Abstract
Ultrasound (US) has always had a relatively limited role in the evaluation of the hip due to the deep location of this joint. However, many hip diseases are well detectable at US, but before approaching such a study it is necessary to be thoroughly familiar with the normal anatomy and related US images. The study technique is particularly important as optimization of various parameters is required, such as probe frequency, focalization, positioning of the probe, etc. Also the patient’s position is important, as it varies according to the area requiring examination. For the study of the anterior structures, the patient should be in the supine position; for the medial structures, the leg should be abducted and rotated outward with the knee flexed; for the lateral structures, the patient should be in the controlateral decubitus position; for the posterior structures the patient must be in the prone position. US study of the hip includes assessment of the soft tissues, tendons, ligaments and muscles, and also of the bone structures, joint space and serous bursae. The purpose of this article is to review the normal anatomy of the hip as well as the US anatomy of this joint.
Keywords: Hip, Hip anatomy, Ultrasound, Hip ultrasound
Sommario
L’ecografia ha sempre avuto un ruolo piuttosto limitato nella valutazione dell’anca, per la sede profonda di quest’articolazione. In realtà molte patologie dell’anca sono ben evidenziabili con l’ecografia, tuttavia, prima di affrontare lo studio delle patologie è necessaria un’accurata conoscenza dell’anatomia normale e dell’anatomia ecografica.
È poi particolarmente importante la tecnica di esecuzione che richiede l’ottimizzazione di vari parametri, frequenza della sonda, focalizzazione, inclinazione della sonda rispetto alle strutture in esame, ecc., oltre alla posizione del paziente che varia a seconda dei distretti esaminati. Per le strutture anteriori il paziente è supino, per le mediali la gamba è abdotta e ruotata verso l’esterno, con ginocchio flesso, per le laterali il paziente è in decubito sul fianco controlaterale, per le posteriori è prono.
Lo studio ecografico dell’anca comprende la valutazione di tessuti molli, tendini, legamenti e muscoli, ma anche delle strutture ossee dello spazio articolare e delle borse sierose.
Scopo della presente articolo è rivalutare l’anatomia normale dell’anca e l’anatomia ecografica di questa articolazione.
Introduction
Before 1970, radiological examination of the hip was based on conventional radiography, stratigraphy, and scintigraphy. Later, computed tomography (CT) and magnetic resonance (MR) imaging were introduced [1,2], but due to the deep location of the hip joint, ultrasound (US) examination has always had a relatively limited role in the assessment of hip pathologies. However, many hip diseases are well detectable at US [3–5] provided that the US operator is familiar with the normal anatomy as well as the US anatomy of this joint, and that the examination is performed accurately and compared to previous diagnostic imaging results, if available. US study of the hip includes assessment of the soft tissues, tendons, ligaments and muscles, and also of the bone structures and joint spaces [6–8].
The purpose of this article is to describe the normal hip anatomy, US examination technique and US appearance of the normal hip anatomy. To facilitate the understanding of these US images, they are compared to more panoramic MR images of the same structures.
Normal anatomy
The hip joint is a “ball-and-socket” type joint that allows a good stability at the expense of a limited range of motion. It is composed of the following structures:
-
1.
Bone structures (femoral head and acetabulum),
-
2.
Fibrocartilaginous structures (acetabular labrum),
-
3.
Cartilage layers covering the hip joint,
-
4.
Capsular-ligamentous structures,
-
5.
Synovial joint,
-
6.
Muscles and tendons,
-
7.
Synovial bursae,
-
8.
Neurovascular structures.
Bone structures
The acetabulum is a cup-shaped cavity located on the outside of the pelvis into which the ball-shaped head of the femur fits, and it is surrounded by a circular bone flap called the acetabular edge. Of the inner surface of the acetabulum, only the most peripheral portion, i.e. the lunate-surface, is used in the articulation, while the central portion, the acetabular pit, accommodates the round ligament extended between the acetabulum and the femoral head, surrounded by adipose tissue and vascular structures.
The femoral head is round and in the center of the head there is a small depression called the fovea capitis femoris to which the round ligament is attached. It is supported by the anatomical neck which is situated at an angle of about 130° to the axis of the femoral shaft in the coronal plane. At the base of the neck there are two trochanters (the greater trochanter and the lesser trochanter) where the periarticular muscles are inserted.
Fibrocartilaginous structures
The acetabular labrum is an axial section of the triangular fibrocartilage whose base is inserted on to the acetabular edge. It performs three main functions: it inserts the capsular-ligamentous structures of the joint, increases the concavity of the acetabular fossa and increases the contact area with the femoral head.
Cartilage layer covering the hip joint
The layers of articular cartilage cover the entire joint surface with the exception of the acetabular fossa and the fovea capitis femoris. The femoral head is covered by cartilage tissue up to the passage between the femoral head and neck.
Capsular-ligamentous structures
The articular capsule is a fibrous sheath. Proximally it inserts on to the edge of the acetabulum and on to the acetabular labrum and distally on to the intertrochanteric line (in front) and between the third medium and distal third of the femoral neck (behind).
Three peripheral thickenings of the capsule form the most important ligaments:
-
•
The iliofemoral ligament = originates below the anterior-inferior iliac spine and inserts on to the femur at the greater trochanter and on to the intertrochanteric line;
-
•
The pubofemoral ligament = originates from the pubic portion of the acetabular edge and from the ileopectineal eminence and blends with the joint capsule;
-
•
The ischiofemoral ligament = its fibers span from the ischium below and behind the acetabular edge and attach to the intertrochanteric line.
The round ligament is located centrally between the acetabular fossa and the fovea capitis of the femoral head.
Synovial joint
The synovial joint lines the inner surface of the joint capsule and forms a complete sheath by surrounding the round ligament.
Muscles and tendons
The muscles and tendons around the hip can be divided into 4 groups on the basis of their anatomical position: the anterior, medial, lateral and posterior structures.
At US the anterior and lateral myotendinous structures are generally easier to distinguish than the posterior groups.
Anterior group
The rectus femoris muscle arises by a short strong tendon from the anterior-inferior iliac spine (the direct tendon) and by another tendon from the superolateral margin of the acetabulum (the indirect tendon). The indirect tendon travels with the central aponeurosis whereas the direct tendon travels with the superficial fascia. The muscle belly travels at the distal third of the thigh in the superficial tendinous lamina of the quadriceps tendon.
The psoas muscle arises from the lateral surface of the spine between the lower margin of the 12th thoracic vertebra and the upper margin of the 5th lumbar vertebrae. Running downwards it becomes thinner and enters the thigh by passing under the inguinal ligament. It is separated from the pubis and the hip joint capsule by a large serous bursa before inserting on to a strong tendon on the medial side of the lesser trochanter.
The iliacus muscle is situated next to the psoas. It arises from the upper portion of the iliac fossa and also from the region of the anterior-inferior iliac spine and from the sacroiliac joint. Running downwards it passes under the inguinal ligament. It continues under the sartorius and rectus femoris muscles to insert on to the lateral margin of the psoas tendon.
The pectineus muscle arises from the pectineal line of the pubis. The fibers pass downwards to be inserted on to the lesser trochanter and the linea aspera.
The sartorius muscle is the longest muscle in the human body. It arises from the anterior-superior iliac spine and runs downwards, crosses the rectus femoris muscle and runs down along the inner thigh. It becomes aponeurotic in the very last portion and inserts on to the proximal tibial metaphysis where it joins the gracilis and semitendinosus muscle tendons to form the conjoined ‘goose’s foot” tendon.
Medial group
The adductor longus muscle arises by a strong tendon from the pubis; it travels downwards and inserts into the middle third of the femur at the vastus medialis muscle.
The adductor brevis muscle arises from the pubis. It is situated under the origin of the adductor longus muscle, travels downwards and inserts by an aponeurosis on to the side of the pectineus muscle below the lesser trochanter.
The adductor magnus muscle arises from the ischium and from the lower surface of the ischial tuberosity. It travels downwards on the side and is inserted by a short aponeurosis to the lower third of the linea aspera.
The gracilis muscle is a straplike muscle that originates by an aponeurosis from the ischium-pubic branch and the body of the pubic bone. Running downwards it becomes thinner and ends in a cylindrical tendon along with the tendons of the sartorius and semitendinosus muscles on the medial surface of the tibia.
Lateral group
The gluteus minimus muscle arises from the lateral surface of the iliac wing, crosses the hip joint and inserts on to the anterior facet of the greater trochanter.
The gluteus medius muscle arises from the lateral surface of the iliac wing, and from here it travels downwards to insert on to the medial and posterior surface of the greater trochanter.
The gluteus maximus muscle arises from the external surface of the iliac wing and the sacrum; it runs downwards on the side and ends at the posterior margin of the greater trochanter and fasciae latae.
The tensor fasciae latae muscle arises at the level of the anterior-superior iliac spine; it travels downwards and just below the greater trochanter it joins the iliotibial tract, a large aponeurotic fascia.
Posterior group
The semimembranosus muscle arises from the ischial tuberosity by a strong tendon; while moving downwards the tendon expands and becomes a membrane (hence the name). The muscle belly travels downwards along the posteromedial surface of the thigh to insert on to the proximal tibial epiphysis.
The semitendinosus muscle arises from the ischial tuberosity by a short tendon in common with the long head of the biceps femoris. Its muscle bundles end in a long, thin tendon that inserts on to the medial surface of the tibia below the tendon of the gracilis.
The long head of the biceps femoris muscle arises, as already mentioned, from the ischial tuberosity by a tendon in common with the semitendinosus muscle. It then runs laterally downwards to the distal portion of the thigh to join the short head which originates from the posterior surface of the femur. The strong distal tendon which joins the two muscle heads is inserted on to the lateral surface of the fibular head.
Synovial bursae
Among the bursae involved in the hip articulation, the iliopsoas bursa and the peritrochanteric bursae have a particularly important role from a clinical point of view.
The iliopsoas bursa is located between the iliopsoas myotendinous junction and the iliopsoas tendon and the hip joint capsule. In 15% of cases it communicates with the coxofemoral joint through a foramen located between the ileofemoral and pubofemoral ligaments.
The peritrochanteric bursae are located in the peritrochanteric region and are divided into:
-
•
large, medium and small. They are located between the gluteus maximus, gluteus medius and gluteus minimus tendons and the greater trochanter.
Neurovascular structures
The neurovascular structures mainly include:
-
a)
the femoral vessels (artery and vein);
-
b)
the nerves: the femoral cutaneous nerves and femoral-sciatic nerve.
Distal to the inguinal ligament there is a pseudo-triangular area (the femoral triangle) bounded by connective tissue:
-
•
medially by the adductor longus;
-
•
laterally by the sartorius muscle;
-
•
superficially by the inguinal ligament;
-
•
deeply by the ileopubic branch.
This region contains the common femoral vein (medial), the common femoral artery (laterally) and the femoral nerve (more lateral than the femoral vessels) and the inguinal lymph node stations.
At the hip joint, the common femoral artery is separated from the femur head by the iliopsoas tendon and corresponding bursa. Below the common femoral artery the deep femoral artery arises and gives origin to the medial circumflex artery.
The small femoral cutaneous nerve travels more laterally than the femoral nerve, emerges from the lateral profile of the psoas muscle and crosses the iliacus muscle passing through an osteofibrous channel formed by a small incisure in the more lateral portion of the inguinal ligament and the anterior-superior iliac spine.
The sciatic nerve penetrates the pelvis in the posterior region of the hip through the greater sciatic foramen and enters the gluteal region running deeply along the lower edge of the piriformis muscle. From here, the nerve continues under the gluteus maximus muscle, between the greater trochanter and the ischial tuberosity, and over the internal obturator muscle, bounded by the femur and adductor magnus muscle.
Anatomy and ultrasound study technique
At US examination, the patient’s position varies according to the structures to be examined.
For the study of the
-
•
Anterior structures (Figs. 1–4), the patient should be in the supine position;
-
•
Medial structures (Fig. 5), the leg should be abducted, rotated outward with the knee flexed;
-
•
Lateral structures (Figs. 6 and 7), the patient should be in the controlateral decubitus position;
-
•
Posterior structures, the patient should be in the prone position.
Fig. 1.
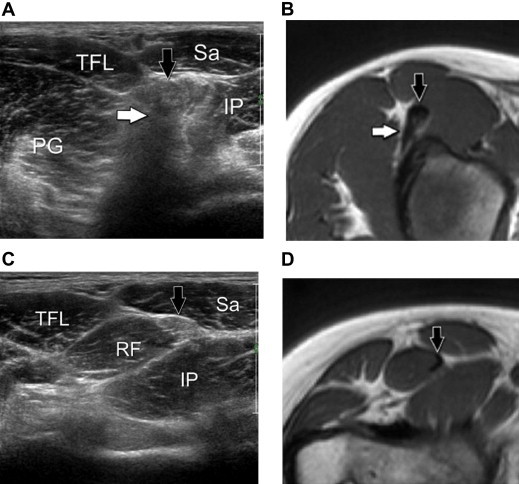
(A, C) US scans obtained at the proximal tendon of the rectus femoris (A) and at the proximal myotendinous junction (B). (B, D) T1-weighted MRI images corresponding to the US scans. US provides visualization of the direct tendon (black arrows) and the indirect tendon (white arrows) of the rectus femoris. In A, the posterior shadow cone of the tendon is an indirect consequence of its obliquity. At the rectus femoris myotendinous junction (DA), it is inserted on to the lateral surface of the direct tendon. TFL: tensor fasciae latae muscle; Sat: sartorius muscle; IP: iliopsoas muscle; PGL: small gluteal muscle.
Fig. 2.
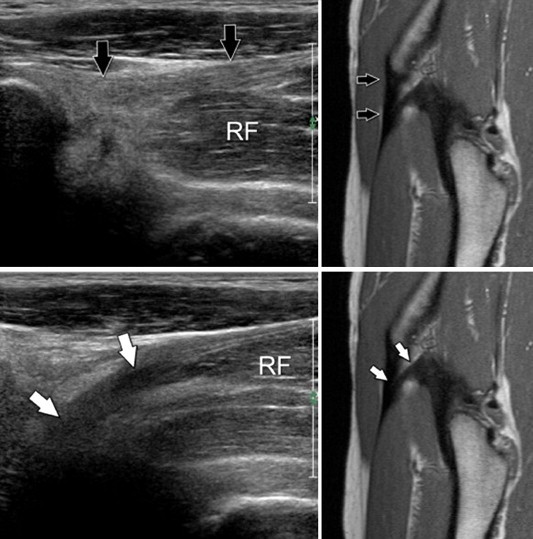
(US images on the left): US Sagittal scan obtained at the direct tendon (black arrows) and indirect tendon (white arrows) of the rectus femoris muscle (RF). The image on the top was obtained by scanning at the medial level as compared to the image below. (MR images on the right): T1-weighted MR image corresponding to the US scans. The direct tendon shows a homogeneous and hyperechoic appearance. Its insertion on to the anterior-inferior iliac spine is well visible on the US image. In physiological conditions the tendon is thicker just before insertion. In B, the indirect tendon appears hypoechoic because of anisotropy.
Fig. 3.
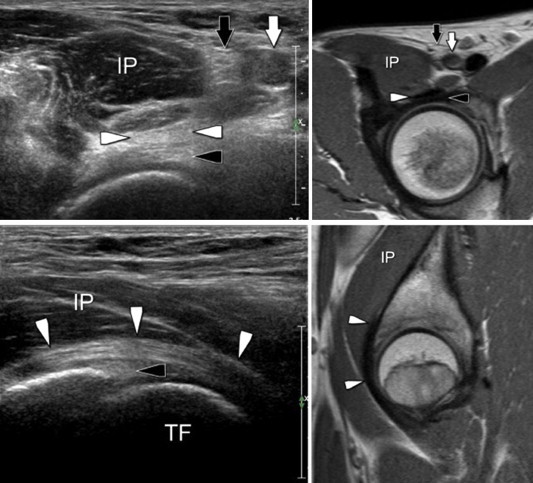
(US images on the left): Axial US scan obtained at the anterior surface of the coxofemoral joint (above). Sagittal US scan obtained at the tendon of the iliopsoas muscle (bottom). (MR image on the right): T1-weighted MR images corresponding to the US scans. US provides visualization of the acetabular labrum. The labrum appears as a hyperechoic homogeneous structure (black arrowheads). The tendon of the iliopsoas muscle runs in front of the labrum (white arrowheads); note the hyperechoic and fibrillar internal structure. IP: iliopsoas muscle; TF: femoral head; black arrow: femoral nerve; white arrow: common femoral artery.
Fig. 4.
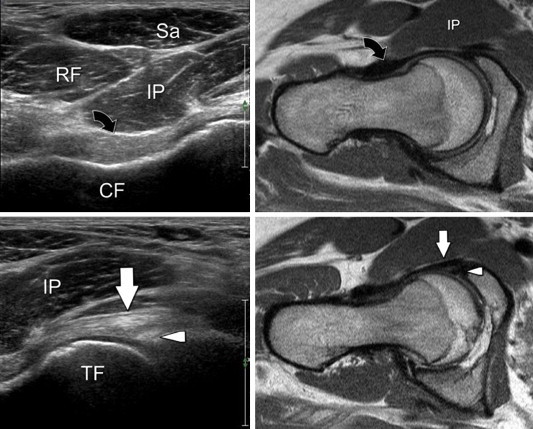
(US images on the left): US oblique axial scans obtained at the femoral neck (top) and the femoral head (below). (MR images on the right): T1-weighted MR images corresponding to the US scans. The ileofemoral ligament appears as a hyperechoic band (curved arrow) in front of the femoral neck (CF). C, D: at the femoral head, the ligament appearing as a fibrillar structure (white arrow) is inserted on to the front edge of the cup near the anterior acetabular labrum (arrowheads). IP: iliopsoas muscle; Sa: sartorius muscle; RF: rectus femoris.
Fig. 5.
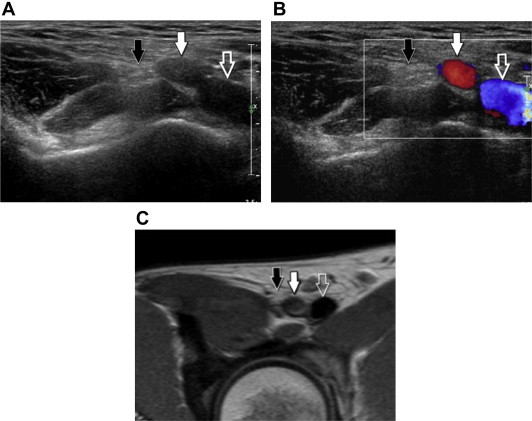
(A, B): US scans obtained at the femoral vessels. (C): T1-weighted MR image corresponding to the US scans. US provides visualization of the common femoral artery (white arrows), the common femoral nerve traveling outside the artery (black arrows) and the common femoral vein inside (empty arrow).
Fig. 6.
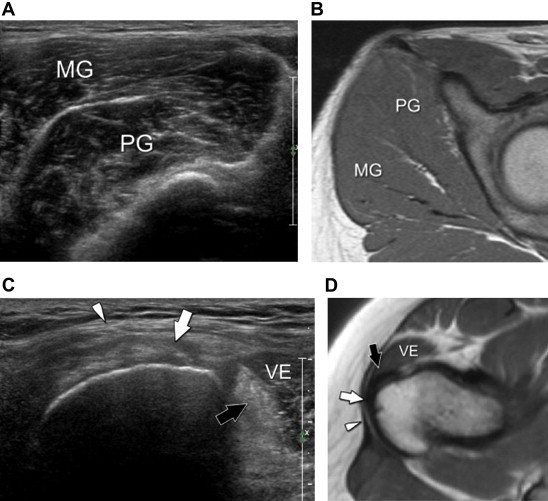
(A, C): axial US scans carried out at the gluteus muscles and their insertion on to the greater trochanter. (B, D): T1-weighted MR images corresponding to the US scans. US provides visualization of the gluteus medius muscle (MG) and the deeper located gluteus minimus muscle (PG). The image obtained at the level of the tendons provides distinction between the tendon of the gluteus minimus muscle (black arrow) traveling in front of the tendon of the gluteus medius muscle (white arrow). Arrowhead: fasciae latae. VE = external vastus muscle (quadriceps muscle).
Fig. 7.

(US images on the left): Coronal US scans carried out at the lateral surface of the hip. (MR images on the right): T1-weighted MR images corresponding to the US scans. • Photo, top = anterior image shows the tendon of the gluteus minimus muscle (black arrow) that inserts on to the lateral surface of the greater trochanter. Arrowhead: fasciae latae. • Photo, mid = image obtained at the middle third of the greater trochanter shows the anterior tendon of the gluteus medius muscle (white arrow). Arrowhead: fasciae latae. • Photo, bottom = posterior image shows the posterior tendon of the gluteus medius muscle (empty arrow) which inserts on to the apex of the greater trochanter.
The examination includes axial, sagittal and oblique scans usually starting with a study of the anterior region of the hip followed by the study of the medial, lateral and posterior regions.
Study of the anterior hip region
Sagittal oblique scans: using the femoral head as a landmark the anterior synovial recess is identified; in physiological conditions it is virtual, whereas it is distended by anechoic fluid in the presence of joint effusion.
The fibrocartilaginous lip, which appears as a hyperechoic triangular structure, and the acetabulum (Fig. 3) are situated proximal to the synovial recess. The iliofemoral ligament is situated on the surface of the lip (Fig. 4). The iliopsoas muscle is characterized by an eccentric, posteromedial tendon and is situated in front of the femoral head and the joint space. Like the synovial recess the iliopsoas bursa, located between the tendon and joint capsule, cannot be assessed under physiological conditions.
Axial scans are extended in the cranio-caudal direction:
-
a)
from the anterior-superior iliac spine,
-
b)
from the anterior-inferior iliac spine to,
-
c)
the proximal third of the thigh.
-
a)
At the level of the anterior-superior iliac spine, the tendon of the sartorius muscle can be seen in the middle, and the tendon of the tensor fasciae latae can be seen on the side. From the insertion, the sartorius muscle travels medially and crosses the rectus femoris, whereas the tensor fasciae latae remains lateral running in front of the vastus lateralis.
The lateral cutaneous femoral nerve is situated at the insertion of the inguinal ligament on to the anterior-superior iliac spine; it has the appearance of normal fascicular nerves.
The nerve is small and not always easily identified. The neurovascular bundle (Fig. 5) is situated at the mid-section of the iliopsoas muscle; it consists of the femoral nerve, which is the most lateral structure, the common femoral artery and the common femoral vein, which is situated medial to the artery. Unlike the artery, the femoral vein collapses if it is compressed with the US probe. On the contrary the Valsalva maneuver causes a distension of the vein due to increased intra-abdominal pressure.
-
b)
At the level of the anterior-inferior iliac spine, scans targeted at the proximal tendon of the rectus femoris show a posterior acoustic shadowing which should not be interpreted as calcification. It is caused by artifact due to obliquity of the indirect tendon which travels deeply to reach the area above the cotyloid cavity (Fig. 1). The direct tendon is more cranially located (Fig. 2) and it inserts on to the anterior-inferior iliac spine.
-
c)
The rectus femoris muscle is situated at the proximal third of the thigh, in front of the intermediate vastus muscle and the femur which constitutes the landmarks. The muscle is easily recognized by the presence of a typical sagittal intramuscular aponeurosis located in front of the muscle. The aponeurosis is visible only in the axial scans of the upper two-thirds of the muscle as a hyperechoic lamina with a characteristic “comma” looking appearance.
Study of the central hip region
Transverse scans should be performed starting from the muscle belly of the adductor muscles and then proceeding to the pubic area following the course of the muscle fibers until their insertion.
Three muscle layers are visible:
-
a)
the long adductor (lateral) and the gracilis (medial) form the most superficial layer;
-
b)
the short adductor forms the intermediate layer;
-
c)
the adductor magnus forms the deep layer.
Study of the lateral hip region (Figs. 6 and 7)
Transverse and longitudinal scans performed above the greater trochanter show:
-
a)
the gluteus maximus (posterior surface),
-
b)
the gluteus medius (anterior surface),
-
c)
the gluteus minimus (deep).
For US identification, the tensor fasciae latae can be used as a landmark; the gluteus minimus and the gluteus medius are behind the tensor fasciae latae.
Like the iliopsoas bursa, also the synovial peritrochanteric bursae cannot be assessed under physiological conditions as the wall is very thin and as there is no internal synovial effusion.
Study of the posterior hip region
Like all other muscles, these should be examined by transverse, sagittal, coronal and oblique scans. The first structure to be US evaluated is the gluteus maximus. At the posterior-inferior level, the proximal origin of the ischiocrural muscle group (semimembranosus, semitendinosus, and long head of the biceps femoris muscle) should be identified. The landmark is the ischial tuberosity. Here the semimembranosus tendon, the conjoined semitendinosus tendon and the long head of the biceps femoris muscle are inserted, and the sciatic nerve is next to them emerging from the piriformis muscle.
Conclusions
In many hip diseases, clinical history and physical examination are not enough to provide a certain diagnosis, and diagnostic imaging is therefore required. Conventional radiography is still the method of choice in all diseases involving the hip region. When it is technically well performed using appropriate projections, it provides a panoramic visualization of the pelvis, coxofemoral joint, sacroiliac joint and pubic symphysis as well as an initial study of the lower lumbar intersomatic discs. Conventional radiography also permits examination of the patient standing in an upright position and it provides visualization of possible soft tissue calcifications.
CT is the gold standard in the evaluation of bone lesions and for identifying the location of the tumor nest in case of osteoid osteoma, evaluation of cortical bone thickening in case of metastases, etc. CT is also essential in the evaluation of total hip replacement where it provides a detailed analysis of the implant position and impingement of the iliopsoas muscle against the prosthetic acetabular component.
MRI is the gold standard particularly in the study of bone marrow pathologies, joint space and periarticular tissues. However, MRI involves a high cost and long execution time, the availability is limited and there are several contraindications.
US can well assess muscles and tendons, it can identify the serous bursae as the origin of pathologies, identify joint effusion and lesions involving the outer cortical surface of the bone. US is particularly useful in the evaluation of periarticular tissues after hip replacement in cases where MRI cannot be performed, and in the detection of intra- or peri-articular synovial effusion. US provides an easy and non-traumatic guidance for needle aspiration for diagnostic purposes or therapeutic infiltrations. US can therefore be taken into consideration for the study of hip diseases in various situations, e.g. in patients presenting contraindications for MRI, who have symptoms suggesting tendon or bursal pathologies, and also for a better understanding of injuries already detected by other diagnostic methods, such as enthesitis.
US examination of the hip can provide excellent results, but only if the US operator is thoroughly familiar with both the normal anatomy and the US anatomy and carries out the examination following an accurate and efficient technique.
Conflict of interest statement
The authors have no conflict of interest.
Appendix. Supplementary data
The following are the supplementary data related to this article:
References
- 1.Conway W.F., Totty W.G., McEnery K.W. CT and MR imaging of the hip. Radiology. 1996;198(2):297–307. doi: 10.1148/radiology.198.2.8596820. [DOI] [PubMed] [Google Scholar]
- 2.Fishman E.K., Magid D., Mandelbaum B.R., Scott W.W., Jr., Weiss P., Hadfield R. Multiplanar (MPR) imaging of the hip. Radiographics. 1986;6(1):7–54. doi: 10.1148/radiographics.6.1.3685485. [DOI] [PubMed] [Google Scholar]
- 3.Rezig R., Copercini M., Montet X., Martinoli C., Bianchi S. Ultrasound diagnosis of anterior iliopsoas impingement in total hip replacement. Skeletal Radiol. 2004;33(2):112–116. doi: 10.1007/s00256-003-0703-4. Epub 2003 Nov 6. [DOI] [PubMed] [Google Scholar]
- 4.Bianchi S., Martinoli C., Keller A., Bianchi-Zamorani M.P. Giant iliopsoas bursitis: sonographic findings with magnetic resonance correlations. J Clin Ultrasound. 2002;30(7):437–441. doi: 10.1002/jcu.10093. [DOI] [PubMed] [Google Scholar]
- 5.Blankenbaker D.G., De Smet A.A. Hip injuries in athletes. Radiol Clin North Am. 2010;48(6):1155–1178. doi: 10.1016/j.rcl.2010.07.003. [DOI] [PubMed] [Google Scholar]
- 6.Malanga G.A., Dentico R., Halperin J.S. Ultrasonography of the hip and lower extremity. Phys Med Rehabil Clin N Am. 2010;21(3):533–547. doi: 10.1016/j.pmr.2010.05.002. [DOI] [PubMed] [Google Scholar]
- 7.Bancroft L.W., Blankenbaker D.G. Imaging of the tendons about the pelvis. AJR Am J Roentgenol. 2010;195(3):605–617. doi: 10.2214/AJR.10.4682. [DOI] [PubMed] [Google Scholar]
- 8.Pasta G., Nanni G., Molini L., Bianchi S. Sonography of the quadriceps muscle: examination technique, normal anatomy. J Ultrasound. 2010;13:85–89. doi: 10.1016/j.jus.2010.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


