Abstract
Introduction
Varicoceles are abnormal dilatations of the pampiniform venous plexus. They are classified as primary or secondary, depending on their cause, and staged clinically on the basis of their extension and on the presence or the absence of spontaneous or induced reversal of blood flow.
Materials and methods
We examined 95 patients (age range: 3–77 years) using Color Doppler ultrasound with settings optimized for the study of slow flow. All patients found to have varicoceles underwent ultrasonographic assessment of the kidneys and retroperitoneum. Findings were classified with a simplified version of the Sarteschi system.
Results
41 (43.1%) of the patients were found to have varicoceles, which were classified as grade 1 in 11 cases, grade 2 in 13, grade 3 in 10, and grade 4 in 7 according to the simplified Sarteschi classification.
Discussion
Our results are with those reported in the literature. They confirm that varicoceles are a frequent finding and ultrasonography is currently the best imaging technique for its diagnosis and also for the post-surgery follow-up.
Keywords: Varicocele, Color Doppler ultrasonography, Infertility
Sommario
Introduzione
Il varicocele è un’anomala dilatazione del plesso pampiniforme; in base all’eziologia può essere distinto in primitivo e secondario, mentre in base all’estensione e alla presenza o assenza di reflussi, spontanei o provocati, può essere classificato in stadi.
Materiali e metodi
Sono stati inclusi nello studio 95 pazienti con età compresa tra 3 e 77 anni. I parametri color Doppler sono stati ottimizzati per la valutazione dei flussi lenti. In tutti i pazienti con varicocele è stato eseguito un esame ecografico di reni e retroperitoneo. Per la classificazione è stata utilizzata quella di Sarteschi, semplificata.
Risultati
I casi di varicocele riscontrati sono stati 41 (43,1%); in base alla classificazione di Sarteschi semplificata 11 pazienti rientravano nel grado 1; 13 nel grado 2; 10 nel grado 3; 7 nel grado 4.
Discussione
I risultati da noi rilevati sono simili a quelli presenti in letteratura, si conferma quindi come il varicocele sia frequente e al momento attuale l’ecografia rappresenti la tecnica di imaging di elezione nello studio di questa affezione, sia per la diagnosi che per il follow-up post-intervento. L’associazione con l’infertilità resta di pertinenza dello spermiogramma.
Introduction
Varicoceles are abnormal dilatations of the pampiniform venous plexus. They occur with an incidence of 15% in adolescent males and 10–15% in adult men [1]. Two types can be distinguished on the basis of etiopathogenesis: primary and secondary [2]. Primary varicoceles are due to venous reflux into the pampiniform plexus from the internal spermatic vein as a result of incontinent venous valves, and they usually occur on the left side (85% of cases) [3]. In fact, the left internal spermatic vein drains into the homolateral renal vein at a 90-degree angle, and as a result of this particular anatomical feature, endoluminal pressure in the renal vein is transmitted backwards, opposing flow from the internal spermatic vein. On the right side, the internal spermatic vein merges with the inferior cava vein at an acute angle, and its drainage is promoted by the negative pressure created by caval blood flow [4]. Secondary varicoceles are the result of increased pressure in the testicular vein, which can be caused by several conditions, such as hydronephrosis, hepatic cirrhosis associated with portal hypertension with splenorenal shunts, abdominal and retroperitoneal neoplasms, and the so-called nutcracker phenomenon, which involves compression of the left renal vein between the superior mesenteric artery and aorta.
Clinically speaking, varicoceles are characterized by the presence of a palpable, soft scrotal mass. In rare cases they are associated with moderate pain, and they can also be associated with infertility. Indeed, the link between varicoceles, sperm alterations, and male infertility, which occurs in 30%–45% of patients with varicocele [5], is well-documented. The risk of infertility is in fact the major indication for treatment.
Diagnostic imaging plays a fundamental role in the diagnosis and staging of varicoceles. Ultrasonography, color Doppler ultrasound (CDUS), and phlebography are all used for this purpose [3,5,6]. CDUS is currently considered the gold-standard method for the assessment of varicoceles. It displays high accuracy in the diagnostic phase, with sensitivity and specificity close to 100% [7], and it is also useful for staging the disease according to appropriate classification systems. Several classification systems have been proposed. The most widely used are the ones developed by Sarteschi (which involves examinations done with the patient lying down and standing and distinguishes five different stages) [8] (Table 1) and by Dubin (which requires examination of patients in the supine position and includes three stages) [9] (Table 2).
Table 1.
Color Doppler ultrasound (CDU) classification of varicocele.
| Grade | Features |
|---|---|
| 1 | Reflux in vessels in the inguinal channel is detected only during the Valsalva maneuver, while scrotal varicosity is not evident in the standard US study |
| 2 | Small posterior varicosities that extend to the superior pole of the testis. Their diameters increase and venous reflux is seen in the supratesticular region only during the Valsalva maneuver. |
| 3 | Vessels appear enlarged at the inferior pole of the testis when the patient is evaluated in a standing position; no enlargement is detected if the patient is examined in a supine position. Reflux observed only under during the Valsalva maneuver. |
| 4 | Vessels appear enlarged even when the patient is studied in a supine position; the dilatation is more marked in the upright position and during the Valsalva maneuver. Testicular hypotrophy is common at this stage. |
| 5 | Venous ectasia is evident even in the prone decubitus and supine positions. Reflux is observed at rest and does not increase during the Valsalva maneuver. |
Table 2.
Dubin classification.
| Grade | Features |
|---|---|
| 0 | Moderate, transient venous reflux during the Valsalva maneuver (physiologic findings) |
| 1 | Persistent venous reflux that ends before the Valsalva maneuver is completed |
| 2 | Persistent venous reflux throughout the entire Valsalva maneuver |
| 3 | Venous reflux that is present under basal conditions and does not change during the Valsalva maneuver |
Currently, no other techniques are used for the assessment of varicoceles, and the role played by phlebography is essentially therapeutic.
Materials and methods
From January through December 2010, 95 patients were enrolled in the present study and underwent testicular ultrasonography. The clinical indications for the sonographic studies varied.
Patient ages ranged from 3 to 77 years. In all cases, CDUS assessment was included to detect possible varicoceles.
The sonographic studies were performed with a Philips IU22 or a GE LOGIQ® E9 scanner with linear high-frequency probes.
Patients were examined only in the supine position. The scrotum was placed on an appropriate support and distended. The latter was accomplished by having the patient exert moderate upward traction on the penis (toward the umbilicus). CDUS assessments were made under basal (resting) conditions and during the Valsalva maneuver.
Color Doppler parameters were optimized for the evaluation of slow flow (Prf 0.7 MHz, wall filter at minimum levels, gain at the maximum level permitted by the presence of artifacts, elective focus on the region of interest) and standardized.
All patients found to have varicoceles underwent ultrasonographic assessment of the kidneys and retro-peritoneum.
We used a simplified version of the Sarteschi classification (Table 3) based on varicocele extension and the magnitude of the reflux, which are the most important risk factors for infertility. However, both parameters were assessed only with the patient lying down because uniform, repeatable evaluation of reflux was technically difficult when the patient was in an upright position.
Table 3.
Simplified color Doppler ultrasound classification of varicoceles.
| Grade | Features |
|---|---|
| 1 | Reflux in the vessels of the inguinal canal that is observed only during the Valsalva maneuver and absence of varicosity on standard ultrasonography |
| 2 | Small varicosities with reflux seen only during the Valsalva maneuver. |
| 3 | Enlarged vessels whose caliber increases during the Valsalva maneuver. |
| 4 | Obvious vessel enlargement with reflux that is present under basal conditions and does not increase during the Valsalva maneuver |
In the report, varicoceles were described without specifying the stage.
It was not possible to obtain sperm analysis in all patients with varicoceles, so no statistical analysis was carried out to identify correlations with these data.
Results
Among the 95 patients we examined, 41 cases of varicocele (43.1%) were identified. In 38 cases (92.7%), this was first time the patient had been diagnosed with varicocele. The other 3 cases (7.3%) involved recurrences of varicoceles that had already been treated; in all cases the stage of the recurrent lesion was lower than that observed before surgery.
Varicoceleshad been clinically detected in 21 cases.
Staging with the simplified Sarteschi classification assigned 11 patients to stage 1(Fig. 1), 13 to stage 2 (Fig. 2), 10 to stage 3 (Fig. 3), and 7 to stage 4 (Fig. 4).
Figure 1.
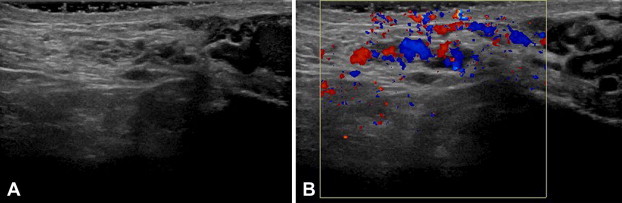
Varicocele (A) with reflux in the vessels of the inguinal canal seen only during the Valsalva maneuver and (B) absence of varicosity on the standard US examination (A) (grade 1).
Figure 2.
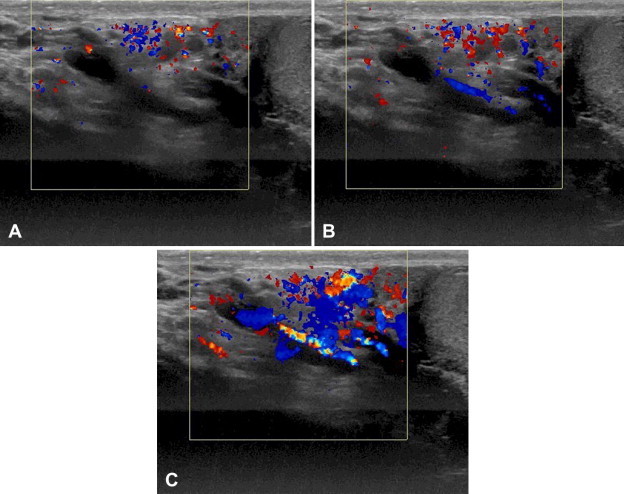
Varicocele with small varicosities (A) that exhibit reflux only during the Valsalva maneuver (B,C) (grade 2).
Figure 3.
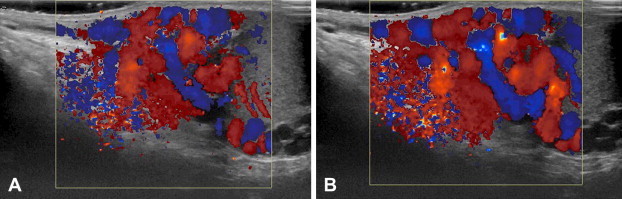
Varicocele with enlarged veins (A) whose calibers increase during the Valsalva maneuver (B) (grade 3).
Figure 4.
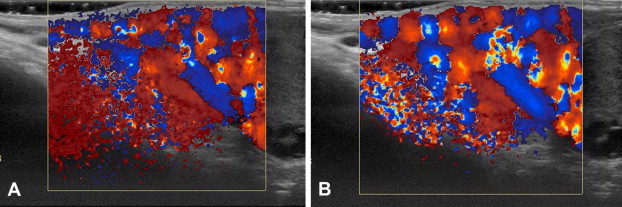
Varicocele with enlarged veins (A) whose calibers do not increase during the Valsalva maneuver (B) (grade 4).
None of the patients we examined presented secondary varicoceles.
Discussion
Most varicoceles are asymptomatic [10]. They usually present as non-painful scrotal swellings; complaints of pain are less common. The physical examination, performed with patients in the supine and upright positions and at rest and during theValsalva maneuver, reveals a compressible mass above, below, or around the testicle.
Dubin and Amelar distinguish three clinical stages. Stage 1 varicoceles are small and can be identified by palpation only during the Valsalva maneuver. Stage 2 varicoceles are also palpable underresting conditions, and stage 3 includes large varicoceles that are visible when the patient is at rest [9]. Subclinical varicoceles may not be detectable clinically, but their presence can be demonstrated by CDUS.
Color Doppler ultrasound is the imaging technique used most frequently to assess varicoceles. The blood vessels of the pampiniform plexus are usually no more than 1.5 mm in diameter.
When a patient with a varicocele is examined at rest, multiple elongated, tortuous anechoic structures are seen above, around, or beneath the testicle [11] (Table 4). The vessel caliber thresholds used by different authors to define varicocele vary from 2 to 3 mm [12]. Under baseline conditions, blood flow may be too slow to be detected by CDUS, but during the Valsalva maneuver the varicocele enlarges and flow reversal becomes evident. Some authors suggest that varicoceles should also be assessed while the patient is standing. CDUS is currently considered the gold-standard technique for varicocele assessment because it allows accurate diagnosis (with a sensitivity and a specificity close to 100%) [7], and it can also be used to stage the lesions using appropriate classification systems.
Table 4.
Imaging modalities used to diagnose varicoceles.
| Methods | Diagnostic criteria |
|---|---|
| Sonography | Tortuous, tubular, anechoic structures adjacent to the testis corresponding to dilated veins of the pampiniform plexus with calibers of 2–3 mm during the Valsalva maneuver |
| Color Doppler sonography | Reflux into the spermatic vein that increases during the Valsalva maneuver; classified as static (grade I), intermittent (grade II), or continuous (grade III) |
| Phelobography | Increase in the caliber of the internal spermatic vein with reflux into the abdominal, inguinal, scrotal, or pelvic portions of the spermatic vein, and the presence of collateral circulation |
| Magnetic Resonance Imaging | Dilatation of the vessels of the pampiniform plexus with signal intensity that varies depending on the flow rate and enhancement after injection of contrast medium |
| Scintigraphy | Intrascrotal accumulation of technetium-99-labeled red cells with reflux observed during dynamic maneuvers |
The literature contains descriptions of several systems for ultrasonographic classification of varicoceles. The Sarteschi classification includes 5 stages and is based on assessment of the lesion when the patient is standing and lying down [8](Table 1), whereas the Dubin classification is based only on findings obtained with the patient in the supine position and it includes 3 stages [9] (Table 2).
Although MRI is not usually employed for imaging diagnosis of varicoceles, these lesions may be discovered fortuitously during MRI performed for other reasons. Therefore, it is important to know their imaging characteristics [13] (Table 4). MRI also reveals dilated vessels which appear as tortuous, tubular structures; low-flow varicoceles produce an intermediate-intensity signal in T1-weighted sequences and hyperintensity in T2-weighted sequences. In the presence of high flow, no signal is observed inside the dilated vessels, which present enhancement after intravenous administration of a paramagnetic contrast agent.
Phlebography reveals enlargement of the internal spermatic vein with reflux into the abdominal, inguinal, scrotal, or pelvic portion of the spermatic vein and the presence of collateral circulation (Table 4).
Some authors have used technetium-99-labeled-red blood cell scintigraphy in patients with varicoceles. It shows intrascrotal accumulation of the radioactive tracer with evidence of reflux during dynamic maneuvers (Table 4).
There are well-documented associations between varicocele and sperm alterations or male infertility (30–45%) [5], so treatment is mandatory. Options include conventional and laparoscopic surgery and interventional radiology [14]. The aim is to improve the sperm parameters and allow spontaneous conception, by obliterating all spermatic veins and preserving the arteries and lymphatic vessels, while minimizing the risk of postoperative complications and lesion recurrence.
A meta-analysis examined data from the various studies dealing with the treatment of varicocele published between 1980 and 2008 [14] and found that 1748 (39.07%) of 4473 men treated with different techniques achieved a spontaneous pregnancy with their partners after treatment. The highest incidence of spontaneous pregnancy was observed after microsurgical varicocelectomy (41.97%), thePalomo procedure (37.69%), Ivanissevich varicocelectomy (36%), embolization by radiological approach (33.2%), and laparoscopic varicocelectomy (30.07%). Post-treatment relapse rates reported in the different studies ranged from 0% to 35%, and the lowest rates were observed in men treated with microsurgical varicocelectomy (1.05%), Ivanissevich varicocelectomy (2.63%), laparoscopic varicocelectomy (4.3%), embolization by radiological approach (12.7%), or the Palomo procedure (14.97%).
CDUS is also the gold-standard method for detection of post-treatment relapses. The examination is performed 1 month after treatment and focuses on the detection of incomplete occlusion of pampiniform plexus and/or the appearance of dilated collateral vessels. Sperm counts and mobility should also be reassessed after 3 months.
Conclusions
Varicocele is a frequent finding, and its association with sterility is extensively documented. Ultrasonography currently represents the imaging technique of choice for the diagnosis of varicoceles and their post-operative follow-up thanks to its widespread availability, high repeatability, low cost, and the absence of adverse effects.
The detection of associated infertility is based on the assessment of sperm counts and mobility. However, sterility is more likely in men with very large varicoceles that have extensive contact with the head of epididymis and are associated with spontaneous reflux.
Conflict of interest statement
The authors have no conflict of interest to declare.
Appendix. Supplementary data
References
- 1.Liguori G., Trombetta C., Garaffa G., Bucci S., Gattuccio I., Salamè L. Color Doppler ultrasound investigation of varicocele. World J Urol. 2004 Nov;22(5):378–381. doi: 10.1007/s00345-004-0421-0. [DOI] [PubMed] [Google Scholar]
- 2.Bhosale P.R., Patnana M., Viswanathan C., Szklaruk J. The inguinal canal: anatomy ed imaging features of common and un common masses. RadioGraphics. 2008;28:819–835. doi: 10.1148/rg.283075110. [DOI] [PubMed] [Google Scholar]
- 3.Horstman W.G., Middleton W.D., Melson G.L., Siegel B.A. Color Doppler US of the scrotum. RadioGraphics. 1991;11:941–957. doi: 10.1148/radiographics.11.6.1749858. [DOI] [PubMed] [Google Scholar]
- 4.Draghi . Athena; 2003. Eco-Color-Doppler dello scroto. [Google Scholar]
- 5.Gazzera C., Rampado O., Savio L., Di Bisceglie C., Manieri C., Gandini G. Radiological treatment of male varicocele technical, clinical, seminal and dosimetric aspects. Radiol Med. 2006 Apr;111(3):449–458. doi: 10.1007/s11547-006-0041-4. [DOI] [PubMed] [Google Scholar]
- 6.Lee J., Binsaleh S., Lo K., Jarvi K. Varicoceles: the diagnostic dilemma. Androl. 2008 Mar–Apr;29(2):143–146. doi: 10.2164/jandrol.107.003467. [DOI] [PubMed] [Google Scholar]
- 7.Dogra V.S., Gottlieb R.H., Oka M., Rubens D.J. Sonography of the scrotum. Radiology. 2003;227:18–36. doi: 10.1148/radiol.2271001744. [DOI] [PubMed] [Google Scholar]
- 8.Sarteschi L.M. Lo studio del varicocele con eco-color-Doppler. G Ital Ultrasonologia. 1993;4:43–49. [Google Scholar]
- 9.Dubin L., Amelar R.D. Varicocele size and results of varicocelectomy in selected subfertile men with varicocele. Fertil Steril. 1970;21:606–609. doi: 10.1016/s0015-0282(16)37684-1. [DOI] [PubMed] [Google Scholar]
- 10.Mohammed A., Chinegwundoh F. Testicular varicocele: an overview. Urol Int. 2009;82:373–379. doi: 10.1159/000218523. [DOI] [PubMed] [Google Scholar]
- 11.Woodward P.J., Schwab C.M., Sesterhenn I.A. From the archives of the AFIP: extratesticular scrotal masses: radiologic-pathologic correlation. RadioGraphics. 2003;23:215–240. doi: 10.1148/rg.231025133. [DOI] [PubMed] [Google Scholar]
- 12.Kim E.D., Lipshultz L.I. Role of ultrasound in the assessment of male infertility. J Clin Ultrasound. 1996;24:437–453. doi: 10.1002/(SICI)1097-0096(199610)24:8<437::AID-JCU4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 13.Beddy P., Geoghegan T., Browne R.F., Torreggiani W.C. Testicular varicoceles. Clin Radiol. 2005;60:1248–1255. doi: 10.1016/j.crad.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 14.Cayan S., Shavakhabov S., Kadioğlu A. Treatment of palpable varicocele in infertile men: a meta-analysis to define the best technique. J Androl. 2009;30:33–40. doi: 10.2164/jandrol.108.005967. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


