Abstract
Purpose
This report compares the skeletal stability and treatment outcomes of 2 similar cohorts undergoing bilateral sagittal osteotomies of the mandible for advancement. The study groups included patients stabilized with 2-mm self-reinforced polylactate (PLLDL 70/30), biodegradable screws (group B), and 2-mm titanium screws placed in a positional fashion (group T).
Materials and Methods
Sixty-nine patients underwent bilateral sagittal osteotomies of the mandibular ramus for advancement utilizing an identical technique. There were 34 patients in group B and 35 patients in group T. Each patient had preoperative, immediate postoperative, splint out, and 1-year postoperative cephalometric radiographs available for analysis. The method of analysis and treatment outcomes parameters are identical to those previously used. Repeated measures analysis of variance was performed with means of fixation as the between-subject factor and time as the within subject factor. The level of significance was set at .01.
Results
There were no clinical failures in group T and a single failure in group B. The average difference in stability between the groups is small and subtly different at the mandibular angle. The data documented similarity of the postsurgical changes in the 2 groups with the only statistically significant difference being the vertical position of the gonion (P < .001) and the mandibular plane angle (P < .01) with greater upward remodeling at gonion in group T.
Conclusions
Two-mm self-reinforced PLLDL (70/30) screws can be used as effectively as 2-mm titanium screws to stabilize the mandible after bilateral sagittal osteotomies for mandibular advancement. The difference in 1-year stability and outcome is minimal.
Biodegradable internal fixation has become increasingly popular in many orthopedic applications and has gained wide acceptance in pediatric craniofacial surgery, where heavy loading of the osteotomy sites rarely occurs and therefore the initial strength of the material is not a major consideration.1,2 Initial reports suggested that biodegradable fixation might not have enough strength for orthognathic procedures, and there has been reluctance to apply this technology to orthognathic surgery because of concerns about the strength of the material, the added time necessary to place it, and the possibility of inflammation or complications related to the degradation process.3,4 The major advantages of biodegradable fixation are that functional stress is gradually transferred to the bone as it remodels and matures, which allows bone to heal to its original strength. The materials almost never require surgical removal, and potentially can be used as a vehicle to release bone healing mediators.5 It appears that implantable copolymers now have adequate strength to maintain most osteotomy sites in approximation while initial bone healing occurs, making them suitable for orthognathic surgery.6,7
Although titanium is the standard for bone plates and screws for human use, it has been reported that the material can be found in local and regional lymph nodes years after placement.8,9 The pathologic consequence, if any, is unknown and the titanium debris has never been definitively linked to a disease. Once the titanium serves the purpose of maintaining the position of bone segments during healing, it is no longer necessary. The most common reasons for removing it, as usually is done in multiple European countries, are concerns of infection and thermal sensitivity. In the United States, sinus symptoms, infection, or the desire of the patient because the plate or screw is palpable are the primary reasons for removal and the incidence has been reported to be 10%.10 In our unit patients are counseled that there is about an 8% chance of necessary removal because of symptoms or infection. Another reason for removal is concern about shielding the bone from normal functional stress, which ultimately influences bone strength, but whether this is clinically significant for orthognathic surgery is not known. Removal of titanium is not always easy. Sometimes osseointegration occurs, and when this happens, removal of bone is necessary to free the material. Breakage during removal can occur, and when this happens the surgeon must decide if it is more prudent to leave the remaining material or continue with removal.
The exact composition of biodegradable materials varies among manufacturers, and the low-grade inflammatory response to biodegradation that occurs is dependent on many factors. These include the exact material used, the method used to form the material, the sterilization process, how it was handled clinically, the amount of material used, and the perfusion of tissues overlying the materials once implanted.11 Polylactate is the principal polymer used in most biodegradable bone plates and screws, with other polymers (usually polyglycolate) added to alter strength and degradation characteristics, and other materials (often trimethylcarbonate) incorporated to improve workability.4 Polylactate originally was supplied using only the l-isomer, and more recently as a mixture of the l- and d-isomers (PLLDL) to enhance the degradation process. The physical properties of polylactate screws are significantly affected by the manufacturing process. Extrusion maximizes cross-links within the material and increases strength. This is a patented process and is only used by a single manufacturer who no longer distributes in North America. Injection or heat molding results in less strength and the need to preheat the material to bend.
The most prevalent postsurgical problem with the usual procedure for mandibular advancement, bilateral sagittal split osteotomy (BSSO), is neurosensory alteration. Symptoms of temporomandibular dysfunction (TMD) also have been reported after this surgery. A recent research report shows that the occurrence of postoperative sensory disturbances and temporomandibular problems after BSSO is not different with conventional titanium screws and biodegradable polylactate screws.11
Stability after mandibular advancement with wire and rigid internal fixation has been studied extensively, and the data are summarized in a recent text.12,13 In a study of sagittal split osteotomies in severely affected patients who required major bone movement, Landes and Kriener reported that biodegradable plates provided adequate stability when 2 plates were attached to each side, but 27% of the patients had complications that included relapse.14 In a prospective study of more typical mandibular advancement with 20 patients in each group, Ferretti and Reyneke reported no difference in stability between patients with copolymer resorbable screws and titanium screws.15 The purpose of this study is to provide comparative information about internal fixation by 2-mm self-reinforced PLLDL (70/30) screws (Bionx; Linduetech Corp, Jacksonville, FL) used to stabilize sagittal osteotomies for mandibular advancement.
Methods
The 69 patients included in this study were treated for isolated mandibular deficiency with bilateral sagittal osteotomies of the mandible with or without genioplasty. None underwent any other orthognathic surgery. All were operated with a standardized technique, and the majority (100% of those with biodegradable screws [group B] and 60% of those with titanium screws [group T]) were operated by a single surgeon (TAT). The ramus was fixated with four 2-mm screws placed transorally in a positional fashion as previously described.16 All but one had associated orthodontic treatment, and all had intermaxillary elastics postsurgically. Their demographic and surgical characteristics are shown in Table 1.
Table 1.
DEMOGRAPHIC AND SURGICAL CHARACTERISTICS OF PATIENTS IN THE BIODEGRADABLE AND TITANIUM SCREW FIXATION GROUPS
| Biodegradable (n = 34)
|
Titanium Screw (n = 35)
|
|||
|---|---|---|---|---|
| N | % | N | % | |
| Female | 18 | 53 | 24 | 69 |
| Genioplasty | 7 | 21 | 9 | 26 |
| Advancement | ||||
| <5 mm | 10 | 29.4 | 20 | 57.1 |
| 5–10 mm | 24 | 30.6 | 14 | 40 |
| >10 mm | 0 | 0 | 1 | 2.9 |
| Mean | SD | Mean | SD | |
|
|
||||
| Age at surgery | 27.5 | 13.0 | 26.8 | 11.2 |
| Mandibular plane angle | 32.0 | 6.3 | 32.0 | 8.4 |
| Advancement at B Point | 5.4 | 2.6 | 5.0 | 2.6 |
Turvey et al. Stability of Mandibular Advancement With Biodegradables. J Oral Maxillofac Surg 2006.
Group B consisted of the first 34 patients who underwent mandibular advancement via sagittal osteotomies and were stabilized with 2-mm bicortical, self-reinforced bone screws placed transorally in a positional fashion. The patients had completed records including immediate presurgery, immediate postsurgery, at splint removal (between 3 and 5 weeks postsurgery) and at least 1-year follow-up. These surgeries were performed between 1999 and 2002. Group T, a nonconcurrent control group, consisted of patients selected from the database who were stabilized with 2-mm titanium screws also placed positionally and had complete records and similar mandibular movements to those in group B.
As in our previous studies, the cephalometric radiographs were digitized using a 140-point model, and cephalometric changes were evaluated relative to a coordinate system with the x axis rotated 6 degrees downward from sella-nasion. The technique and method error have been reported previously.13 Treatment was considered clinically successful if the patient was satisfied with treatment 1 year postsurgery and demonstrated a Class I occlusion, no more than 4-mm overjet, closed bite, and improved facial aesthetics.
Each of the cephalometric measures (Tables 2-5) was analyzed using a repeated-measures analysis of variance with fixation group as the between-subject factor and time as the within-subject factor. The time-by-fixation group interaction was included in all analyses. Because of the number of measures analyzed, level of significance was set at .01.
Table 2.
BIODEGRADABLE FIXATION GROUP (GROUP B): DESCRIPTIVE STATISTICS FOR HORIZONTAL MOVEMENT
| Surgical Change (n = 34)
|
Fixation Change (n = 30)
|
Net Change to 1 Year (n = 34)
|
||||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |
| ANS | 0.24 | 0.75 | 0.08 | 0.66 | −0.20 | 1.77 |
| PNS | 0.13 | 0.47 | 0.07 | 0.59 | 0.64 | 2.24 |
| B | 5.20 | 2.37 | 0.29 | 1.80 | 0.54 | 3.25 |
| Pg | 6.19 | 3.40 | −0.22 | 1.91 | 0.26 | 3.68 |
| Go | 1.81 | 2.37 | 0.69 | 2.10 | 1.88 | 4.34 |
| Me | 6.27 | 3.79 | −0.25 | 2.09 | 0.34 | 4.04 |
| Co | 0.18 | 1.81 | −0.86 | 1.87 | −1.06 | 2.37 |
| XI | 0.07 | 1.00 | 0.40 | 0.99 | 0.21 | 2.74 |
| MI | 5.20 | 2.79 | 0.59 | 1.39 | 0.47 | 2.75 |
| XM | 1.02 | 2.68 | −0.04 | 1.61 | 0.20 | 2.73 |
| MM | 5.44 | 2.62 | 0.67 | 1.86 | 0.11 | 2.40 |
NOTE. Minus sign indicates posterior movement.
Turvey et al. Stability of Mandibular Advancement With Biodegradables. J Oral Maxillofac Surg 2006.
Table 5.
TITANIUM FIXATION GROUP (GROUP T): DESCRIPTIVE STATISTICS FOR VERTICAL MOVEMENT
| Surgical Change (n = 35)
|
Fixation Change (n = 22)
|
Net Change to 1 Year (n = 35)
|
||||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |
| ANS | −0.15 | 0.60 | 0.18 | 0.70 | 0.09 | 0.80 |
| PNS | −0.06 | 0.40 | 0.00 | 0.40 | 0.00 | 0.40 |
| B | 4.01 | 2.30 | −0.93 | 1.70 | −1.37 | 1.80 |
| Pg | 3.17 | 2.70 | −0.36 | 1.70 | −1.15 | 2.10 |
| Go | 0.94 | 2.30 | −1.44 | 2.00 | −4.16 | 3.10 |
| Me | 4.10 | 1.80 | −0.65 | 1.20 | −1.55 | 1.60 |
| Co | 0.04 | 1.50 | −0.75 | 1.60 | –0.063 | 1.60 |
| XI | 0.26 | 0.70 | −0.028 | 0.80 | −0.02 | 1.20 |
| MI | 3.38 | 2.30 | −0.80 | 1.30 | −2.13 | 1.80 |
| XM | 0.90 | 0.90 | −0.43 | 0.90 | −0.39 | 1.00 |
| MM | 3.56 | 1.50 | −1.32 | 1.30 | −2.52 | 1.60 |
NOTE. Minus sign indicates superior movement.
Turvey et al. Stability of Mandibular Advancement With Biodegradables. J Oral Maxillofac Surg 2006.
Results
There were no clinical failures in group T and a single failure in group B. The failure occurred because the patient had greater than 4-mm overjet at the 1-year postoperative time interval and because of lack of compliance he did not complete orthodontics.
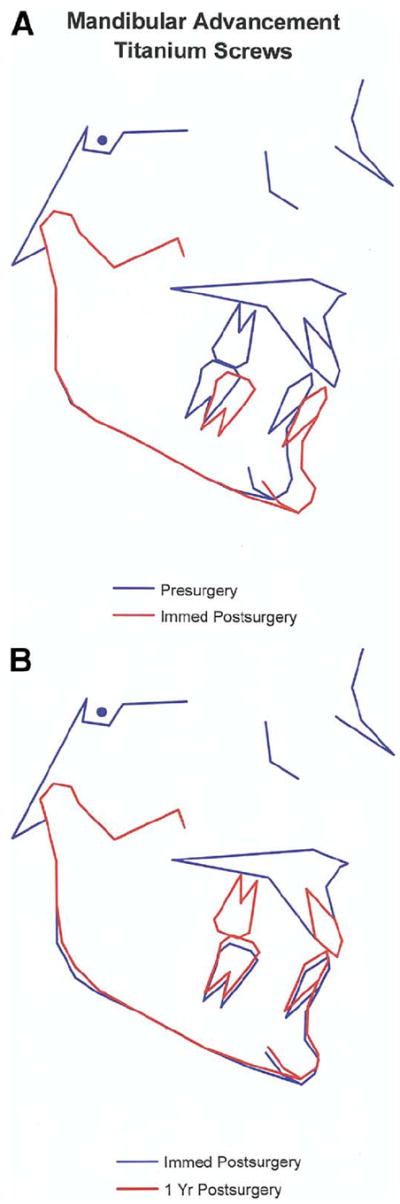
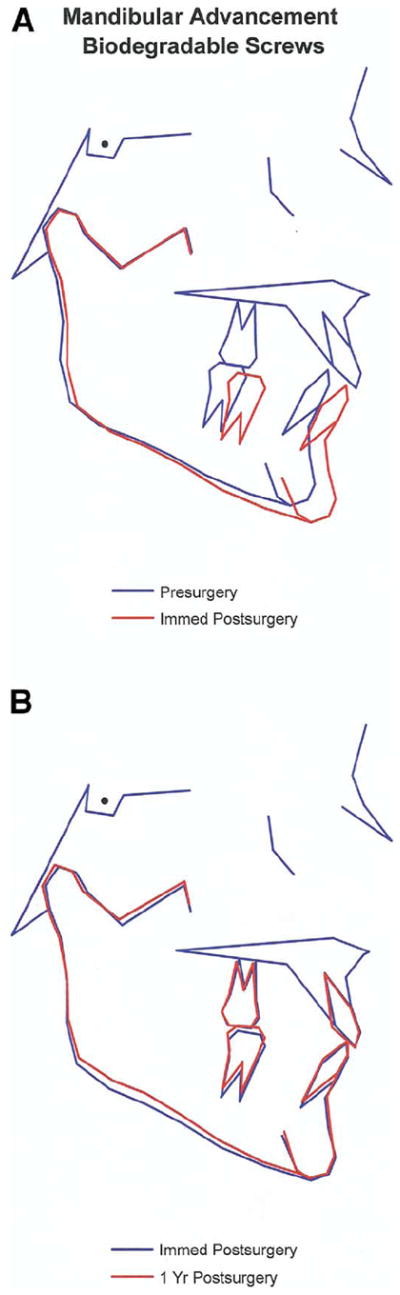
The average change for the 2 groups from immediate postsurgery to 1 year is illustrated in the cephalometric composite superimpositions of Figures 1A and B and 2A and B. The superimpositions make it apparent that the average difference in stability between the biodegradable and titanium fixation groups was quite small. Note that on the average, from postsurgery to 1-year the mandibular position changed only slightly in both groups. There was slightly more upward movement of gonion in the patients with titaniuim screws and slightly more downward movement of pogonion in the patients with biodegradable screws.
FIGURE 1.
A, Composite superimposition from preoperative to postoperative for group B. Notice the similarity with Figure 2A. B, Composite superimposition from immediate post surgery to 1-year post surgery for group B. Notice the subtle difference, especially at the mandibular angle, when compared to Figure 2B.
Turvey et al. Stability of Mandibular Advancement With Biodegradables. J Oral Maxillofac Surg 2006.
FIGURE 2.
A, Composite superimposition from preoperative to postoperative for group T. B, Composite superimposition from immediate post surgery to 1-year post surgery for group T.
Turvey et al. Stability of Mandibular Advancement With Biodegradables. J Oral Maxillofac Surg 2006.
Descriptive statistics for horizontal and vertical changes of landmark positions relative to the coordinate system are presented for the 2 groups in Tables 2 to 5 (x coordinate, horizontal and y coordinate, vertical respectively). These data document the similarity of postsurgical changes in the 2 groups. In the horizontal plane, only gonion and condylion showed average changes larger than a fraction of a millimeter. In the vertical plane, several landmarks showed average vertical changes in the 1- to 2-mm range, with the greatest difference between the titanium and biodegradable groups in the vertical position of gonion (P < .001) and the mandibular plane angle (P < .01). Both can be attributed to somewhat greater upward remodeling at gonion in the patients with titanium screws.
The x and y coordinates of B point, pogonion, menton, mandibular incisor, and mandibular molar showed statistically significant (P < .001) changes over time, as did the x coordinate of condylion and the y coordinate of the maxillary molar, but for all of these measures, the average postsurgical changes were not statistically different for the 2 types of fixation. This same pattern was reflected in analysis of the descriptive statistics for linear and angular measures, which documented significant (P < .001) changes over time in SNB, gonial angle, ramus height (Ar-Go), inclination of the lower incisor to the mandibular plane, and overbite, none of which were different between the 2 groups. The only significant difference in the 2 groups was the change in the mandibular plane angle, which was greater in the titanium group, again reflecting greater remodeling at gonion.
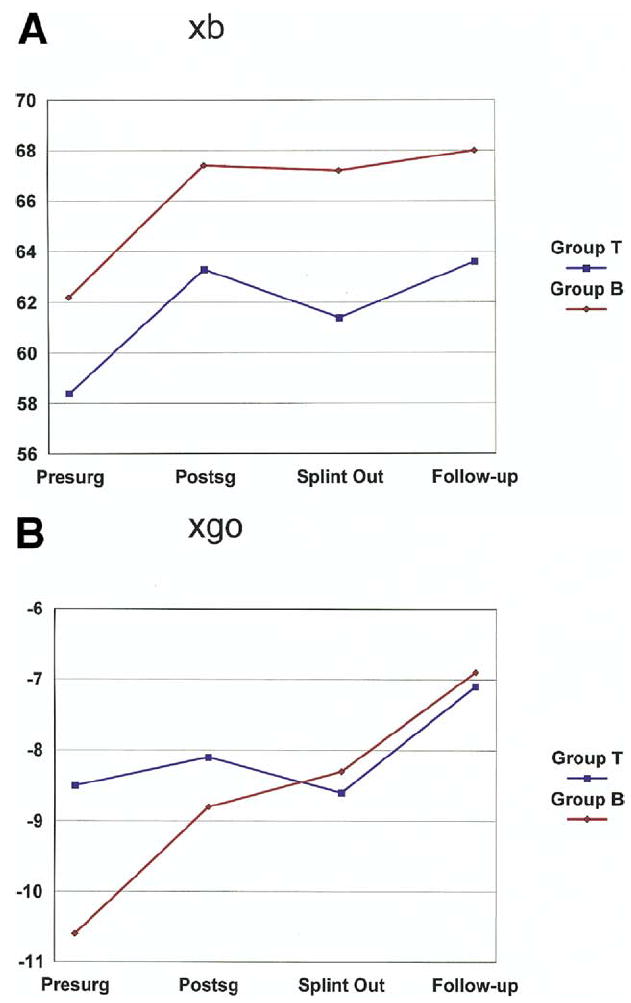
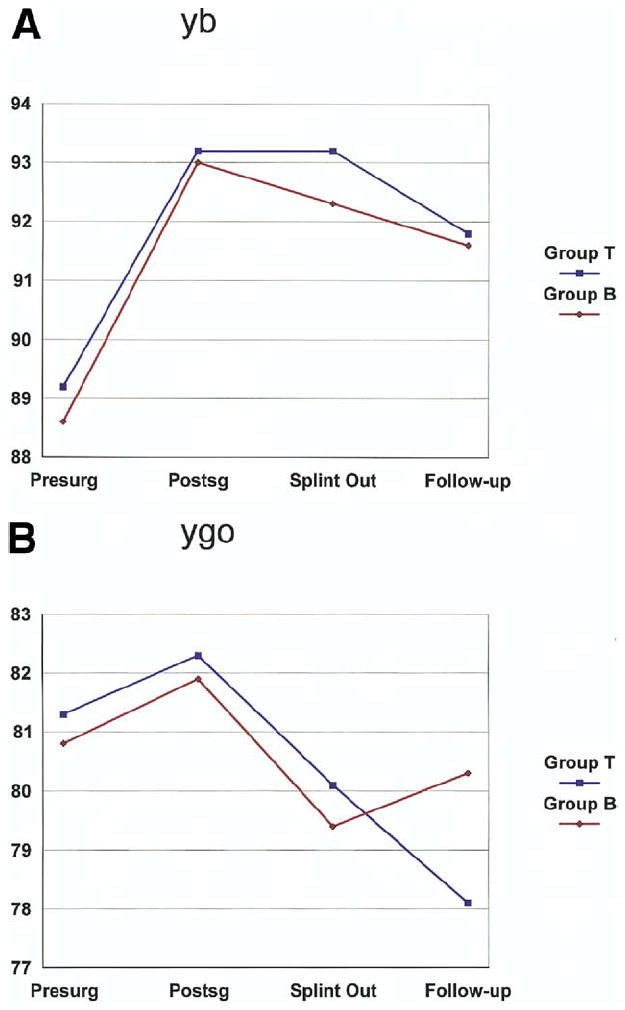
The pattern of change at selected landmarks is shown graphically in Figures 3A and B and 4A and B. In the graphs, if the lines for the 2 groups cross or diverge, the groups are changing in different ways. Note that changes in the chin position for the 2 groups (Figs 3A and 3B) were quite similar, as indicated by the parallelism of the lines. In contrast, there were differences for both the x and y coordinates of gonion. Figure 4A shows the greater vertical change at gonion after the splint removal in the patients with titanium screws, which led to a greater total change compared to the biodegradable patients. In Figure 4B, note the greater early change in the horizontal positon of gonion in the patients with biodegradable screws, but the 2 groups ended in the same place for total horizontal change.
FIGURE 3.
A, Graph illustrating x coordinate change for B point over time for both group B and group T. Notice the parallelism of the lines indicating similar patterns of change. B, Graph illustrating y coordinate changes for B point. Notice the parallelism of the lines suggesting similar patterns between the groups.
Turvey et al. Stability of Mandibular Advancement With Biodegradables. J Oral Maxillofac Surg 2006.
FIGURE 4.
A, Graph illustrating x coordinate changes for Go. Notice the lines crossing indicating a difference between the groups with group B experiencing greater anterior movement of the landmark. B, Graph illustrating coordinate changes for Go. Notice the lines crossing indicating a difference between the groups with group T experiencing more superior rotation of the landmark. These subtle radiographic differences were of no clinical significance.
Turvey et al. Stability of Mandibular Advancement With Biodegradables. J Oral Maxillofac Surg 2006.
Discussion
Patient acceptance of the biodegradable screws is favorable, in the context of their willingness to approve use of this type of fixation. In more than 400 patients treated, only 8 have refused biodegradable fixation and insisted on metal screws instead.17 Kallella et al carefully reviewed the prevalence of complications in their first patients who had fixation with polylactate screws formed with only the l-isomer.11 Although we did not review complications as thoroughly as did Kallella et al, there was no indication of a difference in pain or temporomandibular joint responses between our 2 groups, and as with the PLLL screws used in Finland, there were no problems with an inflammatory response to the self-reinforced 2-mm biodegradable PLLDL (70/30) screws.
The self-reinforced PLLDL (70/30) screws used in this study were withdrawn from North America marketing in May 2002. The product remains distributed in other countries, and its nonavailability in the US market is said to be a business decision not related to safety or manufacturing issues. Currently the principal author uses screws of another copolymer that are manufactured by injection or heat molding rather than extrusion. The screws from this manufacturer have been increased from 2.0 to 2.8 mm to achieve adequate strength. Preliminary clinical outcomes for mandibular advancement surgery using these screws appears to be similar.
We conclude that 2-mm self-reinforced polylactate screws can be used to stabilize BSSO mandibular advancement without compromising the outcomes, which are quite comparable to stabilization with titanium screws. In this study, none of the patients with biodegradable screws required removal of the fixation hardware. It is likely that this will be the case with other modern biodegradable screws, but as material and molding techniques continue to change, it will be important to carefully follow the patients postsurgically to be sure that clinically significant problems have not been inadvertently introduced.
These data indicate that self-reinforced polylactate (formed by extrusion) 2-mm PLLDL 70/30 screws can be used to stabilize BSSO of the mandible for advancement with outcomes that are quite similar to those from stabilization with titanium screws. Although there were subtle differences between the groups at 1 year postsurgery, these were of no clinical consequence.
Table 3.
BIODEGRADABLE FIXATION GROUP (GROUP B): DESCRIPTIVE STATISTICS FOR VERTICAL MOVEMENT
| Surgical Change (n = 34)
|
Fixation Change (n = 30)
|
Net Change to 1 Year (n = 34)
|
||||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |
| ANS | −0.06 | 0.89 | 0.08 | 0.56 | −0.13 | 1.15 |
| PNS | 0.06 | 0.65 | 0.07 | 0.53 | −0.03 | 0.50 |
| B | 4.34 | 1.68 | −0.76 | 1.37 | −1.41 | 2.58 |
| Pg | 4.54 | 1.47 | −0.83 | 1.30 | −1.36 | 2.59 |
| Go | 1.11 | 2.52 | −1.70 | 2.36 | −1.57 | 2.41 |
| Me | 4.84 | 2.24 | −0.80 | 1.18 | −1.56 | 2.24 |
| Co | 0.59 | 1.30 | −0.20 | 1.26 | 0.24 | 2.50 |
| XI | 0.23 | 0.96 | 0.09 | 0.80 | −0.24 | 1.68 |
| MI | 4.61 | 2.12 | −1.05 | 1.39 | −1.73 | 2.08 |
| XM | 0.91 | 1.67 | 0.41 | 1.20 | −0.31 | 1.40 |
| MM | 3.67 | 1.71 | −1.02 | 1.41 | −2.17 | 1.99 |
NOTE. Minus sign indicates superior movement.
Turvey et al. Stability of Mandibular Advancement With Biodegradables. J Oral Maxillofac Surg 2006.
Table 4.
TITANIUM FIXATION GROUP (GROUP T): DESCRIPTIVE STATISTICS FOR HORIZONTAL MOVEMENT
| Surgical Change (n = 35)
|
Fixation Change (n = 22)
|
Net Change to 1 Year (n = 35)
|
||||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |
| ANS | −0.12 | 0.70 | −0.04 | 0.50 | 0.09 | 0.70 |
| PNS | −0.15 | 0.90 | 0.00 | 0.60 | 0.05 | 0.70 |
| B | 4.96 | 2.60 | 0.81 | 1.50 | 0.33 | 2.20 |
| Pg | 6.89 | 4.40 | 0.39 | 1.40 | 0.14 | 2.10 |
| Go | 0.35 | 3.20 | 1.00 | 2.30 | 1.04 | 2.90 |
| Me | 6.94 | 4.60 | 0.55 | 1.70 | 0.06 | 2.50 |
| Co | 0.15 | 1.50 | −0.21 | 1.40 | −0.38 | 1.70 |
| XI | −0.15 | 0.70 | 0.27 | 0.80 | 0.28 | 1.30 |
| MI | 4.32 | 2.10 | 0.68 | 1.10 | 0.10 | 1.40 |
| XM | 0.07 | 1.80 | 0.13 | 0.90 | −0.35 | 1.50 |
| MM | 4.44 | 2.90 | 0.80 | 1.40 | 0.58 | 1.90 |
NOTE. Minus sign indicates posterior movement.
Turvey et al. Stability of Mandibular Advancement With Biodegradables. J Oral Maxillofac Surg 2006.
Acknowledgments
The authors thank Debora Price for her careful digitization of the cephalometric radiographs and preparation of the descriptive statistics. This project was supported in part by NIH R01 DE005215.
References
- 1.Rokkanen PU. Biodegradable fixation devices in orthopedics and traumatology. Am Chir Gynaecol. 1998;87:13. [PubMed] [Google Scholar]
- 2.Imola MJ, Hamlar DD, Shao W, et al. Resorbable plate fixation in pediatric craniofacial surgery: Long term outcome. Arch Fac Plast Surg. 2001;3:79. doi: 10.1001/archfaci.3.2.79. [DOI] [PubMed] [Google Scholar]
- 3.McManners J, Moos KF, El-Attar A. The use of biodegradable fixation in sagittal split and vertical subsigmoid osteotomy of the mandible: A preliminary report. Br J Oral Maxillofac Surg. 1997;35:401. doi: 10.1016/s0266-4356(97)90716-6. [DOI] [PubMed] [Google Scholar]
- 4.Turvey TA, Bell RB, Tejera TJ, et al. The use of self-reinforced biodegradable bone plates and screws in orthognathic surgery. J Oral Maxillofac Surg. 2002;60:59. doi: 10.1053/joms.2002.28274. [DOI] [PubMed] [Google Scholar]
- 5.Weber FE, Eyrich G, Gratz KW, et al. Slow and continuous application of human recombined bone morphogenetic protein via biodegradable polylactate foam spheres. Int J Oral Maxillofac Surg. 2002;31:60. doi: 10.1054/ijom.2001.0154. [DOI] [PubMed] [Google Scholar]
- 6.Kallella I, Laine P, Suuronen R, et al. Osteotomy site healing following mandibular sagittal split osteotomy and rigid fixation with polylactide biodegradable screws. Int J Oral Maxillofac Surg. 1999;28:166. [PubMed] [Google Scholar]
- 7.Suuronen R, Pohjonan T, Hietanen J, et al. A 5-year old in vitro and in vivo study of the biodegradation of polylactide plates. J Oral Maxillofac Surg. 1998;56:604. doi: 10.1016/s0278-2391(98)90461-x. [DOI] [PubMed] [Google Scholar]
- 8.Acero J, Calderon J, et al. The behavior of titanium as a biomaterial: Microscopy study of plates and surrounding tissues in facial osteosynthesis. J Craniomaxillofac Surg. 1999;27:117. doi: 10.1016/s1010-5182(99)80025-0. [DOI] [PubMed] [Google Scholar]
- 9.Meningaud JP, Poupon J, Bertrand J, et al. Dynamic study about metal release from titanium implants in maxillofacial surgery. Int J Oral Maxillofac Surg. 2001;30:185. doi: 10.1054/ijom.2000.0039. [DOI] [PubMed] [Google Scholar]
- 10.Schmidt BL, Perrott DH, Mahan D, et al. The removal of plates and screws after LeFort I osteotomy. J Oral Maxillofac Surg. 1998;56:184. doi: 10.1016/s0278-2391(98)90865-5. [DOI] [PubMed] [Google Scholar]
- 11.Kallela I, Laine P, Suuronen R, et al. Assessment of material- and technique-related complications following sagittal split osteotomies stabilized by biodegradable polylactide screws. Oral Surg Med Oral Pathol Oral Radiol Endod. 2005;99:4. doi: 10.1016/j.tripleo.2004.04.017. [DOI] [PubMed] [Google Scholar]
- 12.Proffit WR, Phillips C. Physiological responses to treatment and postsurgical stability. In: Proffit WR, White RP Jr, Sarver DM, editors. Contemporary Treatment of Dentofacial Deformity. St Louis, MO: Mosby; 2003. [Google Scholar]
- 13.Watzke IM, Turvey TA, Phillips C, et al. Stability of mandibular advancement after sagittal osteotomy with screw or wire fixation: A comparative study. J Oral Maxillofac Surg. 1990;48:108. doi: 10.1016/s0278-2391(10)80197-1. [DOI] [PubMed] [Google Scholar]
- 14.Landes CA, Kreiner S. Resorbable plate osteosynthesis of sagittal split osteotomies with major bone movement. Plast Reconstr Surg. 2003;111:1828. doi: 10.1097/01.PRS.0000056867.28731.0E. [DOI] [PubMed] [Google Scholar]
- 15.Ferreti C, Reyneke JP. Mandibular sagittal split osteotomies fixed with biodegradable or titanium screws: A prospective, comparative study of postoperative stability. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93:543. doi: 10.1067/moe.2002.124091. [DOI] [PubMed] [Google Scholar]
- 16.Turvey TA, Hall DJ. Intraoral self-threading screw fixation for sagittal osteotomies. Early experience. Int J Adult Orthod Orthognath Surg. 1986;4:243. [PubMed] [Google Scholar]
- 17.Turvey TA. The use of biodegradable polylactide plates and screws to stabilize maxillary and mandibular osteotomies. J Craniomaxillofac Surg. 2000;28(suppl 3):151. [Google Scholar]


