Abstract
Rotavirus enteritis is an infectious disease of the small bowel caused by an RNA reovirus. It is manifested by cytotoxic diarrhea [1]. Rotavirus is the most common viral cause of enteritis (incidence 15–35%) [2]. In infants and children with abdominal pain and diarrhea, ultrasonography is the diagnostic study of choice, and its use has increased significantly in young patients. We describe two cases in which portal-vein gas was detected on abdominal ultrasound scans in children with severe dehydration secondary to rotavirus gastroenteritis, which resolved rapidly after treatment.
Keywords: Ultrasound, Rotavirus, Portal-vein gas
Sommario
L’enterite da Rotavirus è una patologia virale del piccolo intestino dovuta ad un RNA reovirus e si manifesta con diarrea citotossica. Il Rotavirus è fra le più comuni cause di enterite. Nei neonati e nei bambini con dolore addominale e diarrea l’ecografia è considerata la metodica di scelta ed il suo impiego è significativamente cresciuto in questa tipologia di pazienti. Descriviamo due casi di pneumatosi portale in neonati con severa disidratazione da gastroenetrite virale, risoltasi rapidamente dopo il trattamento.
Introduction
Rotavirus is a relatively large (70-nm), nonenveloped, double-stranded RNA virus. It is the most common viral cause of enteritis (incidence 15-35%) in infants and children with abdominal pain and diarrhea. The infection is transmitted directly via the fecal-oral route and indirectly via respiratory droplets. The rotaviruses invade the mucosa of the small intestine and symptoms usually appear after an incubation period of 3 days. Ultrasonography is the diagnostic study of choice, and its use has increased significantly in young patients. Ultrasound examinations can detect gas in the portal vein and in the hepatic parenchyma, but there are very few reports of pneumatosis intestinalis and intrahepatic portal vein gas in patients with acute rotavirus infection. The apparent rarity of this association may be due to the rapid disappearance of sonographic evidence once the patient is treated. We describe two cases in which portal-vein gas was detected on abdominal ultrasound scans in children with severe dehydration secondary to rotavirus gastroenteritis, which resolved rapidly after treatment.
Case reports
Case 1
A 28-day-old female newborn was brought to the emergency department with a 2-day history of episodes of bloody diarrhea associated with loss of appetite, abdominal pain, mild weight loss, and crying. The child was in obvious distress and moderately lethargic. Physical examination revealed dry lips and oral mucosa and sunken eyes. Abdominal tenderness was noted, but there were no palpable abdominal masses. The body temperature was 38.8 °C.
Case 2
A 7-day-old female newborn was brought to the emergency department after two episodes of bilious vomiting, passage of feces mixed with blood, clinical deterioration, and onset of lethargy and drowsiness. There were no palpable abdominal masses. The body temperature was 38.5 °C.
Imaging studies
Both patients underwent plain film of the abdomen, which did not reveal any subdiaphragmatic free air or evidence of intestinal obstruction. Plain films were also negative for pneumatosis intestinalis and portal-vein gas (Fig. 1). We also performed abdominal ultrasound in both cases. The liver parenchyma contained numerous linear hyperechogenicities reflecting the presence of gas in the peripheral portal vessels. In the main portal branches, we could see numerous hyperechoic spots consistent with individual air bubbles moving in a hepatopetal direction (Fig. 2).
Fig. 1.

Case 1. Frontal view. Plain film showed no evidence of pneumatosis intestinalis or air in the portal veins.
Fig. 2.
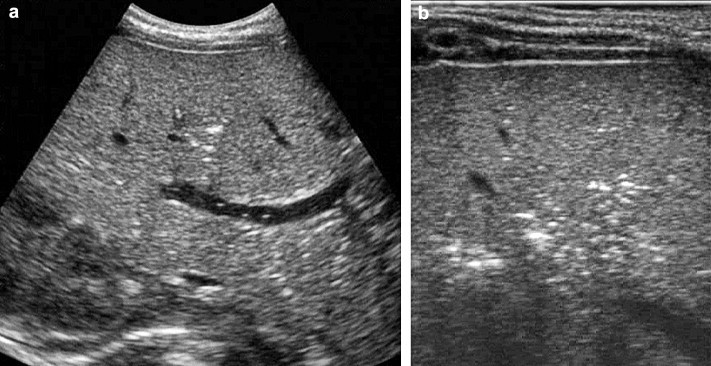
a–b. Case 1. Longitudinal US scan of the liver shows intraparenchymal streak-like echogenicities and mobile echogenic points in the portal trunk (a). Punctate intraparenchymal echogenicities as visualized with linear transducers (b).
Color Doppler ultrasound clearly confirmed the presence of gas in the perivascular spaces rather than in the biliary tract.
Intestinal ultrasound revealed isolated areas of air within the bowel wall (Fig. 3), which displayed normal stratification and thickness. Color Doppler studies showed the presence of normal bowel-wall vascularization with no signs of ischemia.
Fig. 3.
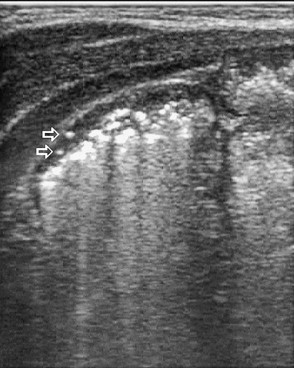
Case 2. Pneumatosis intestinalis is reflected by the presence of punctate echogenicity within the bowel wall (arrows).
Ultrasonography repeated 24 h after rehydration therapy, which produced rapid clinical improvement. The examination revealed significantly reduced amounts of gas in the main portal veins and their peripheral branches (Fig. 4). There was no evidence of intestinal-wall pneumatosis.
Fig. 4.
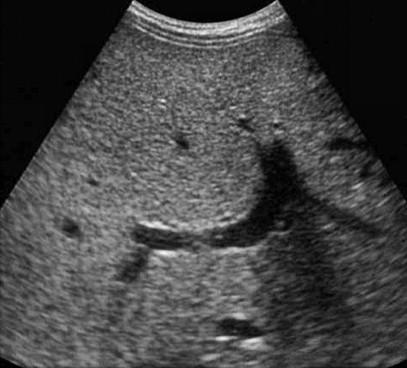
Case 1. Ultrasonography performed 24 h after rehydration shows a significant reduction in echogenicities within the peripheral portal vessels and in the major portal branches.
The presence of rotavirus infection in these two patients was confirmed by rotavirus antigen in the stool. The patients were discharged with a diagnosis of severe rotavirus gastroenteritis.
Informed consent was obtained from the patients for publication of these case reports.
Discussion
Rotavirus is a relatively large (70-nm), nonenveloped, double- stranded RNA virus. Its name refers to the wheel-like appearance it presented when it was observed for the first time in 1973 under an electron microscope [3]. Rotavirus is the most common viral cause of enteritis (incidence 15–35%). The main risk factor is age (most cases are seen in children <2 years, and the infection is uncommon after 4 years of age). Eighty percent of cases occur during the winter season, and 20% during the summer. The infection is transmitted directly via the fecal-oral route and indirectly via respiratory droplets, and symptoms usually appear after an incubation period of 3 days. The rotaviruses invade the mucosa of the small intestine [1].
Infection is common, and extraintestinal complications occur in rare cases. Minor hepatic involvement is commonly seen during acute infection, with elevations of serum transaminase values. More severe hepatic involvement may occur in patients with immune deficiency [4] and those with liver transplants.
There are very few reports of pneumatosis intestinalis and intrahepatic portal-vein gas in patients with acute rotavirus infection [5]. The apparent rarity of this association may be due to the rapid disappearance of sonographic evidence once the patient is treated. Ultrasound examinations can detect gas in the portal vein (and it is more effective that plain abdominal films for this purpose) and in the hepatic parenchyma [6].
In our patients, gas probably entered the portal vein and liver parenchyma as a result of severe damage to the gastrointestinal mucosa caused by the rotavirus infection. Gas within the bowel lumen was forced through the damaged bowel mucosa and reached the liver through the portal circulation.
Although the pneumatosis intestinalis has been previously described in children with rotavirus gastroenteritis [5], it was identified on plain abdominal radiographs. Ultrasound examinations were not performed. In our cases, ultrasound showed the presence of bowel-wall pneumatosis although the amount of air observed was very small. However, there were no other signs of bowel-wall damage (thickening, alteration of normal stratification, signs of ischemia), which are often seen in cases of necrotizing enterocolitis (NEC). NEC is another possible cause of portal-vein pneumatosis in newborns [7], so it is important to distinguish whether the presence of gas in the portal vein is due to this condition or to other potentially less aggressive diseases such as rotavirus infection.
In our two patients, simple intravenous rehydration produced rapid clinical improvement, and this response, along with the absence of bowel-wall alterations on color Doppler ultrasound, was sufficient to exclude NEC as the cause of the portal-vein pneumatosis.
The early and widespread use of ultrasonography for the work-up of acute abdominal emergencies in infants and children may lead to more frequent diagnoses of gas in the portal vein. Since this finding is a sign that usually indicates serious intra-abdominal pathology (often requiring emergency surgery) [8], is important to distinguish cases of benign hepatic portal-vein gas, which are due to diseases that are less dangerous and can be treated conservatively.
Ultrasonography can lead to early detection not only of portal-vein pneumatosis but also other signs that may be diagnostically informative.
Conflict of interest statement
The authors have no conflict of interest.
Supplementary data
References
- 1.De Marco G., Bracale I., Buccigrossi V., Bruzzese E., Canani R.B., Polito G. Rotavirus induces a biphasic enterotoxic and cytotoxic response in human-derived intestinal enterocytes, which is inhibited by human immunoglobulins. J Infect Dis. 2009;200(5):813–819. doi: 10.1086/605125. [DOI] [PubMed] [Google Scholar]
- 2.Malek M.A., Curns A.T., Holman R.C., Fischer T.K., Bresee J.S., Glass R.I. Diarrhea- and rotavirus-associated hospitalizations among children less than 5 years of age: United States, 1997 and 2000. Pediatrics. 2006;117(6):1887–1892. doi: 10.1542/peds.2005-2351. [DOI] [PubMed] [Google Scholar]
- 3.Jayavasu C., Hooniwat Y., Sagaunwong S., Jayavasu J., Chatiyanonda K. A long term study of rotavirus infection in Thai infants and children with diarrhoea. Southeast Asian J Trop Med Public Health. 1982;13(3):373–376. [PubMed] [Google Scholar]
- 4.Gilger M.A., Matson D.O., Conner M.E., Rosenblatt H.M., Finegold M.J., Estes M.K. Extraintestinal rotavirus infections in children with immunodeficiency. J Pediatr. 1992;120(6):912–917. doi: 10.1016/s0022-3476(05)81959-6. [DOI] [PubMed] [Google Scholar]
- 5.Morrison S.C., Czinn S.J. Portal vein gas associated with rotavirus infection. J Pediatr Gastroenterol Nutr. 2001;33(5):626–628. doi: 10.1097/00005176-200111000-00024. [DOI] [PubMed] [Google Scholar]
- 6.Bomelburg T., von Lengerke H.J. Intrahepatic and portal venous gas detected by ultrasonography. Gastrointest Radiol. 1992;17(3):237–240. doi: 10.1007/BF01888557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Miele V., Bibbolino C., Mazzoni G., Calisti A., Adami L. Neonatal necrotizing enterocolitis. Ultrasonographic findings of gas in the portal vein in two cases. Radiol Med. 1999;97(4):313–314. [PubMed] [Google Scholar]
- 8.Hussain A., Mahmood H., El-Hasani S. Portal vein gas in emergency surgery. World J Emerg Surg. 2008;3:21. doi: 10.1186/1749-7922-3-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


