Abstract
There is considerable confusion over the word “pubalgia” with regard to the definition and the etiological causes of this condition. The term pubalgia should be used to indicate disabling pain affecting the pubic region in people who practise sports. Pubalgia affects 10% of those who practise sports and it is particularly prevalent in football players. According to the literature, about 40% of cases of pubalgia are caused by overuse of the symphysis pubis with progressive lesions affecting the rectus abdominal muscles, adductors (rectal-adductor syndrome) and the symphysis itself (osteitis pubis and joint injury). An initial study of the tendons is carried out by ultrasound (US) whereas magnetic resonance imaging (MRI) should be performed to study the bones and joints.
Another 40% of cases of pubalgia are caused by "sports hernia" defined as anteroinferior abdominal wall insufficiency. These alterations can only be identified at dynamic US examination.
About 20% of cases of pubalgia are caused by diseases of the neighboring structures or joints such as diseases of the hip, iliopsoas, hamstring, sacred iliac or nerves, or by urogenital diseases.
Keywords: Pubalgia, Sports hernia, Ultrasound
Sommario
Vi è notevole confusione circa la parola “pubalgia”, sia per quanto riguarda la sua definizione sia per quanto riguarda le sue cause etiologiche. Il termine di pubalgia dovrebbe essere utilizzato per indicare una sintomatologia dolorosa, invalidante che interessa la regione pubica di chi pratica attività sportiva. Sono interessati il 10% di chi pratica attività sportiva con prevalenza per il footbal. Dalla revisione della letteratura circa il 40% delle pubalgie sono da ricondurre a sovraccarico funzionale sulla sinfisi pubica con lesioni progressive che interessano i retti addominali, gli adduttori (sindrome retto-adduttoria), e la sinfisi stessa (osteite pubica e danno alla articolazione). Lo studio dei tendini trova nella ecografia il primo approccio diagnostico riservando alla RM lo studio della componente ossea e articolare.
Un altro 40% dei casi di pubalgia riconosce la causa etiologica nella “sport hernia”, definibile come una insufficienza della parete addominale antero-inferiore. La diagnostica ecografica è l’unica in grado di rilevare tali alterazioni che necessitano per essere individuate un esame dinamico.
Infine in circa il 20% dei casi la pubalgia è causata da patologie di strutture o apparati limitrofi: patologia dell’anca, dell’ileo-psoas, degli hamstring, della sacro iliaca o dei nervi, fino alle patologie urogenitali.
Introduction
Since Spinelli first diagnosed pubalgia in 1932, this term has never ceased to arouse doubts and misunderstandings [1]. Some authors consider pubalgia as a pain localized in the pubic symphysis, others as a pain that affects the pubic area in a wider sense involving other anatomical structures including the non-musculoskeletal structures. According to some authors, this pathology is typical of high-profile athletes, and according to others it may affect anybody engaged in physical activities [2].
At first pubalgia was considered solely as a condition typically caused by overload, but later this diagnosis included also pathologies caused by anatomic weakness (sports hernia) or inflammatory diseases of the symphysis or adjacent to the symphysis pubis as well as urogenital diseases. The very term “sports hernia” or “sportsman’s hernia” was relatively recently introduced, and some authors interpret it as a hernia affecting a person practising sports while others interpret it as a synonym for pubalgia [3] thus adding confusion also to simple literature searches. According to some authors [4] the term pubalgia should cover only the pathology of the wall (pubalgia = sports hernia) while other causes should have their own denomination. This topic is still evolving both in terms of its clinical definition and regarding the etiopatological, diagnostic and therapeutic meaning [5].
The definition of pubalgia as a “disabling pain in the pubic region” might be acceptable, and analysis of the possible causes, anatomical and structural changes and appropriate diagnostic methods is quite complex. According to the literature [6], pubalgia accounts for about 5% of all sports-related pathologies and it affects about 10% of athletes [4]. High-risk sports activities are first of all football followed by hockey, rugby and running. However, the data reported in the literature [7–13] present significant shortcomings of the statistic methodology, e.g. the total number of athletes is not correlated to the specific sport. Given the inconsistencies related to the definition of pubalgia, definition of its causes related to the clinical picture is even more complex. Different pathologies are often present with overlapping clinical features in pubalgic pain [14]. Numerous causes of pubalgia have been described, more than 70 [15,16], such as muscle tendon disorders, osteoarticular disorders and pathologies involving the structures adjacent to the symphysis pubis.
With reference to the classification proposed by Benazzo in 1999 [17], the causes of pubalgia can be grouped somewhat arbitrarily but following a useful methodological approach, starting with pubalgia caused by overload of the symphysis pubis (rectus adductor symphysis syndrome) accounting for approximately 40% of cases, pubalgia caused by parietoabdominal weakness (sports hernia) accounting for about 40% of cases and finally pubalgia caused by pathologies affecting the adjacent organs (column, pelvis and urogenital tract) accounting for about 20% of cases (Table 1). US examination is useful in identifying the different causes of pain and the anatomic injury; investigation is carried out using medium to high-frequency linear probes (9–14 MHz) according to the location and morphology of the patient. Sometimes also color Doppler examination may be useful. There are no known systematic studies reporting on the use of contrast agents or elastosonography in pubalgia.
Table 1.
Clinical classification of pubalgia.
| Possible causes of pubalgia |
|---|
|
Rectus adductor symphysis syndrome
This syndrome is the cause of about 40% of cases of pubalgia, conceptually linked to a functional overload of the symphysis pubis itself. It may cause damage to the insertions of the rectus muscles and the adductor muscles and involve the pubic bones and symphysis pubis.
The symphysis pubis is the point where all static and dynamic forces are loaded in the upright position. Any structural asymmetries (of the limbs or spine) or dynamic asymmetries (of the ground or shoes) therefore result in an excessive load on a particular anatomical structure, usually a tendon insertion. Static and dynamic compensation is provided by the insertions of the adductors and the rectus abdominis muscles (Fig. 1). The lateral forces are loaded mainly on the adductors while the compensating anteroposterior forces are loaded on the rectus. The right and left compartments “turn around” the symphysis pubis joint. The overuse of a tendon and its bone insertion leads to progressive injury which will affect both the tendon and the bone.
Fig. 1.
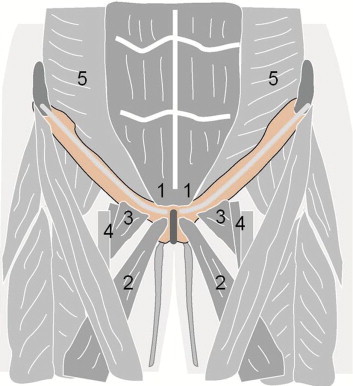
Anatomical diagram of the symphysis pubis and the tendon insertions. The rectus adductor syndrome particularly involves the insertion of the rectus abdominis (1) and the adductor longus (2). Pectineus (3), vessels (4), transverse (5).
Tendon injury initially causes swelling and later calcifications, tear and rupture. All these events are easily documented by US as reported in the literature [18]. US findings may involve both the adductors and the pubic insertion of the rectus abdominis.
The most frequently affected adductor is the adductor longus and more rarely the pectineus and the gracilis muscles, but US findings are similar (Fig. 2). The rectus abdominis are more often involved in sports requiring a constant anteroposterior adaptation (e.g. tennis). US findings are similar to those of the adductors (Fig. 3). Particularly the lateral portion of the tendon is involved at its insertion on to the pubic tubercle, where also the bundles of the adductor longus are joined.
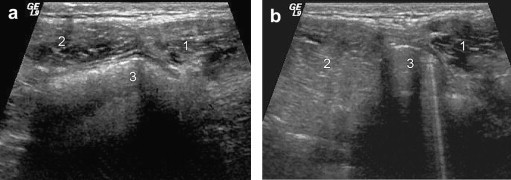
Fig 2.
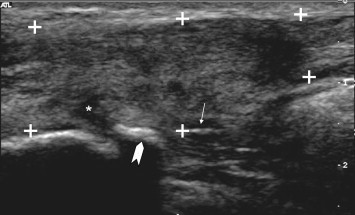
Rectus adductor syndrome. Adductor tendon injury: edema, calcification, rupture. This image of the proximal portion of the adductor longus (+ … +) shows diffuse hypoechoic enlargement and calcification of the tendon (arrow), periosteal detachment (arrowhead) in areas of hypoechoic focal tearing of fibers (∗).
Fig. 3.
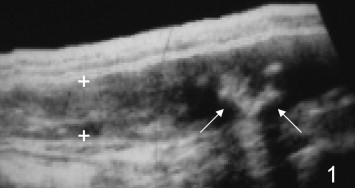
Rectus adductor syndrome. Tendon injuries of the rectus muscles. Sagittal scan of the distal insertion of the left rectus abdominis on the pubis (1) in a tennis player. Within the tendon of the rectus (+) there are irregular calcifications (arrows).
In the early stages, the bone injury at the level of the tendon insertion appears as a retraction of the bone margin with small gaps (Fig. 4) and enlargement of the rima of the symphysis pubis (Fig. 5). As the injury progresses there are osteophytosic reactions and arthritic deformation of the symphysis pubis. Irregular bone margins are detectable by US, but radiography is the gold standard. For a correct assessment of the pathology, a combined evaluation using US and radiography may be appropriate: US to assess the tendon injury and radiography to assess the bone margin.
Fig. 4.
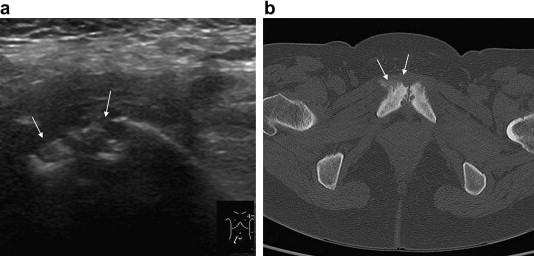
Alterations of the bone margins in rectus adductor symphysis syndrome. (a): the superior-anterior margin of the pubic bone on the right near the symphysis presents irregularities (arrows). (b): corresponding CT findings.
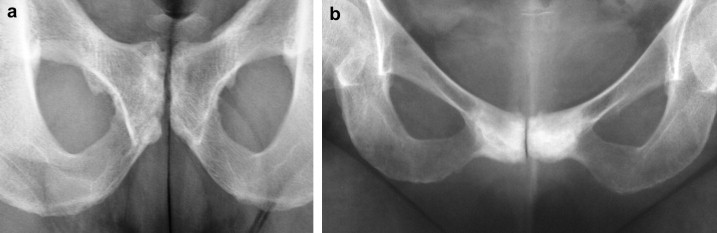
Fig. 5.
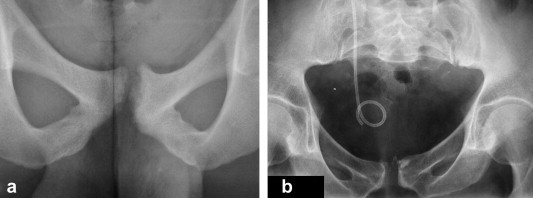
Enlargement of the symphysis pubis. (a): a postero-anterior projection for the study of the symphysis pubis showing retraction and deformation of the bone margins. (b): incidental finding during the study of a urethral pathology (right side) showing enlargement of the symphysis caused by pubalgia due to rectus adductor symphysis syndrome.
Progressive enthesopathy can lead to acute complications with tendon rupture and tendon detachment (Fig. 6). Reduced elasticity of the tendon due to chronic injury may also facilitate muscle distraction.
Fig. 6.
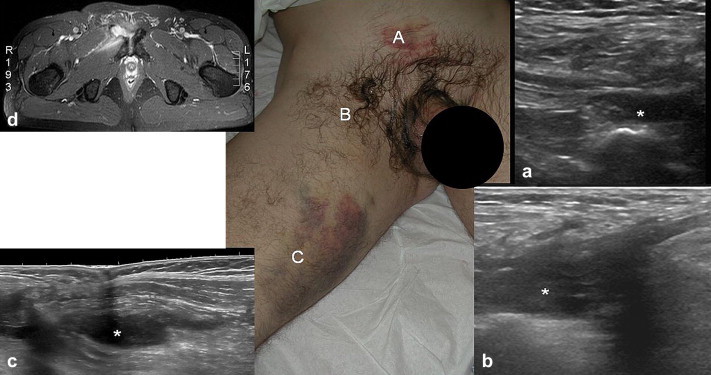
Complication of the rectus adductor syndrome. Partial detachment (∗) of the tendon of the rectus abdominis (a), partial tear (∗) of the adductor longus (b). Second degree distraction (∗) of adductor magnus (c) and corresponding MRI (d).
The symphysis pubis is a fibrocartilaginous joint; from bone maturation there may be a joint cavity or rather a form of joint recess which is visible at MRI T2-weighted sequences as a thin hyperintense line dividing the joint heads.
In pubalgia caused by overuse of the rectus adductor symphysis, the symphysis pubis may be involved as an extension of the above mentioned lesions of enthesopathy.
According to other authors [19,20], alterations in the symphysis pubis should be considered as an independent nosological entity. These lesions should certainly be considered of an independent etiology when they are linked to localized inflammatory diseases, infections and neoplastic pathologies; in these cases clinical and radiological findings will guide the diagnosis [21–23].
Independently of the etiology, the alterations that may be detected are related to changes in the bone margins of the symphysis, partly visible at US and partly at radiography as already mentioned. A second type of anatomical alteration regards the joint capsule. A recess may develop as a result of chronic wear and tear of the central fibrocartilage due to excessive load at the level of the pelvic ring, which is indicative of chronic micro-traumatic avulsions of the tendon fibers and sometimes of the inferior pubic ligament [19].
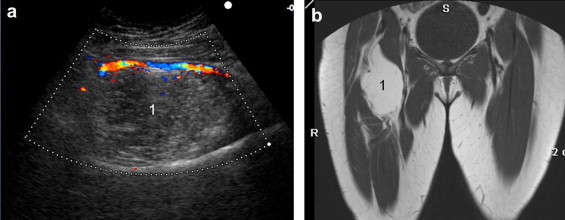
According to some authors, 70% of patients affected by pubalgia have an opening in the joint capsule, which can be demonstrated by MRI [24]. Only the most severe alterations of the joint capsule with periarticular fluid collections can be detected at US, and in this case US may be helpful for US guided diagnostic or therapeutic punctures [23] (Fig. 7). Finally, there may be a predominant involvement of the cancelous bone of the symphysis pubis joint heads.
Fig. 7.
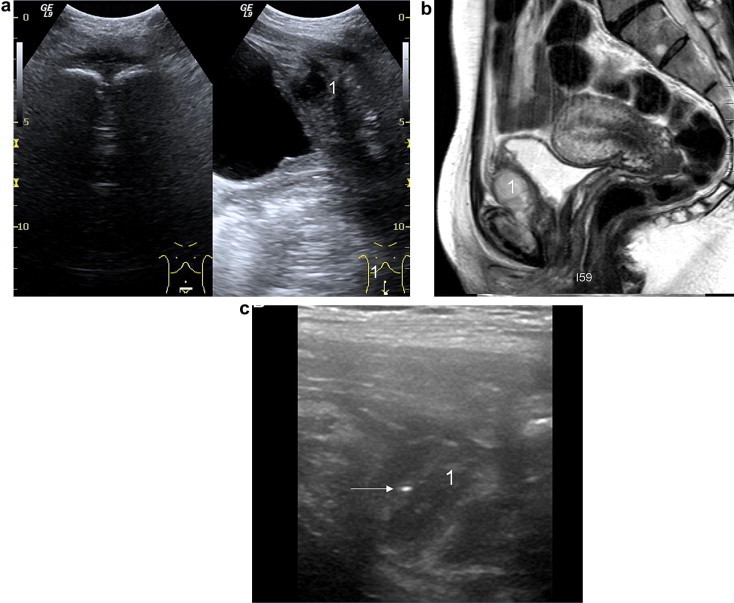
Pubic abscess in a female swimmer. (a): US image shows soft tissue swelling around the symphysis (1) and liquefactive necrosis between the symphysis and the bladder. (b): MRI confirming US diagnosis. (c): this image shows the needle tip (arrows) collecting a sample for bacterial cultivation.
MRI using sequences with high inherent contrast, such as spin echo T2-weighted sequences preferably associated with fat suppression, may show one or both pubic branches as an area with significantly increased signal (Fig. 8). This finding requires attention, as it may be associated with other pathological conditions, but it is strongly suggestive of cancelous bone due to overload [6,19]. In advanced cases this alteration can lead to enlargement of the cancelous bone and become visible also at radiography (Fig. 9).
Fig. 8.
Clearly increased signal from a cancelous area of the left pubic bone due to osteitis.
Fig. 9.
Osteitis pubis, radiography. Progressive trophic alterations caused by osteitis leading to the deformation of the symphysis pubis and progressive hardening of the bone structure. (a): early stage; (b): advanced stage.
Sports hernia
Pathologies affecting the inguinal canal were proposed by Nesovic in the 1970s as an explanation for pubalgia and arbitrarily called “sports hernia” in the absence of a true hernia, but several authors report a high percentage, ranging from 36% to 84%, of nonpalpable hernias in patients affected by persistent forms of pubalgia [25,26].
Joisting [27] defines “sportman’s hernia” as an injury which is common in athletes and in those who practise sports, “peculiar as it cannot be identified at clinical examination or using imaging techniques”, and he attributes this injury to a lesion of the transverse bundle. The definition “sports hernia” has recently been replaced by the term “groin disruption” [28]. This group includes all painful symptoms caused by anatomical defects of the posterior wall, which has no striated muscles [29]. Pathologies affecting the posterior wall of the inguinal canal can be evidenced at two instrumental examinations: herniography [10] and US [30,31].
However, there are also lesions of the anterior wall of the inguinal canal [1] that may occasionally involve pathologies of the nerve branches of the ilioinguinal and iliohypogastric nerves [1,26,28–32]. This second group includes also lesions of the oblique external aponeurosis, conjoint tendon, inguinal ligament and transverse bundle [11,28,33].
Sports hernia can be summarized as a myoaponeurotic defect of the abdominal wall [4,34] which can affect various structures. The anatomy of the abdominal wall in the pubic region may explain the possible causes of sports hernia. In particular, the peculiar relationship between the transverse muscle bundle and the rectus abdominis muscle (Fig. 10). In the presence of hypertrophy of the rectus muscle, which often occurs in athletes, a depression is developed in this anatomical site whose depth is bounded only by the transverse bundle. A weakness here might permit strangulation of a bowel loop between the transverse bundle and the rectus thereby causing pain.
Fig. 10.
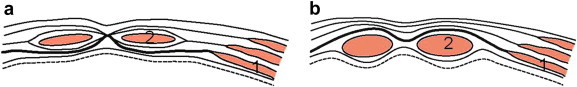
Diagram depicting the relationship between the transverse muscle bundles (1) and the muscle belly of the rectus (2). Above the transverse umbilical plane (a) the bundle arising from the transverse muscular epimysium joins the linea alba running behind the rectus, and below the umbilical line (b) it runs in front of the rectus.
Seen from the inside (Fig. 11) the abdominal wall presents other less resistant areas where bowel loops may be partially strangulated without actually forming a hernia (sports hernia versus occult hernia). Also changes in the structure of the deep as well as the superficial course of the inguinal canal caused by alterations in the external oblique, conjoint tendon, inguinal ligament and transverse bundle (Fig. 12) can cause pain due to sports hernia.
Fig. 11.
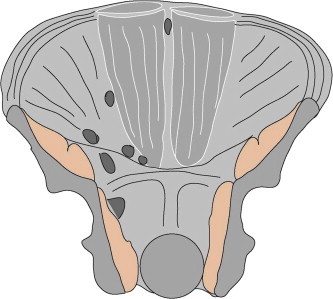
Diagram of the internal abdominal wall with the points of greatest parietal weakness.
Fig. 12.
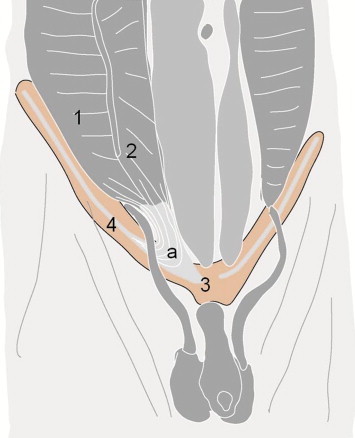
Diagram of the conjoint tendon. The conjoint tendon (a) arises from the union of the distal transverse bundles (1) and the internal oblique muscle (2) which are joined on the pubic tubercle (3) and the inguinal ligament (4).
US examination allows an accurate assessment of the relationship between the transverse muscle and the rectus abdominis muscle in normal conditions and in the presence of sports hernia. Investigation carried out in dynamic conditions (coughing and the Valsalva maneuver) particularly in tension and shortening of the rectus muscles in order to increase the “depression” between the transverse bundle and the muscle belly of the rectus abdominis muscle affected by hypertrophy, permits depiction of the partly strangulated bowel loop between the rectus and transverse bundles (Fig. 13). This type of alteration can be demonstrated only by dynamic US investigation.
Fig. 13.
Normal and dynamic US findings showing sports hernia. Transverse scan in the right iliac fossa at rest (a) and during contraction of the abdominal muscles and partial flexion (b). (b) shows the increased diameter of the rectus abdominis (1) and of the lateral abdominal muscles (2); the bowel loop (3) is "pinched" between the two muscles.
The literature shows US images of hernia in the inguinal canal and reports on the essential role of US in surgical decisions [35]. It is in fact possible that an athlete has a simple inguinal hernia.
At US examination it is much more difficult to identify alterations in the conjoint tendon or inguinal ligament, which are often affected in pubalgia simulating hernia pain. However, the insertional intersection of the inguinal ligament, the conjoint tendon, the lateral bundles of the rectus abdominis and adductor longus on the pubic tubercle should be kept in mind: a lesion in such a location is generally identifiable by US which will show the alterations described for the rectus adductor syndrome. Diagnostic possibilities of MRI in this location depend on the altered intersection of these structures on the bone margin.
In the presence of symptoms suggestive of sports hernia, some authors propose surgical treatment, usually using the Nesovic technique; others claim that surgery does not significantly improve sports hernia [36]. Undoubtedly, numerous surgical techniques and variants are proposed or carried out during surgery. US is performed in the postsurgical follow up to document elimination of the hernia diagnosed before surgery. Sometimes sports hernia is still present, but in case of successful surgery (Fig. 14) it is eliminated and US can show the reinforcement positioned by the surgeon in the area of wall weakness.
Fig. 14.
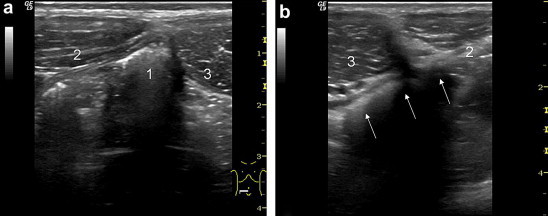
Professional footballer: sports hernia before surgery (a) and after surgery (b). Axial scans in the right (a) and left (b) iliac fossa. Strangulation of the intestinal loop (1) is visible between the transverse (2) and rectus (3) muscles while (b) shows the surgical “net” (arrows) protecting the space between the transverse and the rectus muscles.
Locoregional pathologies
About 20% of cases of pubalgia are caused by pain in the pubic region due to musculoskeletal or genitourinary disorders. Skeletal muscle pathologies can affect the hip joint or the proximal insertion of the anterior (rectus femoris, iliopsoas) or posterior (hamstring) hip muscles. US examination can usually identify disorders of the rectus muscle insertion and pathologies of the iliopsoas. The psoas may be affected by infectious or inflammatory diseases, but also by dynamic pathologies which may cause pubalgia in athletes. Impingement of the iliopsoas muscle (Fig. 15) may cause pubalgia particularly in athletes involved in sports which require strong flexion of the thigh such as pole vault take-off, or in the presence of iliopsoas bursitis (Fig. 16).
Fig. 15.
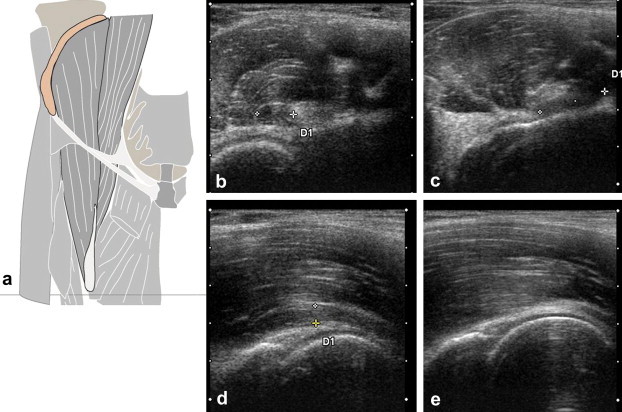
Iliopsoas impingement at US follow up. (a): diagram of the relationships between the ileum and the psoas muscles. (b) and (c): axial sections. (d) and (e): sagittal sections of the inguinal region. (b) and (d): with flexed thigh; (c) and (e): with extended leg. When the thigh is flexed the psoas tendon is visible (+ … +); it is inserted between the ileum and the underlying bone margin, and it moves medially (c) when the thigh is extended.
Fig. 16.

Ileopectineal bursitis. Sagittal scan of the right hip joint showing enlargement with irregular margins of the ileopectineal bursa (1).
Musculoskeletal pathologies involving compression of the nerves radiating to the groin should be kept in mind, such as the Maigne syndrome [37] (or the dorsolumbar hinge syndrome) as well as compression syndromes involving the ilioinguinal, femoral cutaneous, femoral, genitofemoral and obturator nerve branches [38]. In some cases US examination can exclude local pathologies thus directing the study towards other areas such as the spine. In other cases US may show the alteration causing local irritation of the nerve (Fig. 17).
Fig. 17.
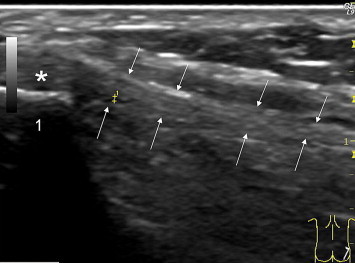
Enthesitis of the iliotibial tract and the transverse bundle which causes ilioinguinal nerve irritation. US shows enlargement, and the insertion (∗) on the tubercle of the iliac crest (1) of the iliotibial band (arrows) appears hypoechoic in the portion where it merges with the gluteal fascia. US also shows the initial tear of the tendon structures (+ .. +). The symptoms in the ilioinguinal nerve region are caused by irritation of the nerve passing near the enthesopathy.
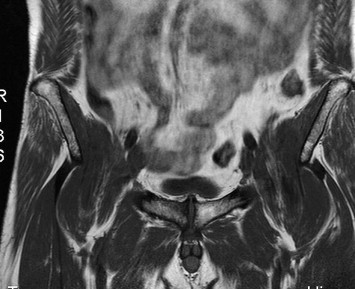
Chronic pathologies may also occupy the locoregional space causing pubalgia, such as lipomas (Fig. 18) or local vascular alterations which are easily depicted at US examination.
Fig. 18.
Lipoma in the adductor muscle. (a): parasagittal scan of the anteromedial root of the right thigh showing a well defined solid mass (1) displacing the vessels. This finding is suggestive of lipoma as confirmed by MRI (b).
The male and female urogenital tract often presents subacute pathologies misdiagnosed as pubalgia, or pubalgia is clinically interpreted as symptoms linked to the urogenital tract. Undoubtedly, clinical symptoms are important in this diagnostic context, however US often provides a specific diagnosis. Prostate, testicular or female urethral diseases are the most common causes and these conditions are all well explored using US as reported in the literature. Pubalgia may also be linked to particular circumstances due to a combination of genital, hernia and inguinal anomalies such as the presence of endometriosis in the inguinal canal (Fig. 18).
Conclusions
Despite the considerable confusion over the definition of pubalgia and sports hernia it seems that all authors are oriented towards considering pubalgia as a situation of discomfort or chronic pain that affects a significant number of people who practise physical activity with prevalence linked to some sports. Patients with pubalgia often present alterations in the symphysis pubis or in the tendon insertions. Sometimes a weakness or defect of the abdominal wall is detected and sometimes the patient presents with adjacent pathologies radiating pain to the pubic area. US examination should be considered as a first-line screening method in pubalgia in close correlation with clinical examination in order to document possible anatomical alterations and to guide subsequent diagnostic workup using radiography and MRI. US examination is furthermore useful for monitoring the evolution of diagnosed alterations linked to pubalgia.
Conflict of interest statement
The authors have no conflict of interest to declare.
Appendix. Supplementary data
The following are the Supplementary data related to this article:
References
- 1.Irshad K., Feldman L.S., Lavoie C., Lacroix V.J., Mulder D.S., Brown R.A. Operative management of “hockey groin syndrome”: 12 years of experience in national hockey league players. Surgey. 2001;130:759–764. doi: 10.1067/msy.2001.118093. [DOI] [PubMed] [Google Scholar]
- 2.Puig P.L., Trouve P., Savalli L. Pubalgia: from diagnosis to return to the sport field. Ann Readapt Med Phys. 2004;47:356–364. doi: 10.1016/j.annrmp.2004.05.003. [DOI] [PubMed] [Google Scholar]
- 3.Zoga A.C., Kavanagh E.C., Omar I.M., Morrison W.B., Koulouris G., Lopez H. Athletic pubalgia and the “sports hernia”: MR imaging findings. Radiology. 2008;247:797–807. doi: 10.1148/radiol.2473070049. [DOI] [PubMed] [Google Scholar]
- 4.Vidalin H., Neouze G., Petit Brunet-Guedi E. Prise en charge chirurgicale des pubalgies du sportif. J Traumatol Sport. 2004;21:166–173. [Google Scholar]
- 5.Campanelli G. Pubic inguinal pain syndrome: the so-called sports hernia. Hernia. 2010;14:1–4. doi: 10.1007/s10029-009-0610-2. [DOI] [PubMed] [Google Scholar]
- 6.Barile A., Erriquez D., Cacchio A., De Paulis F., Di Cesare E., Masciocchi C. Groin pain in athletes: role of magnetic resonance. Radiol Med. 2000;100:216–222. [PubMed] [Google Scholar]
- 7.Berger A. Approches diagnostiques et thérapeutique de la pubalgie du sportif. Thèse Med Genève. 2000 [Google Scholar]
- 8.Durey A., Rodineau J. Les lésions pubiennes des sportif. Ann Méd Phys. 1976;9:282–291. [Google Scholar]
- 9.Durey A. Aspects cliniques de la pubalgie du sportif. J Traumatol Sport. 1984;1:46–50. [Google Scholar]
- 10.Ekstrand J., Hilding J. The incidence and differential diagnosis of acute groin injuries in male soccer players. Scan J Med Sci Sports. 1999;9:98–103. doi: 10.1111/j.1600-0838.1999.tb00216.x. [DOI] [PubMed] [Google Scholar]
- 11.Gilmore J. Groin pain in the soccer athlete: fact, fiction and treatment. Clin Sports Med. 1998;17:787–793. doi: 10.1016/s0278-5919(05)70119-8. [DOI] [PubMed] [Google Scholar]
- 12.Le Gall F. La pubalgie du sportif. A propos de 214 cas. Thèse en médicine. Université de Rennes, 1993.
- 13.Volpi P. La pubalgie: notre experience. J Traumatol Sport. 1992;9:53–55. [Google Scholar]
- 14.Bisciotti G.N. La pubalgia dello sportivo. Inquadramento clinico e strategie terapeutiche. Calzetti e Mariucci Editori Perugia. 2009 [Google Scholar]
- 15.Jarvinen M., Orava S., Kuyala M. Groin pain (Adductor syndrome) Oper Tech Sport Med. 1997;5:133–137. [Google Scholar]
- 16.Gal C. In: La pubalgia. Prevenzione e trattamento. Società Stampa Sportiva, editor. 2000. Roma. [Google Scholar]
- 17.Benazzo F., Mosconi M., Zanon G., Bertani B. Groin pain. J Sports Traumatol Rel Res. 1999;21(1):30–40. [Google Scholar]
- 18.Hölmich P., Bachmann Nielsen M. Ultrasound findings in adductor related groin pain. Ultraschall Med. 2006;27:509–511. doi: 10.1055/s-2006-958487. [DOI] [PubMed] [Google Scholar]
- 19.Faletti C. La pubalgia nello sport: alcune cause infrequenti. II Medico Sportivo. 2009;9:2. [Google Scholar]
- 20.Fricker P.A., Taunton J.E., Amman W. Osteitis pubis in athletes. Infection, inflammation or injury? Sports Med. 1991;12:266–279. doi: 10.2165/00007256-199112040-00005. [DOI] [PubMed] [Google Scholar]
- 21.Baril L., Caumes E., Bricaire F. Pubic pain after a marathon. Lancet. 1998;351:642. doi: 10.1016/S0140-6736(97)10470-6. [DOI] [PubMed] [Google Scholar]
- 22.Durey A. Masson; Paris: 1985. Modifications radiologiques microtraumatiques du pubis. Micro-traumatologie du sport. pp. 185–92. [Google Scholar]
- 23.Ross J.J., Hu L.T. Septic arthritis of the pubic symphysis: review of 100 cases. Medicine (Baltimore) 2003;82:340–345. doi: 10.1097/01.md.0000091180.93122.1c. [DOI] [PubMed] [Google Scholar]
- 24.Brennan D., O’Connell M.J., Ryan M., Cunningham P., Taylor D., Cronin C. Secondary cleft sign as a marker of injury in athletes with groin pain: MR image appearance and interpretation. Radiology. 2005;235:162–167. doi: 10.1148/radiol.2351040045. [DOI] [PubMed] [Google Scholar]
- 25.Ekberg O. Inguinal herniography in adults: technique, normal anatomy, and diagnostic criteria for hernias. Radiology. 1981;138:31–36. doi: 10.1148/radiology.138.1.7455093. [DOI] [PubMed] [Google Scholar]
- 26.Srinivasan A., Schuricht A. Long-term follow-up of laparoscopic preperitoneal hernia repair in professional athletes. J Laparoendosc Adv Surg Tech. 2002;12:101–106. doi: 10.1089/10926420252939600. [DOI] [PubMed] [Google Scholar]
- 27.Joesting D.R. Diagnosis and treatment of sportsman’s hernia. Curr Sports Med Rep. 2002;1:121–124. doi: 10.1249/00149619-200204000-00010. [DOI] [PubMed] [Google Scholar]
- 28.Morelli V., Smith V. Groin injuries in athletes. Am Fam Physician. 2001;64:1405–1414. [PubMed] [Google Scholar]
- 29.Fon L.J., Spence R.A. Sportsman’s hernia. Br J Surg. 2000;87:545–552. doi: 10.1046/j.1365-2168.2000.01462.x. [DOI] [PubMed] [Google Scholar]
- 30.Bradley M., Morgan D., Pentlow B., Roe A. The groin hernia- an ultrasound diagnosis? Ann R Coll Surg Engl. 2003;85:178–180. doi: 10.1308/003588403321661334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Orchard J.W., Read J.W., Neophyton J., Garlick D. Groin pain associated with ultrasound finding of inguinal canal posterior wall deficiency in Australian rules footballers. Br J Sports Med. 1998;32:134–139. doi: 10.1136/bjsm.32.2.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ziprin P., Williams P., Foster M.E. External oblique aponeurosis nerve entrapment as a cause of groin pain in the athlete. Br J Surg. 1999;86:566–568. doi: 10.1046/j.1365-2168.1999.01081.x. [DOI] [PubMed] [Google Scholar]
- 33.Lynch S.A., Renström P.A. Groin injuries in sport: treatment strategies. Sports Med. 1999;28:137–144. doi: 10.2165/00007256-199928020-00006. [DOI] [PubMed] [Google Scholar]
- 34.Albers S.L., Spritzer C.E., Garrett W.E., Jr., Meyers W.C. MR findings in athletes with pubalgia. Skeletal Radiol. 2001;30:270–277. doi: 10.1007/s002560100335. [DOI] [PubMed] [Google Scholar]
- 35.Lorenzini C., Sofia L., Pergolizzi F.P., Trovato M. The value of diagnostic ultrasound for detecting occult inguinal hernia in patients with groin pain. Chir Ital. 2008;60:813–817. [PubMed] [Google Scholar]
- 36.Fitzgibbons R.J., Jr., Giobbie-Hurder A., Gibbs J.O., Dunlop D.D., Reda D.J., McCarthy M., Jr. Watchful waiting vs repair of inguinal hernia in minimally symptomatic men: a randomized clinical trial. JAMA. 2006;295:285–292. doi: 10.1001/jama.295.3.285. [DOI] [PubMed] [Google Scholar]
- 37.Maigne R. Le syndrome de la charnière dorso-lombaire. Lombalgies basses, douleurs pseudo-viscérales, pseudo-douleurs de hanche, pseudo- tendinite des adducteurs. Sem Hôp Paris. 1981;57:545–554. [PubMed] [Google Scholar]
- 38.Bradshaw C., McCrory P., Bell S., Brukner P. Obturator nerve entrapment. A cause of groin pain in athletes. Am J Sports Med. 1997;25:402–408. doi: 10.1177/036354659702500322. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


