Abstract
Ovarian vein thrombosis (OVT) is an uncommon entity typically seen in the post-partum, patients with pelvic surgery, infection, or inflammation, and hypercoagulabilty. Concurrent pulmonary embolism (PE) may occur in these patients; however, is an uncommon complication. Treatment commonly involves anti-coagulation and antibiotics in the setting of pelvic inflammatory disease. Presented is a case report of ovarian vein thrombosis leading to pulmonary embolism in the setting of malignancy, underscoring the importance of inspecting the gonadal vein during interpretation, particularly in the emergency setting.
Keywords: Ovarian vein thrombosis, pulmonary embolism, computed tomography, PE, OVT
CASE REPORT
A 69 year old woman with metastatic pancreatic cancer to liver and spine on chemotherapy presents for routine imaging followup. Incidental thrombus was seen in the right ovarian vein (figures 1 and 2). Additional incidental subtle thrombus was seen in the right inferior pulmonary artery branch (figure 3). A four month prior exam demonstrated a normal appearance of the ovarian vein (figures 4 and 5) without pulmonary embolism (not shown). The patient had no symptoms referable to pulmonary embolism. The referring clinician was immediately notified and the patient started on anticoagulation. Routine 3 month follow up scan demonstrated resolution of the right ovarian vein thrombus (figure 6) and pulmonary embolism (not shown).
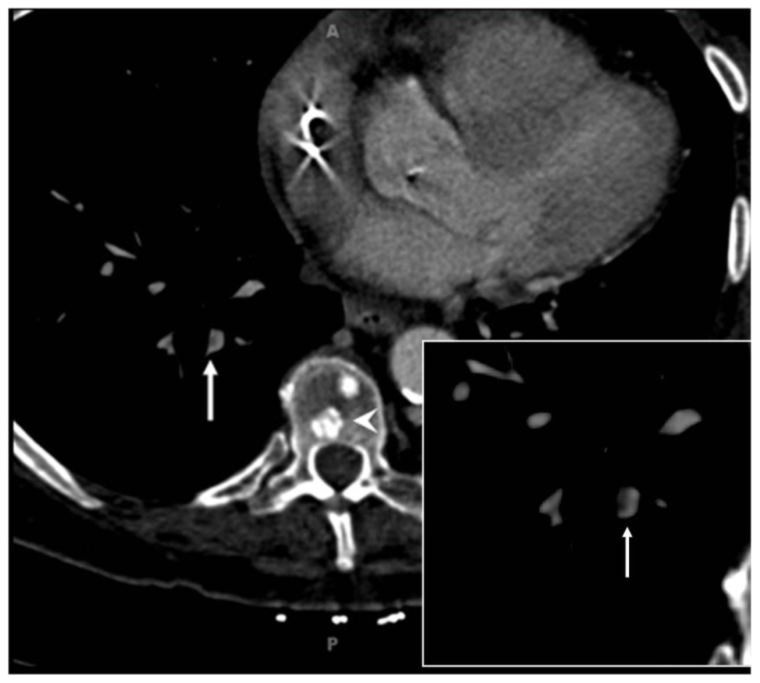
Figure 1.
69 year old woman with metastatic pancreatic cancer and incidentally identified ovarian vein thrombosis complicated by pulmonary embolism. Axial contrast enhanced CT (Siemens Sensation 64, 120 kVp, 325 mAs, 0.75 mm slice thickness, 100 ml Omnipaque 320, portal venous phase) demonstrating a filling defect in right ovarian vein as central hypodensity surrounded by dense contrast (long white arrow), consistent with thrombus. Magnification image insert with ovarian vein thrombus and ureter marked. Note the right ovarian vein is medial to right kidney and anterior to right ureter. The left ovarian vein marked with short arrow demonstrating homogenous opacification without thrombus contrary to right ovarian vein.
Figure 2.
69 year old woman with metastatic pancreatic cancer and incidentally identified ovarian vein thrombosis complicated by pulmonary embolism. Coronal contrast enhanced CT scan (Siemens Sensation 64, 120 kVp, 325 mAs, 3 mm slice thickness, 100 ml Omnipaque 320, portal venous phase) demonstrating dilated (7 mm) right ovarian vein medial to right kidney with a long segment filling defect consistent with thrombus (long white arrows). Also note extensive low density ill-defined hepatic masses consistent with metastatic disease (not marked). Contralateral left ovarian vein (arrow heads) demonstrates homogenous opacification and normal caliber of 3–4 mm.
Figure 3.
69 year old woman with metastatic pancreatic cancer and incidentally identified ovarian vein thrombosis complicated by pulmonary embolism. Thin section axial contrast enhanced CT (Siemens Sensation 64, 120 kVp, 325 mAs, 0.75 mm slice thickness, 100 ml Omnipaque 320, arterial phase) in soft tissue window demonstrating subtle filling defect (white arrows) in right lower lobe pulmonary arterial branch, consistent with pulmonary embolism. Magnification view insert demonstrates thrombus as focal hypodensity within vessel (arrow). Sclerotic osseous metastases are denoted by white arrowhead within thoracic vertebral body. Mediport catheter tip artifact is seen in the right atrium (not marked).
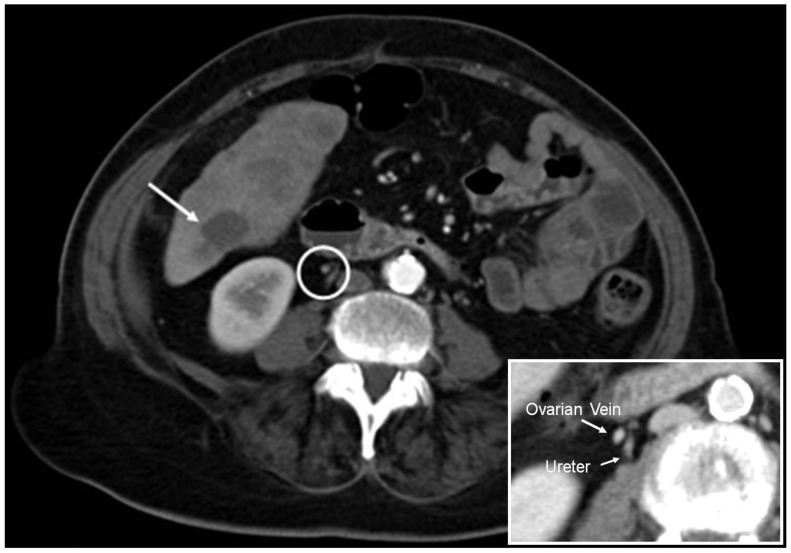
Figure 4.
69 year old woman with metastatic pancreatic cancer and incidentally identified ovarian vein thrombosis complicated by pulmonary embolism. Axial contrast enhanced CT (Siemens Sensation 64, 120 kVp, 350 mAs, 5 mm slice thickness, 100 ml Omnipaque 320, portal venous phase) image from four month prior CT exam demonstrating normal appearance of the ovarian vein as a homogenous focal opacity (white circle) without filling defect. One of many liver metastases is marked by a long white arrow. Insert magnification view labels right ovarian vein and right ureter. Note small well opacified, patent, right ovarian vein adjacent to ureter (marked).
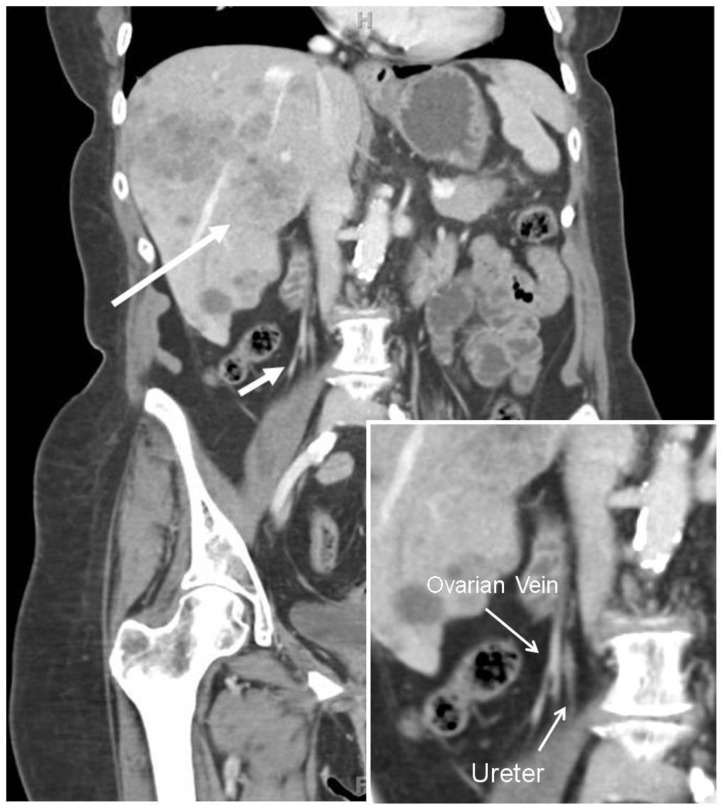
Figure 5.
69 year old woman with metastatic pancreatic cancer and incidentally identified ovarian vein thrombosis complicated by pulmonary embolism. Coronal contrast enhanced CT (Siemens Sensation 64, 120 kVp, 350 mAs, 5 mm slice thickness, 100 ml Omnipaque 320, portal venous phase) reconstruction from four month prior exam demonstrating normal caliber (3–4 mm), homogenously opacified right ovarian vein lateral to right ureter (short large white arrow). One of many liver metastases is marked by a long white arrow. Insert magnification view labels right ovarian vein and right ureter (thin white arrows). Note small well opacified, patent, right ovarian vein of normal caliber (3–4 mm).
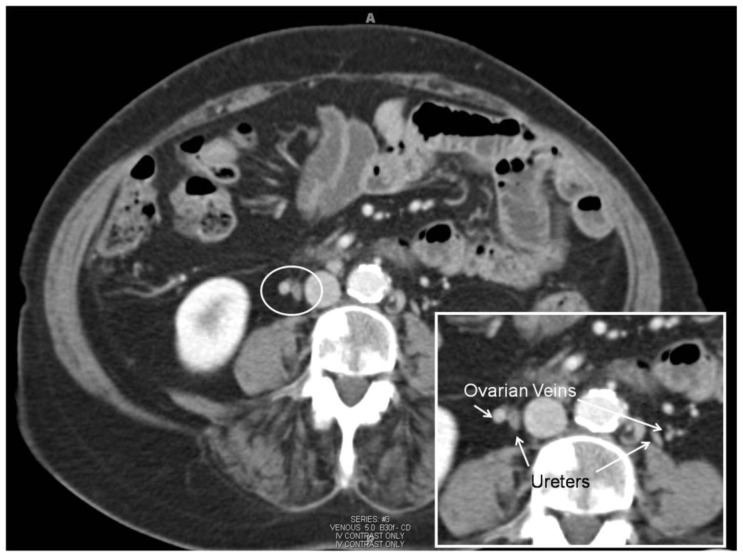
Figure 6.
69 year old woman with metastatic pancreatic cancer and incidentally identified ovarian vein thrombosis complicated by pulmonary embolism. 3 month follow-up CT (Siemens Sensation 64, 120 kVp, 350 mAs, 5 mm slice thickness, 100 ml Omnipaque 320, venous phase) after anticoagulation demonstrating resolution of right ovarian vein filling defect (figure 1a) which now demonstrates well opacified, normal caliber (3–4 mm), right ovarian vein (white circle). Note the sclerotic metastases through the imaged vertebral body (not marked). Magnification insert view demonstrates well-opacified, normal caliber (3–4 mm), both ovarian veins and ureters marked (white arrows). Note normal caliber ovarian veins are anterior and lateral to ureters (marked).
DISCUSSION
Introduction
Pulmonary embolism has an incidence of 1 in 1000 persons per year in the United States, for about 250,000 incident annual cases [1]. Early detection and treatment with anticoagulation is critical to decrease morbidity and mortality [2]. Ovarian vein thrombosis (OVT) causing pulmonary embolism is rare event, with limited etiologies such as postpartum endometritis, post gynecological surgery, pelvic inflammatory disease, and hypercoagulable states such as malignancy [3].
Anatomy
The ovarian veins originate from a venous plexus near the ovary and fallopian tubes and course over the psoas muscle and ureters. The right ovarian vein drains into the inferior vena cava and left renal vein on the left [4]. They normally measure about 3–4 mm in diameter [5]. The vein can be easily visualized at the level of the inferior mesenteric artery as it is surround by fat. [4].
Diagnosis
A thrombosed ovarian vein will be dilated with central hypodensity and peripheral hyperdensity or targetoid appearance on post contrast CT imaging. The sensitivity of contrast enhanced CT to detect OVT approaches 100% although may be overlooked by the inexperienced radiologist given infrequent presentation [6]. Differential of a filling defect on CT would include admixture flow artifact from unopacified blood mixing with opacified blood. This is commonly seen in the femoral veins and inferior vena cava. To our knowledge, on noncontrast imaging, the vein may be normal caliber or expanded, depending on clot burden. The thrombus would likely be isodense and difficult to impossible to visualize without contrast.
Etiology, Presentation, and Prognosis
Pregnancy, being the commonest cause for OVT, occurs with an incidence of 0.05% to 0.018% after vaginal birth and up to 2% after cesarean section [7]. 80–90% of ovarian vein thrombosis will occur on the right side. This is thought to occur due to mass effect from the gravid uterus causing stasis [8]. Thrombus may then embolize to the lungs, being potentially fatal, hence close attention to this location is highly important. The risk of embolization has been estimated to be approximately 13% in one study [8]. To our knowledge, this is the only recent study that quantifies the risk of embolism. These patients may present with right lower quadrant pain and fever [9].
Other less common causes include pelvic inflammatory disease, post pelvic surgery, or hypercoagulablity from, for example, malignancy and hematological disorders [10]. These patients will present with the symptoms respective to the disease process. OVT may be asymptomatic as some patients who have undergone hysterectomy. Study by Yassa et al [11] followed 50 patients after total abdominal hysterectomy and bilateral salpingo-oophorectomy who developed OVT, 75% involving the right ovarian vein. None of these patients developed pulmonary embolism, even after 2 years of followup [11].
OVT can be incidentally identified on imaging for other indications, as in our case, for routine malignancy followup. One series by Jacoby et al [3], followed 6 oncology patients with gonadal vein thrombosis; four with metastatic breast cancer, one with metastatic pancreatic cancer, and one with metastatic adenocarcinoma of unknown primary. These patients did not get anticoagulation nor developed pulmonary embolism. In three patients, thrombosis persisted for up to one year without symptoms [3].
Treatment
Ovarian vein thrombosis is usually treated with antibiotics and anticoagulation given OVT usually occurs in the setting of post-partum endometritis. Although risk for pulmonary embolism is low, these patients are at most risk [7–9]. Treating OVT in the setting of malignancy is debatable without clear evidence for benefit from anticoagulation [10–11]. OVT after hysterectomy is unlikely to be treated given its appearance as a common post-surgical finding [11].
TEACHING POINT
Ovarian vein thrombosis is a rare, yet highly important, entity to recognize, due to possibility of causing pulmonary embolism. Inspection of ovarian veins should be part of every CT interpretation, particularly in the setting of pregnancy, malignancy, pelvic infection and surgery, as a small clot may be overlooked.
Table 1.
Summary table for ovarian vein thrombosis
| Etiology | Idiopathic, hypercoaguable states |
| Incidence | Rare, exact number unknown |
| Gender ratio | Unknown |
| Age predilection | Unknown |
| Risk factors | Gynecological surgery, pelvic inflammatory disease, malignancy |
| Treatment | None versus anticoagulation, both are controversial |
| Prognosis | Favorable on anticoagulation or post hysterectomy, poor in post-partum |
| Findings on imaging | Central filling defect within ovarian vein, typically on right, during venous phase on CT scan |
Table 2.
Differential diagnosis table for ovarian vein thrombosis
| CT | Ultrasound | MRI | Angiography | |
|---|---|---|---|---|
| Ovarian vein thrombosis | Central filling defect surrounded by dense contrast | Echogenic mass expanding vein, noncompressible, no flow | T1 focal hyperintense vein, T2 hyperintense, no flow void on spin echo sequences | Non-opacified vein, filling defect |
| Mixing artifact | Heterogeneous, low to intermediate density | Reverberation artifact, slow flow artifact, incorrect Doppler settings | Flow-related enhancement when vessel in plane with imaging slice | Poor injection |
ABBREVIATIONS
- CT
Computed Tomography
- OVT
Ovarian Vein Thrombosis
- PE
Pulmonary Embolism
REFERENCES
- 1.Horlander KT, Mannino DM, Leeper KV. Pulmonary embolism mortality in the United States, 1979–1998 an analysis using multiple-cause mortality data. Arch Intern Med. 2003;163(14):1711–7. doi: 10.1001/archinte.163.14.1711. [DOI] [PubMed] [Google Scholar]
- 2.Barritt DW, Jordan SC. Anticoagulant drugs in the treatment of pulmonary embolism. A controlled trial. Lancet. 1963;1(7138):1309–1312. doi: 10.1016/s0140-6736(60)92299-6. [DOI] [PubMed] [Google Scholar]
- 3.Jacoby WT, Cohan RH, Baker ME, Leder RA, Nadel SN, Dunnick NR. Ovarian thrombosis in oncology patients: CT detection and clinical significance. AJR. 1990 Aug;155(2):291–294. doi: 10.2214/ajr.155.2.2115254. [DOI] [PubMed] [Google Scholar]
- 4.Govil S, Justus A. Using the ovarian vein to find the ovary. Abdom Imaging. 2006;31:747–750. doi: 10.1007/s00261-005-0268-x. [DOI] [PubMed] [Google Scholar]
- 5.Coakley FV, Varghese SL, Hricak H. CT and MRI of pelvic varices in women. J Comput Assist Tomogr. 1999;73:429–434. doi: 10.1097/00004728-199905000-00018. [DOI] [PubMed] [Google Scholar]
- 6.Savader SJ, Otero RR, Savader BL. Puerperal ovarian vein thrombosis: evaluation with CT, US and MR imaging. Radiology. 1998;167:637–639. doi: 10.1148/radiology.167.3.3283835. [DOI] [PubMed] [Google Scholar]
- 7.Ortin X, Ugarriza A, Espax RM, Boixadera J, Llorente A, Esocoda L, et al. Postpartum ovarian vein thrombosis. Thromb Haemost. 2005;93:1004–5. [PubMed] [Google Scholar]
- 8.Dunnihoo DR, Gallaspy JW, Wise RB, Otterson W. Postpartum ovarian vein thrombophlebitis: a review. Obstetric Gynecological Survey. 1991;46:415–27. doi: 10.1097/00006254-199107000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Dhinakar M, Dhinakar L, Kamona A, Saifudeen A. Puerperal ovarian vein thrombosis presenting as right loin pain and hydronephrosis: Report of 2 cases. OMJ. 2010;25(4):299–302. doi: 10.5001/omj.2010.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hippach M, Meyberg R, Villena-Heinsen C, Mink D, Ertan AK, Schmidt W, et al. Postpartum ovarian vein thrombosis. Clin Exp Obstet Gynecol. 2000;27:24–6. [PubMed] [Google Scholar]
- 11.Yassa NA, Ryst E. Ovarian vein thrombosis: a common incidental finding in patients who have undergone total abdominal hysterectomy and bilateral salpingo-oophorectomy with retroperitoneal lymph node dissection. AJR. 1999;172:45–7. doi: 10.2214/ajr.172.1.9888736. [DOI] [PubMed] [Google Scholar]
- 12.Kuehnl A, Assadian A, Reeps C, Schneider CTM, Stangl M, et al. Floating Caval Thrombus Arising from the Ovarian Vein. Annals of Vascular Surgery. 2009;23(5):688.e7–688.e9. doi: 10.1016/j.avsg.2009.03.012. [DOI] [PubMed] [Google Scholar]