/or epigastralgia. We report a case of a 53 year-old African American female who presented with dysphagia. Computed tomography of the chest and esophagram confirmed esophageal lipoma as the cause of the patient’s symptoms. Accurately diagnosing an esophageal lipoma is crucial in order to rule out potential malignant lesions, relieve patient symptoms and plan the appropriate treatment.
Keywords: Esophageal Lipoma, Esophagus
CASE REPORT
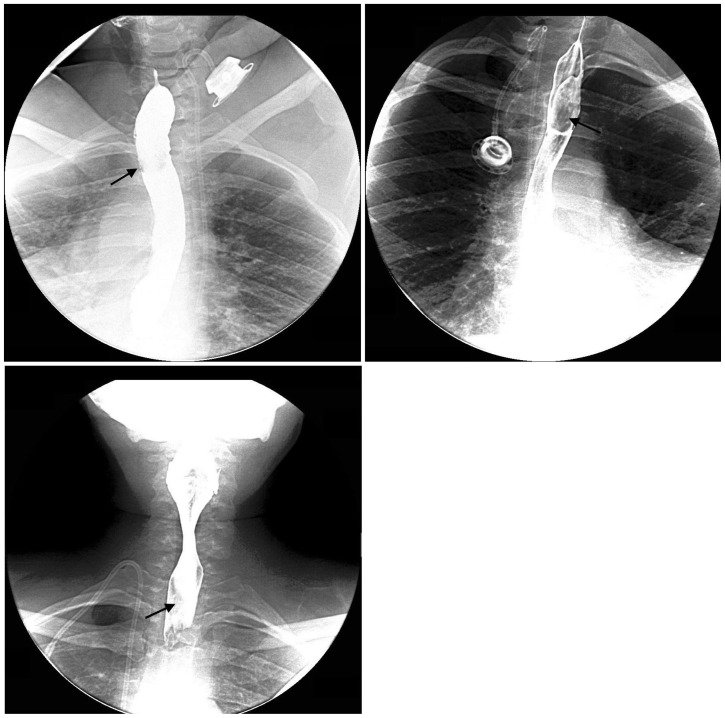
A 53 year-old African American female with Human T-lymphotropic virus Type 1 (Adult T-Cell Leukemia/Lymphoma) presented for an esophagram with a diagnosis of dysphagia. Findings were significant for an upper esophageal submucosal lesion with luminal narrowing (Figure 1). There was no evidence of a “squeeze sign”. The etiology of the filling defect was unclear at this time. Intermittent mild tertiary spasm also likely contributed to the dysphagia.
Figure 1.
53-year-old African American female with dysphagia who presented for a double contrast esophagram was found to have an esophageal lipoma. Upper left image: Left posterior oblique image demonstrates an esophageal submucosal lesion extending from T1–T3, resulting in a filling defect (black arrow). Upper right image: Prone oblique image illustrates that the submucosal lesion in the esophagus has smooth borders (black arrow). A right internal jugular infusion catheter terminates at the junction of the superior vena cava and right atrium. Lower left image: Frontal image further shows the luminal narrowing caused by the esophageal lipoma (black arrow). (Protocol: Double contrast esophagram with thick barium and effervescent granules).
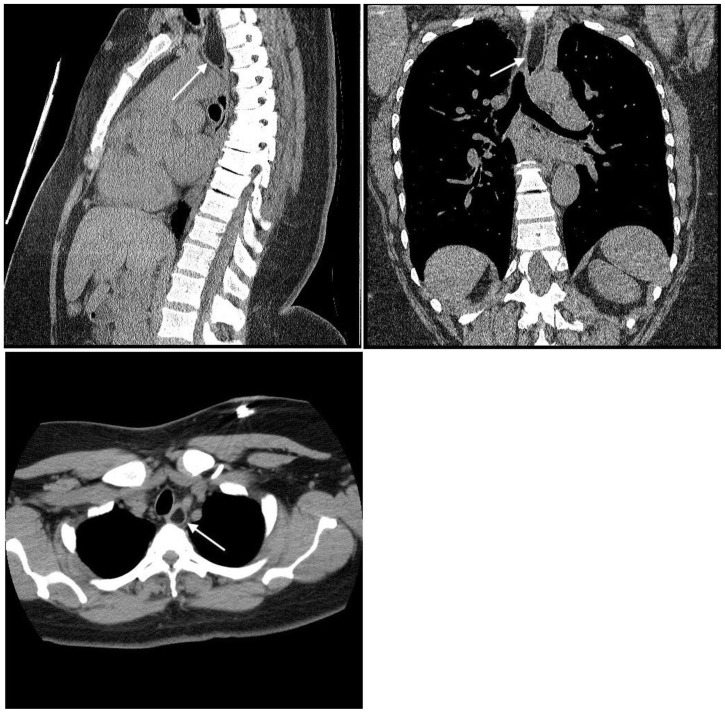
Subsequently, the patient had a CT (computed tomography) of the chest. The study was originally scheduled to evaluate a left lower lung pulmonary nodule prior to the findings discovered on the esophagram, which also warranted additional evaluation with a CT of the chest. The examination showed a hypoattenuating, 4.5 × 1.4 × 1.2 cm submucosal mass in the posterior wall of the upper thoracic esophagus, with Hounsfield units ranging between -90 and -110 (Figure 2). The mass, with imaging characteristics consistent with a lipoma, corresponded to the lesion seen on the prior esophagram. The esophageal mass remained unchanged on three subsequent thoracic CT scans over a course of three years that were performed for further follow-up of the pulmonary nodule. The patient has declined endoscopy and surgical excision of the lesion.
Figure 2.
53 year old African American female presents for evaluation of a left lower lobe pulmonary nodule was found to have an esophageal lipoma. Upper left image: Sagittal non-enhanced CT of the chest demonstrates a submucosal, hypoattenuating lesion with fat density in the thoracic esophagus (white arrow), consistent with an esophageal lipoma. Upper right image: Coronal non-enhanced CT of the chest illustrates the thoracic esophageal lipoma (white arrow). Lower left image: Axial non- enhanced CT of the chest further depicts the esophageal lipoma (white arrow). (Protocol: 64 slice CT scanner, mAs:300, kVp: 120, 5mm slice thickness).
DISCUSSION
Benign esophageal tumors are rare, representing less than 1% of all esophageal neoplasms. In decreasing order of occurrence, lesions that have been found in the esophagus include leiomyomas, fibrovascular polyps, squamous papillomas, granular cell tumors, lipomas, neurofibromas, and inflammatory fibroid polyps. Additional especially rare benign esophageal tumors include hemangiomas and hamartomas [1, 2]. These masses are usually discovered incidentally, as many of them are small and asymptomatic.
Lipomas of the alimentary tract are uncommon, making up 4.1% of all benign tumors. More specifically, lipomas of the esophagus are extremely rare, accounting for only 0.4% of all digestive tract benign neoplasms [3, 4]. They generally become symptomatic only when they are large enough to cause dysphagia, at which time they merit surgical excision [5].
The exact etiology of lipomas is uncertain, however, one theory suggests an association between previous trauma and subsequent lipoma formation [6]. Lipomas are found in all areas of the GI (Gastrointestinal) tract, most commonly in the colon, followed by the small intestine. Less common locations include the stomach and esophagus. Lipomas throughout the GI tract have an incidence of 1 in 600 necropsies [4]. Fewer than 20 surgical cases of esophageal lipomas have been reported in the literature [5].
The likelihood of a lipoma causing symptoms is related to its size. According to Hurwitz et al., no GI tract lipoma under 1 cm caused symptoms, compared with (75%) over 4 cm [7]. 85% of Lipomas in the esophagus are clinically silent, therefore the majority of them are found incidentally on radiographic imaging [8]. If symptomatic, patients can experience dysphagia, regurgitation, recurrent melena and/or epigastralgia [7, 9]. The most frequent complaint is dysphagia.
In general, gastrointestinal lipomas are more common in females, however, esophageal lipomas are more common in men than women with a reported ratio of 27:13 [8, 10]. Esophageal lipomas have been reported in patients between the ages of 4 and 80 years old, with a mean age of 50 [4, 5]. Usually esophageal lipomas originate in the cervical and upper thoracic esophagus [5].
Establishing a correct diagnosis of an esophageal lipoma demands a careful history, thorough radiographic examination and/or inspection with upper GI endoscopy. Radiographically, lipomas present as intraluminal filling defects. Useful signs to differentiate lipomas from other benign or malignant lesions include a smooth surface and “squeeze” sign manifested by changes in contour and configuration as a result of peristalsis [7]. Presentation of a lipoma on upper GI endoscopy is a lesion of yellow color, pliability and a smooth surface. Malignant lesions tend to be friable and irregular, with an ulcerated surface [5].
Leiomyomas, the most common benign esophageal tumor, has subtle differences from that of a lipoma. Radiologically they appear as a well-defined mass with muscle density and occasionally contain nodular calcifications. This translates to a hypoattenuating lesion on CT, a hypoechoic lesion with fine echoes, in the setting of calcifications, on endoscopic ultrasound and a tan mass on upper GI endoscopy [11, 12]. Of particular importance, a liposarcoma, another very rare lesion, should not be confused with a lipoma. There are multiple histologic subtypes of liposarcomas that can range from yellow to a gray-tan color. They appear heterogeneous with areas of increased echogenicity, corresponding to areas of fat, on endoscopic ultrasound [13, 14, 15]. On CT, a liposarcoma is heterogeneous, contains septa and tissue other than fat, as compared to a lipoma, which presents as a homogenous lesion with fat density [4, 5]. Therefore, a homogenous lesion containing fat density on CT is diagnostic of a lipoma [4, 16, 17]. Esophageal lipomas appear as smooth and well-defined hyperechoic lesions on endoscopic ultrasound [11, 17]. On MRI, lipomas can be identified by following fat signal as T1-weighted hyperintensity that becomes hypointense on fat-suppressed images [18]. On the contrary, liposarcomas appear heterogeneous with high signal intensity on T1 and T2 weighted images and leiomyomas are iso intense on T2 -weighted images [12, 19]. Historically, these three lesion types have been evaluated by esophagram, but because all of these lesions present as discrete masses causing filling defects, further evaluation is necessary for definitive diagnosis.
Most esophageal lipomas are small, solitary, are asymptomatic and do not require treatment. Large symptomatic lipomas, however, require surgical resection. The different surgical options include a mini-thoractomy, cervical thoracotomy, endoscopy and videothoracoscopy [5]. In conclusion, careful diagnosis of an esophageal lipoma is necessary to exclude other potential malignant lesions and relieve patient symptomatology.
TEACHING POINT
Lipomas of the esophagus are rare and are usually discovered incidentally unless they are large enough to cause symptoms, most commonly dysphagia. Diagnosis of an esophageal lipoma can be safely accomplished using computed tomography, presenting as a homogeneous lesion with fat density.
Table 1.
Summary table for esophageal lipoma
| Etiology | Exact etiology remains uncertain. One theory suggests a possible link between trauma and lipoma formation |
| Incidence | Extremely Rare; make up 0.4% of all digestive tract benign neoplasms |
| Gender Ratio | Male:Female 27:13 |
| Age predilection | Between 4 and 80 years old |
| Risk factors | N/A |
| Treatment | Small lesions: None Large, symptomatic lesions: Surgical resection |
| Prognosis | Benign Tumor |
| Findings on Imaging |
CT: Homogenous lesions with fat density Upper GI Endoscopy: Lesion of yellow color, pliability and a smooth surface Esophagram: Discrete mass Endoscopic Ultrasound: Well-defined hyperechoic mass MRI: T1-weighted hyperintensity that becomes hypointense on fat-suppressed images |
Table 2.
Differential table for esophageal lipoma
| Lipoma | Liposarcoma | Leiomyoma | |
|---|---|---|---|
| CT | Homogenous lesion with fat density | Heterogenous, contains septa and tissue other than fat | Smooth mass with muscle attenuation +/− calcification |
| Upper GI endoscopy | Lesion of yellow color, pliable and with a smooth surface. | Polypoid mass that is yellow to gray-tan color | Firm, round and tan lesion |
| Esophagram | Discrete mass that invades the lumen | Discrete mass that invades the lumen | Discrete mass +/− calcifications that invades the lumen |
| Endoscopic Ultrasound | Well-defined hyperechoic mass | Heterogeneous with areas of increased echogenicity | Well-defined hypoechoic mass with evenly spaced fine echoes |
| MRI | T1-weighted hyperintensity that becomes hypointense on fat-suppressed images | Heterogeneous with high signal intensity on T1 and T2 weighted images | Iso intense on T2 – weighted images |
ABBREVIATIONS
- CT
Computed Tomography
- GI
Gastrointestinal
- MRI
Magnetic Resonance Imaging
REFERENCES
- 1.Xu GQ, Hu FL, Chen LH. The value of endoscopic ultrasonography on diagnosis and treatment of esophageal hamartoma. J Zhejiang Univ Sci B. 2008 Aug;9(8:):662–6. doi: 10.1631/jzus.B0820049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Toinaga K, Arakawa T, Ando K, et al. Oesophageal cavernous haemangioma diagnosed histologically, not by endoscopic procedures. J Gastroenterol Hepatol. 2000 Feb;15(2:):215–9. doi: 10.1046/j.1440-1746.2000.02042.x. [DOI] [PubMed] [Google Scholar]
- 3.Mayo CW, Pagtalunan RJ, Brown DJ. Lipoma of the alimentary tract. Surgery. 1963 May;53:598–603. [PubMed] [Google Scholar]
- 4.Kang JY, Chan-Wilde C, Wee A, Chew R, Ti TK. Role of computed tomography and endoscopy in the management of alimentary tract lipomas. Gut. 1990 May;31(5:):550–3. doi: 10.1136/gut.31.5.550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang CY, Hsu HS, Wu YC, Huang MH, Hsu WH. Intramural lipoma of the esophagus. J Chin Med Assoc. 2005 May;68(5:):240–3. doi: 10.1016/S1726-4901(09)70216-3. [DOI] [PubMed] [Google Scholar]
- 6.Nickloes TA. Lipomas. Emedicine. 2010. [Accessed January 21, 2012]. Available at: http://emedicine.medscape.com/article/191233-overview#a0102.
- 7.Hurwitz MM, Redleaf PD, Williams HJ, Edwards JE. Lipomas of the gastrointestinal tract. An analysis of seventy-two tumors. Am J Roentgenol Radium Ther Nucl Med. 1967 Jan;99(1):84–9. [PubMed] [Google Scholar]
- 8.Taylor AJ, Stewart ET, Dodds WJ. Gastrointestinal lipomas: a radiologic and pathologic review. AJR Am J Roentgenol. 1990 Dec;155(6:):1205–10. doi: 10.2214/ajr.155.6.2122666. [DOI] [PubMed] [Google Scholar]
- 9.Zschiedrich M, Neuhaus P. Pedunculated giant lipoma of the esophagus. Am J Gastroenterol. 1990 Dec;85(12:):1614–6. [PubMed] [Google Scholar]
- 10.Takubo Kaiyo. Pathology of the esophagus: an atlas and text book. 2nd edition. Hong Kong: Springer; 2009. Benign non-epithelial tumors and tumor- like conditions of the esophagus; p. 134. [Google Scholar]
- 11.Murata Y, Yoshida M, Akimto S, Ide H, Suzuki S, Hanyu F. Evaluation of endoscopic ultrasonography for the diagnosis of submucosal tumors of the esophagus. Surg Endosc. 1988;2(2):51–8. doi: 10.1007/BF00704350. [DOI] [PubMed] [Google Scholar]
- 12.Yang PS, Lee KS, Lee SJ, et al. Esophageal leiomyoma: radiologic findings in 12 patients. Korean J Radiol. 2001 Jul-Sep;2(3):132–137. doi: 10.3348/kjr.2001.2.3.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ruppert-Kohlmayr AJ, Raith J, Friedrich G, et al. Giant liposarcoma of the esophagus: radiological findings. J Thorac Imaging. 1999 Oct;14(4:):316–9. doi: 10.1097/00005382-199910000-00015. [DOI] [PubMed] [Google Scholar]
- 14.Temes R, Quinn P, Davis M, et al. Endoscopic resection of esophageal liposarcoma. J Thorac Cardiovasc Surg. 1998 Aug;116(2:):365–7. doi: 10.1016/s0022-5223(98)70144-8. [DOI] [PubMed] [Google Scholar]
- 15.Xu S, Xu Z, Hou Y, Tan Y. Primary pedunculated giant esophageal liposarcoma: case report. Dysphagia. 2008 Sep;23(3:):327–30. doi: 10.1007/s00455-007-9130-3. [DOI] [PubMed] [Google Scholar]
- 16.Heiken JP, Forde KA, Gold RP. Computed tomography as a definitive method for diagnosing gastrointestinal lipomas. Radiology. 1982 Feb;142(2:):409–14. doi: 10.1148/radiology.142.2.7054830. [DOI] [PubMed] [Google Scholar]
- 17.Thompson WM. Imaging and findings of lipomas of the gastrointestinal tract. AJR Am J Roentgenol. 2005 Apr;184(4:):1163–71. doi: 10.2214/ajr.184.4.01841163. [DOI] [PubMed] [Google Scholar]
- 18.Borges A, Bikhazi H, Wensel JP. Giant fibrovascular polyp of the oropharynx. AJNR Am J Neuroradiol. 1999 Nov-Dec;20(10):1979–82. [PMC free article] [PubMed] [Google Scholar]
- 19.Yang B, Shi PZ, Li X, Xu RJ. Well-differentiated liposarcoma of esophagus. Chin Med J (Engl) 2006 Mar 5;119(5):438–40. [PubMed] [Google Scholar]