Abstract
The unroofed coronary sinus is a spectrum of cardiac anomalies in which part or all of the common wall between the coronary sinus and the left atrium is absent. Most cases are associated with anomalous systemic venous return, such as persistent left superior vena cava.
The diagnosis of this lesion is important to the prognosis of the patient, but it is often difficult because of nonspecific clinical features.
Here we report a case of a complete unroofed coronary sinus and persistent left superior vena cava discovered during a computed tomographic investigation for pulmonary hypertension.
Keywords: Unroofed coronary sinus, Persistent left superior vena cava, Congenital heart disease, Computed tomography
Sommario
“Unroofed coronary sinus” comprende un insieme di anomalie cardiache in cui la parete comune fra seno coronarico e atrio sinistro è parzialmente o completamente assente. La maggior parte dei casi è associata a un ritorno venoso sistemico anomalo, come la persistenza della vena cava superiore sinistra.
La diagnosi di questa anomalia è importante per la prognosi del paziente, ma è spesso difficoltosa a causa dei segni clinici aspecifici.
Qui illustriamo un caso di assenza completa del tetto del seno coronarico associato a persistenza della vena cava superiore sinistra, riscontrato durante un esame di tomografia computerizzata effettuato per ipertensione polmonare.
Introduction
Unroofed coronary sinus is a rare congenital cardiac anomaly in which there is partial (either focal or fenestrated) or complete absence of the roof of the coronary sinus, which results in a communication between the coronary sinus and the left atrium. Unroofed coronary sinus is the rarest type of atrial septal defect. It is often associated with persistent left superior vena cava and other forms of complex congenital heart disease, usually heterotaxia syndromes [1].
The diagnosis of this lesion is important to the prognosis of the patient because of the consequences of brain abscess or cerebral emboli that may result from a right-to-left shunt. However, the diagnosis is often difficult because of nonspecific clinical features [2].
The treatment of unroofed coronary sinus and persistent left superior vena cava is undertaken only after assessing the pre- and post- treatment hemodynamics of all co- existing abnormalities [3].
Case report
A 54-year-old man with rheumatoid arthritis was admitted to our institution for the discovery of pulmonary hypertension.
After an inconclusive transthoracic echocardiography, a transesophageal echocardiography revealed the presence of an interatrial defect of almost 25 mm (Fig. 1).
Figure 1.
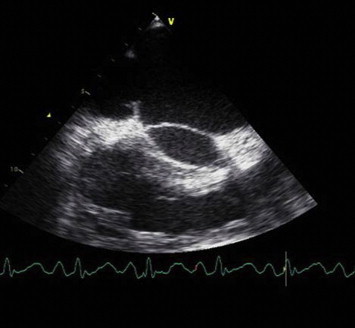
Transesophageal echocardiography reveals the presence of an interatrial defect of almost 25 mm.
So the patient underwent cardiac catheterization which showed a moderate pre-capillary pulmonary hypertension with normal right atrial pressure and an oxymetric gap between the superior vena cava (SVC) and pulmonary artery.
Cardiac computed tomography (CT) was performed, using a dual-source 64-slice scanner (Definition, Siemens, Germany) with a retrospective electrocardiographic gating.
It revealed a wide communication (24 × 26 mm) between the right atrium (RA) and the left atrium (LA) for a complete absence of the roof of the coronary sinus (CS) (Fig. 2a, b and c). The CS was dilated (diameter 27 × 37 mm), with an ostium in the RA of about 38 × 25 mm.
Figure 2.
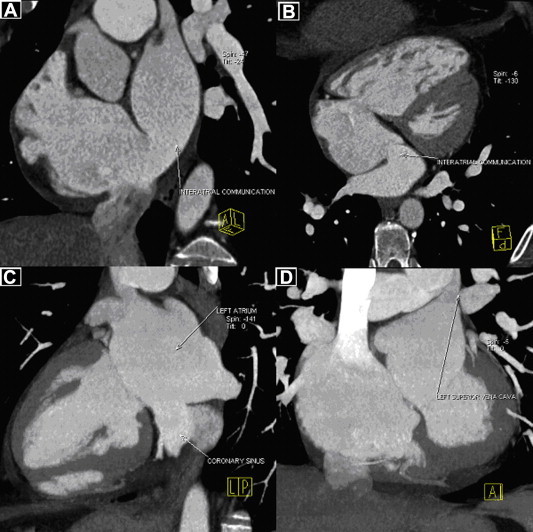
Contrast-enhanced gated multidetector CT. A–B, Multiplanar reformatted images show a wide communication (24 × 26 mm) between the right atrium and the left atrium. C, Maximum intensity projection image shows a complete absence of the roof of the coronary sinus. D, Maximum intensity projection image shows left superior vena cava draining directly to the superior corner of the left atrium.
The great cardiac vein and the posterolateral vein didn't drain into the CS but directly into the LA; the middle cardiac vein merged into the LA next to the ostium of the CS (Fig. 3).
Figure 3.
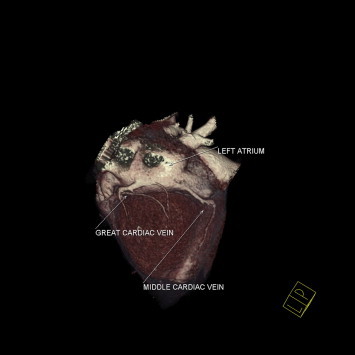
Contrast-enhanced gated multidetector CT. Volume rendering image shows the great cardiac vein and the posterolateral vein draining into the left atrium; the middle cardiac vein merges into the left atrium next to the ostium of the coronary sinus.
CT also revealed a bilateral SVC without an intercommunicating vein, right SVC drainage to RA and left SVC (LSVC) draining directly to the superior corner of the LA between the left atrial appendage and the left superior pulmonary vein (Fig. 2d).
No anomalous pulmonary venous returns were present.
The right ventricle was markedly dilated with a basal transverse diameter of 62 mm; the left ventricle was moderately compressed, with a basal transverse diameter of 36 mm. The interventricular septum showed an inversion of its normal left concavity. The RA was markedly dilated. Enlargement of the LA and of the pulmonary artery and its main branches was also noted.
Informed consent was obtained from the patients' parents for the publication of this case report and accompanying images.
Discussion
The complex of an unroofed coronary sinus (UCS) and a persistent left superior vena cava (LSVC) is a rare congenital heart disease first described by Raghib et al. in 1965 [3].
A normal CS drains the cardiac veins into the RA and it accounts for 75% of the cardiac venous circulation [3], returning blood from nearly all regions of the heart, including the septa [4]. It opens into the RA through a orifice that may be guarded by a thebesian valve of variable size. This orifice is located in the posterior and inferior walls of the RA superior to the tricuspid valve [5]. The first branch of the CS is the posterior interventricular vein, also known as the middle cardiac vein, which courses in the posterior interventricular groove from base to apex. The next two branches are the posterior vein of the left ventricle and the left marginal vein. At this point, the CS becomes the great cardiac vein, which courses in the left atrioventricular groove with the left circumflex artery. It then continues as the anterior interventricular vein in the anterior interventricular groove, coursing from the base of the heart toward the apex adjacent to the left anterior descending artery [6].
CS, as well as SVC, develops from the anterior and common cardinal vein. Of these, the LSVC regresses at the sixth fetal month, and a small portion remains as the left superior intercostal vein and CS. With the deficiency of the left atriovenous fold, the left side of the sinus venosus maintains continuity and represents the termination of the LSVC in the LA. The LSVC does not regress in 0.5% of the general population and in 3–10% of people with congenital heart disease. Most LVCSs drain into the RA via CS, but they may drain into the LA in approximately 10% of case [7].
LSVC is associated with UCS in 75% [8].
UCS and persistent LSVC may be further associated with other cardiac abnormalities such as atrioventricular septal defect, atrial appendage abnormalities and coronary sinus ostial atresia [3].
The morphological types of UCS have been classified into 4 groups: type I, completely unroofed with persistent LSVC (as illustrated in the present case); type II, completely unroofed without persistent LSVC; type III, partially unroofed mid portion; and type IV, partially unroofed terminal portion. The fenestration into the left atrium typically occurs between the left atrial appendage and the left upper pulmonary vein. The size of the defect and the degree of left-to-right shunt generally determine the clinical presentation [1].
The spectrum of symptoms may range from asymptomatic to nonspecific complaints to severe dyspnea with symptoms of overt right-sided heart failure from chronic right ventricular volume overload. Management is guided by the presence of clinical symptoms, with consideration of surgical repair when symptoms prevail [1].
The diagnosis of this lesion is important to the prognosis of the patient because of the consequences of brain abscess or cerebral emboli that may result from a right-to-left shunt [2]. However, UCS is very difficult to diagnose by clinical symptoms and signs only. It should be suspected in patients with left-to-right interatrial shunt and unexplained arterial oxygen desaturation or cerebral complication [8].
Reports on preoperative diagnosis of UCS have relied on cardiac catheterization and angiography, but diagnosis is difficult unless the heart is explored with a catheter through the left arm [7]. However, catheter insertion is not performed via the left arm because manipulation of the catheter is difficult [8]. Therefore, many cases of UCS have been found incidentally during the operation or at necropsy [7].
Echocardiography is the most widely applied non-invasive study technique, but deep structures such as pulmonary veins or CS draining into the posterior wall of the LA are not well delineated by transthoracic echocardiography [7].
Transesophageal echocardiography and cardiac MRI can more accurately assess these posterior structures [1]; in particular MRI provides high contrast between the wall of the cardiovascular structures without the injection of a contrast media [7].
Multidetector CT with its excellent spatial resolution allows for the visualization and accurate anatomic and morphological evaluation of the posterior structures of the heart. Gated cardiac CT is emerging as a potentially useful non-invasive imaging modality for evaluation of the coronary venous system [1].
In conclusion, patients with clinical signs of left-to-right shunt combined with anomalous systemic venous return should be suspected of having UCS.
Because of high resolution of cardiovascular structures, and the easy diagnosis, CT is a good non-invasive tool for evaluation of defects of the wall of the CS.
Conflict of interest
The authors have no conflicts of interest to disclose.
Appendix A. Supplementary material
References
- 1.Thangaroopan M., Truong Q.A., Kalra M.K., Yared K., Abbara S. Images in cardiovascular medicine. Rare case of an unroofed coronary sinus: diagnosis by multidetector computed tomography. Circulation. 2009 Apr 28;119(16):e518–e520. doi: 10.1161/CIRCULATIONAHA.107.707018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ootaki Y., Yamaguchi M., Yoshimura N., Oka S., Yoshida M., Hasegawa T. Unroofed coronary sinus syndrome: diagnosis, classification, and surgical treatment. J Thorac Cardiovasc Surg. 2003 Nov;126(5):1655–1656. doi: 10.1016/s0022-5223(03)01019-5. [DOI] [PubMed] [Google Scholar]
- 3.Kong P.K., Ahmad F. Unroofed coronary sinus and persistent left superior vena cava. Eur J Echocardiogr. 2007 Oct;8(5):398–401. doi: 10.1016/j.euje.2006.06.004. Epub 2006 Jul 11. [DOI] [PubMed] [Google Scholar]
- 4.Chou M.C., Wu M.T., Chen C.H., Lee M.H., Tzeng W.S. Multidetector CT findings of a congenital coronary sinus anomaly: a report of two cases. Korean J Radiol. 2008 Jul;9(Suppl.):S1–S6. doi: 10.3348/kjr.2008.9.s.s1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Adatia I., Gittenberger-de Groot A.C. Unroofed coronary sinus and coronary sinus orifice atresia. Implications for management of complex congenital heart disease. J Am Coll Cardiol. 1995 Mar 15;25(4):948–953. doi: 10.1016/0735-1097(94)00475-6. [DOI] [PubMed] [Google Scholar]
- 6.O'Brien J.P., Srichai M.B., Hecht E.M., Kim D.C., Jacobs J.E. Anatomy of the heart at multidetector CT: what the radiologist needs to know. Radiographics. 2007 Nov-Dec;27(6):1569–1582. doi: 10.1148/rg.276065747. [DOI] [PubMed] [Google Scholar]
- 7.Hahm J.K., Park Y.W., Lee J.K., Choi J.Y., Sul J.H., Lee S.K. Magnetic resonance imaging of unroofed coronary sinus: three cases. Pediatr Cardiol. 2000 Jul-Aug;21(4):382–387. doi: 10.1007/s002460010087. [DOI] [PubMed] [Google Scholar]
- 8.Brancaccio G., Miraldi F., Ventriglia F., Michielon G., Di Donato R.M., De Santis M. Multidetector-row helical computed tomography imaging of unroofed coronary sinus. Int J Cardiol. 2003 Oct;91(2–3):251–253. doi: 10.1016/s0167-5273(03)00042-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


