Abstract
Ureteral polyps are rare causes of ureteropelvic junction (UPJ) obstruction, particularly in children. We report a nine year-old boy with UPJ obstruction initially suggestive of an obstructive urinary stone. CT showed intraureteral calcification at the UPJ and hydronephrosis. A retrograde pyelogram showed narrowing at the UPJ and partial obstruction that was found to be a ureteral polyp. This case illustrates a rare cause of UPJ obstruction that should be considered when the imaging findings and presentation are atypical for more common etiologies of ureteral obstruction.
Keywords: pediatric, fibroepithelial polyp, ureteral polyp, ureteropelvic junction obstruction
CASE REPORT
A nine year-old boy with a prenatal history of stable, grade 2 left hydronephrosis presented to the emergency department with nausea, vomiting, and 10/10 left flank pain that awoke him from sleep. A urinalysis in the emergency department showed microscopic hematuria. A non-contrast CT of his abdomen and pelvis was done during his pain episode and showed left ureteropelvic junction (UPJ) obstruction with calcification at the UPJ (Fig. 1, 2). His pain spontaneously resolved after several hours. The next day, a subsequent renal ultrasound showed grade 3–4 left hydroureteronephrosis without shadowing and an area of hypervascularity suggestive of a mass in the proximal ureter (Fig. 3). A MAG3 Lasix renogram was consistent with left kidney obstruction, with a half-time clearance of 5.5 minutes on the right and 19.2 minutes on the left (Fig. 4).
Figure 1.
9 year-old boy with ureteropelvic junction obstruction found to be caused by a 2cm ureteral polyp. A transverse, non-contrast CT scan shows a calcified ureteral polyp (arrow in A) in the patient’s left ureter, causing proximal obstruction of the renal pelvis (arrows in B). Non-contrast CT of the abdomen and pelvis was obtained on a GE LightSpeed VCT at mA=109–139 with automatic current modulation, kvp=120 and reconstructed into 5 mm thick axial images.
Figure 2.
9 year-old boy with a ureteropelvic junction obstruction found to be caused by a 2cm ureteral polyp. A coronal, non-contrast CT scan shows a ureteral polyp with calcification (arrow) in the patient’s left ureter, causing proximal obstruction of the renal pelvis and hydronephrosis. Non-contrast CT of the abdomen and pelvis was obtained on a GE LightSpeed VCT at mA=109–139 with automatic current modulation, kvp=120 and reconstructed into 5 mm thick coronal images.
Figure 3.
9 year-old boy with ureteropelvic junction obstruction found to be caused by a 2cm ureteral polyp. A) Grayscale renal ultrasound shows grade III hydronephrosis. B) Renal Doppler ultrasound shows blood flow in the kidney, proximal urinary obstruction, and the obstructing hypervascular mass (arrow). Doppler image obtained with a curved transducer at 5 MHz on an Acuson imaging system.
Figure 4.
9 year-old boy with a ureteropelvic junction obstruction found to be caused by a 2cm ureteral polyp. MAG3 lasix renogram shows decreased function in the left kidney is compatible with urinary obstruction.
The patient was scheduled for a retrograde pyelogram to better delineate his anatomy, with plans for a pyeloplasty if a UPJ obstruction was confirmed. The retrograde pyelogram showed irregularity and stenosis of the left proximal ureter, prompting a decision to operate (Fig. 5). At surgery, the ureter appeared grossly normal but upon opening the proximal ureter, a single 2 cm intraluminal, polypoid mass was found (Fig. 6). This mass was excised and a pyeloplasty was performed. Pathology confirmed a fibroepithelial polyp (Fig. 7).
Figure 5.
9 year-old boy with ureteropelvic junction obstruction found to be caused by a 2 cm ureteral polyp. A retrograde pyelogram of the left proximal ureter showed irregularity and stenosis (arrows) but did not reveal a clear etiology for the obstruction. Spot fluoroscopic image was obtained at 69 kVp and 2.12 mA after the retrograde injection of non-ionic water-soluble contrast material.
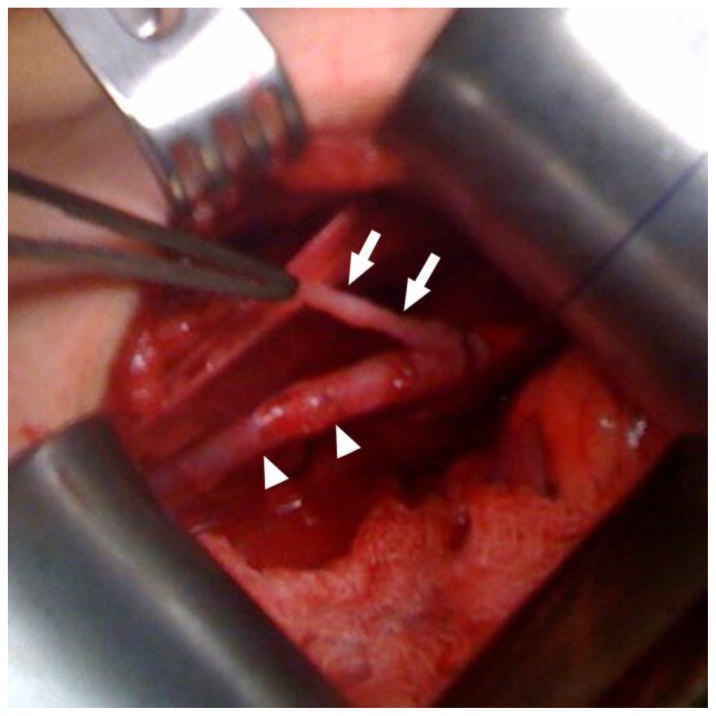
Figure 6.
9 year-old boy with ureteropelvic junction obstruction found to be caused by a ureteral polyp. Intraoperative photo shows the ureter (arrow heads) and 2cm long stalk of the polyp (arrows)
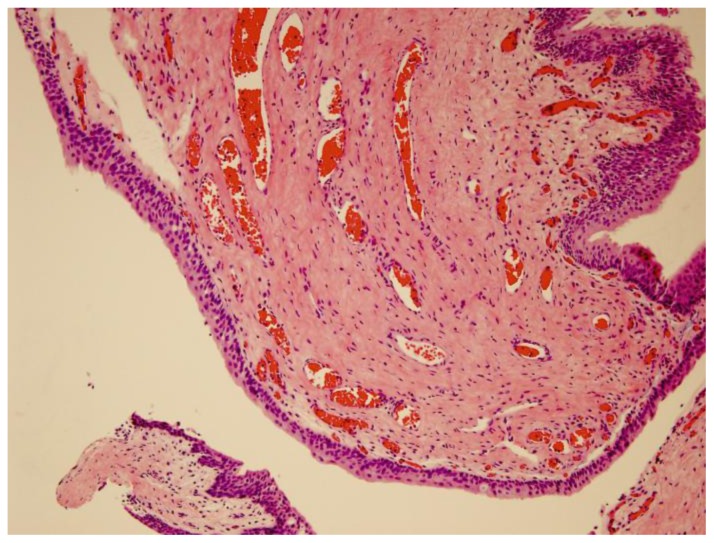
Figure 7.
9 year-old boy with ureteropelvic junction obstruction found to be a ureteral polp. The image is at 200× magnification with a hematoxylin and eosin stain. Pathology showed a fibroepithelial polyp demonstrating a thin, bland urothelial cell lining over a polypoid fibrovascular stroma with frequent dilated and congested small blood vessels
The patient had a follow-up sonogram performed after six weeks after surgery, with planned yearly follow-up thereafter. He is currently doing well without evidence of recurrence based on monitoring for pain and hydronephrosis.
DISCUSSION
Ureteral fibroepithelial polyps are a rare cause of ureteropelvic junction obstructions in children and are found in only 0.5% of children undergoing pyeloplasty [1]. They are benign growths of mesodermal origin that consist of a fibrovascular core covered by normal urothelium and are most commonly found in the upper third of the ureter (Fig. 8). The exact tendency of distribution of these polyps along the ureter remains unclear, but in one case series of 15 children who presented with ureteral fibroepithelial polyps, all of them had polyps located in the upper ureter [2]. Their typical clinical presentation is abdominal or flank pain with or without hematuria. Surgical resection usually results in cure and recurrence is rare. They present more often in boys than in girls, with several case series reporting 80–90% of polyps occurring in boys [1–3]. These polyps also occur more frequently on the left side, though bilateral polyps have been reported [3–5].
Etiologies of UPJ obstruction are divided into primary and secondary obstruction. Primary UPJ obstruction is further subdivided into intrinsic causes-including narrowing of the UPJ from disrupted development of circular musculature and extracellular matrix of the ureter, valvular mucosal folds, persistent fetal convolutions, and ureteral polyps-and extrinsic causes, particularly a crossing lower pole vessel. Secondary obstruction is most commonly caused by stone disease and also by severe vesicoureteral reflux causing tortuosity that leads to kinking of the ureter and subsequent obstruction. Of these etiologies, the most common causes of UPJ obstruction are a congenitally narrowed UPJ, crossing lower pole vessels, and urinary stones (Fig. 9) [6]. Cancerous etiologies of UPJ obstruction are unlikely in children. In particular, transitional cell carcinoma of the ureter may be found in adults but is rare in children.
Ureteral polyps are the most common benign tumors of the ureter, yet one of the rarest causes of UPJ obstruction. Typically, children present with abdominal or flank pain with or without hematuria, along with other nonspecific symptoms, including nausea and vomiting [2]. These children are often diagnosed after a gastrointestinal workup and may have evidence of hydronephrosis on ultrasound. A MAG3 Lasix renogram will quantify the degree of obstruction and renal function.
The treatment for obstructing ureteral polyps at the UPJ remains the open Anderson-Hynes dismembered pyeloplasty, though other techniques described include laparoscopic or robotic pyeloplasty, ureteroscopic resection, and holmium laser resection [7,5].
Radiographic diagnosis is crucial to surgical management. Polyps may be imaged by CT, ultrasound, magnetic resonance urography, excretory urography, and retrograde pyelogram [8,2]. A retrograde pyelogram is preferred for diagnosing ureteral polyps because of its ability to delineate intraluminal lesions. Magnetic resonance urography is also excellent for the tissue contrast it gives and its ability to visualize intraluminal lesions without radiation, which is particularly important in children. However, both modalities can be time consuming and require anesthesia for young patients. CT may show soft tissue filling the UPJ and proximal ureter, and 3D reformations may better reveal their structure and increase diagnostic confidence [2]. Ultrasound may show evidence of hydronephrosis or hydroureter, though dilation is typically mild, or a mildly echogenic structure with a polypoid projection without acoustic shadow. Retrograde pyelogram or excretory urography shows an intraluminal lesion that is smooth or polypoid without marked dilation of the urinary tract [8,6].
In contrast, other causes of UPJ obstruction may show other distinguishing features. In the situation of a crossing lower pole vessel, ultrasound may show evidence of hydronephrosis, as with a polyp. However, CT will show a vessel crossing the ureter at the point of obstruction, and a retrograde pyelogram will lead to visualization of the proximal ureter with an abrupt cut-off. In the case of a stone, ultrasound may show shadowing of the ultrasound beam. On CT, there is often perinephric stranding and radiodense material (the stone) seen, and on retrograde pyelogram, there is typically a filling defect with radiodense material (stone) at the point of urinary obstruction.
Even with appropriate imaging studies, ureteral fibroepithelial polyps remain notoriously difficult to diagnose pre-operatively. In two case series, two of nine patients and zero of fourteen were identified pre-operatively [1,7]. Likewise, the cause of this patient’s UPJ obstruction was not identified until surgical intervention despite several imaging modalities.
This case is interesting because the diagnosis of ureteral polyp was not initially suspected based on pre-operative imaging, and in fact, stone disease was considered because of areas of calcification found on CT. However, the findings on ultrasound indicated a possible noncalculous etiology such as a polyp or other mass. In retrospect, this area of calcification likely represented a small stone behind the obstructing polyp that the patient ultimately passed. It may also have been microcalcification within the polyp, though there was no calcification seen on histology. And though polyps are not typically seen on ultrasonography, this case illustrates the importance of carefully examining Doppler ultrasound imaging for evidence of vascular flow, which can help guide the physician toward a preoperative diagnosis of a ureteral polyp. Though polyps are a rare entity, it is important to consider a ureteral polyp as a cause of UPJ obstruction when building a differential diagnosis.
TEACHING POINT
Ureteral polyps are a rare cause of ureteropelvic junction obstruction in children that should be considered when working up a child with abdominal pain or hematuria. They are difficult to diagnose pre-operatively and therefore require a high index of clinical suspicion and close examination of the patient’s imaging for clues to this etiology.
Table 1.
Summary table for a ureteral polyp in children
| Etiology |
|
| Incidence | True incidence is unknown but estimated to be 0.5% of children undergoing pyeloplasty. |
| Gender ratio | Boys > girls. Case series report that 80–90% of ureteral polyps occur in boys. |
| Age predilection | Unclear, though a case series of 15 patients had a mean age of 9.1 |
| Risk factors | Unknown |
| Treatment | Open, laparoscopic, or robotic pyeloplasty, ureteroscopic resection, holmium laser resection |
| Prognosis | Good with low rate of recurrence |
| Findings on imaging | Can present as a solitary non-obstructive filling defect on radiography. Ultrasound may show signs of ureteropelvic junction obstruction, like hydronephrosis or hydroureter, or a mildly echogenic structure with a polypoid projection without acoustic shadow. CT may show soft tissue filling the UPJ and 3D reformations can sometimes more clearly delineate the structure. However polyps are often not detected on imaging. |
Table 2.
| Differential Diagnosis | Ultrasound | CT Scan | Retrograde pyelogram |
|---|---|---|---|
| Ureteral Fibroepithelial polyp | Hydronephrosis or hydroureter. A vascular mass obstructing the ureter is occasionally seen on Doppler ultrasound | Hydronephrosis or hydroureter with soft tissue obstructing the ureter | Smooth or polypoid intraluminal lesion with proximal dilation of the urinary tract |
| Congenital narrowing of the ureter | Prenatal dilation of the urinary collecting system proximal the stricture | Proximal hydronephrosis and hydroureter without an obstructing mass | Stricture without an obstructing mass |
| Crossing lower pole vessel | Evidence of hydronephrosis during periods of pain, with normal findings after resolution of pain; more common in hydronephrosis found post-natally | Vessel crossing the ureter at the point of obstruction of the urinary collecting system | Visualization of the proximal ureter with an abrupt cut-off |
| Stone Disease | Urinary obstruction proximal to an obstructing stone. Stone may cause shadowing of US beam. | Perinephric stranding and radiodense material (stone) at the point of urinary obstruction | Filling defect and radiodense material (stone) at the point of urinary obstruction |
ABBREVIATIONS
- CT
Computed Tomography
- GI
Gastrointestinal
- MAG3
Mercaptoacetyltriglycine
- MRI
Magnetic Resonance Imaging
- UPJ
Ureteropelvic junction
REFERENCES
- 1.Adey GS, Vargas SO, Retik AB, Borer JG, Mandell J, Hendren WH, Lebowitz RL, Bauer SB. Fibroepithelial polyps causing ureteropelvic junction obstruction in children. J Urol. 2003 May;169(5):1834–6. doi: 10.1097/01.ju.0000061966.21966.94. [DOI] [PubMed] [Google Scholar]
- 2.Niu ZB, Yang Y, Hou Y, Chen H, Wang CL. Ureteral polyps: an etiological factor of hydronephrosis in children that should not be ignored. Pediatr Surg Int. 2007 Apr;23(4):323–6. doi: 10.1007/s00383-007-1884-z. [DOI] [PubMed] [Google Scholar]
- 3.Lavelle JP, Knisely AS, Bellinger MF. Benign fibroepithelial polyps causing symptomatic bilateral intermittent hydroureteronephrosis. J Urol. 1997 Aug;158(2):569. [PubMed] [Google Scholar]
- 4.Bartone FF, Johansson SL, Markin RJ, Imray TJ. Bilateral fibroepithelial polyps of ureter in a child. Urology. 1990 Jun;35(6):519–22. doi: 10.1016/0090-4295(90)80107-x. [DOI] [PubMed] [Google Scholar]
- 5.Romesburg JW, Stein RJ, Desai MM, Lagwinski N, Ross JH. Treatment of child with bilateral ureteropelvic junction obstruction due to fibroepithelial polyps and review of the literature. Urology. 2009 Apr;73(4):929 e9–11. doi: 10.1016/j.urology.2008.04.040. [DOI] [PubMed] [Google Scholar]
- 6.Liddell RM, Weinberger E, Schofield DE, Pelman RS. Fibroepithelial polyp of the ureter in a child. AJR Am J Roentgenol. 1991 Dec;157(6):1273–4. doi: 10.2214/ajr.157.6.1950880. [DOI] [PubMed] [Google Scholar]
- 7.Kojima Y, Lambert SM, Steixner BL, Laryngakis N, Casale P. Multiple metachronous fibroepithelial polyps in children. J Urol. 2011 Mar;185(3):1053–7. doi: 10.1016/j.juro.2010.10.046. [DOI] [PubMed] [Google Scholar]
- 8.Golda N, Kapoor A, DeMaria J. Laparoscopic pyeloplasty: role of preoperative retrograde pyelography. J Pediatr Urol. 2008 Apr;4(2):162–4. doi: 10.1016/j.jpurol.2007.07.006. [DOI] [PubMed] [Google Scholar]
- 9.Cerwinka WH, Kirsch AJ. In: Urinary Tract Obstruction Pediatric Urology. Palmer JS, editor. Humana Press; 2011. pp. 269–85. [Google Scholar]
- 10.Rooks VJ, Lebowitz RL. Extrinsic ureteropelvic junction obstruction from a crossing renal vessel: demography and imaging. Pediatr Radiol. 2001 Feb;31(2):120–4. doi: 10.1007/s002470000366. [DOI] [PubMed] [Google Scholar]
- 11.Fordham LA, Sutherland RW, Gipson DS. In: Imaging of Nephrolithiasis and Urinary Tract Calculi in Children Evidence-Based Imaging in Pediatrics. Medina LS, Applegate KE, Blackmore CC, editors. Springer; New York: 2010. pp. 555–68. [Google Scholar]
- 12.Hwang AH, McAleer IM, Shapiro E, Miller OF, Krous HF, Kaplan GW. Congenital mid ureteral strictures. J Urol. 2005 Nov;174(5):1999–2002. doi: 10.1097/01.ju.0000176462.56473.0c. [DOI] [PubMed] [Google Scholar]