Abstract
Introduction
Acquired renal arteriovenous fistulas (AVFs) include those that occur as a complication of renal biopsy.
Case report
The authors report the case of a woman with recent-onset grade I hypertension, who was referred to our staff for sonographic studies of the kidneys and urinary tract. Laboratory data revealed microhematuria and proteinuria <0.5 g/24 h, and renal function was borderline (MDRD GFR 58 mL/min). Renal sonography of the left kidney revealed an anechoic, arboriform area at the level of the pelvis, which was suggestive of hydronephrosis. The color Doppler examination showed turbulent flow within the anechoic area, with high-velocity arterial flow and arterialization of the venous waveform at spectral analysis. Selective renal angiography later confirmed the presence of a middle renal AVF with pseudoaneurysm, which had been provoked by a renal biopsy performed over 10 years earlier in another center. Since the patient was currently in good health, the prescribed management consisted solely of close clinical and US follow-up.
Discussion
AV fistulas are among the most commonly diagnosed renovascular malformations. The case reported here underlines the importance of using color Doppler ultrasound when obstructive uropathy is suspected, especially in patients who have undergone renal biopsy.
Keywords: Renal arteriovenous malformations, Renal arteriovenous fistula, Pseudoaneurysm, Hydronephrosis
Sommario
Introduzione
Tra le fistole arterovenose (FAV) acquisite vi sono quelle che si formano quale complicanza dell’esecuzione di una biopsia renale.
Caso clinico
Gli autori riportano il caso di una paziente giunta in ambulatorio di ecografia nefrologica per l’esecuzione di un’ecografia dei reni e delle vie urinarie per un’ipertensione sistolica di I grado di recente insorgenza. Negli esami di laboratorio era presente microematuria con proteinuria <0.5 g/24 ore. La funzionalità renale risultava ai limiti inferiori della norma (FG 58 mL/min secondo la formula MDRD). L’esame ecografico evidenziava una formazione anecogena “arboriforme” centropielica a livello del rene sinistro suggestiva per idronefrosi. Il color Doppler mostrava viceversa presenza di flusso turbolento all’interno dell’area anecogena stessa, con flusso arterioso elevato e arterializzazione del flusso venoso all’analisi spettrale. La successiva angiografia renale selettiva confermava il sospetto ecografico di FAV mediorenale sinistra con pseudoaneurisma, conseguente ad una biopsia renale effettuata più di 10 anni prima presso altro Centro. Essendo la paziente in pieno benessere veniva consigliato un più stretto follow-up clinico-ecografico.
Discussione
Tra le malformazioni vascolari renali di non rara osservazione sono le FAV. Il caso descritto ribadisce l’importanza dell’impiego dell’eco color Doppler (ECD) nel sospetto di uropatia ostruttiva, per diagnosticare una FAV, specialmente nei pazienti già sottoposti a biopsia renale.
Introduction
The main renovascular malformations include cirsoid aneurysms and arteriovenous fistulas (AVFs), which can be congenital or acquired. Congenital AVFs are characterized by gross hematuria, hypertension, and abdominal bruits. They are often diagnosed (and sometimes repaired) during infancy-childhood. Acquired AVFs are often caused by trauma, surgery, cancer, or accidents (e.g., as a complication of renal biopsy) [1,2]. We report the case of an AVF involving the left kidney, which was diagnosed many years after a renal biopsy (RB) performed at another center.
Case report
A 73 year-old woman was referred to the renal ultrasonography outpatient unit for sonographic studies of the urinary tract. In 1990, she had undergone open-sky cholecystectomy with appendectomy, and in 2001 colpoperioneoplasty was performed for uterovaginal prolapse. In 2009, neck ultrasound revealed a multinodular parenchymal goiter involving both lobes of the thyroid and the isthmus region as well, which was subsequently confirmed by CT. She had grade 1 systolic hypertension, which had been diagnosed a few months earlier and was well controlled with bisoprolol and low-dose ARB therapy. Renal function was borderline with a serum creatinine 0.93 mg/dL and an MDRD GFR of 58 mL/min (normal:>60 mL/min).The urinalysis revealed mild proteinuria (<0.5 g/24 h, normal:<0.2 g/24 h) and hematuria (15 RBCs/microL – normal: <11).
The ultrasound examination showed an arboriform, anechoic area in and around the pelvis of the left kidney. There was no evidence of uroliths, and the right kidney and bladder appeared normal (Fig. 1). On color Doppler the lesion appeared intensely vascularized with turbulent flow and a characteristic confetti-like mosaic pattern (Fig. 2). Spectral analysis showed high-velocity arterial flow with a reduced systolic-diastolic difference (indicative of low resistance), and high, arterialized venous flow as well, typical of arteriovenous communication (Fig. 3).
Figure 1.

Renal US scan made with a 3.5 MHz probe. Longitudinal scan of the left kidney shows an anechoic area 4.6 cm in diameter in the renal sinus, which is suggestive of hydronephrosis.
Figure 2.

Color Doppler US of the kidney shows a confetti-like, blue-and-red flow pattern within the anechoic lesion.
Figure 3.
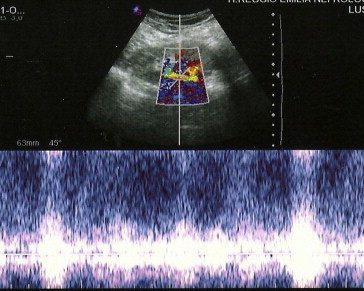
Pulse-wave Doppler US with spectral analysis. The spectral tracing shows turbulent flow with arterialization of the venous waveform.
To evaluate this hypothesis, the patient underwent selective angiography of the left kidney, which confirmed the presence of an AVF, which was fed by a small branch of the inferior polar artery and was associated with a pseudoaneurysm (Fig. 4). Closer investigation revealed that the patient had been hospitalized on a nephrology ward for a renal biopsy (RB) - over 10 years ago. She reported that during that hospitalization she had had a bladder catheter for about 2 weeks because the urine she was passing was “very red.” She was later discharged with a diagnosis of nephritis, and according to the patient, subsequent evaluations revealed no evidence of sequelae.
Figure 4.
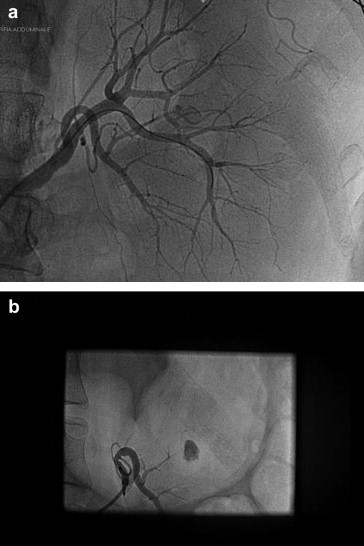
Selective renal arteriography. a. Angiogram confirmed the presence of an AVF in the middle of the left kidney b. A pseudoaneurysm was evident at the site of the malformation.
When seen by our staff, the patient was in good health with no clinically significant proteinuria or hematuria and renal function at the lower limits of normal. In light of these findings, she was advised to undergo periodic sonographic follow-up in our center. This report is being published with her full written consent.
Discussion
Arteriovenous fistulas are a potential complication of renal biopsy reported for the first time by Blake in the early 1960s and confirmed in more recent reports. They occur more frequently in the native kidneys of patients who are immunodepressed with systemic or immunologic disease and in transplanted kidneys, particularly in pediatric patients, because of the relatively superficial location of the biopsied organ. Renal AVFs may be associated with pseudoaneurysms, which are sometimes quite large [3].
The main clinical manifestation of AVF is gross hematuria with little or no anemia. This phase is preceded by microhematuria, which generally appears within the first 48 h after RB. Renal sonography performed within 24 h of the RB may already raise the suspicion of AVR. The lesion appears at the level of the lower pole of the left kidney (the site of choice for RB) and is typically anechoic. The dimensions vary depending on the extension of the AV communication produced by the biopsy.
The ultrasound appearance of the lesion sometimes resembles that of pelvic cysts or hydronephrosis [4]. In these cases, color Doppler studies can be used to confirm that the lesion is actually an AV malformation. The Doppler criteria for diagnosis of renal AVF were established for native kidneys [5], but they have been used above all for identifying these lesions in kidney transplant recipients.
In this case, too, Doppler ultrasonography reveals a typical mosaic pattern at the level of the anechoic lesion with high-velocity arteriovenous flow and spectral analysis findings typical of AVF.
The behavior over time of RB-related AVFs varies: in most cases, spontaneous closure occurs; in others, like the one reported here, the AVF remains patient for years. Color Doppler is not used routinely after RB, and for this reason some authors recommend that it be done immediately after the procedure and repeated 6 months later to reduce the risk of complications like vascular steal or arterial or venous stenosis [6]. In a non-negligible percentage of cases, the presence of persistent hematuria with anemia and/or fever requires selective embolization of the AVF and if this approach is not successful, the fistula will have to be surgical ligated.
In patients with obstructive uropathy (OU), US offers good diagnostic accuracy (total correct results: true positives + true negatives). In most series, sensitivity exceeds 90%. False negatives (patients with obstruction but no dilatation, according to Platt) are caused mainly by dehydration in patients who are elderly or diabetic or by complete obstruction (particularly by calculi), and they are rare (<5% of all cases in most series). In patients with uroliths, the persistence of complete obstruction sometimes reduces glomerular filtration pressure to zero, thereby preventing the formation of hydronephrosis.
In clinical practice, false positives (FP) (patients with dilation but no real obstruction) are more common. Since FPs represent the denominator in the formula used to calculate specificity, the latter parameter is somewhat lower (slightly over 80% in most series). The most frequent causes of FP include hyperhydration (psychogenic or related to other factors), disease of the renal calyx, and diabetes insipidus. Sometimes, even simple nephroptosis (which is most commonly seen in thin women and usually involves the right kidney) can mimic OU, especially if it is associated with substantial ureteral kinking.
It is important to consider renal AVF among the less common causes of FP. The differential diagnosis is actually fairly simple when the patient has recently undergone RB. If, however, the sonogram is obtained many years after the RB procedure-as it was in this case, and the operator is unaware that the patient has had an RB, color Doppler US, together with a complete patient history, is the only way to arrive at a correct diagnosis.
In conclusion, the case reported here shows that, when OU is suspected, renovascular malformations (AVF in particular) should always be considered as a possible cause of FP on the US examination. To facilitate diagnosis, we advise routine use of color Doppler US, especially in patients who have undergone RB.
Appendix. Supplementary material
Supplementary data related to this article can be found online at doi:10.1016/j.jus.2011.10.006.
Conflict of interest statement
The authors have no conflict of interest to declare.
AppendixSupplementary material
References
- 1.Blake S., Hefferman S., McCann P. Renal arteriovenous fistula after percutaneous renal biopsy. Br Med J. 1963 June;1(5343):1458–1460. doi: 10.1136/bmj.1.5343.1458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kopecna L., Mach V., Prochazka J. Arteriovenous fistula as a complication of renal biopsy. Bratisl Lek Listy. 2005;106(6–7):218–220. [PubMed] [Google Scholar]
- 3.Rivera M., Villacorta J., Jimenez-Alvaro S., Quereda C. Asymptomatic large extracapsular renal pseudoaneurysm following kidney transplant biopsy. Am J Kidney Dis. 2011;57(1):175–178. doi: 10.1053/j.ajkd.2010.07.020. [DOI] [PubMed] [Google Scholar]
- 4.Kember P.G., Peck R.J. Renal arteriovenous malformation mimicking hydronephrosis. J Clin Ultrasound. 1998;26:95–97. doi: 10.1002/(sici)1097-0096(199802)26:2<95::aid-jcu8>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 5.Li J.C., Cai S., Jiang Y.X., Dai Q., Zhang J.X., Wang Y.Q. Diagnostic criteria for locating acquired arteriovenous fistulas with color Doppler sonography. J Clin Ultrasound. 2002;30(6):336–342. doi: 10.1002/jcu.10084. [DOI] [PubMed] [Google Scholar]
- 6.Yang C.Y., Lai M.Y., Lu C.L., Tseng H.S., Chiou H.J., Yang W.C. Timing of Doppler examination for detection of arteriovenous fisulta after percutaneous renal biopsy. J Clin Ultrasound. 2008;36(6):377–380. doi: 10.1002/jcu.20459. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


