Abstract
Conflicts, snapping and instability of the tendons are common, and ultrasound (US) is the method of choice for evidencing these conditions thanks to the possibility to perform dynamic maneuvers during imaging studies. A conflict can occur between a tendon and a bone structure, other tendons, the retinacula or pulleys. Snapping can occur due to instability caused by rupture of the retinaculum, conflict between a thickened retinaculum and a bone prominence or due to an abnormal position of the tendon. Instability can occur due to insufficient ability of the retinaculum to keep the tendons in the bone groove or its failure to hold the tendons applied to the bone.
The technique for evidencing conflicts, snapping and instability of the tendons is very demanding because it requires a thorough knowledge of the US appearance and dynamic maneuvers. However, at the present time US examination completed with dynamic maneuvers is the investigation of choice for evidencing these disorders and providing the clinicians with the necessary information.
Keywords: Ultrasound, Tendons, Snapping, Conflicts, Instability
Sommario
Conflitti, scatti ed instabilità dei tendini sono frequenti e l’ecografia è, per la possibilità di eseguire manovre dinamiche, la metodica di elezione per obbiettivarli.
I conflitti dei tendini possono realizzarsi rispetto a strutture ossee, ad altri tendini, a retinacoli e pulegge.
Gli scatti possono avvenire per instabilità da rottura di un retinacolo, per conflitto con un retinacolo ispessito o con una protuberanza ossea, per uno spostamento anomalo rispetto a un altro tendine.
L’instabilità può realizzarsi per insufficienza di un retinacolo nel chiudere una doccia ossea, o per insufficienza, sempre di un retinacolo, a stabilizzare i tendini contro un osso.
La tecnica per l’evidenziazione di conflitti, scatti ed instabilità dei tendini è molto impegnativa, perché richiede la conoscenza della semiotica e manovre dinamiche, ma l’ecografia, completata con manovre dinamiche è, al momento attuale, l’indagine di scelta per la comprensione di queste patologie e per fornire informazioni ai clinici.
Introduction
Conflicts, snapping and instability of the tendons are frequent disorders which are better studied by ultrasound (US) than MRI thanks to the possibility to perform dynamic maneuvers during US examination. Particular dynamic maneuvers are required during the study of each specific disorder in order to evidence the abnormality [1,2]. The purpose of this paper is to describe the required dynamic maneuvers and the relative US appearance.
Tendinous conflicts
Conflicts with the bone structures
Dorsal carpal bones: conflict between the dorsal osteophytes of the carpometacarpal interline and the extensor tendons of the radius and fingers. They are evidenced by extension and flexion movements of the tendons and linked to carpometacarpal flexion.
Anterior conflict of the ankle: dorsal osteophytes and extensor tendons. Flexion and extension movements of the foot and toes [3].
Acromial vault and superior cuff (Figs. 1 and 2): oblique-sagittal scan of the coracoacromial ligament with medial rotation movements of the shoulder, coronal scan of the superior cuff [4] and movements of abduction and rotation involving a feeling of “sticking”. The examination includes searching for bursitis, tendinitis and tendon rupture, particularly of the superficial portion.
Figure 1.
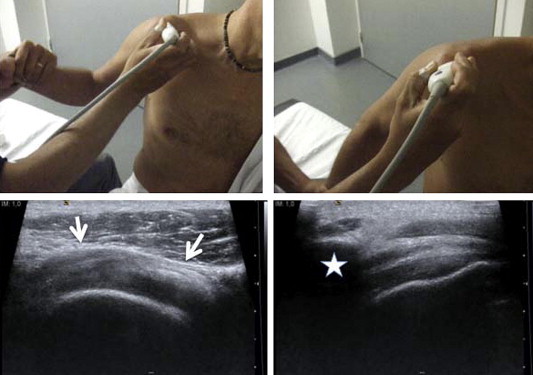
Searching for impingement syndrome. Oblique-sagittal scan on the coracoacromial ligament (white arrows) and rotational movements of the shoulder. Coronal scan of the supraspinatus at the acromion (asterisk) and abduction movements.
Figure 2.
Impingement syndrome, pathological aspects. Convex aspect of the coracoacromial ligament (white arrow). Thickening of the subacromial bursa.
Peroneal trochlea and peroneal tendons (Fig. 3). Peroneus longus tendinopathy. Greater tuberosity of the calcaneus and Achilles tendon (Haglund): dorsiflexion and plantar flexion, bursitis and anterior cleavage of the tendon. Iliotibial band syndrome between the lateral epicondyle and the distal iliotibial band [5]: axial scan at the lateral epicondyle, and flexion-extension of the knee, bursitis between the tendon and the lateral epicondyle.
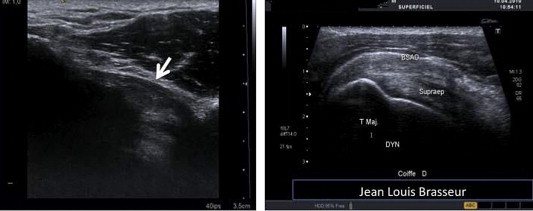
Figure 3.
Hypertrophy of the peroneal trochlea and conflict with the peroneus longus tendon. Coronal CT reconstruction and VCR, axial retromalleolar US image showing tendinopathy of the peroneus longus tendon (arrow) and axial submalleolar image showing hypertrophy of the trochlea (arrowheads).
Patellar tendon and the inferior surface of the trochlea.
Coracoid and anterior cuff: axial scan at the coracoid and medial rotation movements. Conflict between the acromion and the anterior surface of the subscapularis tendon. Posterior superior conflict according to Walch between the posterior edge of the glenoid and the deep surface of the superior cuff [6]: posterior axial scan of the infraspinatus starting from the position of medial abduction-rotation, the hand resting on the opposite shoulder and moving progressively in external abduction-rotation of the shoulder. Lesion of the deep surface of the superior cuff and bone abnormalities of the posterior surface of the glenoid.
Conflicts with other tendons: intersection
Intersection of the abductor pollicis longus and the extensor pollicis brevis tendons with the carpi radialis tendons (Fig. 4): tendinitis, bursitis and tenosynovitis; Doppler image shows hyperemia [7,8].
Figure 4.
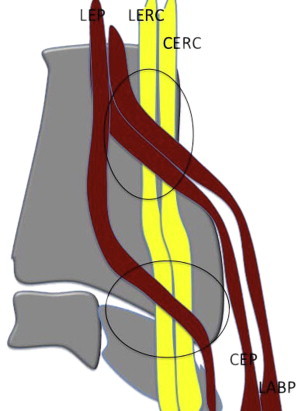
Diagram showing proximal intersection between the radial tendons (LERCH and CERC) and short extensor tendons (CEP) and abductor pollicis longus (LABP); intersection between the radial tendons and the extensor pollicis longus tendon(LEP).
Intersection of the extensor pollicis longus tendon and extensor carpi radialis longus (Fig. 4): tendinitis, bursitis and tenosynovitis.
Conflicts with retinaculum or a thickened pulley
De Quervain’s tendinopathy: the abductor pollicis longus and the extensor pollicis brevis (Fig. 5): thickening of the retinaculum of the first dorsal compartment, stenosing tenosynovitis [9]. Finger flexor tendons and A1 pulley (Fig. 6) [10,11]: thickening of the pulley (>1 mm) where Doppler image shows hyperemia with attachment of the superficial flexor to the pulley during flexion of the finger.
Figure 5.

De Quervain’s tendinitis. Coronal and axial US scans showing thickening of the retinaculum of the first osteofibrous tunnel due to stenosing tenosynovitis of the short extensor tendons (CE) and abductor pollicis longus (LA).
Figure 6.
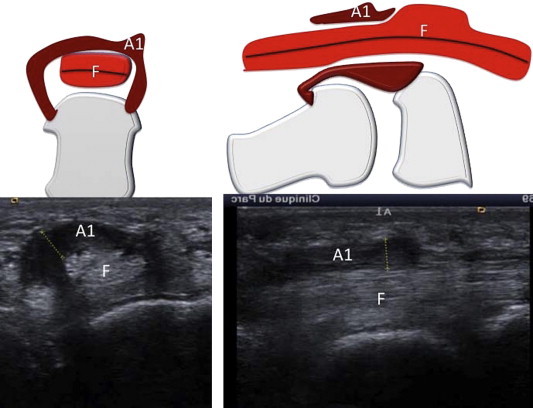
Finger with snapping due to thickening of the A1 pulley, which causes conflict with the superficial flexor during flexion.
Tendons of the ankle and retinaculum: post-traumatic thickening of the retinaculum and tenosynovitis with Doppler image showing hyperemia.
Tendon snapping
Due to instability caused by rupture of the retinaculum
Posterior tibial tendon [12]: evidenced by resisted inversion movements. Peroneal tendons [13]: resisted subversion. Extensor carpi ulnaris tendon (Fig. 7): supination and ulnar deviation. Tendon of the long head of the biceps muscle: lateral rotation of the shoulder.
Figure 7.
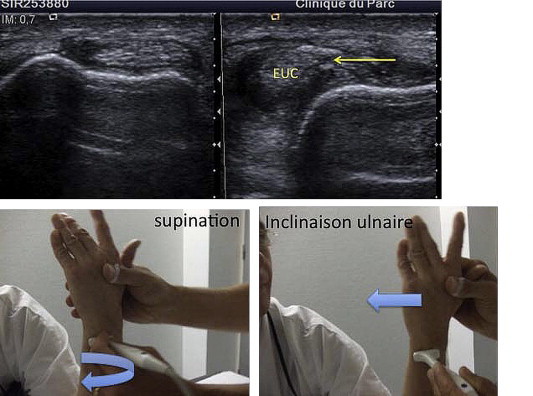
Instability of the extensor carpi ulnaris tendon due to rupture of the sheath. Two dynamic maneuvers are required: supination and ulnar deviation of the wrist.
Due to conflict with a thickened retinaculum [14]
Finger flexor and A1 pulley.
Conflict with a protruding bone
Flexor hallucis longus and protruding posterior process of the talus.
Abnormal displacement
Lateral snapping of the tensor fasciae latae of the hip [1] (Fig. 8); the tendon passes forward from the greater trochanter during hip flexion: axial scan of the greater trochanter with the patient in the lateral decubitus position performing a hip flexion maneuver, which reproduces the snapping. Lateral snapping of the hip with anterior fibers of the gluteus maximus: the same appearance as that of the tensor fasciae latae.
Figure 8.
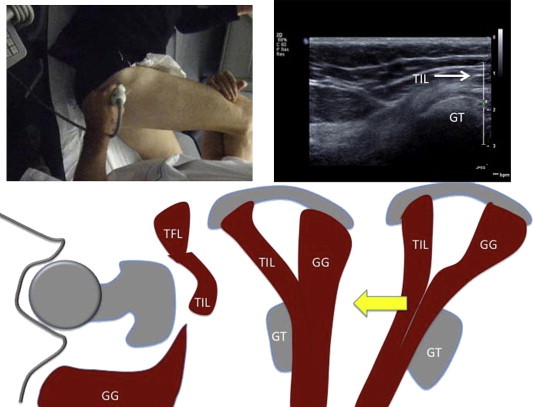
Lateral snapping of the hip due to the iliotibial band (TIL) passing forcefully forward from the greater trochanter (GT) during hip flexion.
Snapping of the distal biceps femoris tendon (Fig. 9) [15]: this condition occurs for numerous reasons. It can be due to snapping of the tendon on an epiphysis of the hypertrophic fibula, to snapping of a tendon caused by the union with the iliotibial band, to a too anterior insertion of the biceps on the fibula or to a bifid insertion of the tendon with an additional insertion on the head of the tibia in conflict with the lateral collateral ligament. These conditions can be identified during flexion-extension movements of the knee.
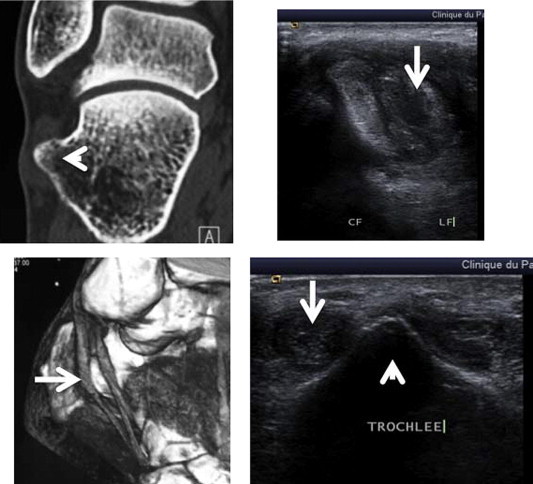
Figure 9.
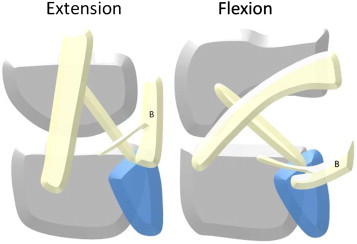
Snapping of the biceps femoris at the knee due to the presence of an accessory head arising from the tibia.
Snapping of the iliopsoas muscle (Fig. 10): during flexion, abduction and external rotation of the hip, the enveloped muscle is interposed between the tendon and the anterior cortical bone of the pelvis. While returning to extension, the tendon snaps against the bone before it finds its initial position.
Figure 10.
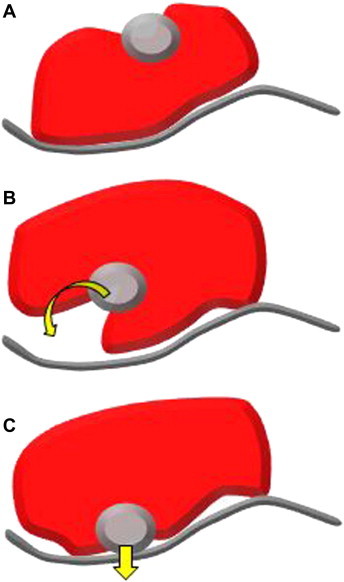
Snapping mechanism of the iliopsoas muscle with the muscle interposed between the tendon and the anterior cortex of the pelvis during flexion, abduction and external rotation of the hip (A). During return to extension, the tendon snaps against the bone while regaining its original position (B, C).
Snapping against another tendon
Sartorius and semimembranosus tendon reflex (Fig. 11) during flexion; the Sartorius tendon is behind the semimembranosus tendon reflex and runs posteriorly during extension. This movement can be sudden and cause snapping, particularly in the presence of semimembranosus tendinopathy.
Figure 11.
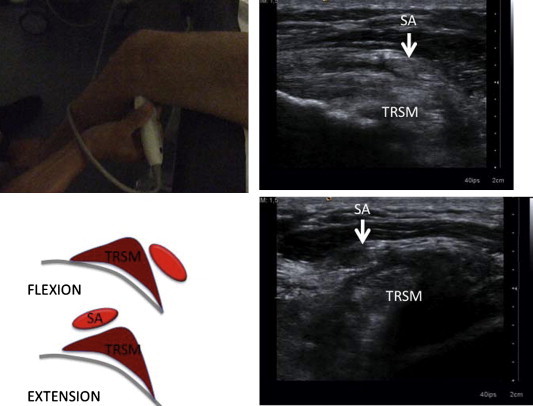
Snapping of the knee. During flexion, the sartorius (SA) is behind the semimembranosus tendon reflex (TRSM) passing anterior to it during extension. This movement may be sudden and cause snapping particularly in the presence of semimembranosus tendinopathy.
Instability
Due to failure of the retinaculum to keep the tendons in the bone groove
Extensor carpi ulnaris and the ulna: the instability must be sought in supination and ulnar deviation of the wrist. A comparative study should be performed to evidence congenital laxity, which frequently occurs. Long head of the humeral bicipital groove of the humerus: lateral rotation [1]. Long head of the biceps and humeral bicipital groove: lateral rotation [1]. Peroneal tendons and lateral retromalleolar groove due to insufficiency of the proximal retinaculum of the peroneal tendons: resisted eversion maneuver of the foot. Search for indirect signs: thickening of the retinaculum and bone avulsion.
Failure of a retinaculum to hold the tendons applied to the bone structure
Flexors of the fingers and pulley (Fig. 12) [10]: resisted flexion, the image shows pathological detachment from the bone. Extensors of the fingers and sagittal band: the extensors are laterally dislocated from the metacarpal heads during flexion [16]. Extensors of the feet and extensor retinaculum: pathological detachment between the extensors and the bone during resisted dorsiflexion.
Figure 12.
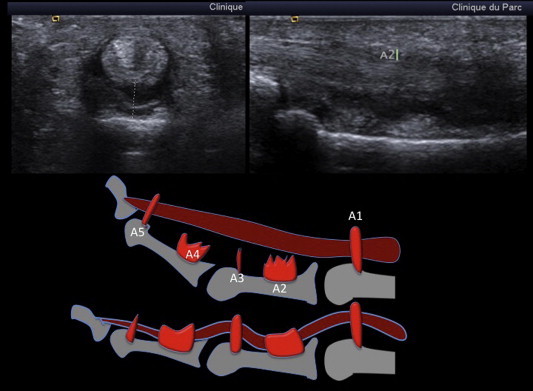
Rupture of the flexor pulleys, identified by resisted flexion, causing a pathological detachment of the phalanx flexor tendons from the bone.
Conclusions
The described disorders are common and US diagnosis is essential. The technique is very demanding because it requires knowledge of US appearance and the required dynamic maneuvers. Video recordings are crucial for understanding the disorders in order to provide the clinicians with correct clinical information.
Conflict of interest
The authors have no conflict of interest to declare.
Appendix. Supplementary data
The following are the supplementary data related to this article:
References
- 1.Bianchi S., Martinoli C. Springer–Verlag; 2007. Ultrasound of the musculoskeletal system. [Google Scholar]
- 2.Bordet B., Borne J., Fantino O., Pialat J.B. US of the ulnal collateral ligament (UCL) at the first metacarpophalangeal (MCP) joint: a new dynamic maneuver to detect stener lesions. J Radiol. 2009 Feb;90(2):217–220. doi: 10.1016/s0221-0363(09)72472-2. [DOI] [PubMed] [Google Scholar]
- 3.Hess G.W. Ankle impingement syndromes: a review of etiology and related implications. Foot Ankle Spec. 2011 Oct;4(5):290–297. doi: 10.1177/1938640011412944. [DOI] [PubMed] [Google Scholar]
- 4.Hughes P.C., Green R.A., Taylor N.F. Measurement of subacromial impingement of the rotator cuff. J Sci Med Sport. 2011 Aug 17 doi: 10.1016/j.jsams.2011.07.001. [DOI] [PubMed] [Google Scholar]
- 5.Fredericson M., Weir A. Practical management of iliotibial band friction syndrome in runners. Clin J Sport Med. 2006 May;16(3):261–268. doi: 10.1097/00042752-200605000-00013. [DOI] [PubMed] [Google Scholar]
- 6.Beaudreuil J., Nizard R., Thomas T., Peyre M., Liotard J.P., Boileau P. Contribution of clinical tests to the diagnosis of rotator cuff disease: a systematic literature review. Jt Bone Spine. 2009 Jan;76(1):15–19. doi: 10.1016/j.jbspin.2008.04.015. [DOI] [PubMed] [Google Scholar]
- 7.de Lima J.E., Kim H.J., Albertotti F., Resnick D. Intersection syndrome: MR imaging with anatomic comparison of the distal forearm. Skeletal Radiol. 2004;33(11):627–631. doi: 10.1007/s00256-004-0832-4. [DOI] [PubMed] [Google Scholar]
- 8.Parellada A.J., Gopez A.G., Morrison W.B., Sweet S., Leinberry C.F., Reiter S.B. Distal intersection tenosynovitis of the wrist: a lesser-known extensor tendinopathy with characteristic MR imaging features. Skeletal Radiol. 2007;36(3):203–208. doi: 10.1007/s00256-006-0238-6. [DOI] [PubMed] [Google Scholar]
- 9.Ilyas A.M., Ast M., Schaffer A.A., Thoder J. De quervain tenosynovitis of the wrist. J Am Acad Orthop Surg. 2007;15(12):757–764. doi: 10.5435/00124635-200712000-00009. [DOI] [PubMed] [Google Scholar]
- 10.Klauser A., Frauscher F., Bodner G., Halpern E.J., Schocke M.F., Springer P. Finger pulley injuries in extreme rock climbers: depiction with dynamic US. Radiology. 2002;222(3):755–761. doi: 10.1148/radiol.2223010752. [DOI] [PubMed] [Google Scholar]
- 11.Nakata W., Katou S., Fujita A., Nakata M., Lefor A.T., Sugimoto H. Biceps pulley: normal anatomy and associated lesions at MR arthrography. Radiographics. 2011 May-Jun;31(3):791–810. doi: 10.1148/rg.313105507. [DOI] [PubMed] [Google Scholar]
- 12.Jain N.B., Omar I., Kelikian A.S., van Holsbeeck L., Grant T.H. Prevalence of and factors associated with posterior tibial tendon pathology on sonographic assessment. PM R. 2011 Nov;3(11):998–1004. doi: 10.1016/j.pmrj.2011.05.025. [DOI] [PubMed] [Google Scholar]
- 13.Tourné Y., Saragaglia D., Benzakour D., Bezes H. Traumatic luxation of the peroneal tendons. Report of 36 cases. Int Orthop. 1995;19(4):197–203. doi: 10.1007/BF00185221. [DOI] [PubMed] [Google Scholar]
- 14.Makkouk A.H., Oetgen M.E., Swigart C.R., Dodds S.D. Trigger finger: etiology, evaluation, and treatment. Curr Rev Musculoskelet Med. 2008;1:92–96. doi: 10.1007/s12178-007-9012-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Date H., Hayakawa K., Nakagawa K., Yamada H. Snapping knee due to the biceps femoris tendon treated with repositioning of the anomalous tibial insertion. Knee Surg Sports Traumatol Arthrosc. 2011 Nov 23 doi: 10.1007/s00167-011-1778-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lopez-Ben R., Lee D.H., Nicolodi D.J. Boxer knuckle (injury of the extensor hood with extensor tendon subluxation): diagnosis with dynamic US-report of three cases. Radiology. 2003;228:642–646. doi: 10.1148/radiol.2283020833. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


