Abstract
The tibialis posterior tendon is the largest and anteriormost tendon in the medial ankle. It produces plantar flexion and supination of the ankle and stabilizes the plantar vault. Sonographic assessment of this tendon is done with high-frequency, linear-array transducers; an optimal examination requires transverse retromalleolar, longitudinal retromalleolar, and distal longitudinal scans, as well as dynamic studies. Disorders of the posterior tibial tendon include chronic tendinopathy with progressive rupture, tenosynovitis, acute rupture, dislocation and instability, enthesopathies. The most common lesion is a progressive “chewing gum” lesion that develops in a setting of chronic tendinopathy; it is usually seen in overweight women over 50 years of age with valgus flat feet. Medial ankle pain must also be carefully investigated, and the presence of instability assessed with dynamic maneuvers (forced inversion, or dorsiflexion) of the foot. Sonography plays an important role in the investigation of disorders involving the posterior tibial tendon.
Keywords: Posterior tibial tendon, Ankle, Sonography
Sommario
Il tendine tibiale posteriore è il tendine più anteriore e più grande del versante mediale della caviglia. Si tratta di un potente flessore plantare e supinatore della caviglia, partecipa alla stabilità della volta plantare.
Per la sua valutazione ecografica si utilizzano sonde lineari ad alta frequenza; per il suo studio ottimale sono necessarie scansioni: retromalleolare assiale, retromalleolare longitudinale, longitudinale distale, completate con studio dinamico.
Le sue patologie sono rappresentate da: tendinopatia cronica e rottura progressiva, tenosinovite, rottura acuta, lussazione e instabilità, patologia dell’entesi.
La sua patologia predominante è la rottura progressiva tipo “chewing gum” su tendinopatia cronica, in donne sovrappeso, di età superiore ai 50 anni, con piede piatto valgo.
Si deve anche considerare attentamente il dolore mediale negli atleti e ricercare l’instabilità attraverso la manovra dinamica di inversione forzata (dorsi-flessione) del piede.
L’ecografia riveste un ruolo predominante nello studio delle patologie del tendine tibiale posteriore.
Introduction
Anatomy of the tibial posterior tendon (TTP)
The tibialis posterior tendon muscle originates on the tibia, the interosseous membrane, and the fibula. It descends within the posterior compartment of the leg, between the flexor digitorum longus (FDL) and the flexor hallucis longus (FHL). It has a central lamina that continues downward with the distal tendon, which terminates at the level of the ankle with a shift in direction of almost 90° around the medial malleolus (Fig. 1).
Figure 1.

Schematic of the anatomy of the tibialis tendon. The sagittal lamina (short arrow) of the muscle is followed by the tendon, which lies behind the medial malleolus (long arrow). The terminal portion fans out beneath the navicular bone and the adjacent tarsals (asterisk).
Its plantar insertion is complex: on one side there are multiple insertions on the navicular tuberosity; on the other, the main tendon has insertions on all of the tarsal bones with the exception of the astragalus, and on the second, third, and fourth metatarsals, with fan-shaped fascicles.
It is largest, most anterior-lying tendon on the medial aspect of the ankle (Fig. 2).
Figure 2.
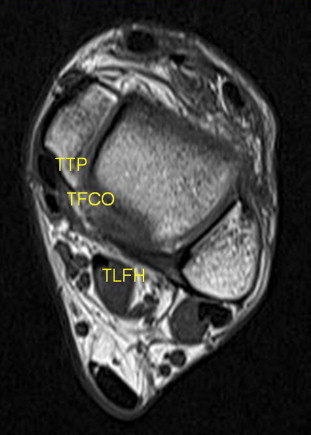
Axial T1-weighted MRI scan through the malleoli. The tibialis posterior tendon (TTP) is immediately behind the malleolus and is about twice as large as the common flexor digitorum (TFCO) located on the posterior border of tibialis posterior tendon.
Function
The TTP is a powerful plantar and supinator of the ankle (supination = adduction + internal rotation). Along with the calcaneonavicular ligament, it is also one of the main sources of support for the medial arch of the foot.
Sonographic examination technique and normal findings
The superficial structure of the tendon should be explored with a high-frequency, linear-array transducer [1–3]. Considering the anatomic concepts described above, the examiner obtains a series of sequential transverse images along the medial malleolus and a longitudinal scan, posterior and inferior to the medial malleolus, all the way to the insertion of the tendon (Fig. 3). The study ends with a systematic exploration of the median collateral and calcaneonavicular ligaments, which is carried out during forced dorsiflexion of the foot.
Figure 3.

Position of the transducer for reference scans. The double arrows indicate the location of scans used to examine the posterior tibial tendon.
Three scans in particular are important. They are supplemented by dynamic studies [4] made during forced inversion (dorsiflexion) of the foot:
-
1.
Transverse retromalleolar scan (Fig. 4): The tendon is identified immediately behind the malleolus. It is twice as large as the flexor digitorum, which lies next to it. The proper position of the tendon is verified, and the synovial sheath and retinaculum (thin hypoechoic stria) are identified.
-
2.
Longitudinal retromalleolar scan: This scan confirms the continuity of the tendon and the absence of irregularities in its caliber. The appearance of the LCM (deltoid ligament), is also assessed.
-
3.
Longitudinal scan of the distal segment: The scan visualizes the major insertion on the navicular bone (which is often hypoechoic and difficult to identify due to anisotropy). It may also reveal an accessory navicular bone, a frequent anatomic variant that favors the development of insertional tendinopathy (Fig. 5). The calcaneonavicular ligament is seen lying deep to the TTP. There is generally a small amount of fluid at this level, which should not be interpreted as evidence of tenosynovitis (Fig. 6).
-
4.
Dynamic study: In the maneuver referred to as forced inversion (dorsiflexion) of the foot, the patient is instructed to adduct and internally rotate the foot against manual resistance applied by the sonographer, using his/her left hand. The transducer is positioned transversally, between the medial malleolus and the TTP, which is covered by the retinaculum (Fig. 7). In general, there is only mild deformation of the retinaculum, and the tendons remain in their normal position behind the malleolus.
Figure 4.
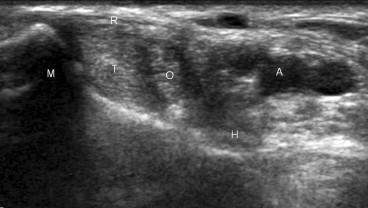
Normal appearance of the retromalleolar region on axial scan: M: malleolus, R: retinaculum, T: tibialis posterior tendon, O: flexor digitorum communis tendon, H: flexor hallucis longus tendon, A: tibial artery.
Figure 5.

Longitudinal section of the insertion of the tibialis posterior tendon (TTP) on the navicular bone (NAV). In this case, an accessory navicular bone is also clearly visualized (dotted line).
Figure 6.

Longitudinal inframalleolar section reveals a small amount of nonpathological fluid (arrow), in the sheath of the posterior tibialis tendon (T). M: malleolus, N: navicular.
Figure 7.

Forced inversion (dorsiflexion) of the foot. The patient is placed in the lateral decubitus positioned beside the examiner and instructed to point his/her forefoot toward the ceiling, against manual resistance provided by the examiner.
Pathological findings
Chronic tendinopathy and progressive rupture
This is the most common tendon disorder [3,5]; it occurs mainly in patients over 50 years of age who are overweight and have valgus flat feet. In the initial stages, as in other types of tendinopathy, the tendon is thickened, more or less fusiform, and hypoechoic. Gradually, microfractures appear as longitudinal fissures, and finally the tendon wears thin and loses its normal mechanical properties although its continuity seems to be at least partially maintained: this type of injury is known as a “chewing gum” lesion (Fig. 8). To make certain there is no pathological thinning, the size of the TTP should be compared with that of the flexor of the adjacent toes. (Promemoria: normal TTP = twice the CFD).
Figure 8.

Longitudinal retromalleolar scan: The tortuous appearance of the posterior tibial tendon (TTP), with loss of its fibrillar structure and frank caliber irregularities, are indicative of a “chewing gum” rupture.
Tenosynovitis
Tenosynovitis can occur before, during, or after a rupture. It is variably associated with suffusion of the sheath, thickening, and hyperemia of the synovia on Doppler.
Acute rupture
Acute ruptures are much less common that chronic ones, but their frequency has probably been underestimated. The clinical settings are also quite different: the acute tear occurs in athletic individuals who have suffered repeated sprains.
The supramalleolar segment of the tendon is in close proximity to the medial ligament, and this is probably a source of error, which can be corrected with sonography.
Dislocation and instability
Dislocation of the tibialis posterior tendon [6–8] is quite rare compared with that of the peroneal tendons; it, too, occurs in athletes as a result of accidental inversion and dorsiflexion of the foot or repeated microtrauma.
The sonogram reveals a retinaculum that is thickened, hypoechoic, or torn, and in some cases corticoperiosteal avulsion (Fig. 9).
Figure 9.
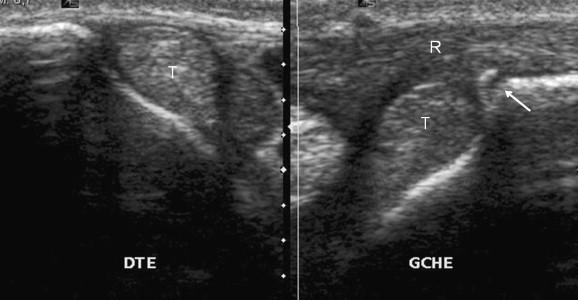
Axial retromalleolar scan of the right (normal) and left ankles. On the left, the retinaculum (R) presents hypoechoic thickening and cortical detachment (arrow). The posterior tibial tendon (T) is normally positioned in both ankles.
True luxation is associated with obvious anterior displacement of the tendon over the malleolus.
In cases of instability without permanent luxation, forced inversion (dorsiflexion) of the foot is a useful maneuver for demonstrating the anomalous course of the tendon, which is shifted anteriorly (Fig. 10).
Figure 10.
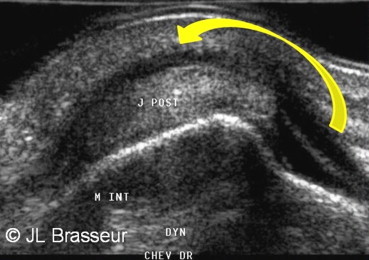
Dynamic maneuver for assessing the stability of the posterior tibial tendon: during the maneuver the tendon shifts anteriorly over the malleolus, reflecting its instability.
Enthesopathy
Enthesopathy can be a component of inflammatory arthritis or an exclusively local disorder, which is often caused by the presence of an accessory navicular bone.
In either case, the classic picture consists of an irregular cortical bone profile, heterogeneity of the tendon insertion, hyperemia on color Doppler, more or less extensive calcifications, in the chronic phases.
Conclusions
Points to remember
The posterior tibial tendon is easy to recognize: it is the largest and the most anterior of the medial ankle tendons, blocked by the retinaculum behind the medial malleolus.
The most common disorder is a progressive “chewing gum” tear, which develops against a background of tendinopathy in overweight women over 50 years of age with flat valgus feet.
Medial pain in an athlete should also be carefully investigated to exclude instability, which can be done with forced inversion (dorsiflexion) of the foot.
Conflict of interests
The authors have no conflicts of interest to declare.
Appendix. Supplementary data
The following is the Supplementary data related to this article:
References
- 1.Hamel J., Seybold D. Ultrasound diagnosis of the posterior tibial tendon. Orthopade. 2002 Mar;31(3):328–329. doi: 10.1007/s00132-002-0309-x. [DOI] [PubMed] [Google Scholar]
- 2.Miller S.D., Van Holsbeeck M., Boruta P.M., Wu K.K., Katcherian D.A. Ultrasound in the diagnosis of posterior tibial tendon pathology. Foot Ankle Int. 1996 Sep;17(9):555–558. doi: 10.1177/107110079601700908. [DOI] [PubMed] [Google Scholar]
- 3.Nallamshetty L., Nazarian L.N., Schweitzer M.E., Morrison W.B., Parellada J.A., Articolo G.A. Evaluation of posterior tibial pathology: comparison of sonography and MR imaging. Skeletal Radiol. 2005 Jul;34(7):375–380. doi: 10.1007/s00256-005-0903-1. [DOI] [PubMed] [Google Scholar]
- 4.Brasseur J.L., Morvan G., Godoc B. Dynamic ultrasonography. J Radiol. 2005 Dec;86(12 Pt 2):1904–1910. doi: 10.1016/s0221-0363(05)81544-6. [DOI] [PubMed] [Google Scholar]
- 5.Janis L.R., Wagner J.T., Kravitz R.D., Greenberg J.J. Posterior tibial tendon rupture: classification, modified surgical repair, and retrospective study. J Foot Ankle Surg. 1993 Jan-Feb;32(1):2–13. [PubMed] [Google Scholar]
- 6.Ouzounian T.J., Myerson M.S. Dislocation of the posterior tibial tendon. Foot Ankle. 1992 May;13(4):215–219. doi: 10.1177/107110079201300409. [DOI] [PubMed] [Google Scholar]
- 7.Goucher N.R., Coughlin M.J., Kristensen R.M. Dislocation of the posterior tibial tendon: a literature review and presentation of two cases. Iowa Orthop J. 2006;26:122–126. [PMC free article] [PubMed] [Google Scholar]
- 8.Prato N., Abello E., Martinoli C., Derchi L., Bianchi S. Sonography of posterior tibialis tendon dislocation. J Ultrasound Med. 2004 May;23(5):701–705. doi: 10.7863/jum.2004.23.5.701. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


