Abstract
Tenosynovitis refers to an inflammatory condition involving the synovial sheath of a tendon. Stenosing tenosynovitis is a peculiar entity caused by multiple factors, including local anatomy, mechanical factors, and hormonal factors. The main forms include de Quervain tendinopathy; trigger finger (stenosing tenosynovitis involving the flexor digitorum tendons); stenosing tenosynovitis of the extensor carpi ulnaris, extensor carpi radialis, or extensor comunis tendons; stenosing tenosynovitis of the flexor hallucis tendon; and stenosing tenosynovitis of the peroneal tendons. The cardinal finding on ultrasonography is the presence of a thickened retinaculum or pulley that constricts the osseofibrous tunnel through which the tendon runs.
Keywords: Tenosynovitis, Stenosing tenosynovitis, Ultrasonography
Sommario
Le tenosinoviti sono infiammazioni delle guaine sinoviali dei tendini. Le tenosinoviti stenosanti sono delle entità particolari, condizionate da molteplici fattori. Si tratta di patologie favorite dall’anatomia locale, da fattori meccanici ed ormonali. Le principali tenosinoviti stenosanti sono: la tendinopatia di de Quervain, la tenosinovite stenosante dei tendini flessori delle dita o dito a scatto, la tenosinovite stenosante del tendine estensore ulnare del carpo, dei tendini estensori radiali del carpo e degli estensori comuni, la tenosinovite stenosante del tendine flessore dell’alluce, la tenosinovite stenosante dei tendini peronei. La loro diagnosi si basa sull’ecografia, che mostra un segno cardine: l’ispessimento del retinacolo o della puleggia rispetto al tendine ed il suo carattere stenosante.
Basic features of stenosing tenosynovitis
Tenosynovitis is characterized by inflammation involving the synovial sheath of a tendon. It can have various causes, including inflammatory processes associated with rheumatic disease, infectious processes, primary tumors of the synovial sheath, hormonal and mechanical factors.
Stenosing forms of tenosynovitis are peculiar entities influenced by various factors—anatomical, mechanical, and in some cases hormonal. Their diagnosis is based on typical sonographic findings of hypertrophy of a retinaculum or pulley, which constricts the osseofibrous tunnel through which the tendon runs and reduces movement of the tendon during dynamic maneuvers.
A disorder favored by local anatomic factors
Stenosing tenosynovitis typically affects tendons that run through osseofibrous tunnels, each enclosed in its own synovial sheath. The tunnel itself lies over cortical bone and is covered by a structure referred to (depending on the location) as a pulley or retinaculum (Fig. 1).
Figure 1.
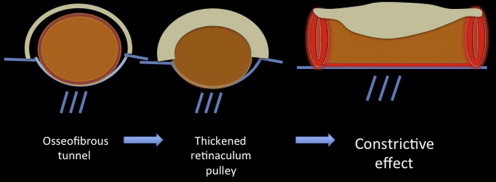
Schematic of osseofibrous tunnels. Thickening of the retinaculum or the pulley exerts a constrictive effect on the tendon.
The pulleys of the flexor digitorum tendons and the retinacula of the wrist and ankle are histologically identical. They consist of three layers [1] with distinct structural and functional features (Fig. 2):
-
-
the superficial layer contains a loose network of connective tissue and blood vessels. It is a thin layer that is in contact with the perimuscular and subcutaneous fasciae. Its "nutritional" role is related to the vascular elements it contains.
-
-
the intermediate layer is thicker. It contains fibroblasts, dense collagen fibers that lie perpendicular to the underlying tendons and bundles of variably oriented fibers, which give it a woven appearance. It provides mechanical strength and also contains hormone receptors.
-
-
the inner layer consists of one or two layers of flattened fibroblasts and cells that secrete hyaluronic acid. This is the gliding layer. It may contain isolated foci of chondroid metaplasia.
Figure 2.
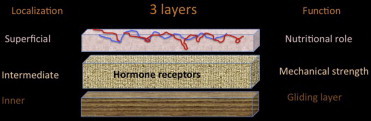
Schematic of the 3 histological layers of the pulleys and the retinacula.
A disorder promoted by mechanical and hormonal factors
Although the pathophysiology of stenosing tenosynovitis is still not clear, constriction resulting from pulley or retinacular deficits is the mechanical factor responsible for the intrinsic damage to the tendon and its sheath (Fig. 1). In their study of trigger finger, Sampson et al. [2] demonstrated the presence of fibrocartilaginous thickening of the A1 pulley. The anatomy of these structures on ultrasound and magnetic resonance imaging has been described by Hauger et al. [3].
Hypertrophy of the pulley (Fig. 3) was documented sonographically by Guerini et al. [4]. The thickness was significantly increased, on the average by 1.8 mm (range 1.1–2.9), compared with that of controls, whose pulleys measured 0.5 mm (mean; range 0.4–0.6). Alteration of the tendon, such as intratendinous nodules (Fig. 4) or tenosynovitis, was observed in only 48–55% of all cases. Chung et al. [5] measured tendon calibers and pulley thicknesses and found significant hypertrophy only in the A1 pulley. In our study of 22 patients with suspected de Quervain tenosynovitis, the severity and frequency of retinacular thickening was similar to that of peritendinous fluid; thickening of the sheath were found in 41%, thickening of the abductor longus tendon in 86% and of the extensor brevis tendon in 68% of the patients, respectively [6].
Figure 3.
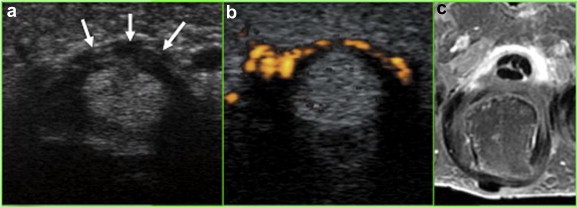
Trigger finger: Axial ultrasound image reveals hypertrophy of the A1 pulley (arrows) (a), hypervascularization on Doppler imaging (b), contrast uptake by the A1 pulley after injection of gadolinium during MR imaging (c).
Figure 4.
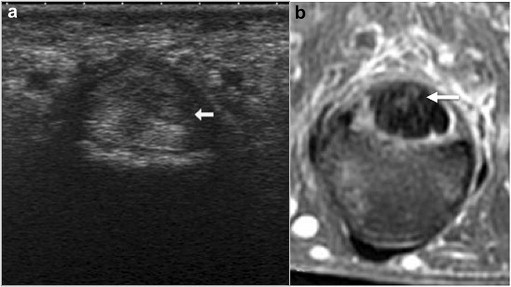
Tendinosis associated with trigger finger. The presence of an intratendinous nodules is manifested by a hypoechoic image on sonography (a) and hyperintensity on MRI (b).
Overuse, repetitive movements, sports-related and professional activities have all been implicated as mechanical causes of pulley and retinacular thickening.
The incidence of de Quervain tenosynovitis is 2.8 cases per 1000 in women and 0.6 cases per 1000 in men. It is more common after the age of 40. Activities that involve repetitive movements of the thumb (flexion, extension, and rotation), ulnar deviation of the carpal, and the use of scissors are all recognized as risk factors. Professional activities can be a cause among nurses [7] and endoscopists [8]. Overuse of the thumbs in females who send text messages from their cell phones has been reported [9], and sports-related activities can also be considered risk factors (e.g., among volleyball players) [10].
Estrogen stimulation and also estrogen deficits have also been considered as possible risk factors, and this hypothesis seems to be confirmed by histological findings of hormone receptors within the intermediate layer of the pulleys and retinacula. Aromatase inhibitors (AIs) and tamoxifen are recommended for adjunct treatment of receptor-positive breast cancers in postmenopausal women, and their principal side effects are the aggravation of musculoskeletal symptoms and reduction of bone mineral density. These painful symptoms can be so severe as to require discontinuation of treatment. In the ATAC (Arimidex, Tamoxifen, Alone or in Combination) study [11], which compared anastrozol and tamoxifen as adjunct therapies for breast cancer, "musculoskeletal symptoms" were reported at the 5-year follow-up visit by 35.6% of the patients on anastrozol and 29.4% of those in the tamoxifen group (p < 0.0001). In almost 60% of these cases there was involvement of the hands and wrists. A recent graduate thesis in medicine examined clinical and sonographic findings on the hands and wrists of 26 patients treated with AIs [12]. In 93% of the cases there were periarticular changes, which consisted of de Quervain tenosynovitis in 50%, trigger finger in 19%, and tenosynovitis of the flexor, extensor, or radial extensor tendons in 33%.
de Quervain tenosynovitis also occurs during the postpartum period as a separate entity known as "baby wrist". It is difficult to distinguish the roles played in this pathology by mechanical stress involved in caring for the baby and hormonal factors related to the pregnancy. In these cases the age at onset is clearly lower (mean 33 years), and the involvement is often bilateral [13].
Diabetes should also be considered in the workup of patients with multiple trigger fingers. The prevalence of trigger finger among diabetics ranges from 10% to 20%, which is much higher than that observed in the general population (1.7–2.6%) [14,15], and Kameyama et al. [16] found a higher frequency of multiple trigger finger in diabetic patients with limited finger mobility.
The main types of stenosing tenosynovitis
de Quervain tendinopathy
In the original 1895 report on the tenosynovitis that bears his name, Fritz de Quervain described the natural history of the disease, its symptoms, and treatment. He also immediately drew parallels between trigger finger and the constrictive tenosynovitis involving the first compartment [17], and sonographic findings support the existence of common elements in these two disorders.
de Quervain tenosynovitis (DQTS) is a mechanical disorder related to hypertrophy of the retinaculum that covers the first dorsal compartment of the wrist. There are several predisposing factors including the presence of a septum that divides the first compartment into two subcompartments [18]. We have demonstrated that this septum can be visualized sonographically as a thin hypo- or hyperechoic (depending on the anisotropy) wall that inserts on a small bone crest and divides the radial tunnel into two compartments, based on correlation with an anatomic specimen (Fig. 5) [19] and surgical findings [20].
Figure 5.
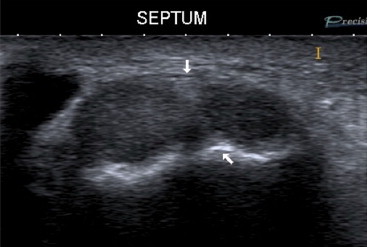
Sonographic visualization of the septum (thin partition stretched between the two arrows) of the first dorsal compartment of the wrist. The septum is inserted on a crest of cortical bone (lower arrow).
In a sonographic study published in 2010 [21], retinacular thicknesses measured in 33 patients with DQTS were significantly greater than those found in 24 controls : 2.01 mm (±0.53 mm) vs. 0.43 (±0.11 mm), respectively (p < 0.0001). Septal thickening may be total and involve both tendons (72.7% of cases) or it may involve only the extensor pollicis brevis or short extensor of the thumb (27.3% of cases). This allows us to distinguish two different clinical forms of de Quervain disease:
-
-
type I or stenosing tenosynovitis of the two tendons with no evidence of a septum (Fig. 6);
-
-
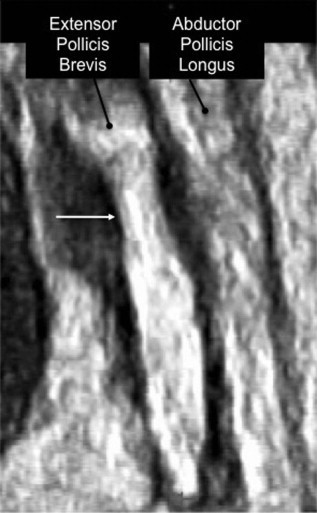
type II or isolated stenosing tenosynovitis of the extensor pollicis brevis (Fig. 7).
Figure 6.
de Quervain tenosynovitis, type I: Global thickening of the retinaculum around the two tendons (abductor longus and extensor brevis), which cannot be distinguished from one another inside the first dorsal compartment of the wrist.
Figure 7.
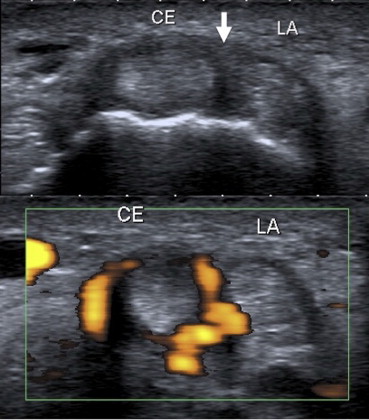
de Quervain tenosynovitis, type II, involving only the extensor brevis pollicis (CE). Note the absence of retinacular thickening near the abductor pollicis longus (LA) and the presence of a thickened septum between the two tendons (arrow).
Distinguishing these two forms is essential for proper treatment. Cortisone-derivative infiltration of the tendon sheath is associated with a failure rate of 15–20% [22,23]. This outcome may be related to the presence of a septum, which supports our view that infiltrations should be performed under sonographic guidance [21] (immediately or after 1-2 failed attempts) with clinical landmarks around the retinaculum.
The constrictive nature of the retinaculum can be appreciated on static ultrasound images (Fig. 8), and dynamic studies performed with 3D transducers allow one to reconstruct multiple consecutive sections (Fig. 9). They also demonstrate that the constriction is present in all spatial planes, the coronal plane in particular (Fig. 10). During and after infiltration, the retinacular hypertrophy diminishes, and the constriction gradually resolves (Fig. 11).
Figure 8.
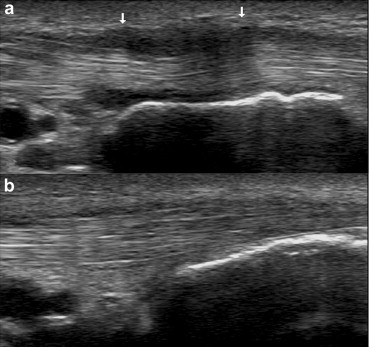
de Quervain tenosynovitis, type II. Sagittal sonographic image of the subcompartments of the extensor pollicis brevis (EPB) (a) and abductor pollicis longus (b) Note constrictive effect of the thickened retinaculum (arrow) on the EPB.
Figure 9.
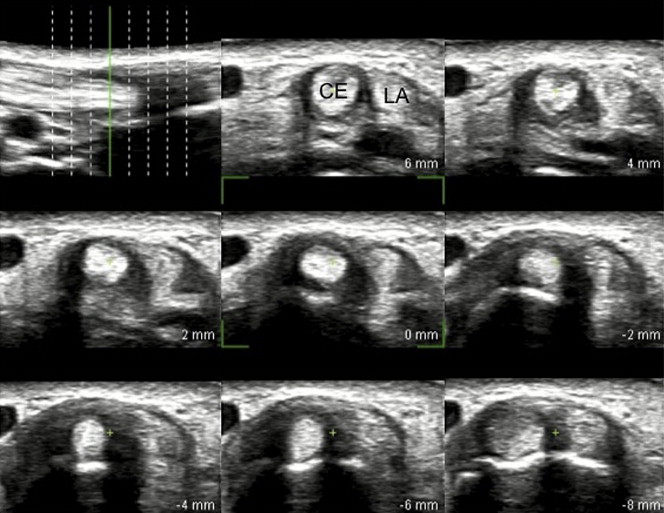
Three-dimensional sonographic appearance of de Quervain tenosynovitis, type II. The 3D acquisition allows axial reconstruction of multiple sections.
Figure 10.
Three-dimensional sonographic appearance of de Quervain tenosynovitis, type II, allows reconstruction in the coronal plane. Note constrictive effects of the retinaculum (arrow) on the extensor pollicis brevis tendon, whereas the abductor pollicis longus tendon has a normal appearance with parallel margins.
Figure 11.

Follow-up of de Quervain tenosynovitis after steroid infiltration. Retinacular thickening and tendon constriction were improved 3 months after treatment.
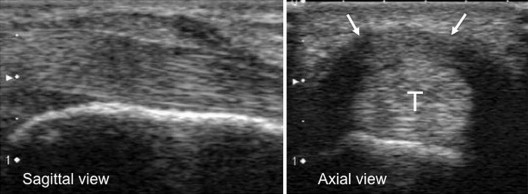
Stenosing tenosynovitis of the flexor digitorum tendons: trigger finger
The sonographic signs of stenosing tenosynovitis of the digits has also been well described. Hypoechoic thickening of pulley A1 next to the metacarpophalangeal joint is a constant finding (Fig. 12), which may be associated with hypervasculiarization on Doppler imaging (91% of all cases), peritendinous effusion (55%), tendinosis (48%), or tendinosis with effusion (39%) [4]. The thumb and ring finger are generally the digits most frequently affected [24].
Figure 12.

Sonographic image (sagittal plane) of the metacarpophalangeal joint of a finger shows hypoechoic thickening of pulley A1 (arrows).
Several studies have confirmed interest in the use of ultrasound guidance during local infiltration therapy [25–27]. When ultrasound guidance is used, the drugs are successfully injected into the tendon sheath in 70% of all cases as opposed to only 15% when the injection is performed blind. There are no reports of intratendinous injections under sonographic guidance, but this complication occurs with 30% of blind injections [25]. A simple technique recommended by Bodor [26] guarantees a high rate (90%) of positive results, with persistent resolution of symptoms 1 year after a single injection. The success rate for blind injections is only 57%.
Stenosing tenosynovitis of the extensor carpi ulnaris, extensor carpi radialis, and extensor digitorum comunis tendons
Several groups have reported cases classified as « stenosing tenosynovitis » of the extensor carpi ulnaris tendon (Fig. 13) [28–31]. One study describes five patients operated on for stenosis caused by the dorsal retinaculum next to the extensor comunis tendons, and we have observed a case of tendinopathy caused by retinacular hypertrophy next to the extensor carpi radialis tendons (Fig. 14). The stenosing nature of the tenosynovitis is always documented by the sonographic image, which reveals hypertrophy of the retinaculum that closes the sixth compartment of the wrist, the compartment of the extensor radialis tendons, or that of the extensor comunis tendons.
Figure 13.

Sonographic appearance of stenosing tenosynovitis of the extensor carpi ulnaris tendon.
Figure 14.
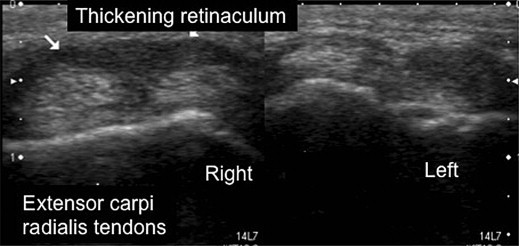
Stenosing tenosynovitis of the extensor carpi radialis tendon. Comparative (right vs. left) axial images demonstrate retinacular thickening (arrow).
Stenosing tenosynovitis of the flexor hallucis tendon
Movement of the flexor hallucis longus tendon can be restricted at the level of the posterior ankle and at its passage between the two sesamoids. This type of tenosynovitis (Fig. 15) is not always stenosing; it has been described in athletes [32], especially runners [33]. Posterior impingement by the talus has been documented in ballet dancers [34,35]. Some groups have described conflict at the level of the sesamoids on the plantar aspect of the great toe [36,37]. In 5 out of 9 cases, there is a history of trauma [37]. The signs may resolve when lidocaine is injected into the tendon sheath, but in most cases surgical release is necessary.
Figure 15.

Tenosynovitis of the flexor hallucis longus tendon. a) Retrocalcaneal osseofibrous tunnel, b) peritendinous effusion fluid and tendinopathy, c) thickening of the synovial sheath.
Stenosing tenosynovitis of the peroneal tendons
The short and long peroneal tendons are held in place behind the lateral malleolus by a proximal retinaculum and the long tendon by a distal retinaculum at the level of the peroneal tuberosity. This retinaculum inserts on the cortical surface of the calcaneus and the apex of the peroneal tubercle. This keeps the tendons in contact with the bone structure and creates an osseofibrous tunnel. The peroneus longus and brevis tendons run posterior and anterior to the tuberosity, respectively. Stenosing tenosynovitis (Fig. 16) can develop when the thickness of this retinaculum increases, especially in the presence of a large peroneal tubercle or a peroneal bone or when the patient has undergone surgical ligament repair [38–42].
Figure 16.
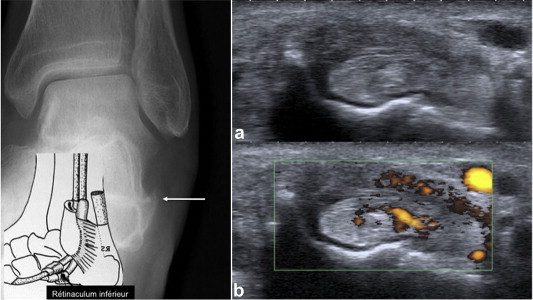
Stenosing tenosynovitis of the peroneal tendons. The stenotic segment is located next to the fibular tubercle (arrow) and the lower peroneal retinaculum. Note retinacular thickening (a) and hypervascularization (b) on sonography.
Conflict of interests
The authors have no conflicts of interest to declare.
Appendix. Supplementary data
References
- 1.Klein D.M., Katzman B.M., Mesa J.A., Lipton J.F., Caligiuri D.A. Histology of the extensor retinaculum of the wrist and the ankle. J Hand Surg [Am] 1999 Jul;24(4):799–802. doi: 10.1053/jhsu.1999.0799. [DOI] [PubMed] [Google Scholar]
- 2.Sampson S.P., Badalamente M.A., Hurst L.C., Seidman J. Pathobiology of the human A1 pulley in trigger finger. J Hand Surg. 1991 Jul;16(4):714–721. doi: 10.1016/0363-5023(91)90200-u. [DOI] [PubMed] [Google Scholar]
- 3.Hauger O., Chung C.B., Lektrakul N., Botte M.J., Trudell D., Boutin R.D. Pulley system in the fingers: normal anatomy and simulated lesions in cadavers at MR imaging, CT, and US with and without contrast material distention of the tendon sheath. Radiology. 2000 Oct;217(1):201–212. doi: 10.1148/radiology.217.1.r00oc40201. [DOI] [PubMed] [Google Scholar]
- 4.Guerini H., Pessis E., Theumann N., Le Quintrec J.S., Campagna R., Chevrot A. Sonographic appearance of trigger fingers. J Ultrasound Med. 2008 Oct;27(10):1407–1413. doi: 10.7863/jum.2008.27.10.1407. [DOI] [PubMed] [Google Scholar]
- 5.Chung H.W. RSNA; Chicago: 2003. Ultrasonography of the trigger fingers on the emphasis of the findings of annular pulley. p. 397. [Google Scholar]
- 6.Vuillemin-Bodaghi V., Morvan G., Mathieu P., Wybier M., Busson J. Détection échographique du septum du premier compartiment dorsal du poignet dans la ténosynovite de de Quervain (abstract) J Radiol. 2005;86(10):1292. [Google Scholar]
- 7.Leite P.C., Barbosa Merighi M.A., Silva A. The experience of a woman working in nursing suffering from De Quervain’s disease. Rev Lat Am Enfermagem. 2007 Mar-Apr;15(2):253–258. doi: 10.1590/s0104-11692007000200010. [DOI] [PubMed] [Google Scholar]
- 8.Shergill A.K., Asundi K.R., Barr A., Shah J.N., Ryan J.C., McQuaid K.R. Pinch force and forearm-muscle load during routine colonoscopy: a pilot study. Gastrointest Endoscopy. 2009 Jan;69(1):142–146. doi: 10.1016/j.gie.2008.09.030. [DOI] [PubMed] [Google Scholar]
- 9.Ashurst J.V., Turco D.A., Lieb B.E. Tenosynovitis caused by texting: an emerging disease. J Am Osteopath Assoc. 2010 May;110(5):294–296. [PubMed] [Google Scholar]
- 10.Rossi C., Cellocco P., Margaritondo E., Bizzarri F., Costanzo G. De Quervain disease in volleyball players. Am J Sports Med. 2005 Mar;33(3):424–427. doi: 10.1177/0363546504268134. [DOI] [PubMed] [Google Scholar]
- 11.Howell A., Cuzick J., Baum M., Buzdar A., Dowsett M., Forbes J.F. Results of the ATAC (Arimidex, Tamoxifen, Alone or in Combination) trial after completion of 5 years’ adjuvant treatment for breast cancer. Lancet. 2005 Jan 1–7;365(9453):60–62. doi: 10.1016/S0140-6736(04)17666-6. [DOI] [PubMed] [Google Scholar]
- 12.Belkhir R. Univeristé Paris V René Descartes; Paris: 2010. Atteinte des mains de patientes traitées par inhibiteurs de l’aromatase: données cliniques et échographiques. [Google Scholar]
- 13.Skoff H.D. "Postpartum/newborn" de Quervain’s tenosynovitis of the wrist. Am J Orthop (Belle Mead NJ) 2001 May;30(5):428–430. [PubMed] [Google Scholar]
- 14.Cagliero E., Apruzzese W., Perlmutter G.S., Nathan D.M. Musculoskeletal disorders of the hand and shoulder in patients with diabetes mellitus. Am J Med. 2002 Apr 15;112(6):487–490. doi: 10.1016/s0002-9343(02)01045-8. [DOI] [PubMed] [Google Scholar]
- 15.Chammas M., Bousquet P., Renard E., Poirier J.L., Jaffiol C., Allieu Y. Dupuytren’s disease, carpal tunnel syndrome, trigger finger, and diabetes mellitus. J Hand Surg Am. 1995 Jan;20(1):109–114. doi: 10.1016/S0363-5023(05)80068-1. [DOI] [PubMed] [Google Scholar]
- 16.Kameyama M., Meguro S., Funae O., Atsumi Y., Ikegami H. The presence of limited joint mobility is significantly associated with multiple digit involvement by stenosing flexor tenosynovitis in diabetics. J Rheumatol. 2009 Aug;36(8):1686–1690. doi: 10.3899/jrheum.081024. Epub 2009 Jun 16. [DOI] [PubMed] [Google Scholar]
- 17.de Quervain F. On a form of chronic tendovaginitis by Dr. Fritz de Quervain in la Chaux-de-Fonds. 1895. Am J Orthop. 1997 Sep;26(9):641–644. [PubMed] [Google Scholar]
- 18.Gousheh J., Yavari M., Arasteh E. Division of the first dorsal compartment of the hand into two separated canals: rule or exception? Arch Iran Med. 2009 Jan;12(1):52–54. [PubMed] [Google Scholar]
- 19.Rousset P., Vuillemin-Bodaghi V., Laredo J.D., Parlier-Cuau C. Anatomic variations in the first extensor compartment of the wrist: accuracy of US. Radiology. 2010 Nov;257(2):427–433. doi: 10.1148/radiol.10092265. [DOI] [PubMed] [Google Scholar]
- 20.Kwon B.C., Choi S.J., Koh S.H., Shin D.J., Baek G.H. Sonographic identification of the intracompartmental septum in de Quervain’s disease. Clin Orthop Relat Res. 2010 Aug;468(8):2129–2134. doi: 10.1007/s11999-009-1199-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Volpe A., Pavoni M., Marchetta A., Caramaschi P., Biasi D., Zorzi C. Ultrasound differentiation of two types of de Quervain’s disease: the role of retinaculum. Ann Rheum Dis. 2010 May;69(5):938–939. doi: 10.1136/ard.2009.123026. [DOI] [PubMed] [Google Scholar]
- 22.Richie C.A., 3rd, Briner W.W., Jr. Corticosteroid injection for treatment of de Quervain’s tenosynovitis: a pooled quantitative literature evaluation. J Am Board Fam Pract. 2003 Mar-Apr;16(2):102–106. doi: 10.3122/jabfm.16.2.102. [DOI] [PubMed] [Google Scholar]
- 23.Ilyas A.M., Ast M., Schaffer A.A., Thoder J. De quervain tenosynovitis of the wrist. J Am Acad Orthop Surg. 2007 Dec;15(12):757–764. doi: 10.5435/00124635-200712000-00009. [DOI] [PubMed] [Google Scholar]
- 24.Kim H.R., Lee S.H. Ultrasonographic assessment of clinically diagnosed trigger fingers. Rheumatology international. Rheumatol Int. 2010 Sep;30(11):1455–1458. doi: 10.1007/s00296-009-1165-3. Epub 2009 Oct 23. [DOI] [PubMed] [Google Scholar]
- 25.Lee D.H., Han S.B., Park J.W., Lee S.H., Kim K.W., Jeong W.K. Sonographically guided tendon sheath injections are more accurate than blind injections: implications for trigger finger treatment. J Ultrasound Med. 2011 Feb;30(2):197–203. doi: 10.7863/jum.2011.30.2.197. [DOI] [PubMed] [Google Scholar]
- 26.Bodor M., Flossman T. Ultrasound-guided first annular pulley injection for trigger finger. J Ultrasound Med. 2009 Jun;28(6):737–743. doi: 10.7863/jum.2009.28.6.737. [DOI] [PubMed] [Google Scholar]
- 27.Godey S.K., Bhatti W.A., Watson J.S., Bayat A. A technique for accurate and safe injection of steroid in trigger digits using ultrasound guidance. Acta Orthop Belg. 2006 Oct;72(5):633–634. [PubMed] [Google Scholar]
- 28.Crimmins C.A., Jones N.F. Stenosing tenosynovitis of the extensor carpi ulnaris. Ann Plast Surg. 1995 Jul;35(1):105–107. doi: 10.1097/00000637-199507000-00020. [DOI] [PubMed] [Google Scholar]
- 29.Nachinolcar U.G., Khanolkar K.B. Stenosing tenovaginitis of extensor carpi ulnaris: brief report. J Bone Jt Surg Br. 1988 Nov;70(5):842. doi: 10.1302/0301-620X.70B5.3192595. [DOI] [PubMed] [Google Scholar]
- 30.Hajj A.A., Wood M.B. Stenosing tenosynovitis of the extensor carpi ulnaris. J Hand Surg Am. 1986 Jul;11(4):519–520. doi: 10.1016/s0363-5023(86)80188-5. [DOI] [PubMed] [Google Scholar]
- 31.Steffens K., Koob E. Diagnosis and therapy of tendovaginitis of the extensor carpi ulnaris (stenosis of the 6th extensor compartment) Z Orthop Ihre Grenzgeb. 1994 Sep-Oct;132(5):437–440. doi: 10.1055/s-2008-1039850. German. [DOI] [PubMed] [Google Scholar]
- 32.Michelson J., Dunn L. Tenosynovitis of the flexor hallucis longus: a clinical study of the spectrum of presentation and treatment. Foot Ankle Int. 2005 Apr;26(4):291–303. doi: 10.1177/107110070502600405. [DOI] [PubMed] [Google Scholar]
- 33.Theodore G.H., Kolettis G.J., Micheli L.J. Tenosynovitis of the flexor hallucis longus in a long-distance runner. Med Sci Sports Exerc. 1996 Mar;28(3):277–279. doi: 10.1097/00005768-199603000-00001. [DOI] [PubMed] [Google Scholar]
- 34.Lamata Iturria M., Lison Torres A., Bento Gerard J., Guillen Montijano F. Bilateral stenosing tenosynovitis of the long flexors of the great toe in a dancer. Apropos of a bilateral case. Rev Chir Orthop Reparatrice Appar Mot. 1988;74(2):190–192. French. [PubMed] [Google Scholar]
- 35.Kolettis G.J., Micheli L.J., Klein J.D. Release of the flexor hallucis longus tendon in ballet dancers. J Bone Jt Surg Am. 1996 Sep;78(9):1386–1390. doi: 10.2106/00004623-199609000-00014. [DOI] [PubMed] [Google Scholar]
- 36.Sanhudo J.A. Stenosing tenosynovitis of the flexor hallucis longus tendon at the sesamoid area. Foot Ankle Int. 2002 Sep;23(9):801–803. doi: 10.1177/107110070202300905. [DOI] [PubMed] [Google Scholar]
- 37.Gould N. Stenosing tenosynovitis of the flexor hallucis longus tendon at the great toe. Foot Ankle. 1981 Jul;2(1):46–48. doi: 10.1177/107110078100200108. [DOI] [PubMed] [Google Scholar]
- 38.Wang X.T., Rosenberg Z.S., Mechlin M.B., Schweitzer M.E. Normal variants and diseases of the peroneal tendons and superior peroneal retinaculum: MR imaging features. Radiographics. 2005 May-Jun;25(3):587–602. doi: 10.1148/rg.253045123. [DOI] [PubMed] [Google Scholar]
- 39.Bianchi S., Delmi M., Molini L. Ultrasound of peroneal tendons. Semin Musculoskelet Radiol. 2010 Sep;14(3):292–306. doi: 10.1055/s-0030-1254519. Epub 2010 Jun 10. Review. [DOI] [PubMed] [Google Scholar]
- 40.Saupe N., Mengiardi B., Pfirrmann C.W., Vienne P., Seifert B., Zanetti M. Anatomic variants associated with peroneal tendon disorders: MR imaging findings in volunteers with asymptomatic ankles. Radiology. 2007 Feb;242(2):509–517. doi: 10.1148/radiol.2422051993. [DOI] [PubMed] [Google Scholar]
- 41.Bruce W.D., Christofersen M.R., Phillips D.L. Stenosing tenosynovitis and impingement of the peroneal tendons associated with hypertrophy of the peroneal tubercle. Foot Ankle Int. 1999 Jul;20(7):464–467. doi: 10.1177/107110079902000713. [DOI] [PubMed] [Google Scholar]
- 42.Boya H., Pinar H. Stenosing tenosynovitis of the peroneus brevis tendon associated with hypertrophy of the peroneal tubercle. J Foot Ankle Surg. 2010 Mar-Apr;49(2):188–190. doi: 10.1053/j.jfas.2009.02.013. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


