Abstract
The suprahyoid region extends from the base of the skull to the hyoid bone and includes the pharyngeal, parapharyngeal, parotid, carotid, masticator, retropharyngeal, and perivertebral spaces, as well as the oral cavity. The areas that can be explored by ultrasound include the parotid, carotid, and masticator spaces; the oral cavity; the submandibular and sublingual spaces; the floor of the mouth; and the root of the tongue. The parotid space contains the parotid gland and the excretory duct of Steno, the facial nerve, the external carotid artery, the retromandibular vein, and the intraparotid lymph nodes. The carotid space in the suprahyoid region of the neck contains the internal carotid artery, the internal jugular vein, cranial nerves IX to XII, and the sympathetic plexus. Only some parts of the masticator space can be explored sonographically: these include the masseter muscle, the zygomatic arch and the outer cortex of the ramus of the mandible, and the suprazygomatic portion of the temporalis muscle. The submandibular space houses the submandibular gland, the submental and submandibular lymph nodes, and the anterior belly of digastric muscle. The facial artery and vein and the lower loop of the hypoglossal nerve all pass through the submandibular space. The sublingual space includes the sublingual gland, the deep portion of the submandibular gland and its main excretory duct, the hypoglossal nerve (cranial nerve XII), the lingual nerve (branch of the mandibular branch of trigeminal), and the glossopharyngeal nerve (IX cranial nerve), and the lingual artery and vein. The mylohyoid muscle forms the floor of the mouth. The deepest portion of the oral tongue, the root, consists of the genioglossus and geniohyoid muscles and includes the septum of the tongue. In this article we present the ultrasound features of the structures located in the suprahyoid region of the neck.
Keywords: Sonography, Anatomy, Neck
Sommario
La regione sovraioidea si estende dalla base cranica all’osso ioide, comprende gli spazi faringeo, parafaringeo, parotideo, carotideo, masticatorio, retrofaringeo, perivertebrale e il cavo orale.
Tra questi sono ecograficamente esplorabili gli spazi parotideo, carotideo, masticatorio e, del cavo orale, gli spazi sottomandibolare, sottolinguale, il pavimento della bocca e la radice della lingua.
Lo spazio parotideo accoglie la ghiandola parotide e il dotto escretore di Stenone, il nervo faciale, l’arteria carotide esterna, la vena retromandibolare e linfonodi intraparotidei.
Lo spazio carotideo, nel collo sovraioideo, comprende l’arteria carotide interna, la vena giugulare interna, i nervi cranici dal IX al XII e il plesso del simpatico.
Lo spazio masticatorio è solo parzialmente esplorabile ecograficamente: è possibile visualizzare il muscolo massetere, l’arcata zigomatica e la corticale esterna del ramo della mandibola, parte del muscolo temporale nel tratto soprazigomatico.
Lo spazio sottomandibolare accoglie la ghiandola sottomandibolare, linfonodi sottomandibolari e sottomentonieri, il venter anteriore del muscolo digastrico; lo spazio sottomandibolare è attraversato dall’arteria, dalla vena faciale e dall’ansa inferiore del nervo ipoglosso.
Lo spazio sottolinguale comprende la ghiandola sottolinguale, la porzione profonda della ghiandola sottomandibolare, col suo dotto escretore principale, i nervi ipoglosso (XII nervo cranico), linguale (ramo della branca mandibolare del trigemino), glossofaringeo (IX nervo cranico), l’arteria e la vena linguali. Il muscolo miloioideo costituisce il pavimento della bocca.
La radice della lingua rappresenta la porzione profonda della lingua orale, è costituita dai muscoli genioglosso e genioioideo, comprende il setto della lingua.
Nel presente articolo vengono presentati gli aspetti ecografici delle strutture situate nella regione sovraioidea del collo.
Introduction
The suprahyoid region extends from the base of the skull to the hyoid bone and includes the pharyngeal, parapharyngeal, parotid, carotid, masticator, retropharyngeal, and perivertebral spaces, as well as the oral cavity. The areas that can be explored by ultrasound include the parotid, carotid, and masticator spaces; the oral cavity; the submandibular and sublingual spaces, the floor of the mouth, and the root of the tongue.
Parotid space
The parotid space is bounded by the superficial layers of the deep cervical fascia. It occupies the space lying below the external auditory canal and the apex of the mastoid process and above the angle of the mandible. It is delimited anteriorly by the masticator space and inferiorly by the submandibular space; the deep boundaries are formed by the parapharyngeal and carotid spaces. It contains the parotid gland, the excretory duct of Steno, the facial nerve, the external carotid artery, the retromandibular vein, and the intraparotid lymph nodes [1–3].
The parotid gland is composed of two lobes, a superficial one that counts for two-thirds of the mass, and a deep lobe (or pharyngeal extension) that accounts for the other third. It is crossed by the facial nerve, the external carotid artery, and the retromandibular vein (Figs. 1 and 2).
Fig. 1.
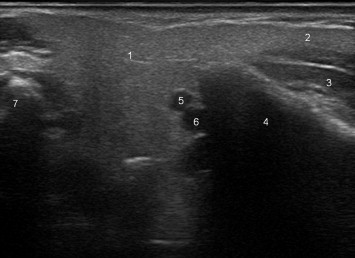
Axial scan of the parotid gland showing the superficial lobe (1), the masseter extension of the gland (2), the masseter muscle (3), the ramus of the mandible (4),the retromandibular vein (5), the external carotid artery (6), and the apex of the mastoid process (7).
Fig. 2.
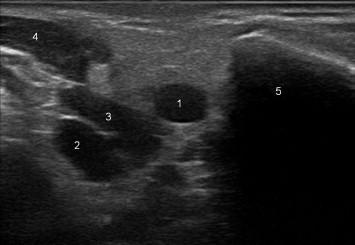
Axial scan of the parotid a few centimeters downstream from that in Fig. 1. It shows the retromandibular vein (1) and the external carotid artery (2), which are separated by the stylohyoid muscles and posterior belly of the digastric muscle (3), the sternocleidomastoid muscle (4) and the ramus of the mandible (5).
The facial nerve emerges from the stylomastoid foramen and forms branches within the parotid gland, lateral to the retromandibular vein. This represents the surgical plane of separation between the superficial and deep lobes of the parotid.
Two vessels can be seen lying posterior to the ramus of the mandible. The medial one is the external carotid artery, and the larger, lateral vessel is the retromandibular vein. It separates the carotid from the facial nerve, which is more lateral.
There are approximately 20 intraparotid lymph nodes. The provide level 1 lymphatic drainage of the external ear and lateral scalp.
The excretory duct of Steno emerges from the anterior border of the parotid gland (masseter extension), runs through the masticator space superficial to the masseter muscle, and passes over the buccinator muscle at the level of the second upper molar; small, accessory islands of salivary tissue sometimes form along its course.
The sonographic appearance of the parotid gland varies with the age of the patient. It is characterized by uniform echoes and hyperechogenicity with respect to the surrounding muscles. With age the echogenicity increases as a result of fatty infiltration, which increases the absorption of the ultrasound beam in deeper planes. While the superficial lobe can always be explored with ease, the deep lobe is more difficult because the ultrasound beam is blocked by the mandible and the mastoid process, especially when the latter is hypertrophic (Fig. 3) [4,5]. The duct of Steno can also be visualized on ultrasound when it is dilated. The facial nerve is not visible.
Fig. 3.
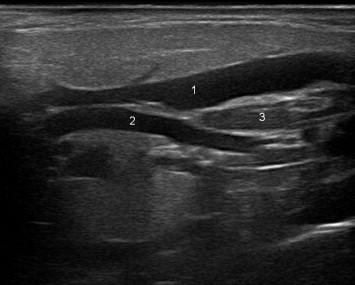
Longitudinal scan of the parotid gland, which shows the retromandibular vein (1) and the external carotid artery (2), whose lower halves are separated by the stylohyoid muscles and the posterior belly of the digastric muscle (3).
The lymph nodes are distributed mainly within the upper and lower poles of the gland. They are oval-shaped with a clearly visible fatty hilum; their short axis is no more than 5–6 mm.
Carotid space
The carotid space extends from the lower border of the jugular foramen-carotid canal all the way to the aortic arch and is delimited by the three layers of the deep cervical fascia. At the boundary between the supra- and infrahyoid spaces, the common carotid artery bifurcates. The external carotid leaves the carotid space and crosses the parotid space in a caudocranial direction. The carotid space in the suprahyoid region of the neck contains the internal carotid artery, the internal jugular vein, cranial nerves IX–XII, and the sympathetic plexus. It is bounded laterally by the parotid space, anteriorly by the masticator and parapharyngeal spaces, and posteriorly by the perivertebral space. The lower half of the space, which contains the origins of the internal and external carotid arteries, is the only portion of sonographic interest; the upper half cannot be explored because it lies deep to the mastoid process [1–3].
The internal carotid is usually posterolateral to the external carotid (which is generally smaller in caliber), and it presents a short dilated segment at its origin, which is an extension of the carotid bulb. In a few individuals (5%–10% of the population), the internal carotid lies medial or anterior to the external carotid or the two vessels may lie within the same frontal plane. The external carotid immediately gives rise to the superior thyroid artery (which is the first of the anterior collateral branches of sonographic interest; the second and third collateral branches are the lingual and facial arteries, respectively. This feature is the most reliable way to identify the vessel on B-mode scans, especially when the two vessels are identical in caliber. The second most reliable identifying feature is the Doppler tracing. Flow within the internal carotid is typical of low peripheral resistance (high diastolic peak), whereas the external carotid has high-resistance flow (lower diastolic peak, systolic peak higher than that of the internal carotid) [4,5].
Masticator space
The masticator space is delimited by the superficial layer of the deep cervical fascia and located anterolateral to the parapharyngeal space. It can be only partially explored with ultrasound: the masseter muscle, the zygomatic arch, the outer cortex of the ramus of the mandible, and the suprazygomatic segment of the temporal muscle (temporal fossa) can all be visualized (Fig. 1), but not the pterygoid muscles, the pterygoid venous plexus, the mandibular branch of the trigeminal nerve or its branches.
The masticator space lies posterior to the parotid space, which is lateral, and the carotid, which is medial. It is crossed by the duct of Steno, which lies superficial to the masseter muscle. Accessory islands of parotid gland tissue are often found along the course of this duct [1–3].
Submandibular space
This space is located deep to the platysma muscle and delimited by the superficial layer of the deep cervical fascia. It lies superior to the hyoid bone and inferolateral to the mylohyoid muscle (floor of the mouth) (Fig. 4). It is bounded posteriorly by the parotid space, and it communicates with the sublingual and parapharyngeal spaces, extending inferiorly into the anterior cervical space of the infrahyoid region of the neck. It contains the submandibular gland, the submandibular and submental lymph nodes, and the anterior belly of the digastric muscle and is traversed by the facial artery and vein and the inferior segment of the hypoglossal nerve [1–3].
Fig. 4.
Sagittal scan of the submandibular space, which shows the platysma muscle (1), the submandibular gland (2) and its lingual extension (3), the mylohyoid (4) and hyoglossus (5) muscles, the palatine tonsils (6), and the sternocleidomastoid muscle (7).
The submandibular gland includes two parts. The large, superficial portion that lies directly beneath the superficial layer of the deep cervical fascia, which constitutes the capsule of the gland, posterior to the facial artery. It is crossed by the facial vein and the cervical branch of the facial nerve (cranial nerve VII). The smaller, deeper portion of the gland, referred to as the lingual extension, envelopes the posterior border of the mylohyoid muscle. It extends anteriorly and contacts the posterior aspect of the sublingual gland, running between the mylohyoid (lateral) and hyoglossal (medial) muscles (Fig. 5).
Fig. 5.
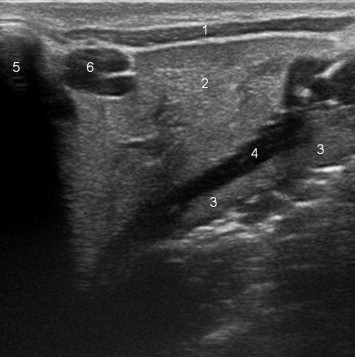
Coronal scan of the submandibular space, which shows the platysma muscle (1), the submandibular gland (2) and its lingual extension (3), the hyoglossus muscle (4) muscles, the angle of the jaw (5), and a periglandular lymph node (6).
The main excretory duct, the duct of Wharton, emerges from the deep extension of the gland and crosses the lateral compartment of the sublingual space, medial to the gland, in relation to the sublingual artery and lingual nerve; it opens into the sublingual sulcus at the apex of the caruncle.
The submental and submandibular lymph nodes (levels I A and I B, respectively) drain the anterior portion of the face, including the oral cavity, the anterior paranasal sinuses, and the orbits.
The hypoglossal nerve crosses the submandibular space and forms a loop before running cranially and anteriorly to innervate the muscles of the tongue.
On ultrasound, the gland appears uniformly hypoechoic with respect to the parotid and sublingual glands [4,5]. Unless they are dilated, the excretory ducts are not visible. Lymph nodes are present around the gland but not within it. Inside the gland, the facial vein can be identified, and superficially the facial artery intersects the posterior pole of the gland.
Sublingual space
The sublingual space is not lined with fasciae: it is located beneath the oral portion of the tongue, superomedial to the mylohyoid muscle (which forms the floor of the mouth), lateral to the genioglossus and geniohyoid muscles (root of the tongue) (Fig. 6).
Fig. 6.
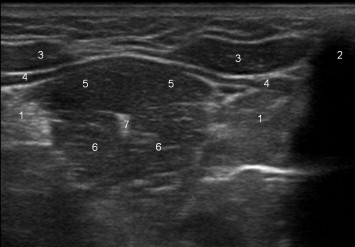
Coronal scan of the sublingual space, which shows the sublingual gland (1), the body of the mandible (2), the digastric (3), mylohyoid (4), geniohyoid (5), and genioglossus (6) muscles; and the hyperechoic raphe of the tongue (7).
The two sublingual spaces communicate with one another by means of an isthmus located under the frenulum of the tongue. At the approximate level of the posterior border of the mylohyoid muscle, the sublingual space communicates directly with the submandibular and parapharyngeal spaces, thanks to the absence of a dividing fascia [1–3]. The anterior third of the mylohyoid muscle is separated from the posterior two thirds by a fissure of variable width, and an extension of the sublingual gland sometimes passes through this opening and enters the submandibular space.
The posterior portion of the sublingual space is divided into lateral and medial compartments by the hyoglossal muscle. The lateral compartment contains the multilobular sublingual gland and its excretory ducts; the deep portion of the submandibular gland with its main excretory duct; the hypoglossal nerve (cranial nerve XII), and the lingual nerve (which originates from the mandibular branch of the trigeminal nerve) (Fig. 7). The medial compartment contains the glossopharyngeal nerve (cranial nerve IX) and the lingual artery and vein.
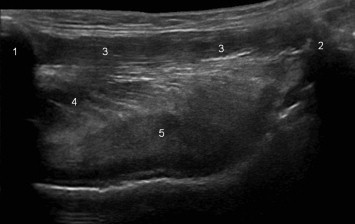
Fig. 7.
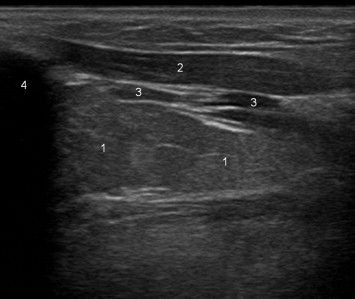
Longitudinal scan of the sublingual gland (1), which shows the digastric (2) and mylohyoid (3) muscles, as well as the symphysis menti (4).
On ultrasound, the gland appears uniformly hyperechoic with respect to the submandibular gland and the surrounding muscles; with advancing age, the gland undergoes fibroadipose involution [4,5].
There are several excretory ducts that drain each of the gland’s lobules along the sublingual fold. The largest lobule is an exception: it drains into the sublingual caruncle lateral to Wharton’s duct. The ducts cannot be visualized on ultrasonography. Medially, the lingual artery can be seen.
Floor of the mouth and base of the tongue
The floor of the oral cavity is formed by the mylohyoid muscle, a quadrilateral sheet consisting of two bellies, whose lower fasciae are in contact with the anterior fascia of the digastric muscle, the submandibular gland, and the superficial cervical fascia. The upper aspect is in contact with the geniohyoid and hyglossus muscles, the sublingual gland, and the lingual and hypoglossal nerves (Fig. 8).
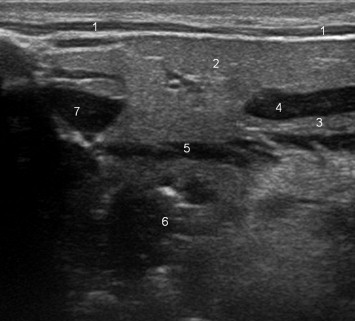
Fig. 8.
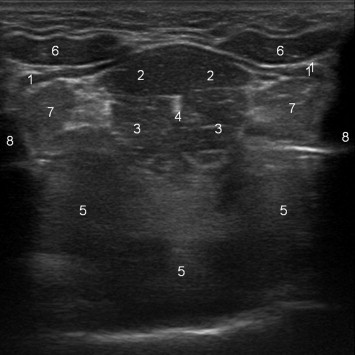
Coronal scan of the floor of the mouth and the base of the tongue: It shows the mylohyoid (1), geniohyoid (2), and genioglossus (3) muscles; the raphe of the tongue (4), the body of the tongue (5), the digastric muscle (6), the sublingual glands (7), and the body of the mandible (8).
It originates from the mandible and its fasciae converge medially to insert in the mylohyoid raphe, a sagittal fibrous lamina, and the hyoid bone [1].
The root of the tongue is the deepest portion of the oral tongue (i.e., the anterior 2/3 of the tongue: the posterior third represents the base of the tongue). It is composed of the genioglossus and geniohyoid muscles and includes the septum of the tongue. It is in contact with the mylohyoid muscle (inferiorly), the intrinsic muscles of the tongue (superiorly and posteriorly), and with the mandibular symphysis (anteriorly) (Fig. 9) [2].
Fig. 9.
Longitudinal, panoramic scan of the tongue showing the symphysis menti (1), the hyoid bone (2), the geniohyoid (3) and genioglossus (4) muscles, and the body of the tongue (5).
The mylohyoid, digastric, hyglossus, genioglossus, and geniohyoid muscles can all be explored sonographically [4].
Conclusions
Various diseases can affect the suprahyoid region of the neck, and imaging studies, ultrasound in particular, are becoming increasingly important for their correct diagnosis and treatment. A thorough knowledge of the region is essential for the completeness of the examination.
Conflict of interest statement
The authors have no conflict of interest.
Appendix. Supplementary material
References
- 1.Harnsberger H.R., Osborn A.G., Macdonald A., Ross J.S. vol. II. Amirsys; 2006. (Diagnostic and surgical imaging anatomy: brain, head & neck, Spine). 126–297. [Google Scholar]
- 2.Balboni G.C. vol 2. Edi-Ermes; 1994. Anatomia umana. (Terza edizione). 20–80. [Google Scholar]
- 3.Harnsberger H.R., Wiggins R.H., Hudgins P.A. vol. III. Amirsys; 2004. (Head and neck). 0–8. [Google Scholar]
- 4.Barozzi L., Busilacchi P., Pavlica P., Zaccarelli A. Idelson-Gnocchi; 1999. Anatomia ecografica. 21–48. [Google Scholar]
- 5.Bialek E.J., Jakubowski W., Zajkowski P., Szopinski K.T., Osmolski A. US of the major salivary glands: anatomy and spatial relationship, pathologic conditions and pitfalls. RadioGraphics. 2006;26:745–763. doi: 10.1148/rg.263055024. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


