Abstract
Tuberculous epididymo-orchitis is a rare complication of intravesical Bacillus Calmette-Guérin (BCG) therapy for urothelial cancer of the bladder. We present such a case, describe its sonographic appearance and review the literature. The difficulties in diagnosing this condition based on imaging alone, given the extensive overlap with the appearance of bacterial epididymo-orchitis, malignant testicular disease and testicular torsion, are discussed. Adequate knowledge of tuberculous epididymo-orchitis is of capital importance in order to ensure a proper diagnosis and treatment.
Keywords: Tuberculous epididymo-orchitis, intravesical Bacillus Calmette-Guérin, BCGitis, granulomatous epididymo-orchitis, tuberculosis, epididymitis
CASE REPORT
A 76-year-old man, with a history of diabetes mellitus type II, hypertension, pericarditis, coronary artery disease and without any previous urological history presented to the emergency room with an intermittent history of hematuria. He was diagnosed with papillary urothelial carcinoma of the bladder and treated with transurethral resection of bladder tumor (TURBT) as well as six treatment of intravesical instillation of BCG. During the following 7 years, he had several recurrences for which he had other transurethral resections and mitomycin chemotherapy.
Seven years after his initial diagnosis of bladder cancer, the patient presented to the emergency room with left testicular pain. He was clinically diagnosed with epididymo-orchitis and treated with a 7-day course of antibiotics which partially relieved his symptoms. Two months later, the patient returned to the emergency room with similar symptoms and was diagnosed and treated for another episode of epididymo-orchitis.
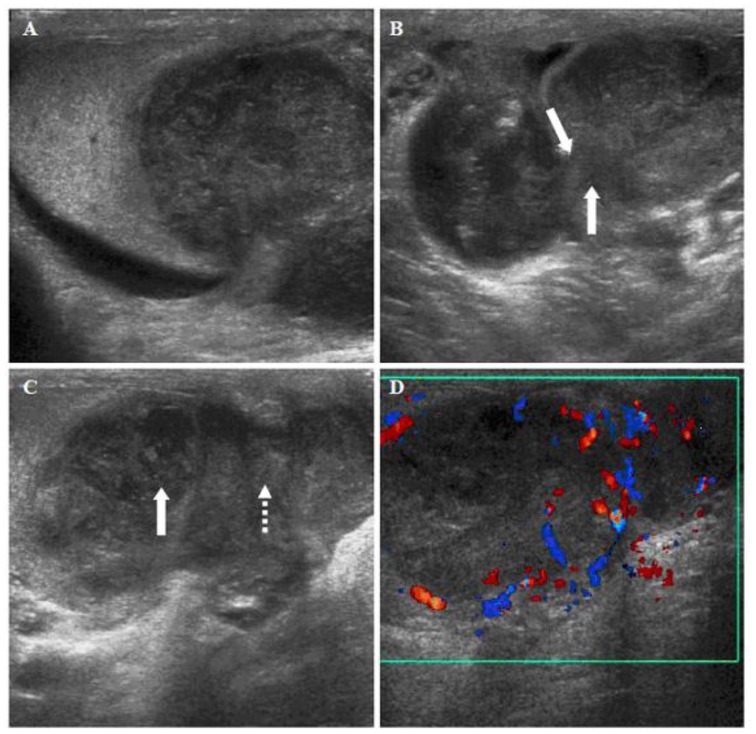
Five months later, the patient returned for the third time with left testicular pain, swelling and a new testicular mass. An ultrasound of the testicle was performed (Figure 1), showing a heterogeneous 3.2 × 3.2 × 2.8 cm mass in the inferior portion of the left testicle which appeared continuous with the epididymal tail. Low-grade internal flow was noted upon Doppler interrogation as well as peripheral linear flow. In addition, the testicular mass was contiguous with a second medial extra-testicular nodule, also demonstrating peripheral linear flow and measuring 2.7 ×2.2 cm. A small hydrocele was present. There was no significant skin thickening. The upper portion of the left testicle, the left epididymal head and body and the right scrotal content were normal. A malignancy was initially suspected by imaging.
Figure 1.
76-year-old male with left tuberculous epididymo-orchitis. Sonographic views of the left testicle, including Doppler ultrasound. A Longitudinal image shows a heterogeneous mass in the inferior portion of the testicle; B transverse image of the lower testicle shows continuity (white arrow) of the testicular lesion (right side) with an extra-testicular lesion medially; C longitudinal image demonstrates extension of the epididymal mass (dotted arrow) into the lower pole of the testicle (white arrow); D Doppler ultrasound of the testicle and epididymis shows internal hypovascularity and peripheral increased flow. (All images obtained with a 12 MHz linear transducer)
The patient was treated with a 2-week course of ciprofloxacin and given a urological follow-up appointment. One month following this treatment, he was seen in the urology clinic. A left radical orchiectomy was planned and performed on the basis of increasing size of the left testicular mass and lack of response to antibiotics.
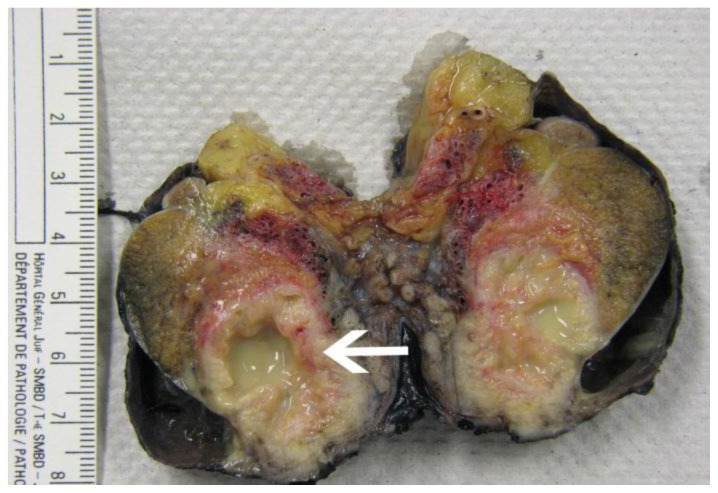
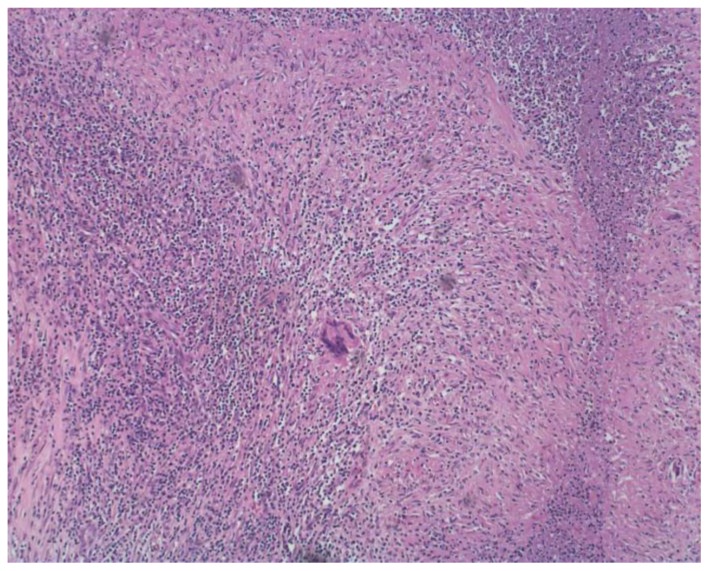
Macroscopically, the left testicle contained an exophytic mass which, upon dissection, demonstrated a necrotic nodule measuring 3.2 ×3.2 × 2.8 cm (Figure 2). The mass was partly intra-testicular and partly extra-testicular, extending beyond the tunica albuginea and the testicular capsule to the tail of the epididymis. On pathological analysis (Figure 3), the left testicle showed multiple necrotizing granulomas with presence of rare acid-fast bacilli. The assay for M. tuberculosis DNA by PCR method was positive. Final cultures grew Mycobacterium bovis, the organism used in BCG therapy. The patient was started on anti-tuberculous treatment.
Figure 2.
76-year-old male with left tuberculous epididymo-orchitis. Macroscopic pathology. Transection of the left testicle and epididymis demonstrates a necrotic caseating nodule measuring 3.2 × 3.2 × 2.8 cm (white arrow).
Figure 3.
76-year-old male with left tuberculous epididymo-orchitis. Microscopic pathology, Hematoxylin and Eosin (H&E) stain. Low power view reveals multiple necrotizing granulomas with central areas of necrosis surrounded by collections of epithelioid histiocytes as well as many Langerhans multinucleated giant cells and a chronic inflammatory infiltrate.
DISCUSSION
“BCGitis”, or BCG-induced tuberculous epididymo-orchitis, is a rare granulomatous infection caused by Bacillus Calmette-Guérin therapy. It has been described in a small number of cases to affect several anatomic locations including the lungs [1], the liver [2,3], the bone marrow and bones [4], the kidneys [5], the eyes [6], the vessels [7,8], the prostate, the epididymis and the testicles [10].
The bacillus of Calmette-Guérin (Figure 4, Table 1) is an attenuated strain of Mycobacterium bovis, initially produced as a vaccine against tuberculosis, but introduced in 1972 as an intravesical treatment for urothelial cancer of the bladder. When instilled into the bladder, these mycobacterias cause an inflammatory/immune reaction responsible for the destruction of tumor cells. It is currently considered, in combination with TURBT, as the treatment of choice for lesions staged T1 (carcinoma extending to the lamina propria but not involving the muscular layer) or less [11].
Table 1.
Summary table for BCG-related tuberculous epididymo-orchitis.
| Etiology | Mycobacterium bovis, used as an intravesical treatment for urothelial cancer of the bladder |
| Incidence | 0.4% of patient treated with intravesical BCG |
| Gender Ratio | Male only |
| Age predilection | Generally, men older then 60 years old |
| Risk factors | Intravesical treatment with BCG, recent instrumentation or catheterization, immunocompromised state, recent urological trauma |
| Treatment | 300 mg of isoniazid for 3 months supplemented with rifampin and isonicotinylhydrazine (INH) with or without fluoroquinolones for 3–6 months +/− corticosteroids |
| Prognosis | Orchiectomy can be avoided if promptly diagnosed and treated |
| Ultrasonography | Variable. Classically, diffuse enlargement with heterogeneous hypoechoic appearance of the epididymis, nodular enlargement of the testis with heterogeneous hypoechoic appearance, linear or focal Doppler signal at the periphery of the epididymis, intra-scrotal extra-testicular calcifications, caseous abscess, sinus tract and skin thickening |
We report a case of tuberculous epididymo-orchitis following intravesical treatment with BCG.
Granulomatous epididymo-orchitis is a rare complication from intravesical BCG therapy for urothelial bladder cancer, with only 12 previous cases described, to our knowledge, in the English literature. A previous extensive study showed that genito-urinary complications occurred in only 0.9% of patients treated with intravesical BCG [9]. Risk factors for “BCGitis” include intravesical treatment with BCG, recent instrumentation or catheterization, immunocompromised state and recent urological trauma.
Clinically, patients usually present with painful or painless scrotal enlargement. Local symptoms may rarely be accompanied by fever and leukocytosis [11].
The infection usually starts as discrete or conglomerate necrotic areas in the epididymis. Whether it begins in the tail of the epididymis [12,13] or initially involves its entire body [14] remains a point of contention. The testis may become involved, either from direct extension from the epididymis or from hematogenous spread [15]. Isolated tuberculous orchitis from hematogenous spread without epididymal involvement is rare [14,17].
Distinct gray scale sonographic patterns of granulomatous epididymitis have been described and include 1) diffuse enlargement of the epididymis with either a heterogeneous or homogeneous hypoechoic appearance and 2) nodular enlargement of the epididymis with a heterogeneous hypoechoic appearance [12–15].
Similarly, individual gray scale sonographic patterns of granulomatous orchitis have been described and include 1) diffuse enlargement of the testis with either a heterogeneous or homogeneous hypoechoic appearance, 2) nodular enlargment of the testis with heterogeneous hypoechoic appearance and 3) multiple small hypoechoic nodules (miliary appearance) in the enlarged testis [12–14].
Other associated sonographic findings include thickened scrotal skin, hydrocele, lack of clear separation between the epididymis and the testis, intra-scrotal extra-testicular calcification (in the epididymis and in the tunica vaginalis of the testis), scrotal abscess, and scrotal sinus tract [15].
The radiological appearance of granulomatous or tuberculous epididymo-orchitis can be a diagnostic challenge, especially given its similarity to bacterial epididymo-orchitis, malignant testicular disease and testicular torsion. Its diagnosis however remains of critical importance for clinical management.
Differentiating tuberculous epididymo-orchitis from bacterial infection
In cases of bacterial infection, patients typically present with fever, dysuria, and severe scrotal pain. Sonographically, diffuse enlargement of the epididymis with hypoechogenicity is usually characteristic of non-tuberculous epididymitis while in most of the reported case of tuberculous epididymo-orchitis, heterogeneity of the epididymis, which is thought to be caused by the various stages of granulomatous infection (caseation necrosis, granuloma formation and fibrosis), was a distinctive sonographic feature [12–14]. The presence of calcifications from chronicity or of a sinus tract draining necrotic pus from a caseous abscess may also enhance the heterogeneous echotexture of the epididymis in tuberculous epididymitis [14]. On color Doppler sonography, non-granulomatous epididymitis usually shows Doppler signal within the affected epididymis whereas granulomatous epididymitis may show linear or focal Doppler signal at the periphery of the epididymis [17].
Differentiating tuberculous epididymo-orchitis from testicular malignancy
The presence of epididymal enlargement together with a testicular lesion is suggestive of an infection rather than a neoplastic process because orchitis is almost always caused by epididymitis, whereas tumors usually partially involve the epididymis from direct extension only in the advanced stage [18]. The sonographic detection of skin thickening and hydrocele is also suggestive of infection rather than testicular tumors.
Differentiating tuberculous epididymo-orchitis from testicular torsion
The sonographic appearance of testicular torsion in the acute phase is usually a diffuse hypoechoic enlargement of the testis while in the later phase, it is heterogeneous secondary to hemorrhage and necrosis. Reactive hydrocele and skin thickening may also occur. In such circumstances where the findings of tuberculous epididymo-orchitis and testicular torsion overlap, color Doppler ultrasound is useful, as venous blood flow in patients with testicular torsion is reduced or absent, whereas it is increased in cases of infection.
Lastly, a history of intravesical BCG instillation and failure of conventional antibiotic therapy are helpful clues in establishing the diagnosis of “BCGitis”. Knowledge of the sonographic appearance of tuberculous epididymo-orchitis and its common mimickers help ensure an accurate diagnosis and appropriate management.
The most recent recommendations for the treatment of localized M. Bovis BCG infection consist of 300 mg of isoniazid for 3 months supplemented with rifampin and isonicotinylhydrazine (INH) with or without fluoroquinolones for 3–6 months [19]. The regimen varies for systemic M. Bovis BCG infection and/or sepsis. Although the diagnosis is often established after orchiectomy because of a suspicion of testicular cancer, as in this case, if BCG-induced granulomatous epididymo-orchitis is part of the differential diagnosis, a biopsy should first be performed.
TEACHING POINT
The radiological appearance of granulomatous or tuberculous epididymo-orchitis can be a diagnostic challenge, especially given its similarity to bacterial epididymo-orchitis, malignant testicular disease and testicular torsion. While the diagnosis of tuberculous epididymo-orchitis has traditionally been made by histological examination following surgery, awareness of its sonographic appearance should help avoid unnecessary orchiectomy.
Table 2.
Sonographic appearance of different testicular lesions included in the differential diagnosis of granulomatous or tuberculous epididymo-orchitis
| Epididymis | Testis | Doppler | Other possible characteristics | |
|---|---|---|---|---|
| Granulomatous or tuberculous epididymo-orchitis | Diffuse enlargement with heterogeneous or rarely homogeneous hypoechoic appearance | Nodular enlargement with heterogeneous hypoechoic appearance or Diffuse testicular enlargement with multiple small hypoechoic nodules | Linear or focal Doppler signal at the periphery of the epididymis | Intra-scrotal extra-testicular calcifications Caseous abscess Sinus tract Skin thickening |
| Bacterial epididymo-orchitis | Diffuse enlargement with homogeneous hypoechoic appearance | Diffuse enlargement with heterogeneous or homogeneous hypoechoic appearance | Diffuse increased blood flow in the epididymis | Fever Dysuria Scrotal pain Hydrocele Skin thickening |
| Malignant testicular lesion | Normal unless rare direct extension | Mass of mixed echogenicity | Mixed vascularity in the testis | Calcifications Cysts |
| Testicular torsion | Normal appearance or Diffuse enlargement with hypoechoic appearance | Normal parenchymal or Diffuse enlargement with hypoechoic (early) or heterogeneous (late) appearance | Reduced or absent blood flow in the testis | Hydrocele Skin thickening Pain |
ABBREVIATIONS
- BCG
Bacillus Calmette-Guérin
- TURBT
Transurethral resection of bladder tumor
- PCR
Polymerase chain reaction
REFERENCES
- 1.Martin Escudero JC, Pérez Peredes G, Asensio Sánchez T, Herreros Fernández V. Granulomatous pneumonitis due to BCG. An Med Interna. 2003;20:105–106. (article in Spanish) [PubMed] [Google Scholar]
- 2.Hunt JS, Silverstein MJ, Sparks FC, Haskell CM, Pilch YH, Morton DL. Granulomatous hepatitis: a complication of BCG immunotherapy. Lancet. 1973;ii:820–821. doi: 10.1016/s0140-6736(73)90860-x. [DOI] [PubMed] [Google Scholar]
- 3.Leebeek FW, Ouwendijk RJ, Kolk AH, Dees A, Meek JC, Nienhuis JE, Dingemans-Dumas AM. Granulomatous hepatitis caused by bacillus Calmette-Guérin (BCG) infection after BCG bladder instillation. Gut. 1996;38:616–618. doi: 10.1136/gut.38.4.616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dederke B, Riecken EO, Weinke T. A case of BCG sepsis with bone marrow and liver involvement after intravesical BCG instillation. Infection. 1998;26:54–57. doi: 10.1007/BF02768758. [DOI] [PubMed] [Google Scholar]
- 5.Soda T, Hori D, Onishi H, Miyakawa M. Granulomatous nephritis as a complications of intrarenal bacille Calmette-Guérin therapy. Urology. 1999;53:1228. doi: 10.1016/s0090-4295(98)00499-3. [DOI] [PubMed] [Google Scholar]
- 6.Guex-Croisier Y, Chamot L, Zogrfos L. Chorioretinitis induced by intravesical Bacillus Calmette-Guérin (BCG) instillations for urinary bladder carcinoma. Klin Montsbl Augenheilkd. 2003;220:193–195. doi: 10.1055/s-2003-38179. [DOI] [PubMed] [Google Scholar]
- 7.Wolf YG, Wolf DG, Higginbottom PA, Dilley RB. Infection of a ruptured aortic aneurysm and an aortic graft with bacillus of Calmette-Guérin after intravesical administration for bladder cancer. J Vasc Surg. 1995;22:80–84. doi: 10.1016/s0741-5214(95)70092-7. [DOI] [PubMed] [Google Scholar]
- 8.Rozenblit A, Wasserman E, Marin ML, Veith FJ, Cynamon J, Rozenblit G. Infected aortic aneurysm and vertebral osteomyelitis after intravesical bacillus Calmette-Guérin therapy. Am J Roentgenol. 1996;167:711–713. doi: 10.2214/ajr.167.3.8751686. [DOI] [PubMed] [Google Scholar]
- 9.Lamm DL, van der Meijden APM, Morales A, Brosman SA, Catalona WJ, Herr HW, Soloway MS, Steg A, Debruyne FM. Incidence and treatment of complications of bacillus Calmette-Guérin intravesical therapy in superficial bladder cancer. J Urol. 1992;147:596–600. doi: 10.1016/s0022-5347(17)37316-0. [DOI] [PubMed] [Google Scholar]
- 10.Sylvester RJ, van der Meijden AP, Lamm DL. Intravesical bacillus Calmette-Guérin reduces the risk of progression in patients with superficial bladder cancer: a meta-analysis of the published results of randomized clinical trials. J Urol. 2002;168:1964–70. doi: 10.1016/S0022-5347(05)64273-5. [DOI] [PubMed] [Google Scholar]
- 11.Türkvatan A, Kelahmet E, Yazgan C, Olçer T. Sonographic findings in tuberculous epididymo-orchitis. J Clin Ultrasound. 2004;32(6):302–5. doi: 10.1002/jcu.20035. [DOI] [PubMed] [Google Scholar]
- 12.Kim SH, Pollack HM, Cho KS, Pollack MS, Han MC. Tuberculous epididymitis and epididymo-orchitis: sonographic findings. J Urol. 1993;50(1):81–4. doi: 10.1016/s0022-5347(17)35404-6. [DOI] [PubMed] [Google Scholar]
- 13.Drudi FM, Laghi A, Iannicelli E, Di Nardo R, Occhiato R, Poggi R, Marchese F. Tubercular epididymitis and orchitis: US patterns. European Radiology. 1997;7(7):1076–78. doi: 10.1007/s003300050257. [DOI] [PubMed] [Google Scholar]
- 14.Chung JJ, Kim MJ, Lee T, Yoo HS, Lee JT. Sonographic findings in tuberculous epididymitis and epididymo-orchitis. J Clin Ultrasound. 1997;25(7):390–4. doi: 10.1002/(sici)1097-0096(199709)25:7<390::aid-jcu7>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 15.Muttarak M, Peh WC, Lojanapiwat B, Chaiwun B. Tuberculous epididymitis and epididymo-orchitis: sonographic appearances. AJR Am J Roentgenol. 2001;176(6):1459–66. doi: 10.2214/ajr.176.6.1761459. [DOI] [PubMed] [Google Scholar]
- 16.Tessler FN, Tublin ME, Rifkin MD. US case of the day. Tuberculous epididymoorchitis. Radiographics. 1998;18:251–253. doi: 10.1148/radiographics.18.1.9460131. [DOI] [PubMed] [Google Scholar]
- 17.Yang DM, Chang MS, Oh YH, Yoon MH, Kim HS, Chung JW. Chronic tuberculous epididymitis: color Doppler US findings with histopathologic correlation. Abdom Imaging. 2000;25:569–562. doi: 10.1007/s002610000092. [DOI] [PubMed] [Google Scholar]
- 18.Muttarak M, Peh WC. Case 91: Tuberculous Epididymo-orchitis. Radiology. 2006;238(2):748–51. doi: 10.1148/radiol.2382031851. [DOI] [PubMed] [Google Scholar]
- 19.Watts MR, Taylor PC, Sintchenko V, Whelan C, Farnworth RH, Jones P, Jelfs P, Carr D, Goldberg H. Implications of Isoniazid Resistance in Mycobacterium bovis Bacillus Calmette-Guérin used for Immunotherapy in Bladder Cancer. Clin Infect Dis. 2011;52(1):86–88. doi: 10.1093/cid/ciq002. [DOI] [PubMed] [Google Scholar]