Abstract
The biceps brachii muscle, which inserts proximally onto the scapula and distally onto the forearm, has several tendons with numerous anatomic peculiarities, which render their sonographic examination highly variable. Proximally, the tendon of the short head of the biceps inserts onto the coracoid process and that of the long head on the superior aspect of the glenoid. The distal biceps tendon is bifurcated, and it generally inserts on the radial tuberosity, around which it rolls during pronation/supination. There is a third distal structure, the Lacertus fibrosus, an aponeurosis that branches off from the medial aspect of the tendon, crossing the median artery and median nerve, and inserting on the superficial aponeurosis of the flexor muscles. The sonographic examination of these tendons focuses on nine separate zones of interest: the glenoid insertion of the long head, its extension to the upper pole of the humeral head, the rotator interval, the reflection to the upper bicipital groove, the bicipital groove, the upper myotendinous junction, the lower myotendinous junction, the distal tendon(s), and the inferior enthesis. Because of their morphological and topographical characteristics, the biceps tendons are subject to a variety of lesions, some of which are frequently misdiagnosed on the basis of clinical findings. Ultrasound plays an important role in detecting and characterizing these lesions. Proper examination of the biceps (the distal portion in particular) is a difficult task that cannot be improvised.
Keywords: Ultrasonography, Biceps, Biceps Tendon
Sommario
Inserito prossimalmente sulla scapola e distalmente sull’avambraccio, il muscolo bicipite brachiale possiede numerosi tendini, che presentano diverse particolarità anatomiche, rendendo il loro studio ecografico molto “vario”.
Prossimalmente, il tendine del capo corto del bicipite si inserisce sulla coracoide; il tendine del capo lungo sul versante superiore della glena. Nella parte distale il tendine del bicipite è bifido e si inserisce, abitualmente, sul tubercolo del radio, attorno a cui si arrotola durante la manovra di prono-supinazione. Oltre a questo tendine bifido, esiste, distalmente, una terza struttura, il “lacertus fibrosus”, aponeurosi che si stacca dal versante mediale del tendine, incrocia l’arteria e il nervo mediano, per inserirsi sull’aponeurosi superficiale dei muscoli flessori.
Lo studio ecografico di questi tendini può quindi essere diviso in 9 zone di interesse: inserzione del capo lungo sulla glena, passaggio al polo superiore della testa, intervallo dei rotatori, riflessione alla parte alta del solco bicipitale, solco bicipitale, giunzione mio-tendinea superiore, giunzione mio-tendinea inferiore, tendine(i) distale, entesi inferiore.
Considerando gli aspetti morfologici e topografici i tendini del bicipite possono essere all’origine di lesioni molto diverse fra loro, alcune delle quali frequentemente misconosciute all’esame clinico.
Il ruolo dell’ecografia nel rilevamento e nella caratterizzazione di tali lesioni risulta quindi molto importante. Occorre tuttavia non sottovalutare il fatto che lo studio del bicipite, principalmente della sua parte distale, è molto difficile e non può essere improvvisato.
Introduction
The biceps brachii muscle inserts proximally onto the scapula and distally onto the forearm. It has several tendons with numerous anatomic peculiarities, which render their sonographic examination highly variable.
Proximally, the tendon of the short head of the biceps follows a rectilinear course and inserts onto the coracoid process; to the best of our knowledge, no lesions have ever been described at this level.
The tendon of the long head of the biceps originates on the superior rim of the glenoid, extends horizontally to the upper pole of the humeral head, and continues on within the rotator interval. Before its entry into the bicipital (or intertubercular) groove, the tendon presents an angulation, which is the result of rotation of the upper extremity that occurred during the course of evolution, as humans assumed an erect position.
An Italian-Canadian study [1] has shown that the distal insertion of the tendon on the radial tuberosity is bifurcated; the presence of a bursa allows it to slide smoothly around the tuberosity during pronation-supination of the forearm. In addition to this bifid tendon, there is a third distal structure known as the Lacertus fibrosus, or bicipital aponeurosis, which detaches from the medial aspect of the tendon, crosses over the median artery and median nerve, and inserts onto the superficial aponeurosis of the flexor muscles.
Passing over the scapulohumeral joint and that of the elbow, the biarticular biceps muscle continues its course on the anterior aspect of the arm, its sole aponeurotic insertion being that with the brachialis muscle situated below it.
The sonographic examination of these tendons focuses on nine separate zones of interest:
-
•
The glenoid insertion of the long head
-
•
Extension to the upper pole of the head of the humerus
-
•
The rotator interval
-
•
Reflection to the upper bicipital groove
-
•
The bicipital groove
-
•
The upper myotendinous junction
-
•
The lower myotendinous junction
-
•
Distal tendon(s)
-
•
Distal enthesis
In light of what we have just said, it is not surprising that we can find all types of tendon disorders here; each of these sectors, however, presents specific lesions.
Insertion of the long head on the superior pole and superior rim of the glenoid
This insertion is characterized by numerous anatomic variants. For the sonographer, its anterior and posterior topography is more important because only the anterior insertions can be visualized sonographically, while the arm is retropulsed and externally rotated (Fig. 1). Mathari [2] described how the topography of this insertion is related to the depth of the bicipital groove—i.e., the more posterior the insertion, the deeper the groove. Therefore, we can visualize (in patients who do not present with rigidity) only the insertions of tendons running through a relatively shallow groove. A precise lesional diagnosis is not possible. Hypoechoic tumefaction (evident on comparison with the contralateral side) is an indirect sign of pathology involving the insertion (superior labrum anterior posterior [SLAP] injuries), and it should be explored further with another diagnostic imaging modality (i.e., arthro-MRI or arthro-CT) [3].
Figure 1.
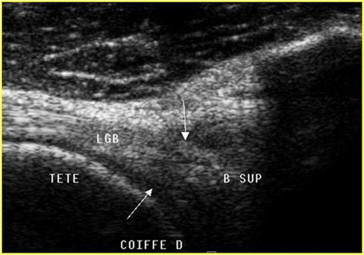
Insertion of the tendon of the long head of the biceps on the upper labrum, while the arm is in a position of retropulsion and externally rotation.
Extension to the upper pole of the humeral head
The arm is maintained in the same position (retropulsion with external rotation), and a scan is made perpendicular to the long head of the biceps at the level of the cephalic cartilage; this section must be comparative. Renoux [4] established that tendon thickness of >2.5 mm at this level should be considered pathological (Fig. 2).
Figure 2.
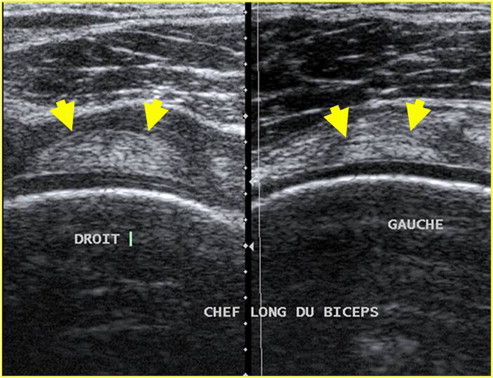
Comparative axial scan of the tendon of the long head of the biceps brachii at the level of the upper pole of the head of the humerus. The right tendon displays thickening (>2.5 mm), a finding indicative of tendinopathy.
This is an extremely important sign because biceps tendinopathy of this type is difficult to demonstrate with other techniques. Aside from the pain it produces, it can also cause problems of entrapment. As demonstrated by Boileau [5], the thickened tendon is unable to slide into the bicipital groove when the arm is abducted.
The rotator interval
The long head then passes into the space that separates the supraspinatus (posterolaterally) and subscapularis (anteromedially) tendons; this canal is covered by the coracohumeral ligament, which merges with the superior glenohumeral ligament to form a retention band that prevents medial luxation of the tendon (Fig. 3).
Figure 3.
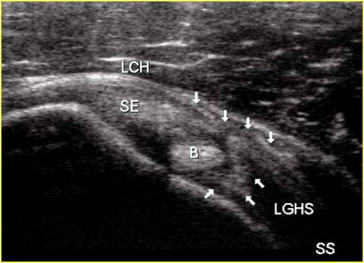
Ligament band that keeps the tendon of the long head within the interval; the superficial layer of the band is formed by the coracohumeral ligament and the deep layer of the superior glenohumeral ligament.
Tendinopathies involving the long head can be observed at this level, especially when the anterior part of the supraspinatus tendon is torn, which leads to retraction of the coracohumeral ligament. The tendon comes into direct conflict with the inferior aspect of the acromion, and this results in microtrauma, which is the cause of the tendinopathy [6]. The tendon appears thickened, hypoechoic, with relatively poorly defined margins (Fig. 4). Almost invariably, this condition is associated with substantial pain and inflammation, which make it difficult for the patient to sleep. It can lead to rupture of the tendon, which diminishes the pain. However, it can also cause cranial displacement of the head with scapulohumeral dysmobility.
Figure 4.
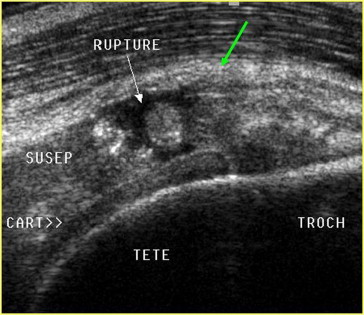
Biceps tendinopathy associated with rupture of the anterior supraspinatus; the tendon appears thickened and rounded.
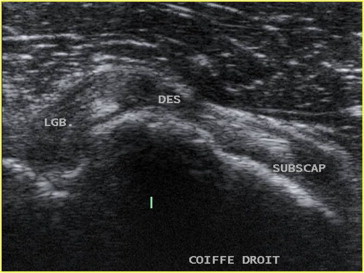
Disinsertion or rupture of the coracohumeral ligament can also lead to luxation of the long head of the biceps on the anterior side of the subscapularis tendon (Fig. 5).
Figure 5.
Rupture of the coracohumeral ligament causing luxation of the long head of the biceps on the anterior aspect of the subscapularis.
Traumatic ligament lesions and calcifications can also produce pain in the area of the rotator interval, and it is important to recall that thickening of the coracohumeral ligament is a valuable indirect sign of capsulitis, as demonstrated by Homsi [7].
Reflection to the upper part of the groove
At this level, the examination should focus mainly on excluding subluxation of the tendon. This phenomenon is facilitated by the angulation of the tendon, which leads to its medial displacement. As we have seen, the ligament band of the rotator interval provides support at this level. Stabilizing effects at the upper part of the groove are provided by the intact subscapularis muscle, which inserts on the medial aspect [of the groove], and its superficial aponeurosis covers the groove and inserts onto its lateral aspect. The depth of the groove itself is the other stabilizing factor [2].
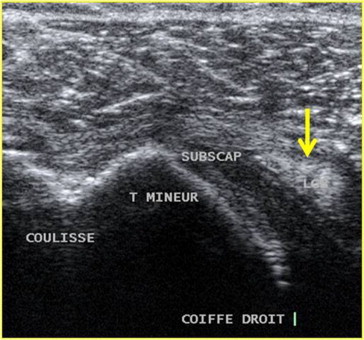
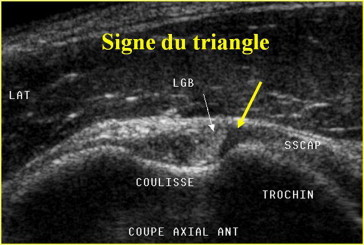
The first element that the sonographer should look for is the hypoechoic triangle, which consists histologically of collagen [2], that lies between the tendon of the long head and the medial border of the upper portion of the bicipital groove (Fig. 6). This triangle is present, regardless of the depth of the groove, and its presence confirms that the tendon of the long head is in its proper position. Its absence is a reliable indirect sign of subluxation (Fig. 7).
Figure 6.
Triangle sign: A hypoechoic zone located between the tendon and the medial border of the groove. Its presence indicates that the tendon is in its proper position.
Figure 7.
Disappearance of the hypoechoic triangle and tendinopathy of the long head. The borders of the tendon facing the medial edge of the groove are indistinct.
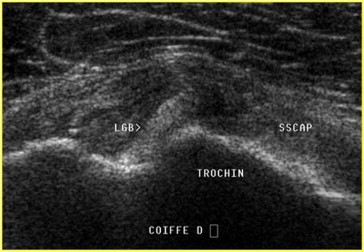
The examination should also exclude disinsertion of the subscapularis tendon. It is facilitated by fasciculation of the tendon, which facilitates its partial disinsertion. The fasciculation frequently begins in the upper part of the groove and later extends downward. The tendon of the long head extends on the medial border (Fig. 8) and then subluxates on the anterior facet of the lesser tuberosity and luxates within the joint [3]. The result is an inflammatory bicipital tendinopathy that is often extremely painful (especially at night), because the tendon is encased in a synovial sheath formed by a recess in the joint cavity.
Figure 8.
Subluxation of the tendon of the long head of the biceps caused by partial disinsertion of the subscapularis tendon; the tendon is extended on the medial border of the groove.
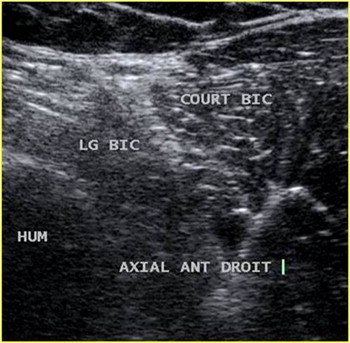
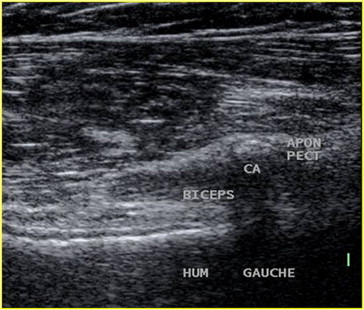
In the groove
Sonographic visualization of the tendon is sometimes hindered by anisotropy artifacts and by the cross-sectional shape of the tendon, which is ovoid with the long axis oblique anteriorly and oriented inward. In the longitudinal plane, the scan should be done in the sagittal–oblique plane with the tendon lying parallel to the probe. This requires anterior displacement of the elbow.
In the axial plane, the surfaces of the section and the definition of the tendon margins are examined; in the longitudinal plane, the focus of the examination is the fibrillar structure of the tendon.
The examination is carried out with the patient seated. Therefore, fluid that collects in dependent zones-i.e., an intra-articular, peritendinous effusion, is often observed in the lower part of the bicipital recess. This is an indirect sign of articular, capsular, ligament, or capsulolabial pathology. It may also be an indicator of bicipital tendinopathy, but the latter is by no means the rule: in the presence of tendinopathy, the entire recess may be completely occupied by the hypertrophic tendon, leaving no space for fluid to accumulate.
At this level, the main signs of tendinopathy are loss of the fibrillar structure on longitudinal scans and heterogeneous, hypoechoic thickening of the tendon on transverse scans; the cross section of the tendon frequently appears rounder and less ovoid (Fig. 9).
Figure 9.
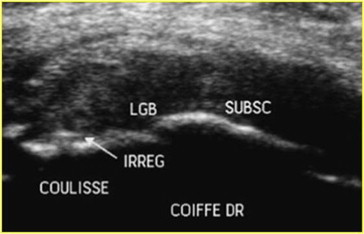
Tendinopathy of the long head of the biceps caused by post-traumatic irregularities of the cortical bone at the base of the groove; the tendon is thickened, rounded, heterogeneous.
Biceps tendinopathy has multiple causes that include subluxation, foreign bodies, bone irregularities within the groove, and the sequelae of tenodesis, but it can also be caused by a cyst that tends to cause buckling of the long head (Fig. 10).
Figure 10.
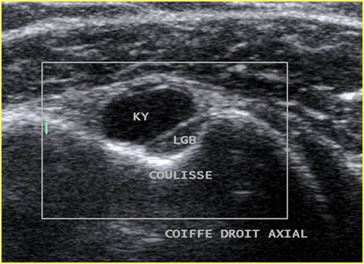
A cyst involving the tendon sheath exerts pressure on the tendon that leads to tendinopathy.
The long head sometimes presents longitudinal fissures. These are rare and should not be confused with the pseudofissures that result from the insertion of the coracohumeral ligament on the upper lateral aspect of the groove [8] (Fig. 11) or with duplication of the tendon (a morphological variant).
Figure 11.
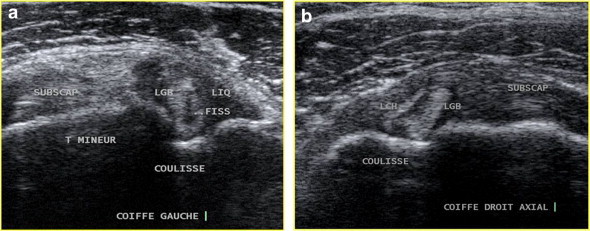
a: True fissuration of the tendon of the long head of the biceps. b: Pseudofissuration caused by insertion of the coracohumeral ligament on the lateral aspect of the groove.
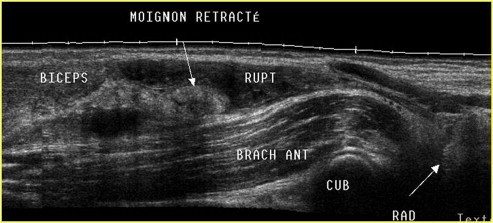
Rupture of the tendon is the third disorder [to look for] in this sector. If the rupture is recent, fragments of the tendon are easily visualized at the ends of both remnants (Fig. 12). With older ruptures (Fig. 13), the operator’s attention is attracted more by the “empty” appearance of the groove.
Figure 12.
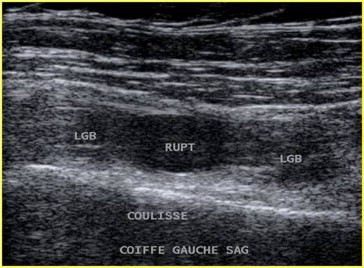
Recent rupture of the long head tendon in the lower part of the groove, with no stump retraction.
Figure 13.
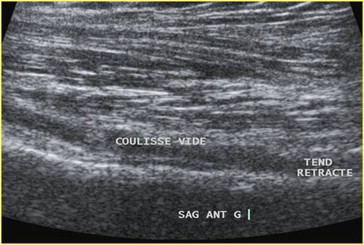
“Empty groove” produced by old rupture of the long head tendon.
The rupture may be partial. In that case, the sonographic diagnosis will be based on dynamic imaging in the transverse plane, like those used for nerve studies (lift technique).
The upper myotendinous junction
Rupture or disinsertion occurring at this level can produce hematomas, which are sometimes massive (Fig. 14) and other times barely detectable. The symptoms associated with rupture also vary widely, but in most cases they are short-lived, lasting no more than 1 or 2 weeks. The result is retraction of both tendon remnants, with a slack, poorly visualized tendon in the groove, and lowering of the muscle belly, which results in the classic “Popeye sign.”
Figure 14.
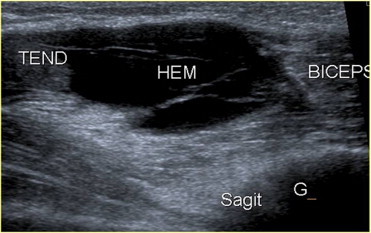
Hematoma caused by recent rupture/disinsertion of the superior myotendinous junction.
With time, fatty degeneration of the belly of the long head (but not the short head) results in another classic finding: the “black and white sign” [6] (Fig. 15).
Figure 15.
Hypoechoic muscle degeneration of the long head caused by an old rupture. The contrast between this muscle and the short head gives rise to the “black and white” aspect.
At this level, the main diagnostic difficulty arises with partial ruptures, which cause episodes of pain that are sometimes quite long. Sonographic diagnosis requires comparative studies of the contralateral limb (Fig. 16).
Figure 16.
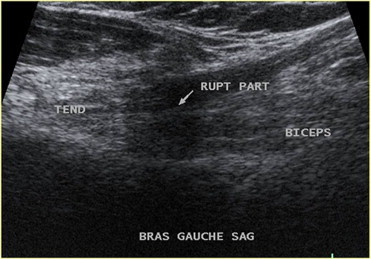
Partial rupture of the superior myotendinous junction associated with atypical pain and no muscle retraction.
It is also important to recall that the myotendinous junction is spanned by the tendon of the pectoralis major, which inserts on the shaft of the humerus. In this area, various disorders can mimic bicipital involvement, including disinsertion, but also calcific tendinitis, which must not be confused with osteochondroma of the base of the bicipital recess (Fig. 17).
Figure 17.
Calcific tendinopathy of the pectoralis major, which is in conflict with the underlying myotendinous junction.
The lower myotendinous junction
The lower myotendinous junction of the biceps is located very close to the surface and can be easily identified during palpation, which facilitates its localization during the sonographic examination. The most common lesions are ruptures, which cause cranial displacement of the muscle belly situated above the junction because the lesion is located above the origin of the L. fibrosus.
Other lesions at this level that can be difficult to diagnose are partial rupture and their sequelae, which lead to fibrous remodeling that causes chronic pain (Fig. 18).
Figure 18.
Focal hypoechoic remodeling caused by partial rupture of the inferior myotendinous junction, which was associated with chronic pain.
The distal tendon and its insertion
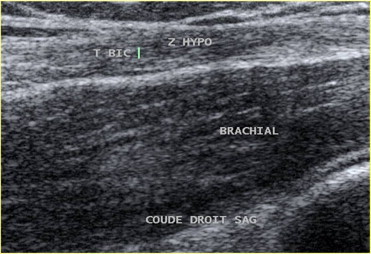
We have already described the anatomical complexity of this zone, which derives from the presence of a double tendon (Fig. 19) and of the L. fibrosus, which frequently prevent the cranial displacement of the muscle that follows tendon rupture.
Figure 19.
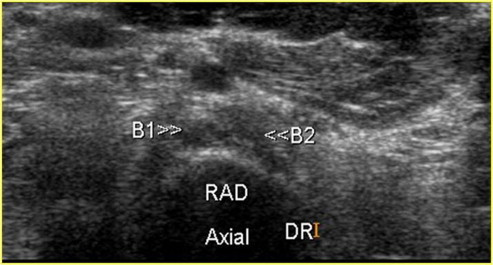
The anisotropy artifact can be used to distinguish the two components of the distal biceps tendon by rendering them hypoechoic.
The fact that this displacement does not occur is the main reason this type of lesion has such mild clinical manifestations; the second reason is related to the topographic location of the pain; most patients, in fact, are referred for sonographic examination of the forearm. The anomalous location of the pain is due to swelling of the damaged tendon, which causes compression of the surrounding blood vessels and nerves [9].
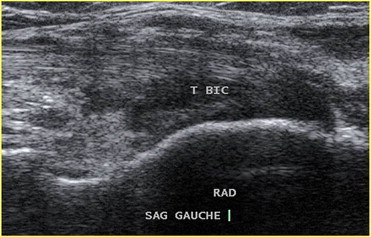
Sonographic exploration of this region is diabolically difficult owing to the curved course of the distal segment of the tendon.
Three examination techniques have been proposed for this purpose:
-
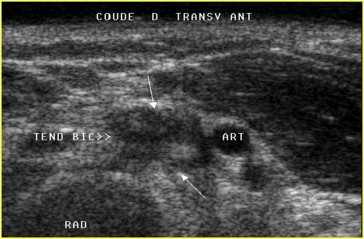
•
Craniocaudal exploration with the patient’s arm in forced supination. The examination begins with an axial scan of the myotendinous junction. Next one identifies the exact point at which the tendon begins to run along the lateral side of the artery. Still running lateral to the artery, the tendon then plunges deeper into the arm, where it frequently appears hypoechoic as a result of anisotropy. It should be followed to its insertion on the radial tuberosity. Considering the latter structure as a fixed point, the examiner rotates the arm 90° so that it can be examined in the sagittal plane.
-
•
The arm is maintained in forced supination, and the examination proceeds in a caudocranial direction, beginning with the tendon’s insertion on the radial tuberosity with the probe angled outward. In this case, one uses use the anisotropy artifact to render the tendon hypoechogenic and to maximize visualization of its margins. The probe is then moved upward, following the course of the tendon to the myotendinous junction.
-
•
A frontal approach with the patient’s arm flexed is sometimes easiest. It allows one to obtain images that are similar to those furnished by magnetic resonance imaging. This approach also allows the arm to be pronated and supination, which is useful for identifying areas of remodeling.
A variety of lesions can be observed at this level, including all types of tendon lesions except luxations.
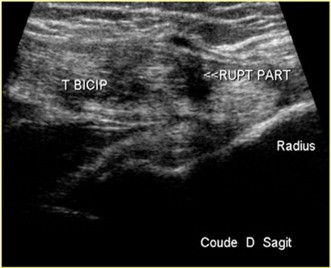
A: Tendon rupture
Rupture can be complete (involving both tendon bundles) or partial (only one of the bundles. Even when complete rupture occurs, displacement of the muscle belly is usually not observed owing to the persistence of the L. fibrosus. The stumps of the tendon, clearly swollen, are enclosed in a sheath (Fig. 20), which exerts pressure on nearby vessels and nerves, and dynamic testing is the only way to determine whether the rupture is complete [10].
Figure 20.
Complete rupture of the distal biceps tendon, which causes thickening of the tendon surface by lacerated tendon fragments and a reactive hematoma.
If the L. fibrosus is also torn, the examination reveals upward displacement of the muscle belly, an empty sheath, and a slack distal fragment (Fig. 21).
Figure 21.
Rupture of the distal tendon with muscle retraction due to coinvolvement of the lacertus fibrosus.
In the presence of partial rupture (involving one of the two bundles), there is no observable muscle displacement, but substantial swelling is seen within the sheath, where one finds a bundle with a normal fibrillar structure, but above all heterogeneous, thickened tendon fragments and a reactive hematoma (Fig. 22).
Figure 22.
Partial rupture of the distal tendon (one of the two bundles) causing thickening of the tendon surface by lacerated tendon fragments and a reactive hematoma.
B: Disinsertion of the tendon
Tendon detachment from its insertion may be partial or complete. In the former case, both bundles are detached from their radial insertions; in the latter case, one of the two bundles remains attached. The sonographic findings are identical to those observed with tendon rupture, the sole difference being the location of the lesions.
In the presence of complete detachment, the cortical bone of the radial tuberosity may also be detached. This requires surgical reinsertion but our experience indicates that cases of this type are quite rare.
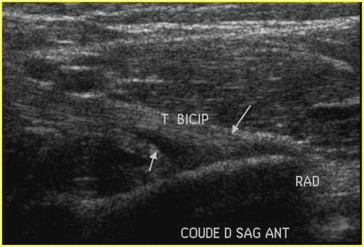
C: Tendinopathy
Tendinopathy is associated with chronic pain that has an insidious onset and progressive course. It causes loss of the fibrillar aspect of the tendon, the structure of which appears disorganized and accompanied by diffuse, heterogeneous thickening. The appearance of these forms of tendinopathy may be worsened by signs of fissuration. This calls for supplementary studies with the tendon relaxed, which are often done with the elbow slightly flexed to avoid collapse of the fissures during extension/supination. If the lesion is chronic, small, hyperechoic, spiculated fragments may be seen at its center.
D: Enthesopathy
Enthesopathies are far more common than tendinopathies. They are associated with hypoechoic swelling [11] that involves one (Fig. 24) or both (Fig. 23) of the tendons that insert on the radial tuberosity. To identify these lesions and assess their severity, the forearm should be placed in a position of forced supination although a posterior approach with the arm flexed (to 0°) can also be useful for this purpose.
Figure 24.
Partial distal enthesopathy (involving only one of the two tendon bundles). In this case the tumefaction involves only part of the insertion zone.
Figure 23.
Distal enthesopathy. Diffuse hypoechoic tumefaction of the distal extremity of the tendon at the level of its insertion on the radial tuberosity.
E: Peritendinopathy
This is often associated with the lesions described above, but certain patients with chronic pain have tendon sheath effusions that are not associated with tendon anomalies (Fig. 25). The fluid collections are always located at some distance from the zone of insertion, a feature that can be used to distinguish tendinopathy from bursitis.
Figure 25.
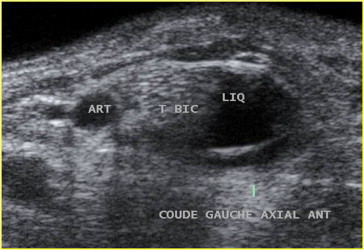
Peritendinopathy: An anechoic fluid collection surrounds the structurally intact tendon and can exert pressure on adjacent nerves and blood vessels.
F: Bursitis
Distention and inflammation of the tendon bursa, which allows the tendon to roll around radial tuberosity. The bursa, distended by a fluid collection, surrounds the distal extremity of the tendon (Fig. 26). The condition can be treated with US-guided infiltration.
Figure 26.
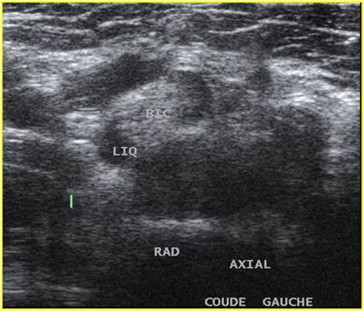
Bicipitoradial bursitis. The bursa, swollen in part by fluid, surrounds the extremity of the tendon at the level of its insertion.
Conclusion
Because of the morphological and topographical features, the biceps tendon—or tendons—can be affected by different types of lesions, some of which are frequently misdiagnosed on the basis of the clinical examination. Ultrasound plays an important role in detecting and characterizing these lesions. It is important to stress, however, that proper examination of the biceps (the distal portion in particular) is a difficult task that cannot be improvised.
Conflict of interest
The authors have no conflicts of interest to declare.
Appendix. Supplementary material
The following are the Supplementary material related to this article:
References
- 1.Tagliafico A., Michaud J., Capaccio E., Derchi L.E., Martinoli C. Ultrasound demonstration of distal biceps tendon bifurcation: normal and abnormal findings. Eur Radiol. 2010;20(1):202–208. doi: 10.1007/s00330-009-1524-1. [DOI] [PubMed] [Google Scholar]
- 2.Azaïez-Mathari A., Lemary J.B., Zeitoun-Eiss D., Brasseur J.L. Echo-anatomie du tendon du chef long du biceps. In: Brasseur J.L., Zeitoun-Eiss D., Dion E., editors. Actualités en échographie de l’appareil locomoteur. Sauramps Médical; Montpellier: 2004. pp. 229–245. [Google Scholar]
- 3.Brasseur J.L. Apport diagnostique de l’échographie dans la pathologie de la coiffe des rotateurs. In: Blum A., Tavernier T., Brasseur J.L., Noël E., Walch G., Cotten A., Bard H., editors. L’épaule une approche pluridisciplinaire. Sauramps Médical; Montpellier: 2005. pp. 149–170. [Google Scholar]
- 4.Renoux J., Zeitoun-Eiss D., Brasseur J.L. Tendinopathie du chef long du biceps: apport de l’imagerie. In: Brasseur J.L., Zeitoun-Eiss D., Renoux J., Grenier P., editors. Tome 3. Sauramps Médical; Montpellier: 2006. pp. 201–214. (Actualités en échographie de l’appareil locomoteur). [Google Scholar]
- 5.Boileau P., Ahrens P.M., Hatzidakis A.M. Entrapment oft he long head of the biceps tendon: the hourglass biceps- a cause of pain and locking of the shoulder. J Shoulder Elbow Surg. 2004;13(3):249–257. doi: 10.1016/j.jse.2004.01.001. [DOI] [PubMed] [Google Scholar]
- 6.Bianchi S., Martinoli C. Shoulder. In: Bianchi S., Martinoli C., editors. Ultrasound of the musculoskeletal system. Springer Verlag; Berlin, Heidelberg, New York: 2009. pp. 189–332. [Google Scholar]
- 7.Homsi C., Bordalo-Rodrigues M., da Silva J.J., Stump X.M. Ultrasound in adhesive capsulitis of the shoulder: is assessement of the coracohumeral ligament a valuable diagnostic tool? Skeletal Radiol. 2006;35(9):673–678. doi: 10.1007/s00256-006-0136-y. [DOI] [PubMed] [Google Scholar]
- 8.Brasseur J.L., Renoux J., Zeitoun-Eiss D. Causes d’erreur en échographie de la coiffe des rotateurs. In: Laredo J.D., Bellaiche L., Wybier M., editors. Savoir Faire en Radiologie ostéo-articulaire. Sauramps Médical; Montpellier: 2006. pp. 43–59. [Google Scholar]
- 9.Brasseur J.L., Parier J., Montalvan B., Bellaïche L., Renoux J., Zeitoun-Eiss D. Echographie de la portion inférieure du biceps. In: Brasseur J.L., Zeitoun-Eiss D., Renoux J., Grenier P., editors. tome 4. Sauramps Médical; Montpellier: 2007. pp. 253–268. (Actualités en échographie de l’appareil locomoteur). [Google Scholar]
- 10.Bach G., Zeitoun-Eiss D., Mercy G., Renoux J., Brasseur J.L. Echographie du tendon distal du biceps brachial. In: Brasseur J.L., Zeitoun-Eiss D., Bach G., Renoux J., Grenier P., editors. tome VII. Sauramps Médical; Montpellier: 2010. pp. 227–234. (Actualités en échographie de l’appareil locomoteur). [Google Scholar]
- 11.Brasseur J.L., Renoux J., Zeitoun-Eiss D. Imagerie du coude microtraumatique en fonction de l’hypothèse du clinicien: musculo-tendineux, capsulo-ligamentaire, ostéo-articulaire, neutro-vasculaire. In: Hérisson C., Rodineau J., editors. Le coude microtraumatique. Masson; Paris: 2006. pp. 35–47. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


