Abstract
We report the case of a 35 years old patient presenting with bilateral pain in the medial aspect of both knees. Ultrasound examination revealed hyperechoic appearance of the subcutaneous tissue and periarticular soft tissue bilateral. Color Doppler studies showed significant vascular signals at the surface of the tibial plateaux. US appearance, together with clinical findings, suggested a diagnosis of simultaneous bilateral fatigue fracture. An MRI confirmed the diagnosis and the patient’s symptoms resolved with rest. US may be a useful imaging tool in the diagnosis of stress fracture.
Keywords: Fatigue fracture, Sonography, Ultrasound, Stress fracture
Sommario
Presentiamo il caso di un paziente di 35 anni con dolore bilaterale nella parte mediale delle ginocchia. L’ecografia evidenziava ipoecogenicità del tessuto sottocutaneo e delle parti molli periarticolari bilateralmente. L’esame con color Doppler mostrava significativi segnali vascolari in corrispondenza del piatto tibiale. L’aspetto ecografico, associato ai segni clinici, suggeriva la diagnosi di simultanea frattura da fatica, bilaterale. La risonanza magnetica confermava la diagnosi e i sintomi del paziente regredivano con il riposo. L’ecografia può essere un’utile metodica nella diagnosi frattura da stress.
Introduction
Stress fractures (SF), bone failures secondary to submaximal chronic overloads, can be divided depending on their pathogenesis in fatigue (FF) and insufficiency fractures (IF). FF result from repeated abnormal stresses on a normal bone and are commonly seen in both amateur and high-level athletes. Their incidence is estimated as high as 61% in certain group of athletes [1–5]. IF are seen when normal stresses are applied to bones weakened by a variety of systemic disorders such as osteoporosis or rheumatoid arthritis.
Although they can affect the upper extremity, FF mostly involve the lower extremity with prevalence for the tibia, the neck of the femur, the metatarsal bones and the calcaneus [1,2,6,7]. Patients present with local pain typically accentuated by activity and diminished by rest. Physical examination can only show pain at palpation, when the fracture involves deep-seated bones, or also reveal local swelling and redness if a superficial bone is fractured. FF can be suspected clinically but an imaging technique is usually required to confirm the suspicion and assess the severity of the fracture. Imaging studies allow early detection of the fracture, instauration of an adequate treatment thus reducing morbidity.
Conventional radiographs are not enough sensitive since presence of cortical discontinuity or formation of a bone callus can take weeks to be evident [8–10]. The sensitivity of bone scan has been demonstrated in various studies but its specificity is low [4,9–11]. Computed tomography (CT) scan can show FF, but due to utilisation of radiation it is less favoured than the magnetic resonance imaging (MRI). MRI is the examination of choice in the early detection of SF but its use is limited by lack of access and associated cost [3]. In the past few years, various authors have reported ultrasound (US) as an inexpensive, non-invasive and ready modality with high sensitivity for the investigation of SF of the metatarsal [10,11]. Reports of SF affecting other bones then metatarsals diagnosed by US are rare [6]. Nevertheless US can be useful in diagnosing SF if the examination is accurately performed by an expenciered sonologist with a high degree of clinical suspicion. We report the case of a young patient with a bilateral simultaneous FF of the tibial plateau diagnosed by US and confirmed by MRI.
Case report
A 35-year-old Caucasian man (172 cm/90 kg, body mass index = 30,4) presented with pain in the medial aspect of both knees. The patient had a sedentary job and regularly engaged in swimming and hiking. History did not showed any systemic disorders/treatment or risk factors predisposing to osteoporosis. Three weeks earlier, he started a jogging program (one-half hour/day, seven days a week) in an attempt to loose weight. After 10 days he reported bilateral medial knee pain first noted during running and then persisting at rest. Clinical examination revealed localized bilateral pain and tenderness on the lower medial aspect of the knees, more evident at the insertion site of the hamstrings. The range of motion of both knees was normal (135° of flexion, 0°of extension) and there was no sign of joint or periarticular inflammation. There was a varus of 10° for both knees. Previous blood tests were referred as normal. Based on clinical findings an initial diagnosis of hamstring tendinopathy was made and a conservative treatment with non-steroidal anti-inflammatory drugs was prescribed and US was obtained to confirm the clinical diagnosis.
A musculoskeletal radiologist with 25 years of experience in US performed the examination using a commercially available equipment with a linear broadband transducer working at 5–12 MHz. Axial, longitudinal and oblique grey-scale and colour Doppler images were obtained on the medial aspect of both knees and proximal tibiae in the supine patient with the knees slightly flexed. A large amount of gel was deployed. US revealed the presence of bilateral thickening and hyperechogenicity of the subcutaneous tissue, paraarticular soft tissues adjacent to the bone cortex and periosteum (Fig. 1). The hyperechoic cortex of both tibias showed mild irregularity without sign of discontinuity. Colour Doppler showed significant vascular signals of the surface of the tibial plateaux. The pes anserinus region and the medial collateral ligament were normal on both sides. Examination of the knee joints was normal. US appearance, together with clinical findings, suggested a diagnosis of simultaneous bilateral FF of the proximal tibiae. An MRI was then obtained to confirm the US findings. MRI was obtained, a week after the US examination, on both knees using a 1,5 T equipment and an 8-channels knee dedicated coil. The examination protocol included coronal (FOV 16 cm, 18 slices thickness 3 mm TR 3000, TE 30) and axial (FOV 15 cm, 18 slices thickness 4 mm TR 2990, TE 15) proton density fat suppressed images, sagittal proton density images with (FOV 17 cm, 24 slices thickness 3.5 mm TR 2685, TE 15) and without (FOV 17 cm, 24 slices thickness 3.5 mm TR 5000, TE 30) fat saturation and sagittal proton density images (FOV 15 cm, 18 slices thickness 4 mm TR 2990, TE 15). On both proximal epiphysis of the tibia MRI showed an irregular hypo intense line roughly parallel to the joint surface. The lines were evident in all sequences and were surrounded by an area of bone marrow oedema appearing hyperintense in PD fat saturated sequences and slightly hypo intense in PD images (Fig. 2). The appearance was typical of an FF. The rest of the examination was normal.
Figure 1.
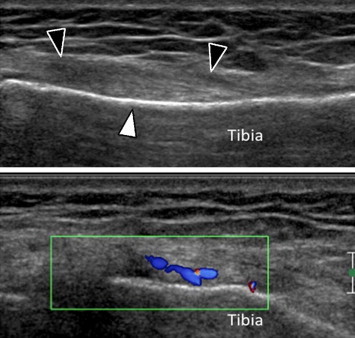
Coronal (top) and coronal colour Doppler (bottom) sonograms obtained over the medial aspect of the left knee. The grey-scale image shows thickening of the soft tissue located between the tibial cortex (white arrowhead) and the inferior part of the medial collateral ligament (black arrowheads). Colour Doppler shows flow signals due to local hypervascular changes.
Figure 2.
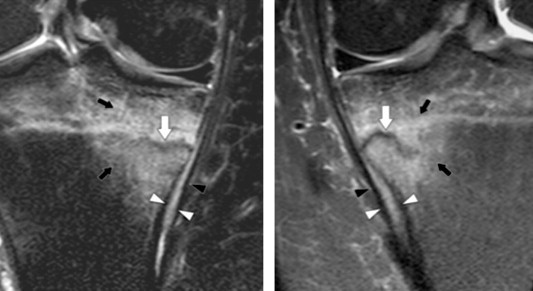
Coronal PD fat sat MRI images obtained on both knees. MRI depicts the stress fracture (white arrows) as a low intensity, serpiginous, line surrounded by an ill-defined hyperintense area related to marrow oedema (black arrows). Note also hyperintensity (withe arrowheads) of soft tissues located between the medial collateral ligaments (black arrowheads) and the bone cortex related to local inflammation.
The patient was treated by rest (crutches) and analgesic treatment upon pain. Physical examination obtained after 1 month showed complete relief of symptoms and signs. Bilateral A–P and lateral radiographs of the knees obtained at this time (Fig. 3) showed a sclerotic subchondral line located at the medial aspect of the proximal metaphysis of both tibiae. The appearance was typical of FF.
Figure 3.

A-P standard radiographs of both knee show two roughly symmetric sclerotic lines (arrows) parallel to the articular surface. This aspect is typical of stress fracture.
Informed consent was obtained from the patient for the publication of this case report.
Discussion
Sports injuries have significantly increased in frequency in the past few years, especially among individuals whose level of physical fitness is ill suited to the intensity or the very nature of the activity undertaken. Although data on the prevalence of sports injuries seem to be difficult to collect, it is estimated that approximately 6% of those who engage in sports require medical care for their injuries [13,14]. Sports injuries can be acute or derive from excessive (overuse injuries) or not well equilibrated (disuse injuries) activity such as excessive training in an unprepared organism. Overuse-disuse injures affect primarily tendons and muscles but depending on the activity and stress applied can also affect bone resulting in FF.
The main site for SF the sacrum (29.6%), the tibia (16,5%), the femur (9.9%), the metatarsus and the calcaneus [2,8]. In most patients, FF cannot be diagnosed only on the basis of clinical findings although a detailed history and careful clinical examination can orient to the diagnosis. Usually an increase in the intensity or duration of physical activity previous to the appearance of pain can be retraced. The main clinical finding is localized pain aggravated from activity and decreased by rest. An imaging modality is required to confirm the clinical suspicion and to start adequate treatment. Conventional radiographs are not sensitive in diagnosing SF since they are normal in the first weeks. The radiographic appearance of SF depends on the bone affected. In tubular bones, although cortical discontinuity is the hallmark of SF, the earliest diagnostic sign is a thin periosteal calcific reaction that can be easily missed if the diagnosis is not suspected. Later on, with bone remodelling, a bone callus becomes evident. In cancellous bones the first radiographic sign is a sclerotic band of the trabecular bone due to bone apposition from the endosteum.
A bone scan is a sensitive method for early diagnosis of a fatigue fracture. The radioactive tracer is incorporated into the cells responsible for bone remodelling within 24 h following the fracture. However, this technique is not sufficiently specific because bone turnover can be increased in a wide variety of others conditions including tumours, infections or inflammations [4,9,14].
At CT-Scan the bone repair reaction appears as bony sclerosis surrounding the line of fracture. In some studies, this technic is even more sensitive and specific than MRI [11,15].
Due to its mutiplanar capabilities and high tissue contrast, MRI is the imaging modality of choice for diagnosing an SF. MRI is sensitive and specific, revealing intramedullary oedema, the periosteal reaction and the fracture line.
Nevertheless it is expensive and still today barely accessible in some countries.
Recent technological advancements have increased the diagnostic possibilities of US in the assessment of musculoskeletal system thus widely increasing its utilisation. Wide accessibility, low cost, as well as absence of side effects, has increased the popularity of this technic. Although its chief application in musculoskeletal disorders is the assessment of soft tissues, US can help in detecting SF. Banal et al. reported 70% sensitivity for US compared to an MRI for the examination of fractures of the second metatarsal [12]. Several studies have described ultrasonographic findings of SF (11,14). Five US hallmarks have been described in SF: [1] cortical disruption which is a rare and late finding [2] posterior shadowing related to periosteal thickening. This sign can be seen only in small bone such as the metatarsals [3] thickening of the periosteum which appears as a hypoechoic band overlying the hyperechoic bone cortex [4] Increased periosteal colour Doppler flow related to local hyperaemia [5] hyperechogenicity of the surrounding soft tissue which indicates soft tissue oedema and inflammatory reaction. Doppler abnormalities and hyperechogenicity of the local soft tissue are most important for establishing an early diagnosis [6,12,15].
Most articles discussing the US appearance of SF have been focused on metatarsals [12,16]. Reports on SF affecting other bones are scanty [6].
The differential diagnosis of periarticular pain of the medial aspect of the knee in sports enthusiasts includes tendinopathy, bursitis and sprain of the medial collateral ligament. In pur case, these diagnosis were excluded by US that allowed demonstration of thickening, oedema and hypervascular changes in the periosteum and adjacent soft tissues associated with irregularities of the bone cortex. These findings were noted at the level of maximal tenderness. The US appearance in our patient was not specific but, considering the clinical findings and the normal appearance of the paraarticular tendons, was highly suspected of an FF. MRI was necessary to establish a definite diagnosis.
Our case shows the importance for the sonologist to perform a comprehensive US examination targeted to all structures from skin to the bone cortex and the necessity to correlate the US findings to clinical appearance. The US findings of local oedema, thickening and hyperaemia of the periosteum could be easily overlooked without considering the clinical appearance.
In case of suspicion of an FF, when evaluating the bone cortex, the sonologist must be careful in considering small cortical discontinuities as fractures since these can correspond to the entries of feeding arteries as it can be demonstrated by colour Doppler. At the proximal medial tibia, we’ve found this physiological discontinuity in 15 healthy subjects aged from 30 to 50 years 80% (unpublished data). Nevertheless the Doppler signal among these subjects was not as intense as in our patient, was closely localized at the discontinuity and and did not affect the periosteum and periarticular tissues.
In conclusion we present a case in which US showed bilateral thickening of the periosteum and periarticular tissues of the medial tibia associated with increased local vascularity at Color Doppler and ruled out the clinical suspicion of hamstrings tendinitis. The US appearance, togheter with the clinical setting, were high presumptive of a bilateral FF that was later confirmed by MRI. US when performed with an accurate technique of examination can strongly indicate a diagnosis of FF in the tibia. MRI is the preferred method of choice to confirm the diagnosis.
Conflict of interest statement
The authors have no conflict of interest to disclose.
Appendix. Supplementary material
References
- 1.Albisetti W., Erugina D., De Bartolomeo O., Tagliabue L., Camerucci E., Calori M.G. Stress fractures of the base of the metatarsal bones in young trainee ballet dancers. Int Orthop. 2010;34:51–55. doi: 10.1007/s00264-009-0784-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pohl M., Mullineaux D., Milner C., Hamill J., Davis I. Biochemical predictors of retrospective tibial stress fractures in runners. J Biomech. 2008;41:1160–1165. doi: 10.1016/j.jbiomech.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 3.Raasch W.G., Hergan D.J. Treatment of stress fractures: the fundamentals. Clin Sports Med. 2006;25:29–36. doi: 10.1016/j.csm.2005.08.013. [DOI] [PubMed] [Google Scholar]
- 4.Sofka C. Imaging of stress fractures. Clin Sports Med. 2006;25:53–62. doi: 10.1016/j.csm.2005.08.009. [DOI] [PubMed] [Google Scholar]
- 5.Warden S., Burr D., Brukner P. Stress fractures: pathophysiology, epidemiology and risk factors. Curr Osteoporos Rep. 2006;4(3):103–109. doi: 10.1007/s11914-996-0029-y. [DOI] [PubMed] [Google Scholar]
- 6.Arni D., Lambert V., Delmi M., Bianchi S. Insufficiency fracture of the calcaneum: sonographic findings. J Clin Ultrasound. 2009;37:424–427. doi: 10.1002/jcu.20577. [DOI] [PubMed] [Google Scholar]
- 7.Matheson G.O., Clement B., McKenzie D.C., Taunton J.E., Lloyd-Smith D.R., Macintyre J.G. Stress fractures in athletes. A study of 320 cases. Am J Sports Med. 1987;15:46–58. doi: 10.1177/036354658701500107. [DOI] [PubMed] [Google Scholar]
- 8.Krestan C., Hojreh A. Imaging of insufficiency fractures. Eur J Radiol. 2009;71:398–405. doi: 10.1016/j.ejrad.2008.04.059. [DOI] [PubMed] [Google Scholar]
- 9.Soubrier M., Dubost J.J., Boisgard S., Sauvezie B., Gaillard P., Michel J. Insufficiency fracture. A survey of 60 cases and review of the literature. Jt Bone Spine. 2003;70:209–218. doi: 10.1016/s1297-319x(03)00024-1. [DOI] [PubMed] [Google Scholar]
- 10.Patel D.S., Roth M., Kapil N. Stress fracture: diagnosis, treatment and prevention. Am Fam Physician. 2011;83(1):39–46. [PubMed] [Google Scholar]
- 11.Gaeta M., Minutoli F., Scribano E., Ascenti G., Vinci S., Bruschetta D. CT and MR imaging findings in athletes with early tibial stress injuries: comparison with bone scintigraphy findings and emphasis on cortical abnormalities. Radiology. 2005;235:553–561. doi: 10.1148/radiol.2352040406. [DOI] [PubMed] [Google Scholar]
- 12.Banal F., Grandjbakh F., Foltz V., Goldcher A. Sensitivity and specificity of ultrasonography in early diagnosis of metatarsal bone stress fractures: a pilot study of 37 patients. J Rheumatol. 2009;36:1715–1719. doi: 10.3899/jrheum.080657. [DOI] [PubMed] [Google Scholar]
- 13.Dreinhöfer K.E., Reichel H., Käfer W. Strategies for prevention and management of musculoskeletal conditions. Lower limb pain. Best Pract Res Clin Rheumatol. 2007;21:135–152. doi: 10.1016/j.berh.2006.10.007. [DOI] [PubMed] [Google Scholar]
- 14.Peris P. Stress fractures. Best Pract Res Clin Rheumatol. 2003;17(6):1043–1061. doi: 10.1016/j.berh.2003.09.006. [DOI] [PubMed] [Google Scholar]
- 15.Ganiyusufoglu A.K., Onat L., Karatoprak O., Enercan M. Hamzaoglu. Diagnostic accuracy of magnetic resonance imaging versus computed tomography in stress fractures of the lumbar spine. Clin Radiol. 2010;65:902–907. doi: 10.1016/j.crad.2010.06.011. [DOI] [PubMed] [Google Scholar]
- 16.Bodner G., Stöckl B., Fierlinger A., Schocke M., Bernathova M. Sonographic findings in stress fractures of the lower limb: preliminary findings. Eur Radiol. 2005;15:356–359. doi: 10.1007/s00330-004-2525-8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


