Abstract
Local injection of cortisone derivatives, sometimes combined with local anesthetics, is frequently administered in rheumatology as the treatment of choice in para-articular diseases or as an adjuvant to systemic therapy in the treatment of arthritis.
One of the most frequent local corticosteroid injections administered in daily clinical practice by rheumatologists, orthopedic surgeons, physiatrists, sports medicine doctors and general practitioners is injection into the subacromialsubdeltoid bursa in the treatment of bursitis and anterior superior impingement syndrome of the shoulder.
Before local corticosteroid injection is administered, it is important to identify possible contraindications and to examine the documentation provided by the patient. Absolute contraindications or those related to the procedure should be evaluated by the prescribing physician but also the physician performing the corticosteroid injection should evaluate possible contraindications to make sure that corticosteroid injection is feasible. The present paper describes the ultrasound (US) guided local corticosteroid injection procedure with particular attention to the equipment required, the position of the patient and the examiner as well as the approach. The main advantage of US guidance during corticosteroid injection is the possibility to identify vascular structures, nerves and tendons situated in the needle path in order to avoid these structures and be sure to inject the drug into the appropriate location. When all rules are complied with and the corticosteroid injection is carried out by an experienced physician, it is virtually painless and is performed in just a few minutes.
Keywords: Subacromial-subdeltoid bursa, Sonography, Local corticosteroid injection
Sommario
L’infiltrazione locale di derivati cortisonici, uniti o non ad anestetici locali, è una modalità terapeutica di utilizzo molto frequente in reumatologia, praticata come terapia di elezione delle patologie para-articolari o come adiuvante al trattamento sistemico nella cura delle artriti.
Una delle più frequenti infiltrazioni locali, nella pratica clinica giornaliera di reumatologi, ortopedici, fisiatri, medici dello sport e medici generici è l’iniezione nella borsa sinoviale sottoacromiondeltoidea, quale trattamento della borsite e nella sindrome da conflitto antero-superiore della spalla.
Prima di eseguire una procedura di infiltrazione locale è importante individuare eventuali controindicazioni e visionare la documentazione fornita dal paziente. Anche se la valutazione delle controindicazioni assolute o relative alla procedura spetta, di principio, al medico prescrittore, è compito del medico ecografista che pratica l’infiltrazione accertarsi della fattibilità della infiltrazione e della presenza di eventuali controindicazioni.
Viene presentata la tecnica di esecuzione dell’infiltrazione locale ecoguidata, con particolare attenzione al materiale necessario, alla posizione del paziente e dell’esaminatore e alle vie di accesso.
I principali vantaggi dell’infiltrazione ecoguidata sono quelli di riconoscere strutture vascolari, nervose e tendinee poste sul decorso dell’ago, in modo da poterle evitare e di poter iniettare il farmaco con certezza nella sede desiderata.
Quando tutte le regole vengono rispettate e l’infiltrazione è praticata da un professionista qualificato, è praticamente indolore e viene realizzata in soli pochi minuti.
Introduction
Local injection of cortisone derivatives, sometimes combined with local anesthetics, is frequently administered in rheumatology as the treatment of choice in para-articular diseases or as an adjuvant to systemic therapy in the treatment of arthritis.
Corticosteroids can be injected into a synovial cavity (joints, tendon sheaths, periarticular bursae) or the paratendinous soft tissue. The objective of the procedure is to 1) inject the smallest possible, effective amount of drug (in order to reduce side effects associated with excessive amounts of drugs) as close as possible to the target; 2) introduce the needle through the surrounding tissues as safely as possible without damaging vessels, nerves and tendons situated in the needle path.
Previously corticosteroid injections were carried out under clinical guidance based on palpatory findings alone. Clinical experience generally permits local corticosteroid injection to be carried out effectively, but there is no evidence confirming the correct performance when the procedure is guided only by clinical data. An incorrect injection technique can be painful for the patient and lead to accidental intra-tendinous injection of cortisone leading to possible tendinopathy or permanent injury.
Local corticosteroid injection guided by imaging ensures a correct injection into the chosen target and reduces the harmful effects of an injection which is not adequately performed [1]. Previously, local corticosteroid injections were also performed under the guidance of conventional radiology (e.g. intra-articular injection of drugs during arthrography) or CT guidance (injections into the rachis). In these cases both the patient and the radiologist are exposed to ionizing radiation, and the injection must necessarily be performed in a department of radiology with a consequent increase in costs. Thanks to the technological progress, new software and hardware, low cost and the dynamic nature of this method, US has in the recent years become a quick and safe procedure for guiding local corticosteroid injections [2–12]. This technique does furthermore not use ionizing radiation and can be carried out also in the general practitioner’s surgery.
One of the most frequently performed local corticosteroid injections administered by rheumatologists, orthopedic surgeons, physiatrists, sports medicine doctors and general practitioners is injection into the subacromial-subdeltoid bursa as a treatment of bursitis and anterior superior impingement syndrome of the shoulder. The practical advantages of US guidance is the ability to confirm clinical diagnosis before local corticosteroid injection is administered, identify the most suitable approach on the basis of the anatomy and local pathology, monitor the progress of the needle in real-time and make sure that the drug is being injected into the appropriate location [11,12].
The present paper will describe in detail US guided corticosteroid injection into the subacromial-subdeltoid bursa. The purely technical aspect of the procedure will be evaluated and also the attitude towards the patient for whom this procedure should be as simple, effective and painless as possible as well as free of complications. It is not the authors’ intention to provide general instructions for performing a local corticosteroid injection into the subacromial-subdeltoid bursa but only to describe a technique which has been successfully used in their daily practice for about 25 years.
Pre-injection evaluation
Contraindications
Before local corticosteroid injection is administered it is important to identify possible contraindications and to examine the documentation provided by the patient. Absolute contraindications or those related to the procedure should be evaluated by the prescribing physician, but also the physician performing the corticosteroid injection should evaluate possible contraindications to make sure that corticosteroid injection is feasible.
These are the main contraindications and the authors’ approach to them:
-
•
Systemic or local infection in progress. Absolute contraindication because of the risk of blood-borne infectious bursitis.
-
•
Diabetes. Relative contraindication. Usually local corticosteroid injection is administered using a delayed-release form of steroid and reducing the dose to 50%; the patient is requested to check blood sugar every day for a week after the injection. In case of doubt the diabetes specialist should be consulted.
-
•
Hypertension. Relative contraindication. Daily blood pressure measurement for a week after corticosteroid injection.
-
•
Treatment with anti-coagulant or anti-aggregation drugs. Relative contraindication. If the treatment is well-controlled (adequate International Normalized Ratio (INR) values), local corticosteroid injection is generally well tolerated. The authors never take the initiative to suspend anti-coagulant treatment but prefer contacting the patient’s general practitioner to obtain his/her opinion on the possible need to temporarily suspend the treatment. If the general practitioner consents, local corticosteroid injection is carried out with particular care to avoid adjacent vessels using a 27 gauge needle in order that the injection causes as little damage as possible.
-
•
Allergic reactions to disinfectants (including iodine) and local anesthetics. This phenomenon rarely occurs; the solution is to use products which are well-tolerated by the patient.
-
•
Glaucoma. The specialist ophthalmologist’s opinion must be obtained.
-
•
Previous corticosteroid injection. The authors do not administer more than 3–4 corticosteroid injections per patient per year.
The decision to perform a local corticosteroid injection is the result of a careful evaluation of the patient’s clinical situation (severity of pain), possible contraindications and the general practitioner’s opinion. In cases of doubt, the authors postpone or do not perform the injection and refer the patient to other therapeutic modalities.
Preliminary US examination
After carefully evaluating possible contraindications and after having studied previous images presented by the patient, a complete US examination of the affected shoulder is carried out. If US examination precedes local corticosteroid injection, the usual US gel is substituted by a colorless liquid disinfectant (Hibitane) in order to allow the skin to be in contact with the disinfectant during the whole procedure. If there is a diagnostic difference between preliminary US examination and the indication for local corticosteroid injection, the requesting physician should be contacted to decide on the most appropriate procedure.
US guided local corticosteroid injection technique
The following material is required:
-
•
Sterile Gauze
-
•
Sterile gloves (not considered essential if the infiltration is done correctly according to the rules indicated below). The gloves are intended to protect the physician rather than the patient. Surgical mask.
-
•
Skin disinfectant. The authors prefer Hibitane®.
-
•
30–70 mm long needles, caliber ranging from 21 to 27 gauge.
-
•
Local anesthetic. The authors prefer a 1% lidocaine solution.
-
•
Corticosteroids, generally a delayed-release form. The authors prefer Diprophos® which is a mixture of rapid and delayed-release steroids.
Position (patient and physician)
Most of the US guided corticosteroid injections into the subacromial-subdeltoid bursal space performed in the authors’ department are carried out with the patient sitting on the couch with his/her back turned to the physician. This technique is particularly useful in anxious patients because the handling of syringes and needles takes place outside the patient’s field of view, thus reducing anxiety.
If a there is small fluid collection in the bursa it is important to perform US examination in different positions in order to identify the position in which the fluid tends to collect. In this position it is easier to puncture the fluid-filled bursa. By performing a static and dynamic study, the shoulder is examined in different degrees of rotation so that the fluid is accumulated according to the pressure changes exerted on the subacromial-subdeltoid bursa.
If there is no fluid collection but a thickening of the bursal wall, the injection should be directed toward the thickened portion of the subacromial-subdeltoid bursa. When the most adequate position of the shoulder has been identified, the patient is asked to keep this position while the US probe and skin are disinfected. It is recommended that the physician wears a surgical mask for his own and the patient’s safety. The authors do not use sterile US probe covers, but the probe is disinfected using the same disinfectant which is applied to the patient’s skin. It is recommended that other departments contact their US equipment manufacturer to assess if the probe will be damaged by contact with disinfectant.
With the probe in one hand and the syringe in the other, the skin is punctured after application of more disinfectant. The skin is always punctured at a distance of about 2–3 cm from the probe in order to avoid contact between the needle and the probe. As soon as the needle has penetrated the subcutaneous tissues, its progress must be real-time monitored on the US image. When the US beam is perpendicular to the long axis, the needle is visible as a hyperechoic structure with posterior comet-tail artifact.
The authors generally use a 5 cm long needle caliber 23 Gauge. In particularly anxious patients and in patients receiving (well-managed) anti-coagulant therapy and who are unable to postpone corticosteroid injection, a 27 Gauge needle is used, as it is less traumatic and better tolerated. However, thin needles are more difficult to identify on the US image and furthermore, the thinner the needle the more difficult it is to perform the injection. Delayed-release corticosteroids are injected because of their long-lasting effect. A local anesthetic (lidocaine) can be associated for an analgesic effect. As a rule the authors inject a dose of cortisone mixed with 2–3 cc of 1% lidocaine solution.
Approaches (Fig. 1)
Figure 1.
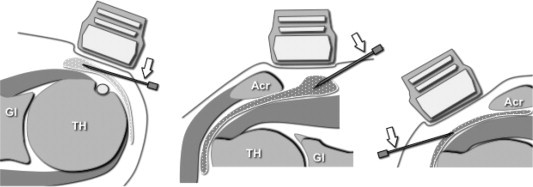
US guided corticosteroid injection into the subacromial-subdeltoid bursa. From left to right: anterior, superior, lateral approaches. Note that the needle is parallel or slightly oblique compared to the surface of the probe. In each picture, the needle tip is inside the subacromial-subdeltoid bursa which is for didactic purposes shown as extended by synovial fluid. Gl = glenoid; TH = humeral head; Acr = acromion; arrow = needle.
The anterior, superior or lateral approach may be the most convenient (depending on the quantity and location of the bursal fluid collection, the patient’s physical structure and the physician’s experience). However, in most cases the authors perform corticosteroid injection using the lateral approach (Fig. 2).
Figure 2.
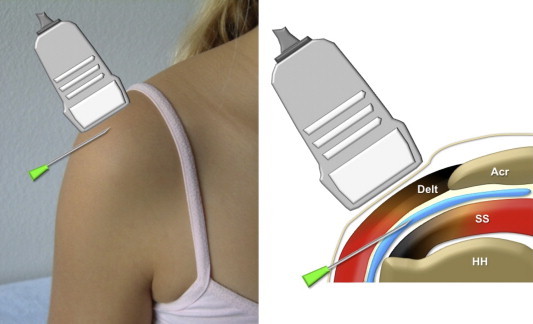
Lateral approach. Left: position of the probe and needle. Right: sagittal drawing showing the needle path. Note the distance between the skin puncture site and the probe; the needle is advancing perpendicular to the US beam in order to improve its US visibility. Delt = deltoid muscle; HH = humeral head; SS = supraspinatus tendon; Acr = acromion.
Anterior approach
The probe is positioned on the axial plane of the front of the shoulder and the needle is inserted in the latero-medial direction to permit its entrance into the subacromial-subdeltoid bursa.
Superior approach
This approach can be used when the fluid collection is situated mainly in the cranial part of the subacromial-subdeltoid bursa between the bottom surface of the trapezium and the upper surface of the supraspinatus. The probe should be positioned in the supraspinatus fossa, parallel to the axis of the supraspinatus with the lateral edge over the acromion. The needle will progress in the medio-lateral direction (Fig. 3). This approach is generally better tolerated by the patient and there is no risk of intra-tendinous injection.
Figure 3.
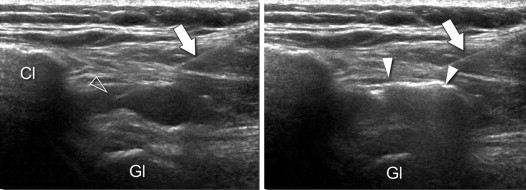
Superior approach. Oblique coronal US scans (see Fig. 1, the central image). Left: image showing the needle correctly positioned before injection. Arrow = needle; arrowhead = the needle tip inside the subacromial-subdeltoid bursa which is distended by synovial fluid. Right: US scan taken during corticosteroid injection (white arrowheads); note that the drug is being correctly injected into the bursa. Cl = clavicle; GL = glenoid.
Lateral approach
This is the most frequently used approach. The probe is positioned parallel to the long axis of the supraspinatus. The needle can be guided by short axis scans and by long axis scans. The authors prefer long axis scans, which allow visualization of the progress of the needle until the tip has entered the subacromial-subdeltoid bursa. This is possible also in the absence of fluid collection (Fig. 4).
Figure 4.
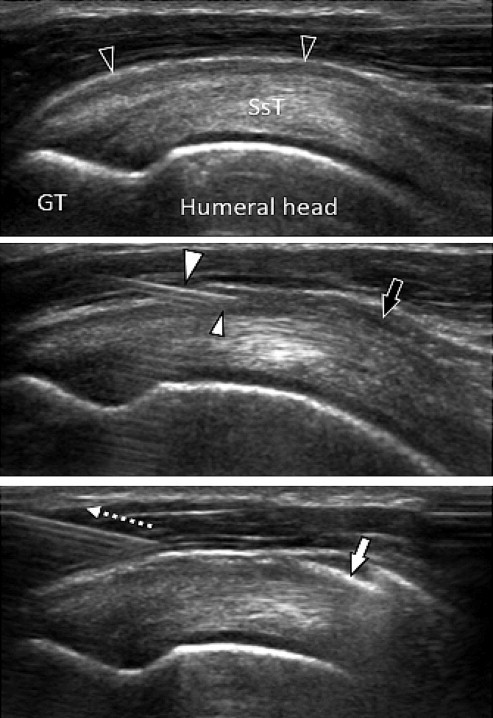
Lateral approach. Oblique coronal US scans (see fig. 1, the right image). Above: image taken before corticosteroid injection; note the significant thickening of the subacromial-subdeltoid bursa (empty arrowheads). SsT = supraspinatus tendon; GT = greater tuberosity of the humerus. Center: The needle (large white arrowhead) is correctly positioned; the tip (small white arrowhead) is inside the subacromial-subdeltoid bursa. A small amount of injected drug (black arrow) is visible inside the subacromial-subdeltoid bursa. Bottom: When the corticosteroid injection is completed the needle is removed (dotted arrow); air microbubbles (white arrow).
When the tip of the needle appears to be inside the subacromial-subdeltoid bursa, a small amount of liquid is injected to confirm the correct position (fluid passing from the needle tip into the bursa). The injection can be visualized in real-time as a spreading "cloud" of hyperechoic echoes inside the bursa (Fig. 4). Real-time US monitoring of the progress of the needle and injection of the drug is particularly useful in subacromial bursitis caused by rupture of rotator cuff calcifications. In such cases it is of paramount importance to avoid that the needle causes further damage to the calcification in order to prevent release of more calcium crystals inside the bursa (Fig. 5).
Figure 5.
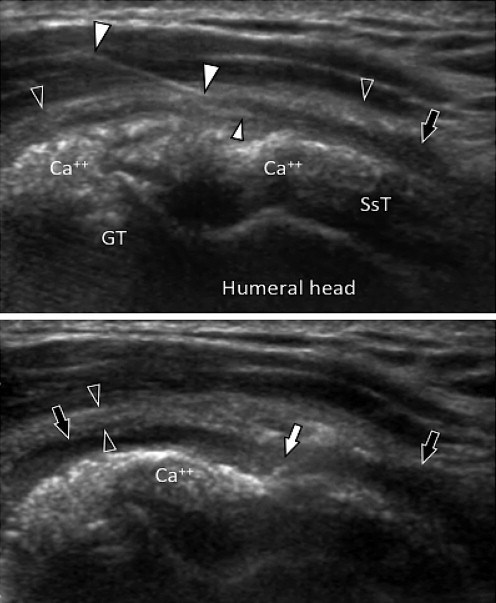
Lateral approach. Oblique coronal US scans (see fig. 1, the right image). Above: large calcifications (Ca + +) of the supraspinatus tendon (SsT). Poorly defined calcifications, significant wall thickening (black arrowheads) and subacromial-subdeltoid bursal fluid collection (arrow) indicate a calcium migratory syndrome (from the tendon to the bursa). The needle (large white arrowheads) was positioned under careful real-time US guidance to avoid damaging the tendon calcifications. The tip (small white arrowhead) is inside the subacromial-subdeltoid bursa. Below: After completion of corticosteroid injection the bursa is distended by the drug (black arrows); note the presence of small air bubbles inside the subacromial-subdeltoid bursa (white arrow).
The patient is requested to avoid loading the shoulder for 2–3 days after corticosteroid injection to maximize the therapeutic effect and reduce spread of the injected drug into the surrounding tissue. A short immobilization is required only in case of bursitis due to apatite calcium crystals. The patients are always informed of the possibility of renewed pain in the hours following the injection (microcrystalline synovitis) and the possibility that a rash may appear.
Complications and side effects
When a local corticosteroid injection is performed by an expert, it is virtually painless and the procedure takes only a few minutes. Complications may occur, but it is the physician’s responsibility to inform the patient about possible risks and obtain informed consent. The physician who performsthe injection should be available in case of possible complications, and it is good practice to give the patient a mobile phone number to contact in case of need.
Complications
The most severe complication is the onset of infection. Corticosteroid injection into the subacromial-subdeltoid bursa may cause bursa infection or soft-tissue abscess. Septic arthritis can theoretically occur as a result of infection of the subacromial-subdeltoid bursa if it communicates with the glenohumeral joint after rupture of the rotator cuff.
If infection occurs despite all the precautions, it will present the classical signs of inflammation: Swelling, warm skin and pain sometimes accompanied by fever. Although the risk of infection is low, the patient should be instructed to contact the performing physician or the general practitioner immediately if these symptoms appear in order to start appropriate treatment.
Side effects
A temporary vasovagal reaction may occur during or after corticosteroid injection, usually within 5–10 min. Although it is not life-threatening, it can be unpleasant for the patient and may occasionally be accompanied by a loss of consciousness and marked hypotension. The greatest danger in these cases is the possibility of falling injury. For this reason the corticosteroid injection is performed with the patient sitting on the couch where he/she can lie down if required. Vasovagal reactions resolve spontaneously, in most cases without requiring drug therapy.
A painful reaction may complicate local corticosteroid injection; it is related to microcrystalline synovitis in cases where delayed-action corticosteroid is used. The pain will disappear spontaneously or upon administration of analgesic medication.
Flushing of the skin may occur 2–3 days after corticosteroid injection, sometimes associated with a warm sensation in the cheeks. This is a reaction to the corticosteroid; it is harmless and will disappear within 48 h and is not related to allergies. This reaction is not a contraindication to future local corticosteroid injections.
On rare occasions there may be skin atrophy or depigmentation at the injection site if the corticosteroid injection was performed in a too superficial, subcutaneous site.
Conclusions
The efficacy of local corticosteroid injection is elevated in the treatment of certain inflammatory and degenerative rheumatic disorders. The main advantage of US guidance during corticosteroid injection is that vascular, neural and tendinous structures situated in the needle path are identified so that they can be avoided, and the drug drug can with certainty be injected into the appropriate location.
US guided corticosteroid injection into the subacromial-subdeltoid bursa is a simple procedure which is in most cases well-tolerated by the patients. However, when it is carried out certain rules must be followed:
-
•
The patient’s clinical history must be studied in detail particularly in order to exclude possible contraindications;
-
•
Diagnostic US examination is required before local corticosteroid injection is performed;
-
•
Strict aseptic precautions must be observed;
-
•
The patient should be monitored for 10–15 min after the injection in case of early complications;
-
•
A physician must be easily contactable if late complications should occur.
Conflict of interests
The authors have no conflict of interest to declare.
Appendix. Supplementary material
The following are the Supplementary material related to this article:
References
- 1.Weidner S., Kellner W., Kellner H. Interventional radiology and the musculoskeletal system. Best Pract Res Clin Rheumatol. 2004;18:945–956. doi: 10.1016/j.berh.2004.05.011. [DOI] [PubMed] [Google Scholar]
- 2.Sibbitt W.L., Jr., Peisajovich A., Michael A.A., Park K.S., Sibbitt R.R., Band P.A. Does sonographic needle guidance affect the clinical outcome of intraarticular injections? J Rheumatol. 2009;36:1892–1902. doi: 10.3899/jrheum.090013. [DOI] [PubMed] [Google Scholar]
- 3.Jeyapalan K., Choudhary S. Ultrasound-guided injection of triamcinolone and bupivacaine in the management of De Quervain’s disease. Skeletal Radiol. 2009;38:1099–1103. doi: 10.1007/s00256-009-0721-y. [DOI] [PubMed] [Google Scholar]
- 4.Grassi W., Farina A., Filippucci E., Cervini C. Sonographically guided procedures in rheumatology. Semin Arthritis Rheum. 2001;30:347–353. doi: 10.1053/sarh.2001.19822. [DOI] [PubMed] [Google Scholar]
- 5.Jacob D., Cyteval C., Moinard M. L’échographie interventionnelle. J Radiol. 2005;86:1911–1923. doi: 10.1016/s0221-0363(05)81546-x. [DOI] [PubMed] [Google Scholar]
- 6.Adler R.S., Sofka C.M. Percutaneous ultrasound-guided injections in the musculoskeletal system. Ultrasound Q. 2003;19:3–12. doi: 10.1097/00013644-200303000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Bodor M., Flossman T. Ultrasound-guided first annular pulley injection for trigger finger. J Ultrasound Med. 2009;28:737–743. doi: 10.7863/jum.2009.28.6.737. [DOI] [PubMed] [Google Scholar]
- 8.Wank R., Miller T.T. ShapiroJF. Sonographically guided injection of anesthetic for iliopsoas tendinopathy after total hip arthroplasty. J Clin Ultrasound. 2004;32:354–357. doi: 10.1002/jcu.20043. [DOI] [PubMed] [Google Scholar]
- 9.DeFriend D.E., Schranz P.J., Silver D.A. Ultrasound-guided aspiration of posterior cruciate ligament ganglion cysts. Skeletal Radiol. 2001;30:411–414. doi: 10.1007/s002560100374. [DOI] [PubMed] [Google Scholar]
- 10.Fanucci E., Masala S., Fabiano S., Perugia D., Squillaci E., Varrucciu V. Treatment of intermetatarsal Morton’s neuroma with alcohol injection under US guide: 10-month follow-up. Eur Radiol. 2004;14:514–518. doi: 10.1007/s00330-003-2057-7. [DOI] [PubMed] [Google Scholar]
- 11.Bianchi S., Mariacher S. Ultrasound guided injections in rheumatology. Rheuma-Schweiz. 2011;3:17–18. [Google Scholar]
- 12.Chen M.J., Lew H.L., Hsu T.C., Tsai W.C., Lin W.C., Tang S.F. Ultrasound-guided shoulder injections in the treatment of subacromial bursitis. Am J Phys Med Rehabil. 2006;85:31–35. doi: 10.1097/01.phm.0000184158.85689.5e. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


