Abstract
Introduction
The authors report on an ultrasound (US) outreach program for the nomadic people living in Yushu, a remote area of Qinghai, Tibet, People's Republic of China (PRC) about 4800 m above sea level. The program was carried out in cooperation with ROKPA INTERNATIONAL, a non-profit organization (NGO) that aims at helping the poorest peoples living in remote regions of the world.
Materials and methods
A hand-held US scanner (Sonosite 180 Plus, Sonosite Inc., Bothell, WA, USA) equipped with a 3.5–5 MHz convex probe was used at a local clinic for 21 days in 2007 and for 32 days in 2009.
Results
A total of 1128 US examinations were performed (578 in 2007 and 550 in 2009). The main diagnoses were: Echinococcal cysts (66 cases; 6.23%) – Biliary tract and intrahepatic gallstones (10% of patients examined) – Ascariasis – Acute and chronic hepatitis, liver cirrhosis, abdominal masses – Abdominal tuberculosis – Miscellaneous (trophoblastic tumor, megacalicosis, splenomegaly in acute leukemia).
After the first experience in 2007, collaboration with the local hospital was established for the treatment of patients affected by active echinococcal cysts using albendazole and puncture, aspiration and injection of scolicidal agent and re-aspiration (PAIR) and subsequent follow-up.
Discussion and conclusions
US scanning was well accepted by the local population and allowed diagnosis, classification and choice of treatment of the echinococcal cysts according to recent criteria based on a stage-specific approach. Percutaneous treatment was also introduced, but more training of local healthcare providers is needed to secure continuation of this practice.
Further experience may help improve the standard of health care services offered to the nomadic populations in this remote area.
Keywords: Ultrasonography, Cystic echinococcosis, International cooperation
Sommario
Introduzione
Scopo dello studio è valutare i risultati dell’integrazione dell’ecografia nel programma di assistenza alla popolazione nomade della ONG Rokpa International a Yushu, Qinghai, Tibet, PRC. Il programma fornisce dal 2003 assistenza sanitaria alla popolazione povera dell’altipiano (4.800 mt s l m)
Materiali e metodi
Un ecografo portatile Sonosite 180 Plus (Sonosite Inc, Bothell, WA, USA) con sonda convex da 3,5-5 MHz è stato usato per 21 gg nel 2007 e per 32 gg nel 2009 per esami addominali offerti alla popolazione che si presentava all’Ambulatorio e in un villaggio di tende nomadi.
Risultati
Sono stati eseguiti 1128 esami ecografici (578 nel 2007 e 550 nel 2009). Le principali patologie riscontrate: – Cisti da echinococco (66 casi, 6.23%). – Calcolosi della colecisti, delle vie biliari, intraepatiche (10% dei pazienti esaminati). – Ascaridiasi – Steatosi, epatiti acute e croniche, cirrosi epatica, masse addominali solide. – Tubercolosi addominale. – Altre varie (gravidanza, mola vescicolare, megacalicosi renale, splenomegalia da leucosi acuta).
Dopo la prima esperienza del 2007, è stata avviata una collaborazione con l’Ospedale locale per l’echinococcosi cistica, con trattamento dei pazienti con cisti attive con PAIR e albendazolo e follow-up dei medici locali.
Discussione e conclusioni
L’introduzione dell’ecografia, bene accettata dalla popolazione locale, ha migliorato lo standard assistenziale, permettendo diagnosi, classificazione e scelta del trattamento delle cisti da echinococco, l’introduzione dei trattamenti percutanei e una migliore allocazione delle risorse economiche per la cooperazione.
L’impiego di un ecografo portatile a batteria si è rivelato agevole ed efficace in un contesto di popolazione isolata in un ambiente estremo, con gravi problematiche sanitarie e umane.
Introduction
The authors present an ultrasound (US) program carried out in 2007–2009 on the Tibetan Plateau in Yushu, Qinghai, People's Republic of China (PRC) about 4800 mt above mean sea level at a clinic which has since 2003 provided free medical assistance to the Tibetan nomads. The aim of this paper is to describe the morbid conditions that were encountered and to demonstrate the usefulness of a portable US scanner in an extreme environment.
Geographic and environmental framework
Yushu (Fig. 1) is located on the eastern road which ascends from Xining after having crossed some mountain passes at up to 5600 m above sea level on the Tibetan Plateau in order to move on toward Chendu and Lasha. The area is inhabited mainly by ethnic Tibetans and it is very poor and undeveloped (Fig. 2). Herding and subsistence agriculture are still the main activities, and a substantial part of the population living around the city is nomadic and illiterate. The sanitary conditions are still inadequate. Although the region is very rich in water (Asia's great rivers have their origin here and there are big lakes) the groundwater is already polluted [1]. People bathe and wash in the river and use the river water for cooking and washing their clothes, and potable water quality control is inadequate. Slaughtering and meat handling as well as preparation of dairy products are poorly controlled and cows are walking freely in the roads. Stray dogs are a serious problem which is being addressed, and in the area several cases of rabies and plague have been registered [2]. The food (based on rice and barley) contains low levels of vitamins and is rich in animal fat from meat and yak milk [3].
Figure 1.

Yushu, Qinghay, PRC.
Figure 2.

View of the Tibetan Plateau.
The urbanization has affected part of the population but it has not improved sanitation and nourishment as processed food has been introduced, and it is often expired. The environment, the land and the buildings are not adequately controlled by the authorities; this is evidenced by the fact that the recent earthquake which struck Yushu on April 14, 2010 claimed more than 6000 victims and destroyed 95% of households.
High-altitude hypoxia and adaptation difficulties as well as long, very cold winters and flooding in late summer add to the discomfort [3,4]. Finally, access to health care and prevention is difficult. The town has one “public” hospital and numerous private clinics. In fact all health care is paid for and the nomadic population has no access to it as they have a low income and are often illiterate.
In this context, the humanitarian organizations play an important role as they have been present on the territory for many years. ROKPA (a word which in Tibetan means help) is an international organization based in Zurich, which is active in a series of developing countries, especially in Asia. ROKPA operates an orphanage-school in Yushu and an outpatient medical, dental and eye care service in the summer months. It also deals with traditional Tibetan medicine and the protection of local artistic traditions such as poetry and dance (www.rokpainternational.org).
Traditional medicine is widely used and the patients who requested our care had in many cases already undergone traditional treatment. In some cases, the patients willingly accepted diagnostic tests and particularly US examination, but they preferred traditional treatments based on herbs, and resorted to Western medicine only when they were in a serious condition.
Materials and methods
Since 2003 the health care program has been organized by a team of medical doctors from various countries around the world, who offer medical examinations and some basic services such as blood pressure measurement, measurement of visual acuity and glasses as well as dental care. In 2006 some Italian doctors joined the organization and started collaborating with the local hospital and nursing service. In August 2007, US and physiotherapy were introduced. In 2008 the Tibetan Plateau was not accessible.
In July and August 2009 clinical and US collaboration continued as a pilot project on echinococcosis involving diagnosis and locoregional treatment. The project was presented to the local public health authorities, but it was interrupted in 2010 because of the earthquake.The aim of the collaborating medical doctors is not to replace the local medical doctors in the clinical and diagnostic activity related to the most common diseases, but to support a population segment that would not normally have access to health care, by constructively integrating their assistance with locally available resources.
Organization of the activity
Clinical examination at the clinic of the “Yushu Medical School and Orphanage” included also collection of the patients' medical and personal records which were registered in a clinical file.
The team consisted of 3 medical doctors who performed clinical examinations, 1 medical doctor who performed US examinations, 1 nurse, 1 anesthesiologist (for interventional procedures), 1 medical doctor who coordinated contact and health care procedures with the local hospital and 1 physiotherapist. In agreement with the Chinese law, all medical aid workers had presented certification to the Office of Public Hygiene of Yushu proving that they were legally qualified medical practitioners and signed a form.
US examination: a portable US machine “SonoSite 180 Plus” equipped with a 3.5–5 MHz convex probe and color Doppler US mode for abdominal examination and post-interventional follow-up, was borrowed from the company Esaote-Medmark, Trezzano sul Naviglio, Italy, in 2007. Later, in 2009, this equipment was donated to the Medici Vicentini per il Mondo NPO by the “Sound Care” program. For interventional procedures such as puncture, aspiration and injection of scolicidal agent and re-aspiration (PAIR) and US guided catheterization, the US equipment belonging to the Yushu People's Hospital was used.
Patients: US examination was offered also to all children and staff personnel of the orphanage, including the teachers. The clinic of the “Yushu Medical School and Orphanage” is the only one available for the nomadic population of the area and the patients sometimes travel a long way to get to the clinic during the summer. Every morning there were long lines of people seeking medical help for themselves or their relatives as they were not able to pay for health care (Fig. 3). All patients were willing to undergo US examination and this was considered as a verbal informed consent to the procedure. No written consent was requested/obtained in view of the high illiteracy rate and the fact that US examination was part of a diagnostic and therapeutic process. No patient ever refused US examination. Some US examinations were performed in a nomadic tent village and in the house of some elderly patients. Generally, no written report was issued, but the US diagnosis was written in the patient's clinical file (Fig. 4).
Figure 3.

Patients waiting for US examination.
Figure 4.
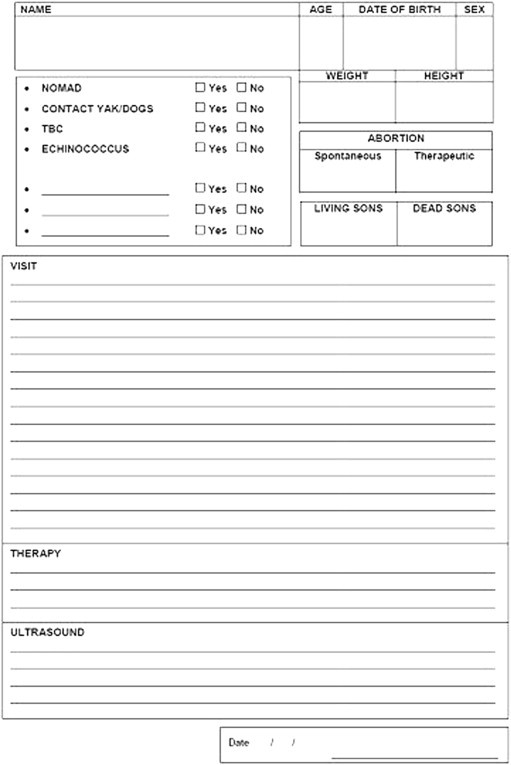
Clinical file.
A group of interpreters provided by ROKPA allowed interacting with the patients and the doctors of the hospital, none of whom spoke English; they translated into and from Tibetan and Mandarin Chinese. The visiting doctor who accompanied the sickest patients to the hospital presented the case to the local doctors. In some cases, the portable US machine with stored images of a case was brought to the hospital to discuss the images with the local doctors; this method proved a highly effective way to communicate with them. A written report was issued in English if the patients were referred to the Qinghay University Affiliated Hospital in Xining, Qinghay, PRC. For patients with echinococcosis, a special form was filled in. In a few cases long-distance medical follow-up was possible by telephone contact with a hospital doctor and some interpreters.
After an accurate explanation provided by a local doctor, written informed consent issued by the hospital in Chinese and Tibetan was obtained from patients who required interventional procedures. If the patient was illiterate, the form was signed by a literate member of the family. A copy of the agreement is kept by the hospital and another copy is kept by the Medici Vicentini per il Mondo NPO. All written material is kept in the archives of the Association as confidential material. After removing all sensitive data the images were downloaded using the appropriate program “Sonolink” installed in the US machine.
Results
The characteristics of the studied population and the main pathologies are reported in Table 1. The outcome of 22% of US examinations was classified as pathological. Table 3 lists the symptoms most frequently presented by the patients who contacted the clinic. The different pathologies are analyzed below with a description of some interesting cases which were diagnosed by US.
Table 1.
Outcome of US examinations.
| US examinations | 1128578 (2007) + 550 (2009) | |
|---|---|---|
| Patients | ||
| Mean age (years) | 38 (range: 2 months–82 years) | |
| Gender (male/female) | 438/690 | 1:2 |
| Results | ||
| Infections | 121 | 10.8 % |
| Cystic echinococcosis | 66 | 6.23% |
| Suspected multilocular echinococcosis | 2 | |
| Abscess | 4 | |
| Ascaridiasis | 2 | |
| Abdominal tuberculosis | 2 | |
| Cirrhosis | 8 | |
| Acute and chronic hepatitis | 35 | 3.10% |
| Gallstones (gall bladder and intrahepatic) | 112 | 9.92% |
| Abdominal masses | 12 | |
| Neoplastic lesions of the liver | 11 | |
| Mola vesicularis | 1 | |
| Various (malformation, hemangioma, simple cyst) | 48 | |
| Examinations yielding pathological outcome | 249 | 22% |
Table 3.
Main symptoms presented by the patients who were submitted to US.
| Symptoms | Patients | % |
|---|---|---|
| No symptom | 585 | 51.8% |
| At least one symptom | 543 | 48.1% |
| Abdominal pain | 275 | 24.3% |
| Jaundice | 36 | 3.1% |
| Nausea and vomiting | 199 | 17.6% |
| Swelling of the abdomen | 89 | 7.8% |
| Fever | 54 | 4.7% |
| Weight loss | 41 | 3.6% |
| Diarrhea | 112 | 9.9% |
| Other symptoms (itching, skin lesions, fatigue, hemoptysis, hematuria, constipation, abnormal menstrual cycle) | 187 | 16.5% |
Hepatic steatosis and cholelithiasis
The Tibetan patients frequently had a hyperechoic and enlarged liver with findings suggestive of steatosis. Steatosis, particularly when associated with obesity, can be attributed to food which is too rich in fat and poor in vitamins [3]. However, US does not distinguish steatosis from fibrosis, so part of these patients might have fibrosis caused by viral hepatopathy (see below). Liver cirrhosis was suspected when the patient was not obese and US examination revealed hilar lymph nodes, splenomegaly and an irregular liver echo texture.
Cholelithiasis is often associated with steatosis in obese patients thereby suggesting a possible common metabolic origin. However, this disease was very frequent (112 cases; 9.9% of patients) and also present in patients who were not overweight or carriers of other metabolic risk factors.The gall stones were morphologically similar to those which are seen in Italian clinics, with the exception that they were frequently associated with intrahepatic calcifications which was a common finding. These findings are probably suggestive of previous parasitism. In the children of the orphanage and more often in those who were beggars, ascaridiasis was frequently detected, although only two patients presented images of live worms in the biliary tree.
Chronic hepatitis, cirrhosis, hepatocellular carcinoma (HCC)
Hepatitis B virus is widespread in Tibet. The exact prevalence of hepatitis B in Yushu is not known, but the problem is known and some organizations are conducting programs for the diagnosis and treatment in collaboration with the Chinese health authorities [5]. Some of the patients involved in this program were aware of their infection, as tests for hepatitis B surface antigen (HBsAg) can be performed at the hospital in Yushu. In other patients the finding of an inhomogeneous liver, sometimes with focal lesions, led to diagnostic suspicion of chronic viral hepatitis. Abnormalities suggestive of chronic hepatitis were found in 3.2% of patients examined. In 8 cases there was a US picture highly suggestive of cirrhosis, sometimes with ascites.
Alcoholism is rarely the cause of chronic liver disease among the nomadic people in this area, but alcoholism exists in the city although it is punishable by law. Urbanization has led to more widespread alcoholism, smoking and gambling and also to the spread of diseases such as tuberculosis, which is favored by overcrowding.
One of our young interpreters, a leader of the organization, was diagnosed chronic HBV-related hepatitis. US showed a 5 cm lesion situated in the right lobe of liver segment VI. She received locoregional therapies in Xining, but the disease progressed with rapidity and she died in December 2009.
The local prevalence of hepatitis C is not known, but it is present in Tibet [6].
Tuberculosis
Tuberculosis is a well known problem throughout Asia and particularly in Tibet, Nepal and Mongolia [7]. Poverty and malnutrition associated with overcrowding and urbanization favor the spread of this disease. The International Red Cross and the Damian Foundation (www.damianfoundation.org) working in Yushu since 2009 distribute free medication, which may not always be immediately available. Several patients presenting to our clinic with hemoptysis and other typical symptoms (weight loss and poor appetite) were referred to the clinics run by these organizations.
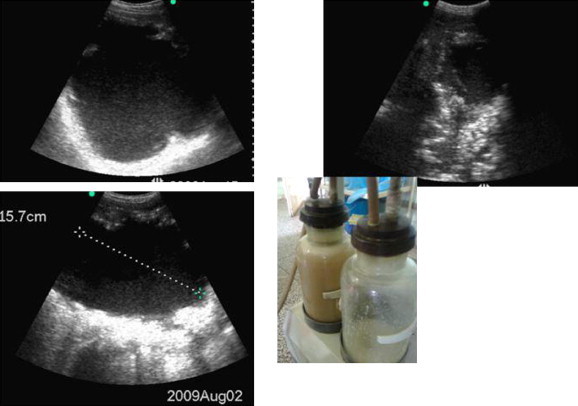
A clinical case: A 49-year-old patient with a large abscess (Fig. 5) was rushed to the hospital in Yushu in a state of septic shock and quickly submitted to surgical drainage which yielded a large amount of purulent material. US image showed a considerable amount of corpusculated fluid mixed with gas due to the presence of anaerobic bacilli. The abundance of solid material suggests bacterial infection of a hydatid cyst. After surgery the patient slowly recovered, but at the time of our departure from Yushu he was still hospitalized.
Figure 5.
Hepatic abscess.
Echinococcosis
Given the frequent cases of echinococcus granulosus liver cysts diagnosed in the course of the US outreach program in 2007, a pilot project was launched in 2009 which included locoregional treatment of simple cases in collaboration with local physicians (Fig. 6). The preliminary results are summarized in Table 2. The prevalence of cystic lesions was 6.23% which is in agreement with other studies carried out in the same region [8,9].
Figure 6.
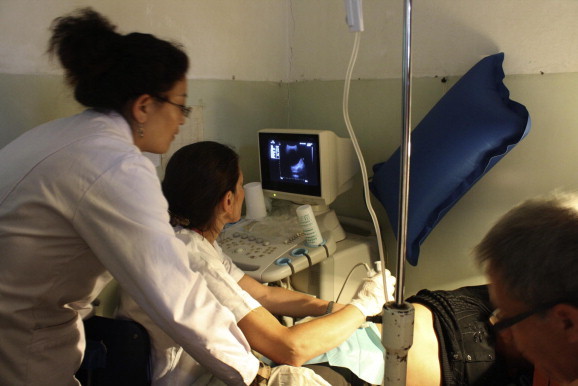
The medical team in action.
Table 2.
Screening for cystic echinococcosis.
| No | % | |
|---|---|---|
| Patients | 1058a | |
| Patients with cysts | 66b/1058 | 6.23 |
| Age (years) | 42 (range: 3–70) | |
| Sex ratio (male/female) | 24/42 | 1:2.3 |
| Patients with active cysts (CE1–CE2) | 39/66 | 59% |
| Patients with transitional cysts (CE3 a/b) | 11/66 | 16.6% |
| Patients with inactive cysts (CE4–CE5) | 29/66 | 43.9% |
| Patients with active and inactive cysts | 10/66 | 15% |
Bold represents more relevant data.
Patients screened in 2007 are excluded from this calculation.
Several patients had more than one type of cyst.
Echinococcus granulosus liver cysts are found in patients in all stages of life (Fig. 7) and often in children and adolescents who have already undergone surgery several times for this pathology. This suggests that the infection is still spreading and that control measures are needed. The only treatment which is available locally is surgery of complicated cases, and relapse is frequent.Multilocular echinococcosis (ME) was suspected in some cases, but it was not possible to diagnose with certainty because appropriate serology tests were not available. ME may be difficult to differentiate from cancer and this diagnostic problem can sometimes not be solved by US alone. Patients with suspected ME were referred to the University Clinic in Xining.
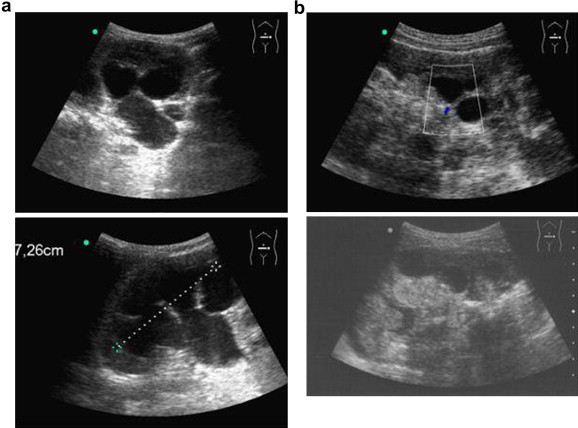
Figure 7.
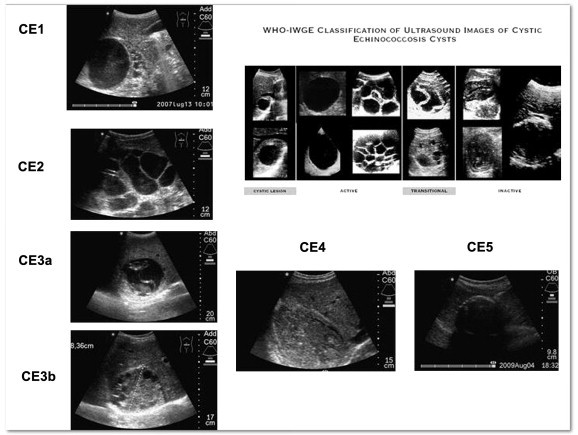
Cases of cystic echinococcosis in different stages of life in Yushu, and WHO-IWGE classification.
Malformation and neoplastic lesions
Patients with obvious physical defects, such as polio victims and children with congenital brain damage, hydrocephalus and cleft palate were often examined at the clinic. A little girl hosted by the orphanage was affected by megacalicosis (Fig. 8a); one US examination was sufficient to differentiate this pathology from cysts and neoplastic lesions. US revealed space-occupying lesions in the liver in 11 patients. The presence of intralesional vascularity on color Doppler allowed diagnosis in cases of doubt.
Figure 8.
Megacalicosis (a) trophoblastic tumor (b).
Pregnancy and molar pregnancy
The US equipment was not used for obstetric purposes. In some cases pregnancy was incidentally revealed and the patient was referred to the local obstetric care. A young patient reported that she did not feel fetal movements despite her advanced pregnancy and was found to be suffering from trophoblastic neoplasia (Fig. 8b). She was referred to the hospital for further investigation and surgery.
Discussion
Since 2003 the medical clinic in Yushu has been a stable point of reference for the local population, as it allows the nomadic people to seek help for at least some emergencies although they do not have access to health care. However, the clinic can only deal with basic, uncomplicated diseases, and the more difficult cases are referred to the local hospital. Coverage of expenses for drugs, diagnostic examinations and hospital stay as well as surgery should be guaranteed though, as the nomadic population is generally unable to pay. These problems are common among nomadic peoples who often require health care as they are frequently affected by neglected zoonotic diseases [10]. On the other hand, the recent history of our own country has taught us that improved living conditions and nutrition is associated with reduction and sometimes disappearance of many diseases, especially infectious diseases.
Before 2007, US was the most frequently requested examination at the local hospital. However, the US equipment obtained in connection with the current program made it possible to transfer the funds previously spent on US examinations to the care of the patients. The elevated number of pathological findings (22% of examinations yielded pathological outcome) shows that the studied population needs urgent intervention and preventive care [11,12] and that the role of US is essential in the diagnosis of diseases of high prevalence such as echinococcus cysts [13].
Many patients were symptomatic (48.1% of cases); the most frequently encountered symptoms were abdominal pain, fever, jaundice, weight loss and swelling of the abdomen (Table 3).
US permitted diagnosis of the most frequent diseases in loco [14]. More than 40% of patients with pathological ultrasound findings were affected by infectious diseases (echinococcosis, hepatitis, tuberculosis).
Through screening and cooperation it should be possible to offer the studied populations continuous preventive and therapeutic treatment [15]. It is well known that certain infections including echinococcosis can be identified at US screening [13], that these diseases can be cured also in a context of limited resources [16] and that most of them can be prevented. Particularly echinococcosis can be controlled through preventive measures such as health education and veterinary safety controls [17].
US screening permits an estimation of the prevalence of the disease and identification of its active forms, it is a valuable tool for management planning and for selecting patients who require locoregional treatment and for treatment guidance [18]. In some patients, familiarity with the US patterns of deformations and neoplastic lesions was essential for making a correct differential diagnosis of infectious diseases. In particular, the “mola vesicularis” which is characterized by a “soap bubble” pattern and other trophoblastic tumors are frequent findings in developing countries [19] as they are associated with a high birth rate. If these neoplastic lesions are identified early, they can be removed and the patient will have a good prognosis, whereas they can be lethal because of severe hemorrhage and malignant transformation if they are identified too late.
Conclusions
Ultrasound is an essential diagnostic tool in a context of limited resources [20]. In our experience US was accepted without difficulty, and its use was integral to clinical practice. Further studies and exchange of experience are required to set up programs which address the health problems of the populations living in extreme poverty.
Conflicts of interest
The authors have no conflict of interest to disclose.
Acknowledgement
The authors thank Medmark SRL (Trezzano sul Naviglio) for generously lending the US machine in 2007 and for technical assistance, and also the Sound Care Foundation (Bothell, WA) for the donation of the US machine in 2009. Thank you also to all the volunteers of ROKPA.
Footnotes
Award for the best oral presentation at the XXII SIUMB National Congress.
Appendix A. Supplementary data
References
- 1.Feng J., Wang T., Xie C. Eco-environmental degradation in the source region of the Yellow River, Northeast Qinghai-Xizang Plateau. Environ Monit Assess. 2006;122(1–3):125–143. doi: 10.1007/s10661-005-9169-2. [DOI] [PubMed] [Google Scholar]
- 2.Wang H., Cui Y., Wang Z., Wang X., Guo Z., Yan Y. A dog-associated primary pneumonic plague in Qinghai Province, China Clin Infect Dis. 2011;52(2):185–190. doi: 10.1093/cid/ciq107. [DOI] [PubMed] [Google Scholar]
- 3.Wu T. The Qinghai–Tibetan plateau: how high do Tibetans live? High Alt Med Biol. Winter. 2001;2(4):489–499. doi: 10.1089/152702901753397054. [DOI] [PubMed] [Google Scholar]
- 4.Foggin P.M., Torrance M.E., Dorje D., Xuri W., Marc Foggin J., Torrance J. Assessment of the health status and risk factors of Kham Tibetan pastoralists in the alpine grasslands of the Tibetan plateau. Soc Sci Med. 2006;63(9):2512–2532. doi: 10.1016/j.socscimed.2006.06.018. [DOI] [PubMed] [Google Scholar]
- 5.Zhao S.M., Li H.C., Lou H., Lu X.X., Yu X.F., Gao D.H. High prevalence of HBV in Tibet, China. Asian Pac J Cancer Prev. 2001;2(4):299–304. [PubMed] [Google Scholar]
- 6.Jia L., Yu J., Yang J., Song H., Liu X., Wang Y. HCV antibody response and genotype distribution in different areas and races of China. Int J Biol Sci. 2009 Jun 13;5(5):421–427. doi: 10.7150/ijbs.5.421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang L.D. Tuberculosis control in China and its prospect. Zhonghua Jie He He Hu Xi Za Zhi. 2006 Aug;29(8):505–506. [PubMed] [Google Scholar]
- 8.Yu S.H., Wang H., Wu X.H., Ma X., Liu P.Y., Liu Y.F. Cystic and alveolar echinococcosis: an epidemiological survey in a Tibetan population in southeast Qinghai, China. Jpn J Infect Dis. 2008 May;61(3):242–246. [PubMed] [Google Scholar]
- 9.Schantz P.M., Wang H., Qiu J., Liu F.J., Saito E., Emshoff A. Echinococcosis on the Tibetan Plateau: prevalence and risk factors for cystic and alveolar echinococcosis in Tibetan populations in Qinghai Province, China. Parasitology. 2003:127. Suppl:S109-20. [PubMed] [Google Scholar]
- 10.Zinsstag J., Ould Taleb M., Craig P.S. Editorial: health of nomadic pastoralists: new approaches towards equity effectiveness. Trop Med Int Health. 2006 May;11(5):565–568. doi: 10.1111/j.1365-3156.2006.01615.x. [DOI] [PubMed] [Google Scholar]
- 11.Budke C.M., Jiamin Q., Qian W., Torgerson P.R. Economic effects of echinococcosis in a disease-endemic region of the Tibetan Plateau. Am J Trop Med Hyg. 2005 Jul;73(1):2–10. [PubMed] [Google Scholar]
- 12.Wang L.Y., Wu W.P., Li S.Z., Fu Q., Wang Q., Tian T. [The risk evaluation and response to the spread of hydatid disease after Yushu earthquake in Qinghai Province] Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi. 2010 Aug;28(4):315–317. [PubMed] [Google Scholar]
- 13.Macpherson C.N., Bartholomot B., Frider B. Application of ultrasound in diagnosis, treatment, epidemiology, public health and control of Echinococcus granulosus and E. multilocularis. Parasitology. 2003:127. doi: 10.1017/s0031182003003676. Suppl: S21-35. [DOI] [PubMed] [Google Scholar]
- 14.Groen R.S., Leow J.J., Sadasivam V., Kushner A.L. Review: indications for ultrasound use in low- and middle-income countries. Trop Med Int Health. 2011 Sep 1 doi: 10.1111/j.1365-3156.2011.02868.x. [DOI] [PubMed] [Google Scholar]
- 15.Crump J.A., Sugarman J., Working Group on Ethics Guidelines for Global Health Training (WEIGHT) Ethics and best practice guidelines for training experiences in global health. Am J Trop Med Hyg. 2010;83(6):1178–1182. doi: 10.4269/ajtmh.2010.10-0527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brunetti E., Schantz P.M., Zeyhle E., Filice C. Treatment of echinococcosis at rural hospital level in Africa. Trop Doct. 2003;33(1):58–59. doi: 10.1177/004947550303300130. [DOI] [PubMed] [Google Scholar]
- 17.Nori M. China Proceedings of the International Congress on Yak, Chengdu, Sichuan, PR 2004. 2004. Providing support to the para-veterinary service in Tibetan areas: the case of ASIA project in Chengduo county, Yushu Tibetan Autonomous Prefecture, Qinghai Province. [Google Scholar]
- 18.Brunetti E., Garcia H.H., Junghanss T. International CE Workshop in Lima, Peru, 2009. Cystic echinococcosis: chronic, complex, and still neglected. PLoS Negl Trop Dis. 2011 Jul;5(7):e1146. doi: 10.1371/journal.pntd.0001146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Green C.L., Angtuaco T.L., Shah H.R., Parmley T.H. Gestational trophoblastic disease: a spectrum of radiologic diagnosis. Radiographics. 1996;16(6):1371–1384. doi: 10.1148/radiographics.16.6.8946542. [DOI] [PubMed] [Google Scholar]
- 20.Maru D.S., Schwarz R., Jason A., Basu S., Sharma A., Moore C. Turning a blind eye: the mobilization of radiology services in resource-poor regions. Glob Health. 2010;6:18. doi: 10.1186/1744-8603-6-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


