Abstract
Aims:
Since its description in 1980, percutaneous endoscopic gastrostomy has become the modality of choice for providing enteral access to patients who require long-term enteral nutrition. This study aimed to evaluate current indications and complications associated with PEG feeding.
Methods:
We conducted a retrospective analysis of all patients who referred to our endoscopic unit of the Department of Gastroenterology and Hepatology of the Medical Center University of Sarajevo for PEG tube placement over a period of 7 years. Medical records of 359 patients dealing with PEG tube placement were reviewed to assess indications, technical success, complications and the need for repeat procedures.
Results:
The indications for enteral feeding tube placement were malignancy in 44% (n=158), of which 61% (n=97) patients were suffering of head and neck cancer and 39% (n=61) of other malignancy. Central nervous disease was the indication in 48.7 % (n=175) of patients. Cerebrovascular accidents (CVA) accounted for 20% (n=73), head injury for 16% (n=59) and cerebral palsy for 11% (n=38). In 6.13% (n=22) of patients minor complications occur which included wound infection (0.8%), inadvertent PEG removal (2.5%) and tube blockage (1.1%). 11 patients experienced major complications including hemorrhage, tube migration and perforation. There were no deaths related to PEG procedure placement and the overall 30-day mortality rate due to primary disease was 15.8%. Oral feeding was resumed in 23% of the patients and the tube was removed subsequently after 6 -12 months.
Conclusions:
Percutaneous endoscopic gastrostomy is a save and minimally invasive endoscopic procedure associated with a low morbidity (9.2%) rate, easy to follow-up and to replace when blockage occurs. Over a seven-year period we noticed an increase of 63% in PEG placement at our department.
Key words: PEG, enteral nutrition, tube feeding.
1. INTRODUCTION
Since its introduction in the early 1980s (1]) percutaneous endoscopic gastrostomy (PEG) has become the modality of choice for providing longterm enteral nutrition in patients with inadequate oral intake. It has now replaced surgical gastrostomy, which was associated with a markedly higher rate of complications (2). Several studies have clearly shown the advantages of PEG tube over nasogastric tube feeding in medium- and long-term enteral feeding. Feeding via nasogastric tubes was found to have higher rate of complications and discomfort as well as a lower nutritional efficacy when compared with nutrition via PEG tubes. PEG-feeding, therefore, has rapidly spread and over the last three decades expanded the range of indications (3, 4).
This study aimed to review and evaluate indications and complications associated with PEG tube placement in a single, tertiary care University Hospital over a seven-year period.
2. MATERIALS AND METHODS
We conducted a retrospective review of PEG tube placement in our institution, the Medical Center University of Sarajevo, performed between January 2005 and October 2012. Corresponding patient medical records were reviewed to assess primary diagnosis and complications occurring during PEG tube placement as well as complications associated with PEG use. The patient charts included patient demographics, follow-up information and outcome. Additional follow-up information was also obtained by direct telephone contact with the referring doctor, family or nursing personnel.
The PEG placement was performed using the pull technique described by Ponsky and Gauderer (1). No routine antibiotic prophylaxis before PEG placement was used.
3. RESULTS
Between January 2005 and October 2012 a total of 366 PEG procedures were performed of which 359 tubes were successfully inserted. In 7 patients PEG insertion failed due to anatomical anomaly or malignant GI obstruction, these patients were excluded from the study. 48 patients were children, in the age between 3 months and 14 years, mean age 5.7 years with 67% being male. The mean age of the adult patient cohort (n=311) was 65.7 years (range 19 to 84 years) with 63% being female. The number of PEG tube placements annually has increased from 37 in 2005 to 63 in 2011, which was accompanied by the annual increase of overall endoscopic procedures performed in our unit.
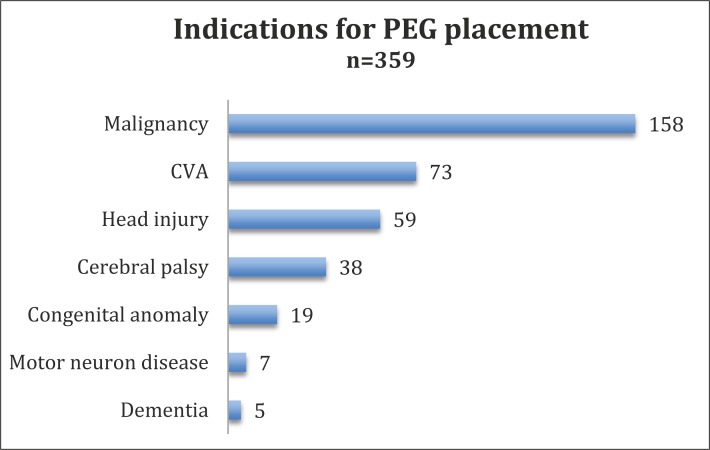
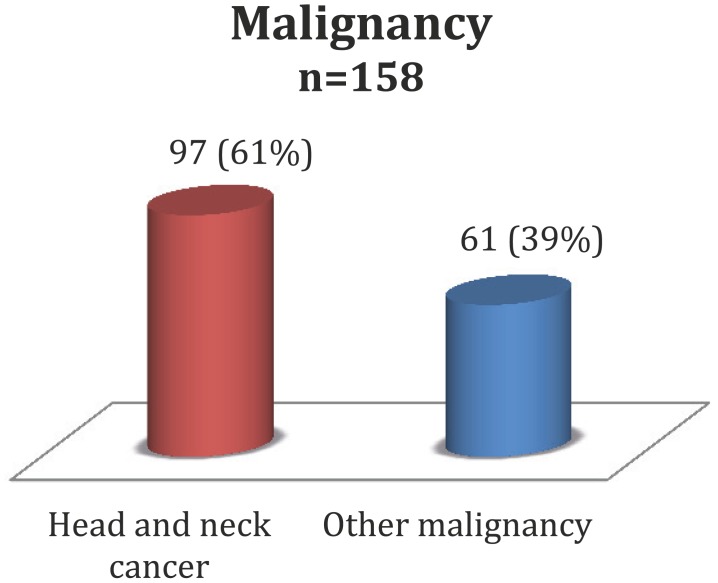
The indications for PEG tube placement were malignancy in 44% (n=158), of which 61% (n=97) patients were suffering from head and neck cancer and 39% (n=61) of other malignancy. Central nervous disease was the indication in 48.7 % (n=175) of patients. Cerebrovascular accidents (CVA) accounted for 20% (n=73), head injury for 16% (n=59) and cerebral palsy for 11% (n=38). 19 patients (5%) suff ered from a congenital anomaly, 7 (2%) from a motor neuron disease and 5 (1%) from dementia. (Figure 1 and 2).
Figure 1.
Indications for PEG placement.
Figure 2.
Malignancy as indication for PEG placement.
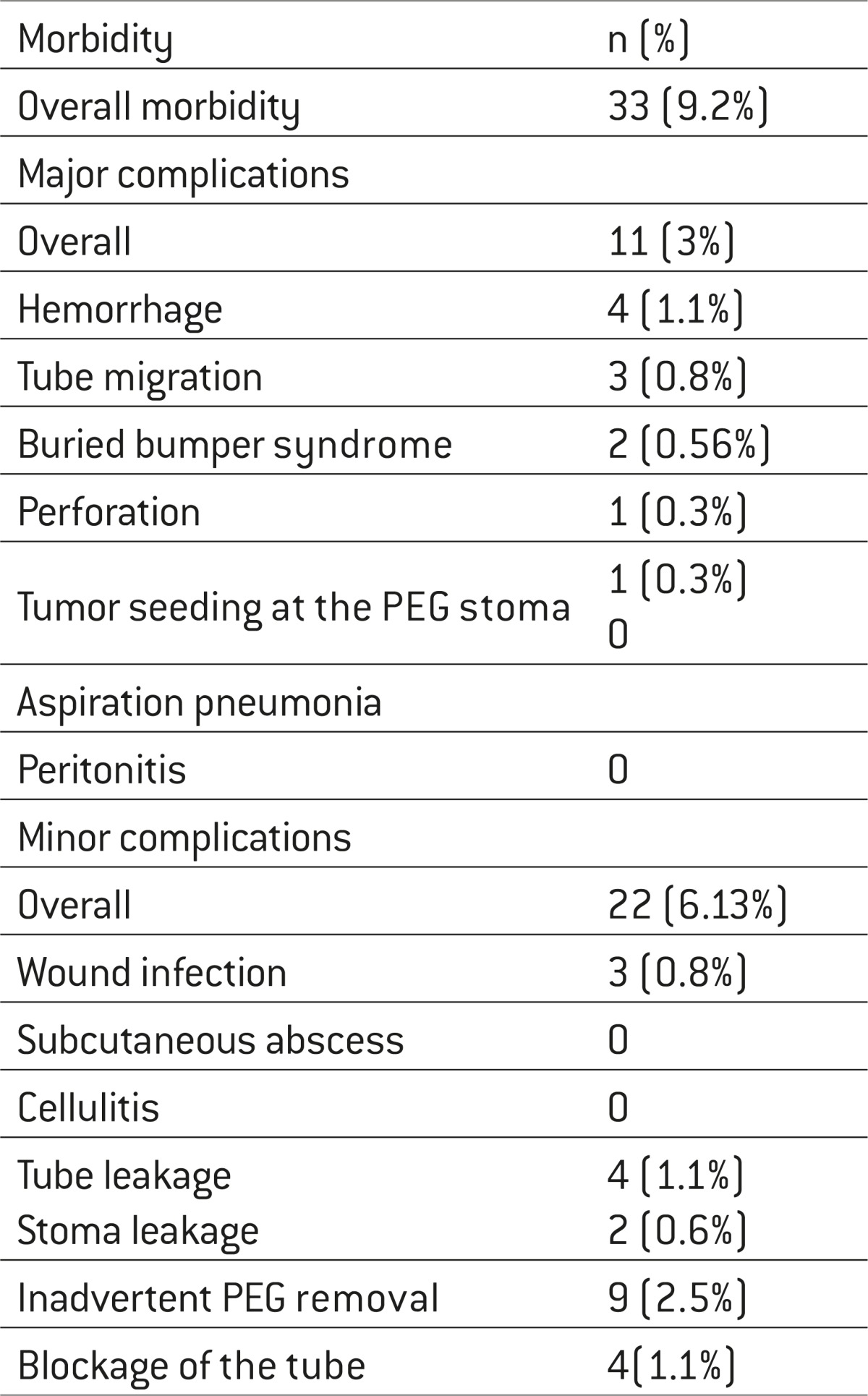
In 6.13% (n=22) of patients minor complications occurred after PEG tube insertion, which included wound infection (n=3, 0.8%), tube leakage (n=4, 1.10%), stoma leakage (n=2, 0.56%), inadvertent PEG removal (n=9, 2.5%) and tube blockage (n=4, 1.1%). 11 patients (3%) experienced major complications including hemorrhage (n=4, 1.1%), tube migration (n=3, 0.8%) and buried bumper syndrome (n=2, 0.56%). In one patient during PEG placement duodenal perforation occurred, which was resolved by endoscopic clipping. There was one case of tumor seeding at the PEG stoma in a patient with pharyngeal adeno-carcinoma. No patient developed neither peritonitis nor aspiration pneumonia after PEG placement. There were no deaths related to PEG procedure placement. 57 (15.8%) patients died within 30 days due to primary disease. Oral feeding was resumed in 23% of the patients and the tube was removed subsequently after 6 -14 months (Table 1).
Table 1.
Morbodity associated with PEG placement
 |
4. DISCUSSION
Although success rates greater than 95% have been reported for PEG, procedure-related complications are common. Complications related to PEG placement and feeding are traditionally stratified as major and minor. In our retrospective analysis we noticed a success rate of 98% PEG tube placement, an overall complication rate of 9.2% and no procedure-related deaths. Th ese results are in line with a large meta-analysis, which reported a procedure-related morbidity of 9.4% and mortality of 0.53% (5, 6).
In our analysis 22 patients experienced minor complications including 3 wound infections and no case of subcutaneous abscess or cellulitis. The wound infection rate in the literature ranges from 5-25% (7, 8, 9). Antibiotic prophylaxis reduces the infection rate to about 3 % (10, 11). Currently, there is still a controversial debate in the literature as to whether a single administration of an antibiotic, as a general prophylaxis, provides eff ective protection against peristomal infection. The European Society of Parenteral and Enteral Nutrition recommend that, in experienced hands under established hygienic conditions, routine antibiotic prophylaxis is not mandatory for PEG placement (12). Our results confirm this recommendation as we noticed a very low infection rate of 0.8%, although our patients did not routinely receive periprocedural antibiotics. Only fi ve patients received a single dose of an antibiotic (2g of cephazolin i.v.) prior PEG insertion, all of them were highly immunocompromised.
We therefore concluded that technique-related factors, as small abdominal wall incision and low traction on the PEG tube, have a great impact on PEG site infections. Nevertheless, in immunocompromised patients (patient with diabetes mellitus, patients on immunomodulatory and corticosteroid medication) we highly recommend the use of a single dose of an antibiotic as general prophylaxis.
Blockage of the tube is a common problem seen in patients with longterm enteral nutrition via PEG. 16-31% of PEG tubes had at least 1 episode of significant blockage during 18 months of follow-up, of which 7% required removal (13). In our review only 4 (1.1%) patients showed an irreversible tube blockage that required tube exchange. We advise frequent water flushes (before and after feeding), administering liquid medication or well- ground pills to avoid feeding-tube blockage.
In our series we noticed two cases of buried bumper syndrome (BBS), which is an uncommon but serious complication of PEG, occurring in 1.5-1.9% of patients (14). A variety of techniques have been used to manage the BBS (15, 16). In our unit both cases were managed endoscopically, without further complications. We concluded the endoscopic approach of the BBS as a minimal invasive and safe method.
Indication in 44% of our patient group was malignant disease, the majority of them (61%) suffering from head and neck cancer. It has been clearly shown that PEG-feeding is effective in reducing weight loss, malnutrition and hospitalization in this patient group (17). Current practice includes pre-treatment PEG placement in the management of patients undergoing chemoradiation [18]. However, even in those patients who get PEG in a later stage of disease and in those who remain dependent on enteral feeding PEG has been shown to contribute to improved quality of life (19).
The high mortality rate of 15.8% within 30 days after PEG placement is more likely to be related to advanced primary diagnosis and poor general condition than to the procedure itself. Previous studies that involve a heterogeneous population report 30-day mortality rates ranging from 9-31% (20, 21). Factors that predicting successful long-term outcome of PEG tube feeding have not been well studied, but it seems like co-morbidity aff ects patient’s survival. Another study reported an overall mortality rate of 28% in patients after PEG placement, which increased to 54% in the subgroup of patients with dementia (22). In our report just 1% of patients suffered from dementia with no evidence of higher 30-day mortality rate and it seems that PEG placement in this patient group continuous to be a major area of controversy.
5. CONCLUSIONS
Our 7-year clinical experience showed that PEG placement is a save and minimally invasive endoscopic procedure associated with a procedure-related low morbidity (9.2%) rate, easy to follow-up and to replace when blockage occurs. PEG provides durable access for enteral nutrition, prevents malnutrition and reduces hospitalization in cancer patients. Over a seven-year period we noticed an increase of 63% in PEG placement at our department.
Conflict of interest
None declared.
REFERENCES
- 1.Gauderer MW, Ponsky JL, Izant RJ., Jr Gastrostomy without laparotomy: a percutaneous endoscopic technique. J Pediatr Surg. 1980;15:872–875. doi: 10.1016/s0022-3468(80)80296-x. [DOI] [PubMed] [Google Scholar]
- 2.Grant JP. Comparison of percutaneous endoscopic gastrostomy with Stamm gastrostomy. Ann Surg. 1988 May;207(5):598–603. doi: 10.1097/00000658-198805000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Löser C. Clinical aspects of long-term enteral nutrition via percutaneous endoscopic gastrostomy (PEG) J Nutr Health Aging. 2000;4(1):47–50. [PubMed] [Google Scholar]
- 4.McClave SA, Ritchie CS. The role of endoscopically placed feeding or decompression tubes. Gastroenterol Clin North Am. 2006;35:83–100. doi: 10.1016/j.gtc.2005.12.003. [DOI] [PubMed] [Google Scholar]
- 5.Disario J. Endoscopic approaches to enteral nutritional support. Best Pract Res Clin Gastroenterol. 2006;20:605–630. doi: 10.1016/j.bpg.2006.02.002. [DOI] [PubMed] [Google Scholar]
- 6.Lin HS, Ibrahim HZ, Kheng JW, et al. Percutaneous endoscopic gastrostomy: strategies for prevention and management of complications. Laryngoscope. 2001;111:1874–1852. doi: 10.1097/00005537-200110000-00033. [DOI] [PubMed] [Google Scholar]
- 7.Lee JH, Kim JJ, Kim YH, et al. Increased risk of peristomal wound infections after percutaneous endoscopic gastrostomy in patients with diabetes mellitus. Dig Liver Dis. 2002;34:857–861. doi: 10.1016/s1590-8658(02)80256-0. [DOI] [PubMed] [Google Scholar]
- 8.Gencosmanoglu R, Koc D, Tozun N. Percutaneous endoscopic gastrostomy: results of 115 cases. Hepatogastroenterology. 2003;50:886–888. [PubMed] [Google Scholar]
- 9.McClave SA, Chang WK. Complications of enteral access. Gastrointest Endosc. 2003;58:739–751. doi: 10.1016/s0016-5107(03)02147-3. [DOI] [PubMed] [Google Scholar]
- 10.Dormann AJ, Wigginghaus B, Risius H, et al. Antibiotic prophylaxis in percutaneous endoscopic gastrostomy (PEG) - results from a prospective randomized multicenter trial. Z Gastroenterol. 2000;38:229–234. doi: 10.1055/s-2000-14862. [DOI] [PubMed] [Google Scholar]
- 11.Jafri NS, Mahid SS, Minor KS, Idstein SR, Hornung CA, Galandiuk S. Meta-analysis: antibiotic prophylaxis to prevent peristomal infection following percutaneous endoscopic gastrostomy. Aliment Pharmacol Ther. 2007;25:647–656. doi: 10.1111/j.1365-2036.2007.03247.x. [DOI] [PubMed] [Google Scholar]
- 12.Löser C, Aschl G, Hébuterne X, Mathus-Vliegen EM, Muscaritoli M, Niv Y, Rollins H, Singer P, Skelly RH. ESPEN guidelines on artifi cial enteral nutrition - percutaneous endoscopic gastrostomy (PEG) Clin Nutr. 2005 Oct;24(5):848–861. doi: 10.1016/j.clnu.2005.06.013. [DOI] [PubMed] [Google Scholar]
- 13.Blacka J, Donoghue J, Sutherland M, et al. Dwell times and functional failure in percutaneous endoscopic gastrostomy tubes: a prospective randomized controlled comparison between silicon polymer and polyurethane percutaneous endoscopic gastrostomy tubes. Aliment Pharmacol Ther. 2004;20:875–882. doi: 10.1111/j.1365-2036.2004.02191.x. [DOI] [PubMed] [Google Scholar]
- 14.Rino Y, Tokunaga M, Morinaga S, et al. The buried bumper syndrome: an early complication of percutaneous endoscopic gastrostomy. Hepatogastroenterology. 2002;49:1183–1184. [PubMed] [Google Scholar]
- 15.Boyd JW, DeLegge MH, Shamburek RD, Kirby DF. The buried bumper syndrome: A new technique for safe endoscopic PEG removal. Gastrointest Endosc. 1995;41:508–511. doi: 10.1016/s0016-5107(05)80013-6. [DOI] [PubMed] [Google Scholar]
- 16.Braden B, Brandstaetter M, Caspary WF, Seifert H. Buried bumper syndrome: treatment guided by catheter probe US. Gastrointest Endosc. 2003;57:747–751. doi: 10.1067/mge.2003.184. [DOI] [PubMed] [Google Scholar]
- 17.Raykher A, Russo L, Schattner M, et al. Enteral nutrition support of head and neck cancer patients. Nutr Clin Pract. 2007;22:68–73. doi: 10.1177/011542650702200168. [DOI] [PubMed] [Google Scholar]
- 18.Raykher A, Schattner M, Friedman A, et al. Safety and effi cacy of pretreatment placement of PEG tubes in head and neck cancer patients undergoing chemoradiation treatment. Clin Nutr. 2004;23:757. [Google Scholar]
- 19.Senft M, Fietkau R, Iro H, et al. The influence of supportive nutritional therapy via percutaneous endoscopic guided gastrostomy on the quality of life of cancer patients. Support Care Cancer. 1993;1:272–275. doi: 10.1007/BF00366049. [DOI] [PubMed] [Google Scholar]
- 20.Light VL, Slezak FA, Porter JA, Gerson LW, McCord G. Predictive factors for early mortality aft er percutaneous endoscopic gastrostomy. Gastrointest Endosc. 1995;42:330–335. doi: 10.1016/s0016-5107(95)70132-x. [DOI] [PubMed] [Google Scholar]
- 21.Dharmarajan TS, Unnikrishnan D, Pitchumoni CS. Percutaneous endoscopic gastrostomy and outcome in dementia. Am J Gastroenterol. 2001;96:2556–2563. doi: 10.1111/j.1572-0241.2001.04099.x. [DOI] [PubMed] [Google Scholar]
- 22.Sanders DS, Carter MJ, D’Silva J, et al. Survival analysis in percutaneous endoscopic gastrostomy feeding: a worse outcome in patients with dementia. Am J Gastroenterol. 2000;95:1472–1475. doi: 10.1111/j.1572-0241.2000.02079.x. [DOI] [PubMed] [Google Scholar]