Abstract
Breast augmentation and breast reconstruction are increasingly common operations. All radiologists need to be able to recognize the normal appearances of the more commonly used implants on various imaging modalities and breast radiologists in particular are facing new challenges when imaging the women involved. This work aims to review the normal and abnormal findings in women undergoing breast implant surgery using ultrasonography, mammography, and magnetic resonance imaging.
Keywords: Breast implants, Mammography, Ultrasound, Magnetic resonance imaging, Breast implant rupture
Sommario
Gli interventi chirurgici additivi e di ricostruzione della mammella sono sempre più comuni. Tutti i radiologi dovrebbero essere in grado di riconoscere, attraverso le varie metodiche, il normale aspetto delle protesi mammarie più spesso utilizzate; in particolar modo i radiologi che si occupano di diagnostica senologica. Scopo di questo lavoro è quello di ricapitolare gli aspetti radiologici, normali e patologici delle protesi mammarie, agli esami ecografici, mammografici e di risonanza magnetica.
Introduction
The first silicone breast prosthesis was used in the early sixties. Multiple variations and changes have been made to the structure and contents of the breast implant over the years. Indications include dissatisfaction with the size of the breast, or with increasing ptosis and flattening of the breast after pregnancy or with increasing age. Occasionally, women have congenital absence or underdevelopment of one breast and may request unilateral, rather than bilateral surgery, to correct this asymmetry. Breast reconstruction is now commonly undertaken following mastectomy for breast carcinoma or prophylactic mastectomy for women at high risk of developing malignant breast disease. A working knowledge of the more common breast implant types is essential for accurate interpretation of mammographic (XR-mammography), ultrasound and magnetic resonance images (MRI). The single lumen silicone gel-filled implant is the most common silicone prosthesis and silicone is very radiopaque. This prosthesis consists of a silicone elastomer shell filled with silicone gel. The elastomer shell can be smooth or textured. A textured shell is “roughened” by the creation of tiny finger-like projections in the shell. Texturing was introduced to decrease the incidence of breast hardening or capsular contractions. Silicone implants may be placed behind the breast or beneath the pectoral muscle (subpectoral); in patients with little or no breast tissue, the implant contour may be visible and the edge palpable if placed behind the breast. Therefore subpectoral implants have been advocated for small-breasted women and for post-mastectomy reconstruction to achieve cosmetic improvement [1,2]. Also subpectoral placement has been advocated to avoid masking recurrent carcinoma in post-mastectomy patients. Double-lumen implants are occasionally seen and are composed of both silicone and saline. The bilumen implant consists of a small outer lumen of saline surrounding a larger inner lumen of silicone gel. The expander implant is the reverse, consisting of an outer lumen of silicone gel and an inner expandable lumen of saline. Expander type implants can be gradually filled through a subcutaneous port and tubing, designed to aid in breast reconstruction after mastectomy. Saline implants are another implant type that consist of an outer silicone elastomer shell filled with saline. A valve is usually present that allows for the adjustment of size of the saline implant. Saline implants are less radiopaque than silicone ones. When an implant is placed, a fibrous capsule forms around it, essentially representing the layer of scar tissue that forms around any device implanted in the body [3].
Radiologists need to be able to recognize the normal appearance of the more commonly used implants on various imaging modalities and to be able to detect breast implant complications.
Rupture of a breast implant and leakage of silicone are thus important complications, and the most important factor predisposing to rupture is age of the implant. The clinical observation that older implants are more likely to rupture is consistent with results of mechanical studies, which suggest a weakening of the implant shell with increasing time after implantation [4,5]. There are two types of rupture: intracapsular rupture, in which a tear or disruption of the shell occurs such that a significant portion of the silicone gel lies outside the shell but within the capsule and the shell collapses into the gel to varying degrees; extracapsular rupture, when there is displacement of silicone gel from a ruptured implant through the fibrous scar or capsule into the adjacent tissues, often caused by a strong external force. There are several reasons for implant rupture described in the literature. Although cases of iatrogenic rupture after manual compression or compression during mammography are reported as well as rupture secondary to trauma, most implant ruptures have no obvious traumatic origin and seem to occur over time [6,7]. It is difficult to diagnose rupture on clinical examination based solely on non-specific findings such as palpable nodules, asymmetry or tenderness. Because of concerns about the potential dangers of rupture and leakage of implants, radiologists are often asked to evaluate the integrity of silicone implants.
All examinations begin with the patient interview. Detailed questions are asked concerning her breast implant history including date of implantation, type of implant, additional surgeries or complications, history of rupture, reason for placement, and symptoms. Symptoms can include pain; palpable, masses in the axilla, breast or chest wall; or change in size, shape, or texture of the breast. The presence of symptoms is not a reliable predictor of rupture: Robinson and colleagues found a frequency of rupture of 72% among women with symptoms versus 71% among women without symptoms [8].
The aim of this work is to provide diagnostic criteria to be applied in the evaluation of breast implants. In breast implants ultrasound imaging has to be regarded as first level examination; in fact it is a non-invasive, cheap and easily available technique whereby usually well accepted by patients. It can be performed by using a high resolution unit with a linear array transducer centered at 7,5–10 MHz and tissue harmonic imaging, with the patient in the supine position with her ipsilateral arm raised behind her head to examine the medial part of the breast, while the lateral part of the breast is best studied by using oblique position of the patient. Breast ultrasound can often be a valid means to diagnose problems concerning breast implants. Nevertheless its performance requires so much as an accurate knowledge of breast both benign and malignant disorders as of breast implants imaging features. Furthermore it is extremely important to know ultrasound limits and pitfalls, which can lead to regrettable misdiagnosis. Therefore all doubtful cases should always be investigated through breast MRI. Anyway, in the integrated breast imaging, physicians should remind that patients with breast implants as women without implants should always undergo breast ultrasound and traditional XR-mammography, the latter only in case of appropriate age, as first level examination. Detection of breast cancer is the first indication to XR-mammography, but this technique can also provide informations about implants integrity, showing such alterations as capsule deformity, extracapsular rupture but no intracapsular rupture because of high density of silicone, which hides internal structures of implants. XR-mammography should be performed with standard craniocaudal and mediolateral oblique views; “Eklund view” with posteriorly displacing of implants aids better tissue detail [9].
Breast MRI needs a field strength of at least 1 T to avoid diagnostic accuracy impairment; in our Department both 1.5 T and 3 T magnets are available. MRI is performed with bilateral breast surface coil and the patient in the prone position. Our imaging protocol includes for 1.5 imager: transverse T2w fat suppressed (TIRM) and axial T2 with silicone suppression; transverse three dimensional dynamic T1w gradient-echo (GRE) acquired before and five time after contrast agent administration. The imaging parameters for the T1w GRE sequence were identical for all patients with repetition time: 8.1msec, echotime: 4 ms, flip angle: 30°; one signal acquired; rectangular field of view of ≤36 cm and matrix: 496 × 512. The section thickness is 1.5 mm for each patient. To eliminate the signal from fat, image subtraction (contrast-enhanced-unenhanced) is used. To evaluate breast implant integrity no contrast agent is required, although it can be useful to detect inflammatory changes around implants and it is almost necessary to depict cancer arising behind and near the implant. For this reason contrast agent is mandatory in case of patients with previous diagnosis of breast cancer, in order to better detect breast cancer recurrence. Contrast agent administration (0.2 mmol/kg bodyweight) is via antecubital venous access at standard flow rate of 2/mL/sec followed by a 10 mL saline flush.
Diagnostic criteria of breast implants on XR-mammography, ultrasound and magnetic resonance
Mammography
Alterations most commonly detected by this technique are extracapsular rupture and capsular contractions. Extracapsular rupture cause silicone leakage which can be associated with granulomatous response and formation of painful nodules. For this reason extracapsular rupture should be assumed in case of presence of radiopaque material among breast tissue or farther in the axilla. Sometimes extracapsular silicone can mimic breast cancer therefore in this case extracapsular rupture should always be considered [10]. Regarding capsule contracture, occurring in 23–60% of patients, it is the most frequent cause of patient discomfort, radiographic signs are not always present but the typical appearance is a thicker profile capsule [9,10]. Usually diagnosis of intracapsular rupture is not possible, sometimes it can be suggested by a contour bulge (Fig. 1). Other abnormalities, observable on XR-mammography, are calcifications, which may depend on chronic inflammatory response and seroma.
Fig. 1.

Breast implant: intracapsular rupture. (a) Oblique mammogram of the right breast shows a contour bulge. (b) Ultrasound image shows the implant with multiple layers of the collapsed implant shell visible as sets of parallel echogenic lines (stepladder sign). (c) Axial T2 weighted image (TIRM) shows lines of low-signal intensity internally, also known as the “linguine sign” and salad oil sign.
Ultrasounds
Breast ultrasound can identify implants integrity and abnormalities as capsular contracture, peri-implant fluid collection and extracapsular rupture but less reliably intracapsular rupture. The most reliable US sign of implants integrity is a completely anechoic interior (Fig. 2). The posterior interface may be difficult to visualize because of its depth.
Fig. 2.
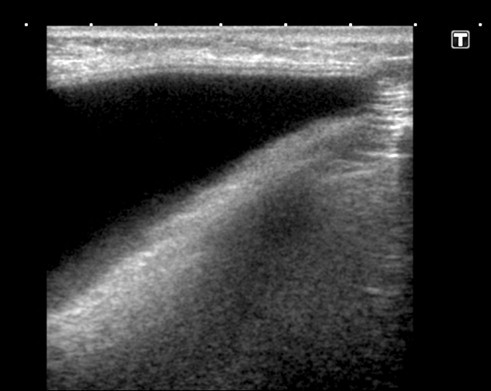
Normal submammary silicone breast prosthesis: ultrasound image shows the typical triangular, predominantly anechoic, appearance of an intact silicone breast prosthesis.
Ultrasonography can easily detect extracapsular rupture because of echogenic appearance of silicone among soft tissue, which is due to differences in acoustic impedance between silicone gel and soft tissue. In fact extracapsular rupture is characterized by extracapsular silicone which appears more often as hyperechoic nodules or hypoechoic nodule surrounded by hyperechoic tissue; this pattern is usually called as snowstorm. Less frequently extracapsular rupture has the appearance of an anechoic/hypoechoic mass. This aspect has been explained by two theories, the first suggests that this noise is caused by reverberations within and between tiny droplets of silicone in the breast parenchyma, the second proposes instead that this noise is caused by phase aberration [10,11]. Anyway echogenic pattern is the most frequent as bulge or hernia usually appear as anechoic and contiguous with the implant. In case of extracapsular rupture axilla evaluation can be recommended to detect either adenopathy or free silicone.
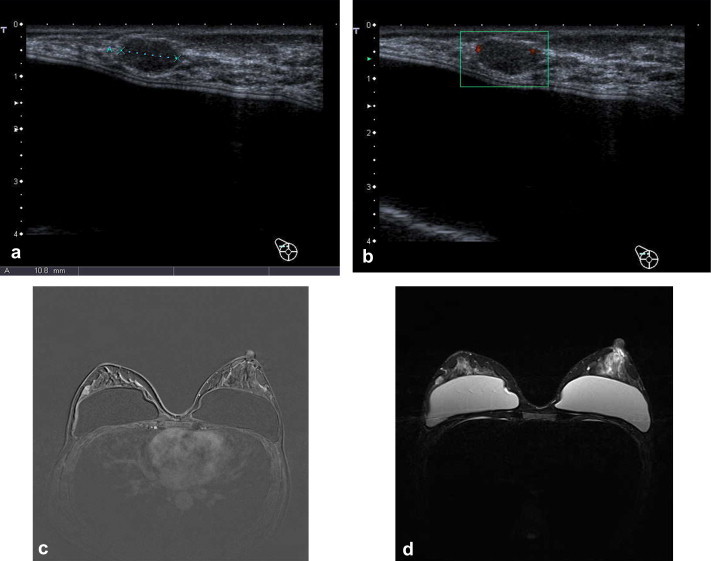
Intracapsular rupture is determined by shell rupture with silicone contained within fibrous capsule and it occurs more frequently than extracapsular rupture. Most significant US sign of intracapsular rupture are step ladder sign, consisting in discontinuous parallel echogenic lines, determined by the collapse of shell and echodense aggregates within the implant lumen [12] (Fig. 3). Further sign of intracapsular rupture is accumulation of low-level homogeneous echoes in the silicone gel probably due to influx of body fluids that mix with silicone producing a change in echotexture. Anyway central internal echoes can be caused even by implants infolding and they should be differenciated from intracapsular rupture, although it is not always easy particularly in case either of double-lumen implants or of implants with textured coatings.
Fig. 3.

Right breast ultrasound (a, b) reveals parallel hyperechogenic lines (step ladder sign) due into intracapsular rupture, confirmed at breast MRI (c).
Magnetic resonance imaging
Breast MRI might resolve diagnostic doubt especially in cases where with ultrasonography, it is difficult to distinguish between radial folds and intracapsular rupture. Linguine sign is the most common sign associated with intracapsular rupture. As previously mentioned, intracapsular rupture is determined by shell’s rupture with the capsule intact. This situation produces shell’s collapse and folds, represented by curvilinear hypointense lines. Other subtle signs of early intracapsular rupture are hypointense, subcapsular lines which are generated by minimal displacement of shell and are parallel to fibrous capsule and the teardrop sign which depends on displacement and invagination of shell. These signs, characteristics of implant rupture, should always be differentiated from normal findings in intact implants such as radial folds. In fact radial folds are infolding of normal implants which appear as hypointense lines emanating from the fibrous capsule-shell junction, they usually are thicker than linguine sign and always connect to the periphery of the implant. Another finding in case of intracapsular rupture is the so-called salad oil sign resulting from the mixing of the fluid around the implant and the internal silicone (Fig. 1). Extracapsular rupture can be suggested by the presence of silicone outside the capsule, which can be best and easily seen with silicone only sequences [13–15].
Even in patients among whom implants evaluation can be considered the main indication, actually the real main role of breast imaging is detection of breast cancer.
In case of breast implants report should include:
-
•
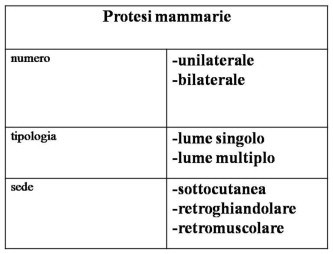
number, type and location of implants (Table 1) (Figs. 2,4–7);
-
•
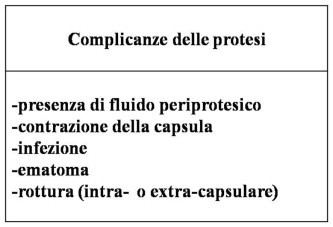
Any complications and implant failure (Table 2) (Figs. 1,3,8,9).
Table 1.
The table shows informations about breast implants.
| Breast implants | |
|---|---|
| number | unilateral |
| bilateral | |
| type | single lumen |
| multiple lumen | |
| location | subcutaneous |
| subglandular | |
| subpectoral | |
Fig. 4.

Axial T1 FLASH 3D, normal subpectoral breast implant of the left breast (single lumen).
Fig. 5.

Axial T2 weighted image of a double-lumen implant in the left breast.
Fig. 6.

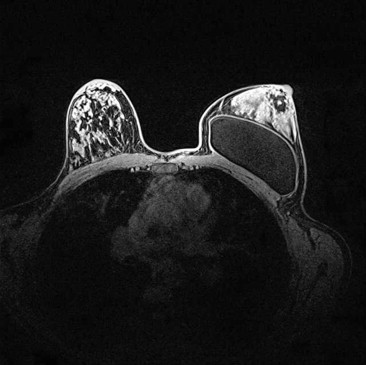
The patient (48 yo) with previous diagnosis of bilateral breast cancer (IDC) underwent bilateral mastectomy and breast implant positioning. MRI [axial T1 FLASH 3D (a), axial TIRM T2 (b) sequences] shows breast implants location.
Fig. 7.
Axial T1 weighted image of submammary silicone implant in a young patient with hypoplasia of the left breast.
Table 2.
The table shows a list of implants complications.
| Implants complications |
|---|
| -presence of peri-prosthetic liquid |
| -capsular contraction |
| -infection |
| -hematoma |
| -rupture (intra- or extracapsular) |
Fig. 8.

Contractures of breast with implant: ultrasound image shows a rounded implant shape instead of the typical triangular appearance.
Fig. 9.

Follow-up ultrasound in a patient with previous breast cancer and quadrantectomy detected the presence of peri-prosthetic fluid after two years by the surgery.
An accurate study of breast parenchyma and of peri-prosthetic regions is always mandatory to detect either breast cancer or cancer recurrence (Figs. 10–12).
Fig. 10.
Breast ultrasound (A,B) depicted suspicious nodule on the right breast in a patient previous underwent mammoplasty augmentation. The patient underwent MRI with contrast medium [axial T1 FLASH 3D (C), axial T2 TIRM (d)] which confirmed the presence of a doubtful nodule. Six months MRI follow-up revealed a dimensional increase of the nodule; at pathology it was proved be IDC (Invasive Ductal Carcinoma).
Fig. 11.
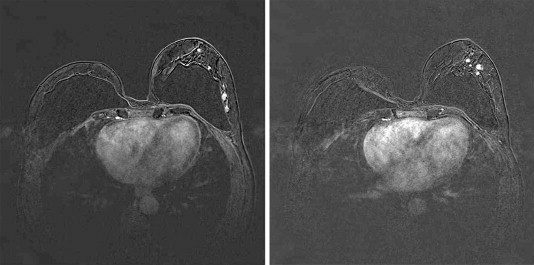
50 yo, woman with previous diagnosis of ILC (Invasive Lobular Carcinoma) of the right breast, the patient underwent right mastectomy and bilateral breast implants positioning. MRI, performed for breast implants evaluation detected a suspicious nodule on the controlateral breast (IDC, Invasive Ductal Carcinoma). The patient previous underwent negative ultrasound.
Fig. 12.

The patient with suspicious nodule at both XR-mammography and ultrasound underwent breast MRI which confirmed local breast cancer recurrence on the left breast.
Conclusions
Even in patients among whom implants evaluation can be considered the main indication, actually the real main role of breast imaging is detection of breast cancer.
Although there is no difference in tumor size, incidence of metastatic disease and stage between women with and without breast augmentation, sometimes a delay in breast cancer diagnosis can occur in women with breast implants. In fact mammographic evaluation can result more difficult and the presence of scar tissue complicates ultrasound imaging interpretation, above all in patients who previously underwent first mastectomy and then implant positioning. Since these patients are at increased risk for local recurrence and secondary cancer in the contralateral breast, all suspicious lesions must be investigated with breast MRI. In recent years contrast-enhanced magnetic resonance mammography has emerged as the most sensitive imaging modality for the detection and diagnosis of breast lesions [16–18].
Numerous studies have confirmed the superior diagnostic performance of contrast-enhanced magnetic resonance mammography compared to conventional mammography and ultrasound [17–19] and the greater potential of the method for effective cancer screening in women with high familial risk of breast cancer [17,20,21].
Ultrasound is the first level method in the evaluation of the prosthesis. Data in literature show a sensitivity of 77% and a specificity of 69% [22].
However, in some cases, ultrasound alone is not enough and the combination of different imaging techniques becomes an important diagnostic tool. MR imaging is generally accepted as the technique of choice for evaluating implant integrity, with a sensitivity of 72–94% and a specificity of 85–100%, depending on the applied MR study protocol and on the diagnostic criteria used for the definition of implant status [23,10].
In the breast implant evaluation clinical examination, XR-mammography and ultrasound can be used as the first examination in the follow-up of symptomatic and asymptomatic patients. MRI is the most sensitive technique and its utility seems to reside in better detection of intracapsular rupture and investigation of imaging findings suspicious at XR-mammography and US.
Conflict of interest statement
The authors have no conflict of interest.
Appendix A. Supplementary material
References
- 1.McDonald H.D. Reconstruction of the breast. In: Lippman M.E., Lichter A.S., Danforth D.N., editors. Diagnosis and management of breast cancer. Saunders; Philadelphia: 1988. pp. 468–485. [Google Scholar]
- 2.Chang W.H.J., Petry J.J., editors. The breast–an atlas of reconstruction. Williams & Wilkins Company; Baltimore: 1984. Augmentation mammoplasty; pp. 29–56. [Google Scholar]
- 3.Dowden R.V. Definition of terms for describing loss of gel from breast implants. AJR Am J Roentgenol. 1993;160:1360. doi: 10.2214/ajr.160.6.8498263. [DOI] [PubMed] [Google Scholar]
- 4.van Rappard J.H., Sonneveld G.J., van Twisk R., Borghouts J.M. Pressure resistance of breast implants as a function of implantation time. Ann Plast Surg. 1988;21:566–569. doi: 10.1097/00000637-198812000-00013. [DOI] [PubMed] [Google Scholar]
- 5.Greenwald D.P., Randolph M., May J.W., Ir Mechanical analysis of explanted silicone breast implants. Plast Reconstr Surg. 1996;98:269–275. doi: 10.1097/00006534-199608000-00008. [DOI] [PubMed] [Google Scholar]
- 6.Goin J. High-pressure injection of silicone gel into an axilla a complication of closed compression capsulotomy of the breast. Case report. Plast Reconstr Surg. 1978;62:891–895. doi: 10.1097/00006534-197812000-00013. [DOI] [PubMed] [Google Scholar]
- 7.de Camara D.L., Sheridan J.M., Kammer B.A. Ruptures and aging of silicone gel breast implants. Plast Reconstr Surg. 1993;91:828–834. [PubMed] [Google Scholar]
- 8.Robinson O.G., Bradley E.L., Wilson D.S. Analysis of explanted silicone implants: a report of 300 patients. Ann Plast Surg. 1995;34:1–7. doi: 10.1097/00000637-199501000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Gannot M.A., Harris K.M., Ilkhanipour Z.S., Costa-Greco M.A. Augmentation mammoplasty; normal and abnormal findings with mammography and US. Radiographics. 1992 Mar;12(2):281–295. doi: 10.1148/radiographics.12.2.1561417. [DOI] [PubMed] [Google Scholar]
- 10.O’Toole Melissa, CaskeT Cynthia I. Imaging spectrum of breast implant complications: mammography, ultrasound, and magnetic resonance imaging. Semin Ultrasound CT, MRI. October 2000;21(5):351–361. doi: 10.1016/s0887-2171(00)90029-5. [DOI] [PubMed] [Google Scholar]
- 11.Harris K.M., Ganott M.A., Shestak K.C., Losken H.W., Tobon H. Silicone implant rupture: detection with US. Radiology. 1993;187:761–768. doi: 10.1148/radiology.187.3.8497626. [DOI] [PubMed] [Google Scholar]
- 12.Caskey C.I., Berg W.A., Anderson N.D., Sheth S., Chang B.W., Hamper U.M. Breast implant rupture: diagnosis with US. Radiology. 1994;190:819–823. doi: 10.1148/radiology.190.3.8115633. [DOI] [PubMed] [Google Scholar]
- 13.Kaiser Werner A. Springer; May 2007. Signs in MR-mammography. [Google Scholar]
- 14.Glynn C., Litherland J. Imaging breast augmentation and reconstruction. Br J Radiol. 2008;81:587–595. doi: 10.1259/bjr/61567884. [DOI] [PubMed] [Google Scholar]
- 15.Soo M.S., Kornguth P.J., Walsh R., Elenberger C.D., Georgiade G.S. Complex radial folds versus subtle signs of intracapsular Rupture of Breast Implants: MR findings with surgical correlation. AJR Am J Roentgenol. 1996;166:1421–1427. doi: 10.2214/ajr.166.6.8633456. [DOI] [PubMed] [Google Scholar]
- 16.Fischer U., Kopka L., Grabbe E. Breast carcinoma: effect of preoperative contrast-enhanced MR imaging on the therapeutic approach. Radiology. 1999;213:881–888. doi: 10.1148/radiology.213.3.r99dc01881. [DOI] [PubMed] [Google Scholar]
- 17.Warner E., Plewes D.B., Shumak R.S., Catzavelos G.C., Di Prospero L.S., Yaffe M.J. Comparison of breast magnetic resonance imaging, mammography, and ultrasound for surveillance of women at high risk for hereditary breast cancer. J Clin Oncol. 2001;19:3524–3531. doi: 10.1200/JCO.2001.19.15.3524. [DOI] [PubMed] [Google Scholar]
- 18.Sardanelli F., Giuseppetti G.M., Panizza P., Bazzocchi M., Fausto A., Simonetti G. Sensitivity of MRI versus mammography for detecting foci of multifocal, multicentric breast cancer in fatty and dense breasts using the whole-breast pathologic examination as a gold standard. AJR Am J Roentgenol. 2004;183:1149–1157. doi: 10.2214/ajr.183.4.1831149. [DOI] [PubMed] [Google Scholar]
- 19.Van Goethem M., Schelfout K., Dijckmans L., Van Der Auwera J.C., Weyler J., Verslegers I. MR mammography in the pre-operative staging of breast cancer in patients with dense breast tissue: comparison with mammography and ultrasound. Eur Radiol. 2004;14:809–816. doi: 10.1007/s00330-003-2146-7. [DOI] [PubMed] [Google Scholar]
- 20.Kriege M., Brekelmans C.T., Boetes C., Besnard P.E., Zonderland H.M., Obdeijn I.M. Efficacy of MRI and mammography for breast-cancer screening in women with a familial or genetic predisposition. N Engl J Med. 2004;351:427–437. doi: 10.1056/NEJMoa031759. [DOI] [PubMed] [Google Scholar]
- 21.Kuhl C.K., Schrading S., Leutner C.C., Morakkabati-Spitz N., Wardelmann E., Fimmers R. Mammography, breast ultrasound, and magnetic resonance imaging for surveillance of women at high familial risk for breast cancer. J Clin Oncol. 2005;23:8469–8476. doi: 10.1200/JCO.2004.00.4960. [DOI] [PubMed] [Google Scholar]
- 22.Di Benedetto G., Cecchini S., Grassetti L., Baldassarre S., Valeri G., Leva L. Comparative study of breast implant rupture using mammography, sonography, and magnetic resonance imaging: correlation with surgical findings. Breast J. 2008;14:532–537. doi: 10.1111/j.1524-4741.2008.00643.x. [DOI] [PubMed] [Google Scholar]
- 23.Ikeda D.M., Borofsky H.B., Herfkens R.J., Sawyer-Glover A.M., Birdwell R.L., Glover G.H. Silicone breast implant rupture: pitfalls of magnetic resonance imaging and relative efficacy of magnetic resonance, mammography, and ultrasound. Plast Reconstr Surg. 1999;104:2054–2062. doi: 10.1097/00006534-199912000-00016. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


