Abstract
The carpal tunnel is an osteofibrous canal situated in the volar wrist. The boundaries are the carpal bones and the flexor retinaculum. In addition to the medial nerve, the carpal tunnel contains nine tendons: the flexor pollicis longus, the four flexor digitorum superficialis and the four flexor digitorum profundus. Ultrasound (US) study of the carpal tunnel generally involves short-axis imaging of the tendons, and in the presence of disease, long-axis imaging and dynamic maneuvers are added. There are numerous reports of anatomical variants of the wrist involving vessels, nerves, tendons and muscles, and they can all be studied by US. Some are particularly relevant from a clinical point of view and will therefore be accurately described. The anatomy is complex, and the US operator should therefore be thoroughly familiar with the normal anatomy as well as the anatomical variants that may have a role in the pathogenesis of carpal tunnel syndrome or influence treatment.
Keywords: Carpal tunnel, Ultrasound, Flexor tendons, Median nerve
Sommario
Il tunnel carpale è un canale osteo-fibroso localizzato nella regione volare del polso, delimitato profondamente, medialmente e lateralmente dalle ossa del carpo e superficialmente dal retinacolo dei flessori.
Al suo interno decorrono nove tendini: il flessore lungo del pollice, i quattro flessori superficiali delle dita, i quattro flessori profondi delle dita ed un nervo, il mediano.
Lo studio ecografico del tunnel carpale avviene generalmente per asse corto rispetto ai tendini ed è completato, almeno in presenza di patologia, da scansioni per asse lungo e manovre dinamiche.
A livello del polso esistono poi numerose varianti anatomiche coinvolgenti vasi, nervi, tendini e muscoli, tutte ben valutabili ecograficamente. Alcune hanno una maggior rilevanza clinica e sono pertanto oggetto di una descrizione più accurata.
L’anatomia normale è complessa, ma la sua conoscenza è essenziale per lo studio della patologia, come è essenziale la conoscenza delle varianti anatomiche che possono avere un ruolo nella patogenesi della sindrome del tunnel carpale o condizionarne le terapie.
Introduction
The continuous technological evolution has provided the possibility to perform an increasingly accurate study of the anatomical structures of the musculoskeletal system. Nowadays, thanks to the high spatial resolution images provided by the various radiological methods, it is possible to investigate very small anatomical structures. This evolution has had an effect also on ultrasound (US) examinations, and lesions or structures of less than 1 mm in diameter can therefore easily be studied. This is a particular advantage in the study of anatomical regions whose small size previously precluded an accurate study.
On the basis of these considerations, it was decided to offer a revision of the US anatomy of the carpal tunnel. Some of the US images were compared with magnetic resonance (MR) images of the same lesions/areas.
Normal anatomy
The carpal tunnel is an osteofibrous canal located in the volar wrist. The boundaries are the carpal bones forming the floor, and the flexor retinaculum (or transverse carpal ligament) forming the roof (Fig. 1A). The retinaculum is about 3–4 cm wide and inserts into the scaphoid tuberosity and into the pisiform (proximal carpal tunnel) (Fig. 1) and subsequently into the trapezium and the hook of the hamate (distal carpal tunnel) (Fig. 2). On the radial side it divides into two layers, a superficial layer and a deep layer to accommodate the tendon of the flexor carpi radialis [1].
Fig. 1.
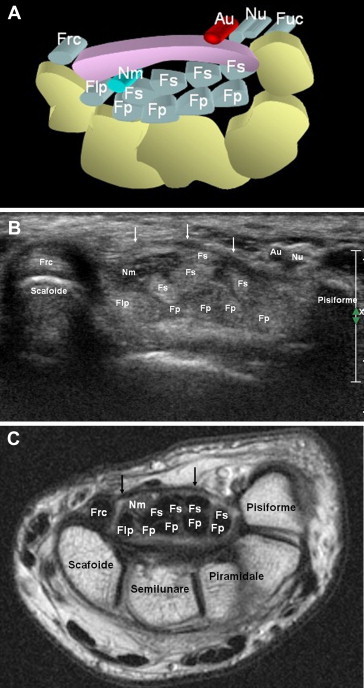
Proximal portion of the carpal tunnel. The carpal tunnel is an osteofibrous canal situated in the volar wrist. The boundaries are the carpal bones and the flexor retinaculum (A). The carpal tunnel contains nine tendons: the flexor pollicis longus, the four flexor digitorum superficialis and the four flexor digitorum profundus as well as the median nerve (B, C). The retinaculum (arrows) appears as a ribbon-like structure, hypoechoic (B) or hypointense (C), proximally it inserts to the tuberosity of the scaphoid and the pisiform.
Fig. 2.
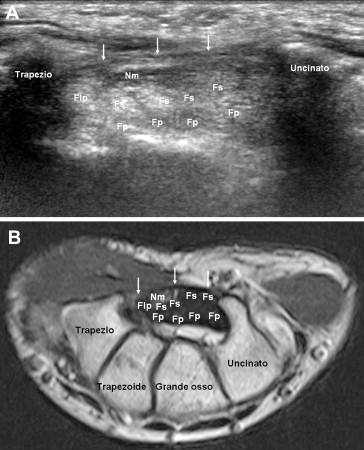
Distal carpal tunnel. Distally the retinaculum, which is about 3–4 cm wide, inserts to the trapezium and the hook of the hamate (arrows).
The carpal tunnel contains nine tendons and a nerve: the flexor pollicis longus, the four flexor digitorum superficialis, the four flexor digitorum profundus as well as the median nerve. The flexor pollicis longus has its own synovial sheath, whereas the flexor digitorum superficialis and profundus have a common synovial sheath.
The flexor carpi radialis tendon, the flexor carpi ulnaris tendon and the palmaris longus tendon travel outside the carpal tunnel, but in close contact with it. The flexor carpi radialis tendon inserts into the scaphoid and the base of the second metacarpal bone after passing through the canal formed by the splitting of the flexor retinaculum. The flexor carpi ulnaris tendon inserts into the pisiform, whereas the palmaris longus tendon continues with the palmar fascia or inserts into the flexor retinaculum.
US image of the carpal tunnel structures
Tendons consist mostly of type I collagen fibers which are oriented mainly parallel to the long axis. Under physiological conditions, the US image shows the tendons as fibrillar structures consisting of multiple parallel lines if obtained in long-axis direction and as multiple hyperechoic punctiform images, if obtained in short-axis direction. However, when the US beam is not parallel to the tendons these may appear hypoechoic; this is an artifact called anisotropy. In this case, there is an area of lower echogenicity that should not be misinterpreted as pathological. This phenomenon regularly occurs in the study of carpal tunnel syndrome, as it is linked to the curved course of the tendon bundles.
Nerves are composed of multiple axons gathered in bundles. They are surrounded by the perinerve, i.e. thin concentric layers of dense connective tissue. The bundles are further grouped and bound together by a matrix of connective tissue, the epinerve. US examination shows the peripheral nerves as multiple hypoechoic parallel lines (groups of bundles) surrounded by the hyperechoic perinerve and epinerve, [2] (Fig. 3). US image is defined as trabecular. US structure of the flexor retinaculum is similar to that of the tendons. The only part of the bones that can be assessed by US is the cortex which appears as a continuous hyperechoic line (Figs. 1 and 2).
Fig. 3.
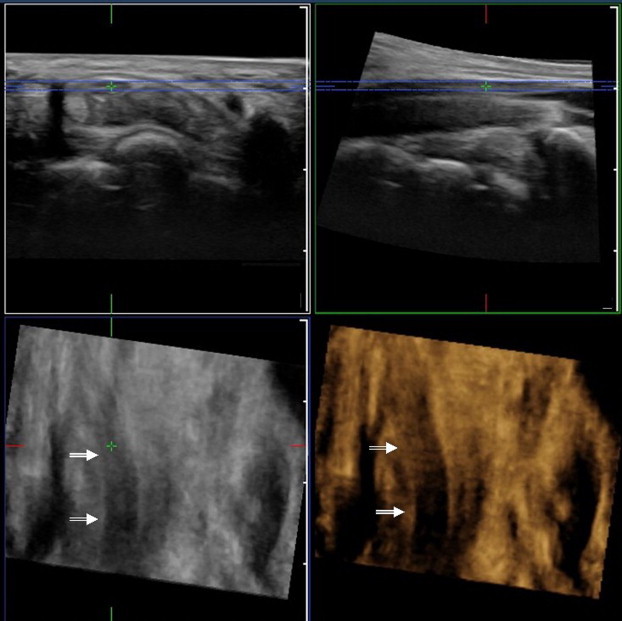
Coronal three-dimensional reconstruction of the median nerve. The median nerve is located at the carpal tunnel immediately below the flexor retinaculum, superficial to the flexor pollicis longus and the superficial flexor tendons to the index and middle fingers.
US study of the carpal tunnel
US images of the carpal tunnel are generally obtained in short-axis direction compared to the tendons. The median nerve is normally the first to be assessed. The examination usually begins in the forearm where the nerve is located between the flexor digitorum superficialis and flexor digitorum profundus muscles. When travelling towards the periphery, the median nerve becomes superficial, reaches the carpal tunnel and travels through it in a superficial position just below the flexor retinaculum (Figs. 1–3). Here it usually travels superficially to emerge between the tendons of the flexor pollicis longus and the flexor digitorum superficialis to the index and middle fingers. After assessment in the transverse plane, the nerve is evaluated along the longitudinal axis. Longitudinal images are very useful in case of focal compression of the nerve because they show the compressed portion of the nerve as well as the proximal and/or distal swollen portion.
In the palm, the median nerve supplies sensory branches to the palmar surface of the thumb, index, middle finger and the radial palmar surface of the ring finger; it also supplies a motor branch and innervation to the thenar eminence as well as the first and second lumbrical muscles [1].
At the wrist, a small branch leaves the median nerve on the radial side; this palmar cutaneous branch [3] travels towards the flexor carpi radialis to innervate the cutaneous and subcutaneous tissue situated on the side of the hand. Identification of this nerve and possible anatomical variants of its course is extremely important as it might otherwise be at risk of injury during surgery. Identification of nerves requires dynamic maneuvers like identification of the tendons.
The flexor pollicis longus tendon is the next to be evaluated. It is easily recognized, first of all because it is the most radial tendon in the carpal tunnel and because it is oval (Figs. 1 and 2). Recognition can be facilitated by a dynamic maneuver that involves bending of the thumb.
Recognition of the superficial and deep flexor tendons of the fingers is more complex (Figs. 1 and 2) and also in this case dynamic maneuvers may be helpful. The flexor digitorum profundus tendon of the fingers is inserted into the distal phalanx. By blocking the middle phalanx and moving the distal phalanx, the tendon, which moves in the carpal tunnel, is the flexor digitorum profundus tendon of the finger in question. The flexor digitorum superficialis tendon of the fingers is inserted into the middle phalanx. By blocking the thumb and the three other fingers and moving only the free finger, the tendon, which moves in the carpal tunnel, is the flexor digitorum superficialis of the finger in question. Evaluation of the carpal tunnel should not be limited to the proximal portion (Fig. 1B,C) as it should be extended distally to include the trapezium and the hook of the hamate (Fig. 2) where a fluid collection may be suggestive of synovitis of the flexor tendons. When this US technique has been established, it should be repeated in a standardized manner to ensure that all the structures of interest are evaluated at each examination.
Anatomic variants
The wrist presents numerous anatomical variants involving vascular structures, nerves, tendons and muscles. Some of these are clinically relevant and the US operator should therefore be familiar with them [3]. Persistent median artery is among these variants (Fig. 4). In an adult, the hand normally receives blood from the ulnar and radial arteries. However, some people (12%–23% of the population) have a third artery, the median artery, which in most cases regresses during the second month of intrauterine life.
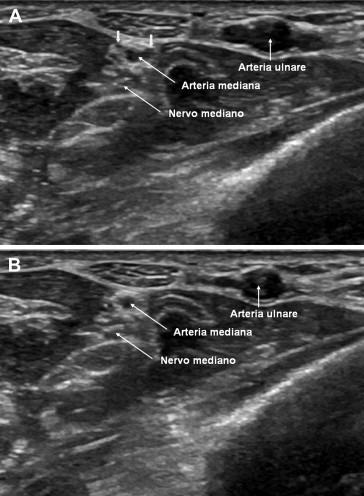
Fig. 4.
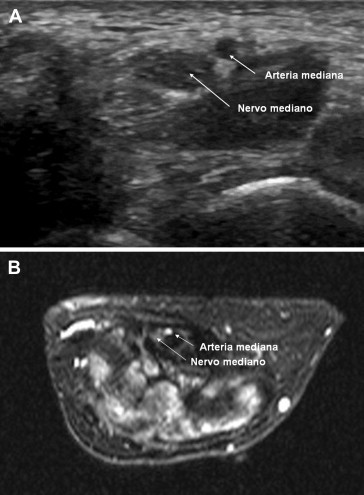
Persistent median artery. In adults, the hand receives blood from the ulnar and radial arteries. However, some people have a third artery, the median artery (A, B), which normally regresses during the second month of intrauterine life.
The median artery arises from the ulnar artery and travels towards the periphery along the ulnar side of the median nerve (Fig. 4). It is usually asymptomatic, but it may cause or be a contributing cause of carpal tunnel syndrome. It travels superficially and it might therefore be injured during surgery for carpal tunnel syndrome unless its existence and course are established. Persistent median artery is often associated with other anomalies of which the most frequent is bifid median nerve; in that case the median artery is often located between these two nerves (Fig. 5A). Detection of the median artery can be facilitated by color-Doppler examination (Fig. 5B). The presence of veins in the carpal tunnel is much rarer (Fig. 6). Bifid median nerve is the most common nerve variant (Fig. 7), often associated with persistent median artery (Fig. 5) or the presence of an anomalous muscle belly of the flexor digitorum superficialis.
Fig. 5.

Persistent median artery associated with bifid median nerve. The median artery (arrows) is situated between the two nerves (A); identification can be facilitated by color-Doppler examination (B).
Fig. 6.
Veins travelling in the carpal tunnel. In addition to the structures which are normally situated in the carpal tunnel, the image shows a median artery and two veins (arrows) (A). Differentiation between artery and vein is possible by using the transducer to compress the wrist; unlike the artery the vein will collapse (B). A reversed palmaris longus muscle is evident on the volar side compared to the vascular-nervous structures.
Fig. 7.

Bifid median nerve. Proximal bifurcation (A, B) is a quite common anatomic variant. US shows two nerves travelling adjacent to each other in the distal forearm (A).
The median nerve normally travels in the carpal tunnel as a single nerve, and it splits at the distal border of the transverse carpal ligament, where it gives rise to the branches which supply innervation to the fingers. Proximal bifurcation is a relatively common anatomic variant which has been found in 1%–3% of patients who undergo surgery for carpal tunnel syndrome. US examination shows two nerves travelling adjacent to each other in the forearm and inside the distal carpal tunnel (Fig. 7). The diameter of the two nerves may vary considerably, but generally they are approximately the same size; asymmetry, where one nerve is larger than the other, is uncommon. Early division in terminal branches (Fig. 8) is even less common. The US operator should always report the presence of bifid median nerve, as one of the nerves might otherwise be damaged during arthroscopic carpal tunnel decompression.
Fig. 8.
Median nerve divided into three branches. Proximal trifurcation is an extremely rare anatomical variant. US image shows three nerves travelling in the carpal tunnel just below the flexor retinaculum (arrows).
The median nerve has a motor branch which supplies innervation to the first and second lumbricals, to the opposition of the thumb, to the abductor pollicis brevis and to the lateral surface of the flexor pollicis brevis. However, this motor branch presents anatomic variants of which the most common affects 46%–90% of the population. The motor branch arises from the median nerve distal to the transverse carpal ligament on the radial side; this variant is so frequent that it is considered as normal anatomy. In the second variant, the origin is below the ligament; this variant may occur in approximately 33% of subjects and in this case the motor branch arises inside the carpal tunnel. The third variant is of transligamentous origin and it affects about 25% of subjects; in this case the motor branch penetrates and passes through the carpal ligament travelling towards the muscles of the thenar eminence.
The fourth anatomical variant is rare. In this case the motor branch arises on the ulnar side and crosses the median nerve when travelling to the muscles of the thenar eminence. In yet another variant, the motor branch may present a superficial course compared to the transverse carpal ligament.
Two variants affecting the palmar cutaneous branch have been described in the literature. In one variant, the nerve arises on the radial side of the median nerve [3]; in the second variant, the palmar cutaneous branch arises on the ulnar side of the median nerve and crosses it, takes a transligamentous course and penetrates the transverse carpal ligament. Detection of these variants is important, because damage to this nerve during surgery can lead to the development of a neuroma [4].
At the wrist, the ulnar nerve normally travels through the tunnel known as Guyon’s canal, an osteofibrous canal situated along the anteromedial portion of the carpal tunnel extending about 4 cm from the pisiform to the hook of the hamate [5]. The ulnar nerve supplies sensory and motor branches to the hand, and very rarely it travels inside the carpal tunnel. There may be an anomalous connection between the median and ulnar nerve in the forearm (Martin-Gruber anastomosis) resulting in various innervation patterns of the intrinsic hand muscles. This condition is generally caused by fibers from the median nerve travelling to reach the ulnar nerve, and it affects 6%–31% of the population. The Marinacci communication, also known as a reverse Martin-Gruber anastomosis, is a rare condition in which the communicating nerve fibers run from the ulnar nerve to the median nerve [6].
The flexor pollicis longus is usually independent of the flexor digitorum superficialis and flexor digitorum profundus tendons. However the flexor pollicis longus, flexor digitorum superficialis and flexor digitorum profundus arise from the same mesodermal tissue and there may be a tendinous connection between them. This tendinous connection between the flexor pollicis longus tendon and the flexor digitorum profundus tendon to the index finger is known as the Limburg-Comstock syndrome, and it occurs quite frequently. Patients with this anomaly cannot flex the thumb without bending also the distal phalanx of the index finger [3,7]. This anomalous connection is rarely symptomatic, but it may sometimes mimic carpal tunnel syndrome due to tenosynovitis.
The palmaris longus muscle is the muscle of the human body which has the greatest number of possible variants. Two variants are particularly important and must be identified before surgery. In one variant, the palmaris longus tendon travels inside the carpal tunnel. The second variant is the known as reversed palmaris longus. Normally, the muscle belly in the palm is in proximal position and the tendon in distal position. However, in some people this is reversed and the tendon is in proximal position and the muscle belly in distal position (Fig. 9). In reversed palmaris longus, the muscle may travel inside the carpal tunnel. In this case the muscle causes friction and the patient may develop carpal tunnel syndrome.
Fig. 9.
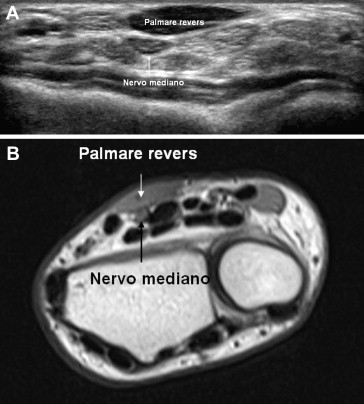
Reversed palmaris longus. Normally, the muscle belly in the palm is in proximal position and the tendon in distal position, but in some people this position is reversed and the tendon is in proximal position and the muscle belly in distal position. In this variant, the muscle often enters into conflict with the carpal tunnel structures and may cause carpal tunnel syndrome.
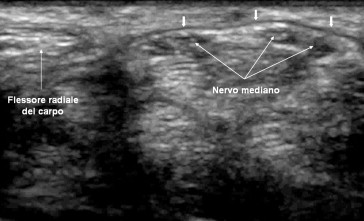
Other anomalies may affect the flexor digitorum superficialis, e.g. the muscle belly may extend into the carpal tunnel (Fig. 10). At the wrist there may be some accessory muscles, such as an accessory flexor digitorum superficialis to the index finger, and the palmar surface may present an accessory flexor digitorum superficialis indicis muscle [8].
Fig. 10.
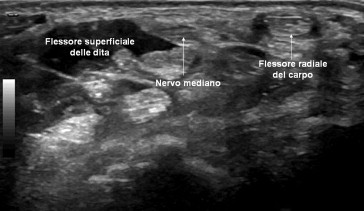
Flexor digitorum superficialis with the muscle belly in the carpal tunnel. Normally only the flexor digitorum tendons travel in the carpal tunnel whereas the muscle belly stops before reaching it; this variant can cause carpal tunnel syndrome.
The flexor digitorum superficialis is usually of humeral, ulnar and radial origin. It travels in the forearm and is split into a more superficial bundle and a deeper bundle, passes through the carpal tunnel and gives origin to four tendons to the index, middle, ring and little fingers. The tendons to the index and little fingers arise from the deep fibers.
The accessory flexor tendon to the index finger arises from the flexor digitorum close to the carpal tunnel. Some anatomical variants are known, such as the accessory to the index finger where the muscle belly is situated entirely in the palm of the hand. Another variant is the accessory digastric muscle to the index finger where the muscle belly is situated partly in the forearm and partly in the palm; a third variant is characterized by a muscle belly that extends into the carpal tunnel without passing through it.
A rare accessory muscle is the so-called flexor carpi radialis brevis vel profundus. It arises from the palmar surface of the distal radius, crosses the pronator quadratus, passes under the flexor retinaculum and inserts into the base of the third or fourth metacarpal bones. This condition has been described mainly in anatomical preparations, but it may cause symptoms of carpal tunnel syndrome [8]. Cases have furthermore been reported in which the second lumbrical muscle arose inside the carpal tunnel from the flexor digitorum superficialis [3]. Also this condition may cause carpal tunnel syndrome.
Conclusions
The US equipment available today provides an accurate assessment of the palmar surface of the wrist and the carpal tunnel. US examination is not particularly complicated from a technical point of view, but it is essential that the US operator is thoroughly familiar with the local anatomy and is able to recognize possible anatomical variants. This is important as some of these variants occur quite frequently and the presence of one or more anatomical variants may sometimes play a role in the pathogenesis of carpal tunnel syndrome and/or have an influence on the therapy.
Conflict of interest statement
The authors have no conflict of interest.
Appendix.
The following are the Supplementary data related to this article:
References
- 1.Martinoli C., Bianchi S., Gandolfo N., Valle M., Simonetti S., Derchi L.E. US of nerve entrapments in osteofibrous tunnels of the upper and lower limbs. RadioGraphics. 2000;20:S199–S217. doi: 10.1148/radiographics.20.suppl_1.g00oc08s199. [DOI] [PubMed] [Google Scholar]
- 2.Lee J.C., Healy J.C. Normal sonographic anatomy of the wrist and hand. RadioGraphics. 2005;25:1577–1590. doi: 10.1148/rg.256055028. [DOI] [PubMed] [Google Scholar]
- 3.Mitchell R., Chesney A., Seal S., Mc. Knight L., Thoma A. Anatomical variations of the carpal tunnel structures. Can J Plast Surg. 2009;17:3–7. [PMC free article] [PubMed] [Google Scholar]
- 4.Adani R., Leo G., Tarallo L., Marcoccio I., Fregni U. Il trattamento dei neurinomi dolorosi del ramo sensitivo del nervo radiale. Riv Chir Mano. 2005;42(3):127–134. [Google Scholar]
- 5.Vezeridis P.S., Yoshioka H., Han R., Blazar P. Ulnar-sided wrist pain. Part I: anatomy and physical examination. Skeletal Radiol. 2010;39:733–745. doi: 10.1007/s00256-009-0775-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gutmann L. Median-ulnar nerve communications and carpal tunnel syndrome. J Neurol Neurosurg Psychiatr. 1977;40:982–986. doi: 10.1136/jnnp.40.10.982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Watson A.H. What can studying musicians tell us about motor control of the hand? J Anat. 2006;208:527–542. doi: 10.1111/j.1469-7580.2006.00545.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sookur P.A., Naraghi A.M., Bleakney R.R., Jalan R., Chan O., White L.M. Accessory muscles: anatomy, symptoms and radiologic evaluation. RadioGraphics. 2008;28:481–499. doi: 10.1148/rg.282075064. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


