Abstract
Megacystis microcolon intestinal hypoperistalsis syndrome is a rare congenital anomaly. Several pathogeneses have been described so far, but there is no single mechanism that can explain all the findings of the syndrome. Affected newborns usually present clinically in the first few days of life. The mainstay of diagnosis is a pre or a postnatal imaging evaluation using ultrasound or magnetic resonance imaging. We report an unusual urinary tract finding in a patient with the classic triads of the syndrome that was diagnosed with both pre and postnatal imaging evaluation.
Keywords: Megacystis, Microcolon, Hypoperistalsis
CASE REPORT
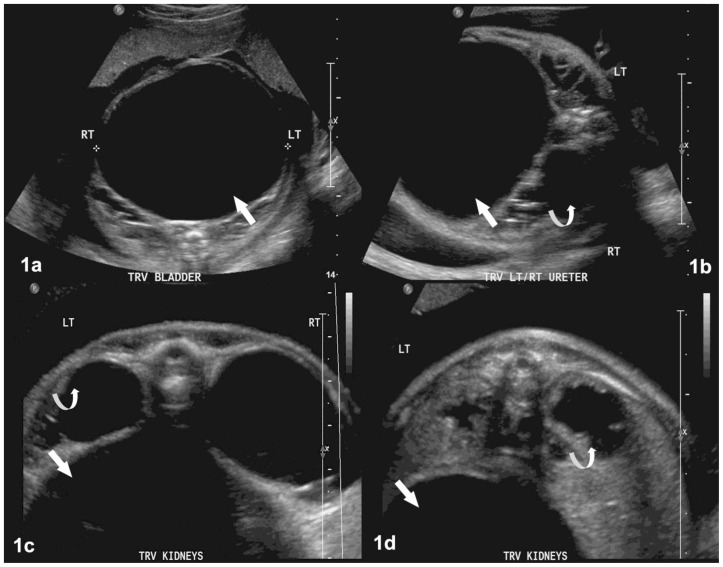
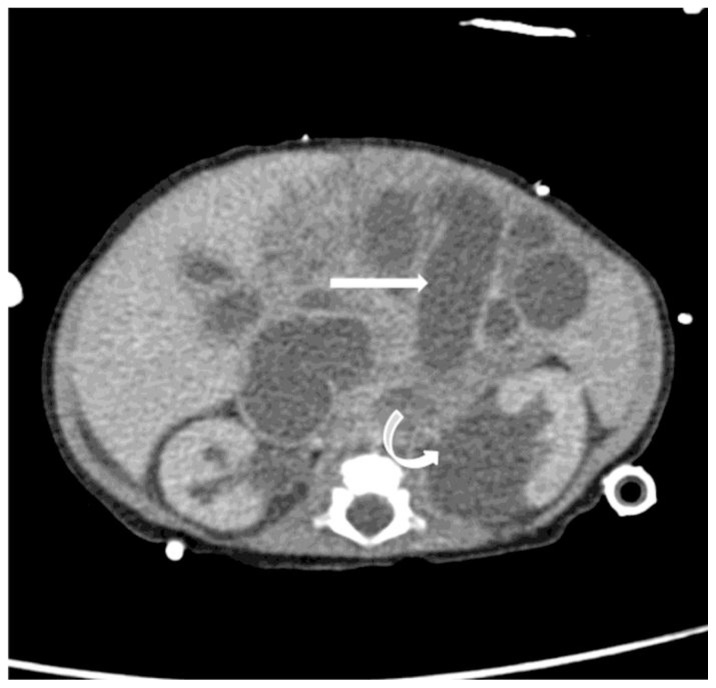
A 23-year-old primigravid patient was referred to our hospital because of abnormal pre-natal ultrasound (US) findings noted at an outside institution. Sonographic evaluation of the fetus at 27 weeks of gestation at our hospital revealed a markedly distended urinary bladder, severe bilateral megaureters and pelvicaliectasis in combination with polyhydramnios (Fig. 1). Fetal magnetic resonance imaging (MRI) confirmed the sonographic findings and also demonstrated markedly distended proximal small bowel loops and diminutive distal colon (Fig. 2). Based on this constellation of findings, the diagnosis of megacystis microcolon intestinal hypoperistalsis syndrome (MMIHS) was made. The mother was followed expectantly and gave birth to a female neonate at 36 weeks of gestation. The diagnosis of MMIHS was confirmed with postnatal US, computerized tomography (CT) (Figure 3) and contrast enema examinations. All the features of the syndrome including a massively enlarged urinary bladder, small colon and distended proximal bowel loops having little or no peristalsis were identified. However, an unusual and striking radiographic appearance was noted on an antero-posterior (AP) abdominal radiograph taken on the fifth postnatal day. There was a large air filled structure in the mid abdomen that was concerning for a loculated free intra-peritoneal air or a massively distended bowel loop. Further evaluation with a decubitus radiograph and US demonstrated that the gas filled structure was actually the urinary bladder. A repeat radiograph the same day showed the presence of air refluxing into the ureters and collecting systems as well (Fig. 4). A voiding cystourethrography (VCUG) performed at the age of 20 days further confirmed the findings by depicting the intravesical gas as a filling defect in the urinary bladder. An associated grade 1 reflux was also noted on the left side (Fig. 5). The delay in doing the VCUG is attributed to the initial difficulty in recognizing the air to be intravesical. Decompression of the distended bladder was performed at the bedside under ultrasound guidance with a syringe that resulted in drainage of a large amount of urine and air. Post procedure radiographic evaluation showed marked improvement. The patient later underwent laparoscopic evaluation at 2 months of age that confirmed a megacystis, a malrotated microcolon and multiple small intestinal atresias. A fistula to the bladder was not clearly identified. At surgery, multiple enterotomy stricturoplasties and primary bowel anastomoses were performed. The patient is being evaluated for potential small bowel transplantation.
Figure 1.
Prenatal US images of a 27 weeks old female fetus with the diagnosis of Megacystis Microcolon Intestinal Hypoperistalsis Syndrome (MMIHS): Axial plane imaging at different levels (1a–1d) using a Philips scanner with a 3.5 MHz curved transducer demonstrate a markedly distended urinary bladder (straight white arrows) and severe ureteropelvicaliectasis with thinned out renal parenchyma bilaterally (curved white arrows).
Figure 2.
MR Image of this female fetus with a diagnosis of MMIHS at 27 weeks of gestational age in sagital (2a) coronal (2b) and axial (2c) planes. (Protocol: 1.5T MR scanner, T2 Half Fourier Acquisition Single Shot Turbo Spin Echo (HASTE) sequence, TR=1100, TE=84, no contrast). There is a markedly distended urinary bladder (straight arrow) with ureteropelvicaliectasis and marked renal parenchymal thinning (curved arrows). The bowel loops are compressed posteriorly and a diminutive colon was noted on another plane (not shown). There was an associated polyhydramnios detected (black curved arrow).
Figure 3.
Axial contrast enhanced computed tomography (CT) scan of the abdomen performed at the age of 2 months in this female infant with MMIHS revealed markedly distended, fluid-filled small bowel loops (straight arrow) and bilateral ureteropelvicaliectasis (curved arrow) which was more severe on the left side. There was no free intraperitoneal air detected (protocol: 36mAs, 80kV, 3mm slice thickness, with 8ml Iohexol (Omnipaque 300, GE health care, Princeton, NJ) injection).
Figure 4.
A frontal (4a) and lateral (4b) abdominal radiographic evaluation of this female neonate with a diagnosis of MMIHS at the age of five days demonstrated a distended, air-filled bladder (straight arrow) and air outlining the renal collecting systems (curved arrows).
Figure 5.
A lateral view from a VCUG performed in this female neonate with MMIHS at the age of 20 days showed a distended urinary bladder with evidence of intravesical air and air contrast level (curved arrow). A grade I vesicoureteric reflux was noted on the left side (straight arrow).
DISCUSSION
MMIHS is a rare congenital syndrome that was first described in 1976 by Berdon et al (1). It represents the most severe form of functional intestinal obstruction in the newborn and is generally associated with a fatal outcome. So far there have been 227 reported cases of this syndrome (2). There is a clear preponderance to female neonates (F:M ratio of 2.4:1) but male neonates usually present with the most severe form of the disease (2). Several hypotheses including genetic, myogenic, neurogenic and hormonal abnormalities have been reported as possible mechanisms in the pathogenesis of MMIHS. However, none of these were found to be the sole mechanism and a multifactorial etiology involving interplay of all the above factors is more plausible (3). Affected neonates present clinically in the first few days of life with abdominal distention, bilious emesis, failure to pass meconium and inability to void. Prognosis is generally poor with death occurring in the first few weeks or months of life (2, 4). Imaging plays a central role in diagnosing MMIHS both during pregnancy and after delivery. Although fetal US evaluation was previously reported to be the modality of choice for prenatal diagnosis of MMIHS, this has significantly changed after the advent of fetal MRI (5, 6). It has been shown that fetal MRI is superior in visualizing the abnormal bowel, bladder and the collecting systems (5). The excellent depiction of the abnormalities in the prenatal MR imaging of our case also reiterates this fact. Multimodality imaging and laparoscopic evaluation of the newborn also demonstrated findings in keeping with MMIHS. To our knowledge the findings of a urinary tract massively distended with air in a newborn has not been previously described in conjunction with MIMHS or for that matter with any other condition. The gas filled distended bladder, ureters and pelvicalyces on plain abdominal radiographs were very striking. No definite iatrogenic cause could be elucidated. No fistulous communication between the bladder and bowel was visualized during surgery. A urine culture failed to demonstrate a bacterial pathogen. High-grade bilateral vesicoureteric reflux must have been present that was not depicted on the VCUG to explain the air in both pelvicalyces. Following drainage of the bladder, the air progressively disappeared and was not found to reappear. In summary, no etiology was found to explain the self limiting massive air in the collecting systems.
Having a neonate with dilated bilateral renal collecting systems with an enlarged bladder should make one think of a neurogenic bladder with severe vesicoureteric reflux, urethral obstruction or bladder neck obstruction (with any or all combinations of these). In a male infant, megacystis with hydronephosis is most commonly secondary to posterior urethral valves (PUV). In our case report the patient was female which excludes this diagnosis. The diagnostic considerations when having megacystis include PUV in males, Prune-Belly syndrome and MMIHS [7]. Prune-Belly is a much rarer cause of megacystis and occurs almost exclusively in males with stigmata of cryptorchidism and absence/abnormal abdominal wall musculature. Finally, the diagnostic considerations for microcolon include ileal atresia, meconium ileus, proximal colonic atresia and total colonic aganglionosis [8]. Usually these entities present alone and not so closely associated with hydronephosis and megacystis as in our case. Meconium ileus is always seen in neonates with cystic fibrosis which can be diagnosed using specific laboratory studies like the sweat chloride test. Total colonic aganglionosis can be confirmed by colon biopsy revealing the absence of normal ganglion cells. Intestinal hypoperistalsis can occur in situations where there is diffuse intestinal neuronal dysplasia. Although the constellation of all three findings, severely dilated urinary bladder, microcolon and hypoperistalsis of the intestines, steer the clinician and radiologist to the diagnosis of MMIHS, each of these entities separately has a differential diagnosis.
TEACHING POINT
Megacystis microcolon intestinal hypoperistalsis syndrome (MMIHS) is a rare congenital anomaly characterized by a triad of markedly dilated non-obstructed urinary bladder, microcolon and decreased or absent intestinal peristalsis. Diagnosis is made with pre- or postnatal abdominal US and/or MRI. The radiologist should be aware of the possibility of unusual presentation of air filled bladder, ureters and pelvicalyces in this syndrome.
Table 1.
Presentation and Imaging of Most Important Differential Diagnoses for MMIHS
| Clinical features | X-ray (KUB) | US | Fluoroscopy (VCUG or Enema) | MRI (fetal) | |
|---|---|---|---|---|---|
| URINARY TRACT FINDINGS | |||||
| Posterior urethral valves | -Males -Urine retention -Dribbling -Urinary ascites -UTI -Sepsis |
-Normal -Shadow of distended bladder |
-Dilated bladder -Thickened wall -Trabeculations -Dilated posterior urethra (‘key-hole” configuration) -Hydronephrosis -Ascites -Small dysplastic kidneys |
-Dilated posterior urethra - With or without dilated and trabeculated bladder - Urethral valves may be seen |
-Fetal hydronephrosis -Distended urinary bladder -Urinary ascites -Oligohydramnios |
| Prune Belly syndrome | -Males -Distended abdomen with laxity of anterior abdominal wall -Decreased urine output |
-Bulging flanks -Distended bladder |
Dysplastic kidneys -Cryptorchidism -Hydronephrosis -Dilated ureters |
-No bladder trabeculation -Conical narrowing of posterior urethra - Anterior urethra atresia -Stenosis or megalourethra -VUR -Urachal remnant |
Absent or hypoplastic abdominal wall muscles -Megacystis -Dysplastic kidneys -Oligohydramnios |
| Neurogenic bladder | May have predisposing neurologic abnormality (i.e. spina bifida, cerebral palsy) | -Signs of enlarged bladder in pelvis or normal | Distended bladder with thickened and trabeculated wall | -Elongated, upward pointing bladder -Trabeculations (Christmas tree appearance) +/− VUR |
-Megacystis Thickened bladder wall +/− hydronephrosis |
| Vesicoureteric reflux (VUR) | Urinary tract infections -Fever -Pyuria -Bacteriuria |
Normal | -Bilateral hydronephosis -Dilated ureters -Normal or echogenic kidneys |
-Reflux of contrast from bladder to ureters | Fetal hydronephrosis |
| MICROCOLON | |||||
| Ileal atresia | -Abdominal distention -Failure to pass meconium -Bilious emesis |
-LOW obstruction -Distended bowel with air- fluid levels |
-Dilated loops of bowel filled with hypoechoic fluid or air | Microcolon with contrast filling normal caliber SB with sharp transition at site of obstruction into dilated SB | -Dilated fluid filled bowel -Little meconium in the colon +/− polyhydramnios |
| Meconium Ileus | -Abdominal distention -Failure to pass meconium -Cystic fibrosis |
-LOW obstruction- Dilated SB -Air mixed with meconium in RLQ “soap- bubble” pattern -Calcifications -Mass effect from pseudocyst -Perforation |
-Dilated bowel filled with hyperechoic luminal content (meconium) -Calcifications -Walled off pseudocyst -Males: calcifications in scrotum |
Microcolon filled with meconium seen as filling defects -Contrast ends in dilated SB filled with meconium |
-Dilated bowel -Abdominal calcifications -Large pseudocyst |
| Total colonic aganglionosis | -Abdominal distention -Failure to pass meconium |
-Features of low bowel obstruction -Many dilated loops of bowel |
-Dilated loops of bowel filled with meconium or just fluid -Non-specific appearance |
-Normal colon -Microcolon -Pseudotransition in left colon -Or normal short colon “?” colon |
-Non-specific findings |
Table 2.
Summary of clinical and imaging findings in patients with Megacystis microcolon intestinal hypoperistalsis syndrome (MMIHS)
| Etiology | Unknown, probably multifactorial involving an interplay of genetic, myogenic, neurogenic and hormonal abnormalities |
| Incidence | Rare, 227 cases reported so far |
| Gender ratio | F:M= 2.4:1 |
| Age at presentation | Neonates, in the first few days of life |
| Treatment | Surgical correction |
| Prognosis | Poor, most patients die within the first few years of life |
| Imaging findings |
Prenatal imaging: US and MRI will demonstrate a markedly enlarged urinary bladder (with possible dilatation of upper urinary tract), small colon, and diminished intestinal peristalsis. An associated maternal polyhydramnios will be detected. The findings are more clearly seen on fetal MRI. Postnatal imaging: ultrasound of the neonate can further demonstrate the marked bladder enlargement, dilated small bowel loops with diminished peristalsis. VCUG may be needed to evaluate the presence of vesicoureteric reflux. Plain abdominal x-ray may be used if there is a clinical suspicion of free peritoneal air. |
ABBREVIATIONS
- AP
antero-posterior
- CT
computerized tomography
- HASTE
Half Fourier Acquisition Single Shot Turbo Spin Echo
- MMIHS
Megacystis microcolon intestinal hypoperistalsis syndrome
- MRI
magnetic resonance imaging
- US
ultrasound
- VCUG
voiding cystourethrography
REFERENCES
- 1.Berdon WE, Baker DH, Blanc WA, Gay B, Santulli TV, Donovan C. Megacystis-microcolon-intestinal hypoperistalsis syndrome: a new cause of intestinal obstruction in the newborn. Report of radiologic findings in five newborn girls. AJR Am J Roentgenol. 1976;126(5):957–64. doi: 10.2214/ajr.126.5.957. [DOI] [PubMed] [Google Scholar]
- 2.Gosemann JH, Puri P. Megacystis microcolon intestinal hypoperistalsis syndrome: systematic review of outcome. Pediatr Surg Int. 2011;27(10):1041–6. doi: 10.1007/s00383-011-2954-9. [DOI] [PubMed] [Google Scholar]
- 3.Puri P, Shinkai M. Megacystis microcolon intestinal hypoperistalsis syndrome. Semin Pediatr Surg. 2005;14(1):58–63. doi: 10.1053/j.sempedsurg.2004.10.026. [DOI] [PubMed] [Google Scholar]
- 4.White SM, Chamberlain P, Hitchcock R, Sullivan PB, Boyd PA. Megacystis-microcolon-intestinal hypoperistalsis syndrome: the difficulties with antenatal diagnosis. Case report and review of the literature. Prenat Diagn. 2000;20(9):697–700. doi: 10.1002/1097-0223(200009)20:9<697::aid-pd891>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 5.Munch EM, Cisek LJ, Jr, Roth DR. Magnetic resonance imaging for prenatal diagnosis of multisystem disease: megacystis microcolon intestinal hypoperistalsis syndrome. Urology. 2009;74(3):592–4. doi: 10.1016/j.urology.2009.02.071. [DOI] [PubMed] [Google Scholar]
- 6.Melek M, Edirne Y, Beger B, Cetin M. Megacystis- microcolon-intestinal hypoperistalsis syndrome: a case report. Gastroenterol Res Pract. 2009;2009:282753. doi: 10.1155/2009/282753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bulas D, Farmer D. Caffey’s pediatric diagnotic imaging. 11th ed. Philadelphia: Mosby; 2008. perinatal diagnosis and therapy of abdominal, pelvic, retroperitoneal abnormalities; pp. 162–163. [Google Scholar]
- 8.Bloom D, Slovis T. Caffey’s pediatric diagnotic imaging. 11th ed. Philadelphia: Mosby; 2008. congenital anomalies of the gastrointestinal tract; p. 205. [Google Scholar]