Abstract
Introduction:
Nowadays an increasing number of lung resections are being done because of the rising prevalence of lung cancer that occurs mainly in patients with limited lung function, what is caused by common etiologic factor - smoking cigarettes. Loss of lung tissue in such patients can worsen much the postoperative pulmonary function. So it is necessary to asses the postoperative pulmonary function especially after maximal resection, i.e. pneumonectomy.
Objective:
To check over the accuracy of preoperative prognosis of postoperative lung function after pneumonectomy using spirometry and lung perfusion scinigraphy.
Material and methods:
The study was done on 17 patients operated at the Clinic for thoracic surgery, who were treated previously at the Clinic for Pulmonary Diseases “Podhrastovi” in the period from 01. 12. 2008. to 01. 06. 2011. Postoperative pulmonary function expressed as ppoFEV1 (predicted postoperative forced expiratory volume in one second) was prognosticated preoperatively using spirometry, i.e.. simple calculation according to the number of the pulmonary segments to be removed and perfusion lung scintigraphy.
Results:
There is no significant deviation of postoperative achieved values of FEV1 from predicted ones obtained by both methods, and there is no significant differences between predicted values (ppoFEV1) obtained by spirometry and perfusion scintigraphy.
Conclusion:
It is necessary to asses the postoperative pulmonary function before lung resection to avoid postoperative respiratory failure and other cardiopulmonary complications. It is absolutely necessary for pneumonectomy, i.e.. maximal pulmonary resection. It can be done with great possibility using spirometry or perfusion lung scintigraphy.
Key words: pneumonectomy, spirometry, perfusion lung scintigraphy.
1. INTRODUCTION
In recent years there has been increase in the number of patients who need thoracic surgery, first of all different types of pulmonary resection for primary bronchial cancer, particularly among patients whose lung function is impaired due to the different degrees of bronchial obstruction. In all these patients it is necessary to assess functional status after lung surgery performed, although in these patients we may ask - what is the risk of postoperative complications in relation to disease that certainly has fatal outcome if not treated surgically?
This problem is differently treated in the literature. Various methods are recommended for evaluation of postoperative lung function. Some authors recommend measuring only FEV1 (forced expiratory volume in one second) (1, 2, 3, 4, 5, 6, 7, 8, 9), and some recommend that in addition to FEV1, in cases where there are diffuse interstitial changes of lung and DLCo (transfer factor for CO) should be determined (2, 3, 4). Other authors consider that there is the need for complete spiropletysmographic processing: (FEV1), vital capacity (VC), forced vital capacity (FVC), flow-volume curve, pulmonary resistance (Rt), residual lung volume (RV), bronchodilator test, maximum voluntary minute ventilation (MMV) and total lung capacity (TLC) (10, 11, 12, 13), but all require to do the analysis of gases in the blood. If there is hypercapnia, i.e. high partial pressure of carbon dioxide in arterial blood (Pa CO2) >45 mm Hg (6 kPa) it does not give the approval for the surgery. If there is hypoxemia i.e. decreased partial pressure of oxygen in arterial blood (PaO 2) <60 mmHg (8 kPa) or arterial oxygen saturation (SaO2) below 90% it does not give the approval for the surgery (1, 3, 10, 14, 15, 16, 17). Many authors require to be done and ventilation–perfusion or a perfusion lung scintigraphy especially for planned pneumonectomy (2, 3, 19, 20, 21, 22).
2. OBJECTIVE
To check over the accuracy of preoperative prognosis of postoperative lung function in pneumonectomy using spirometry and lung perfusion scinigraphy and to compare the results of preoperative prediction obtained by these two methods.
3. MATERIAL AND METHODS
The study was done on 17 patients surgically treated at the Clinic for thoracic surgery, KCU Sarajevo, who were treated previously at the Clinic for Pulmonary Diseases “Podhrastovi” in the period from 01. 12. 2008. to 01. 06. 2011. All of them had some form of bronchial cancer. Left or right pneumonectomy was made.
The control group consisted of the same patients whose predicted values of the parameters of postoperative lung function were compared with the actual values of these parameters after pneumonectomy that is planned in a multidisciplinary meeting (thoracic surgeon, pulmonologist and radiologist).
Lung function tests were done when the patient was clinically stable and after taking the complete bronchodilator treatment, if it was needed.
All patients were undergone to complete spiroplethysmographic processing as follows: FVC, FEV1, flow-volume curve, RT including bronchodilator test, RV and TLC. Arterial blood gas analysis was also performed.
If there was a disturbance in blood gases: hypoxemia i.e. PaO2 below 60 mm Hg (8kPa) or SaO2 below 90%, with or without hypercapnia i.e. PaCO2 above 45 mmHg (6kPa) approval for operation was not given. We tried with bronchodilator therapy and with oxygen therapy, to achieve the normalization gases in blood. If the blood gases normalized patients were given the approval for the surgery.
If there was bronchospasm it also did not give the approval for surgery because bronchospasm is accompanied with vasospasm and a significant increase in pulmonary vascular resistance and that is a big surgical risk. If bronchospasm is relieved by appropriate bronchodilator therapy patients were given the approval for the surgery.
If there was hyperinflation of lung parenchyma in great degree i.e. the RV greater than 300% of normal values, which indicating a distinct bronchial obstruction, we did not give permission for operation. If the appropriate bronchodilator therapy decreased RV to values below 300% of standard values patients were given the approval for the surgery.
The degree of damage of the lung function is primarily determined based on the FEV1 because it is the most objective parameter of lung function which indicates the obstructive and restrictive disorders of lung function and indicates the type and degree of damage of ventilatory lung function.
In all patients on the basis of measured preoperative lung functional parameters, we predicted postoperative lung function.
In all patients the residual pulmonary function was predicted as follows: it is assumed that each segment of the lung, and there are total 19 of them (upper right lobe - 3, right middle lobe - 2, right lower lobe - 5; upper left lobe - 3, lingula - 2, lower left lobe - 4 segments) in the healthy lung contributes equally to ventilation that is 1/19 (nineteenth part) or 5.26% of total lung ventilation (100%).
Predicted postoperative FEV l (ppo FEV l) in absolute values (l-L) is calculated as follows:
Ppo FEV1 = preoperative FEV l × (19 segments–the number of segments to be removed) ÷ 19 or by the formula.
Ppo FEV1 =preoperative FEV1 × (l–(S x 5.26) ÷ 100.
(S = number of segments to be removed).
Both formulas provide the same result. If there was bronchoscopic evidence of stricture or obstruction of segmental bronchi of the parts of lungs in particular which have not been planned for resection then we used the following formula:
ppoFEV1 = preoperative FEV1 × {(19-a)–b} ÷ (19-a), where a = number of obstructed segments, b = number of no obstructed segments to be resected.
Then the predicted postoperative FEV1 was expressed as a percentage (%) of normal values for the patient’s FEV1 (ppoFEV1%) and was calculated by the following formula:
% ppoFEV1 = {ppo FEV1 (in Liters) × 100} ÷ normal FEV1 (L) for this patient.
For normal spirometric parameters are taken “European standards” or CECA norms that are established under the auspices of the European Community for Coal and Steel, which was the forerunner of today’s European union, and taking into account height, weight, age and sex of the patient and which are entered into the computer of every spyropletismographic apparatus.
In 10 patients residual pulmonary functional reserve was calculated, not only by spirometry, but also on the basis of findings of perfusion lung scintigraphy according to the formula:
ppo FEV1 = preoperative FEV1 × (1–fraction of total perfusion of removed lung).
In these 10 patients we compared the ppo FEV1 values obtained by calculation based on the number of segments to be removed and the values obtained from a lung scintigraphy.
Complete spiropletysmographic processing was done on the apparatus MasterLab-Jaeger, and determination of blood gases on the Radiometer ABL 505 apparatus in the Laboratory for Clinical Respiratory Physiology at the Clinic “Podhrastovi” and perfusion lung scintigraphy by gamma camera was done at the Institute of Nuclear Medicine of Clinical center of University of Sarajevo.
Lung function tests were done within 7-10 days before surgery and were performed after the patient took a bronchodilator (if it was needed) and after 2 months after surgery when it is considered that the stabilization of the functional lung status was achieved. If it was done more than one testing, for preoperative calculation was taken the highest value achieved. We compared the predicted and the realized values of postoperative FEV1 and compared predicted values obtained by both methods. Results were statistically analyzed by SPSS and Microsoft Office Excel. Statistical significance was determined at an interval of 95%.
4. RESULTS
Results obtained by spirometric calculation are presented in the four tables.
In 9 males with left pneumonectomy there was no significant differences between predicted and achieved values. Higher values of prognosis were achieved-realized in 6 patients but with no significant differences to predicted ones (Table 1).
Table 1.
The ratio between predicted and realised values of FEV1- left pneumonectomy -males
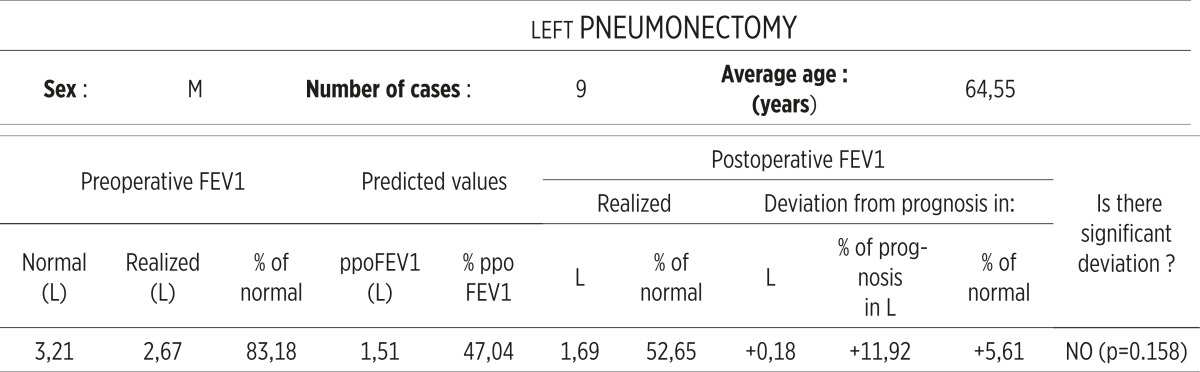 |
Smaller values of prognosis were achieved in 2 patients but with no significant differences to predicted ones. In 2 females with left pneumonectomy there was no significant differences between predicted and achieved values. Higher value of prognosis was achieved in 1 patient but with no significant difference to predicted one. Smaller value of prognosis was achieved in 1 patient but with no significant difference to predicted one. In 5 males with right pneumonectomy there was no significant differences between predicted and achieved values. Higher values of prognosis were achieved in 4 patients but with no significant differences to predicted ones. Smaller value of prognosis was achieved in 1 patient but with no significant differences to predicted one. In 1 female with right pneumonectomy there was no significant differences between predicted and achieved value Smaller value of prognosis was achieved (Table 2, 3).
Table 2.
The ratio between predicted and realised values of FEV1 - left pneumonectomy -females
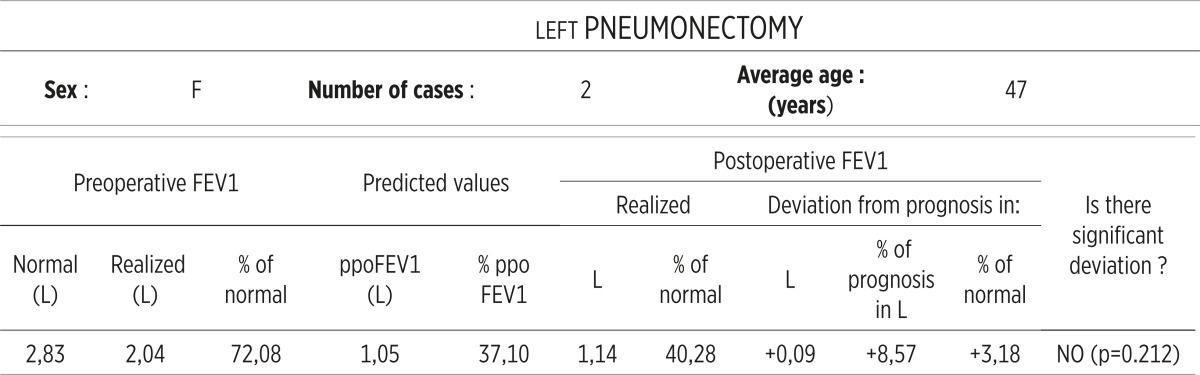 |
Table 3.
The ratio between predicted and realised values of FEV1 -right pneumonectomy -males
 |
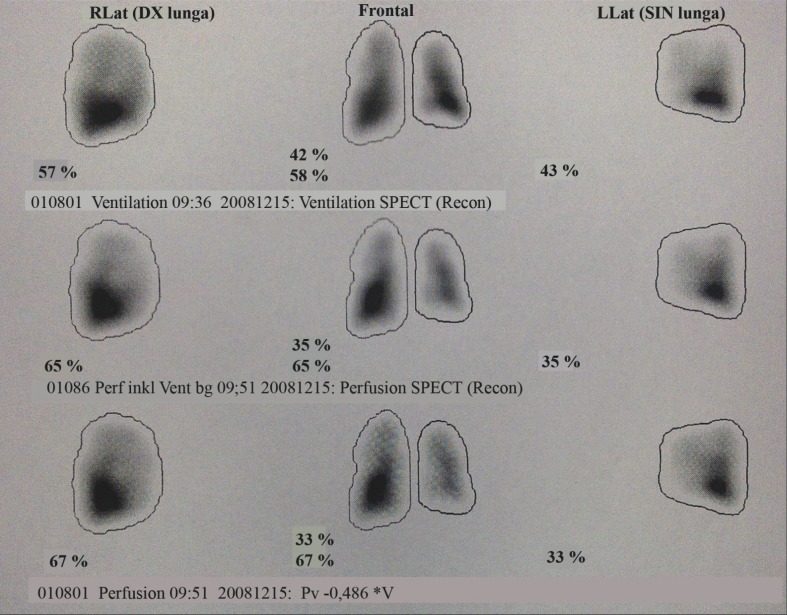
In 10 patients residual pulmonary functional reserve i.e. postoperative FEV1 was prognosticated not only by spirometry but also by perfusion lung scintigraphy. On the Figure 1. there is the presentation of perfusion scintigraphy done in one of them. In all of patients we performed ventilation/perfusion scintigraphy but only the results of perfusion scintigraphy we took into consideration. There were no statistically significant differences between the % ppo FEV1 obtained by spirometry and lung perfusion scintigraphy (p> 0.05).
Figure 1.
Example of Ventilation /perfusion scintigrapfy done in one patient.
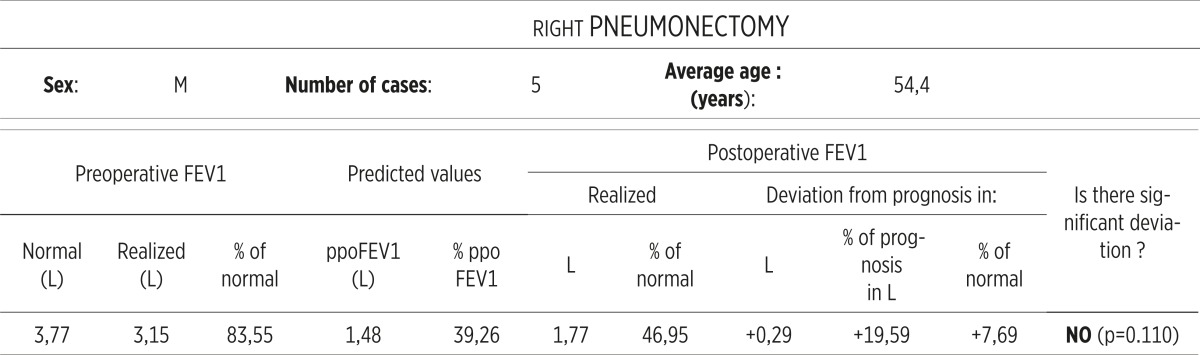
The maximum deviation was in one patient with left pneumonectomy where the %ppoFEV1 calculated by scintigraphy was for 11% higher than the value calculated by spirometry (Table 4).
Table 4.
The ratio between prediceted and realised values of FEV1 - right pneumonectomy-females
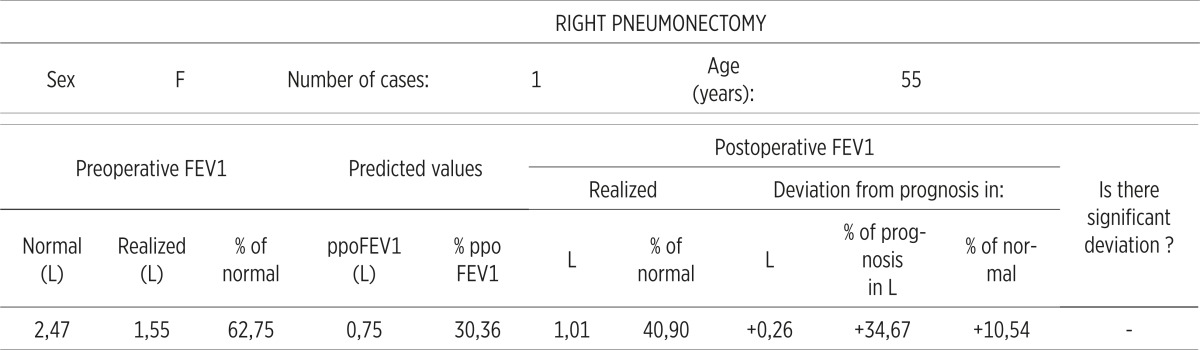 |
From the results above it is seen that the postoperative lung function after pneumonectomy can be predicted with a great per cent of confidence according to preoperative values and that there are no significant differences between these two methods: spirometry and perfusion lung scintigraphy.
5. DISCUSSION
For many patients with lung diseases, including lung cancer presented as localized disease, surgical resection is the only potentially curative option that provides the best perspective for long-term survival (14). However, high levels of coexisting illnesses make it difficult to undergo these patients to surgery. Smoking cigarettes, which is a major cause of cancer, causes chronic obstructive pulmonary disease (COPD), as well as atherosclerotic vascular disease, all of which reduces the ability of the patient for resection surgery (1). Decision to operate in such patients is much more difficult due to the lack of respiratory reserve which is the main determinant of postoperative morbidity and mortality (15, 23, 24). Patients with airway obstruction are limited in their daily life before the surgery, and an additional loss of lung tissue due to resection contributes to their inability. Loss of lung tissue in such patients can worsen much the postoperative pulmonary ventilatory function which can lead to respiratory failure and various cardiopulmonary complications, including death. The aim of the surgeon performing the operation of resection, especially in high-risk patients with already impaired preoperative pulmonary function, should be curative resection with preservation of the maximum amount of functional lung tissue. In all patients, especially ones with compromised pulmonary function, it is necessary to predict the probably post-resection lung function and identify possible steps to prevent complications during and after surgery and chronic pulmonary insufficiency (Table 5).
Table 5.
Comparison of % ppo FEV1 values obtained by spirometry and perfusion lung scintigraphy
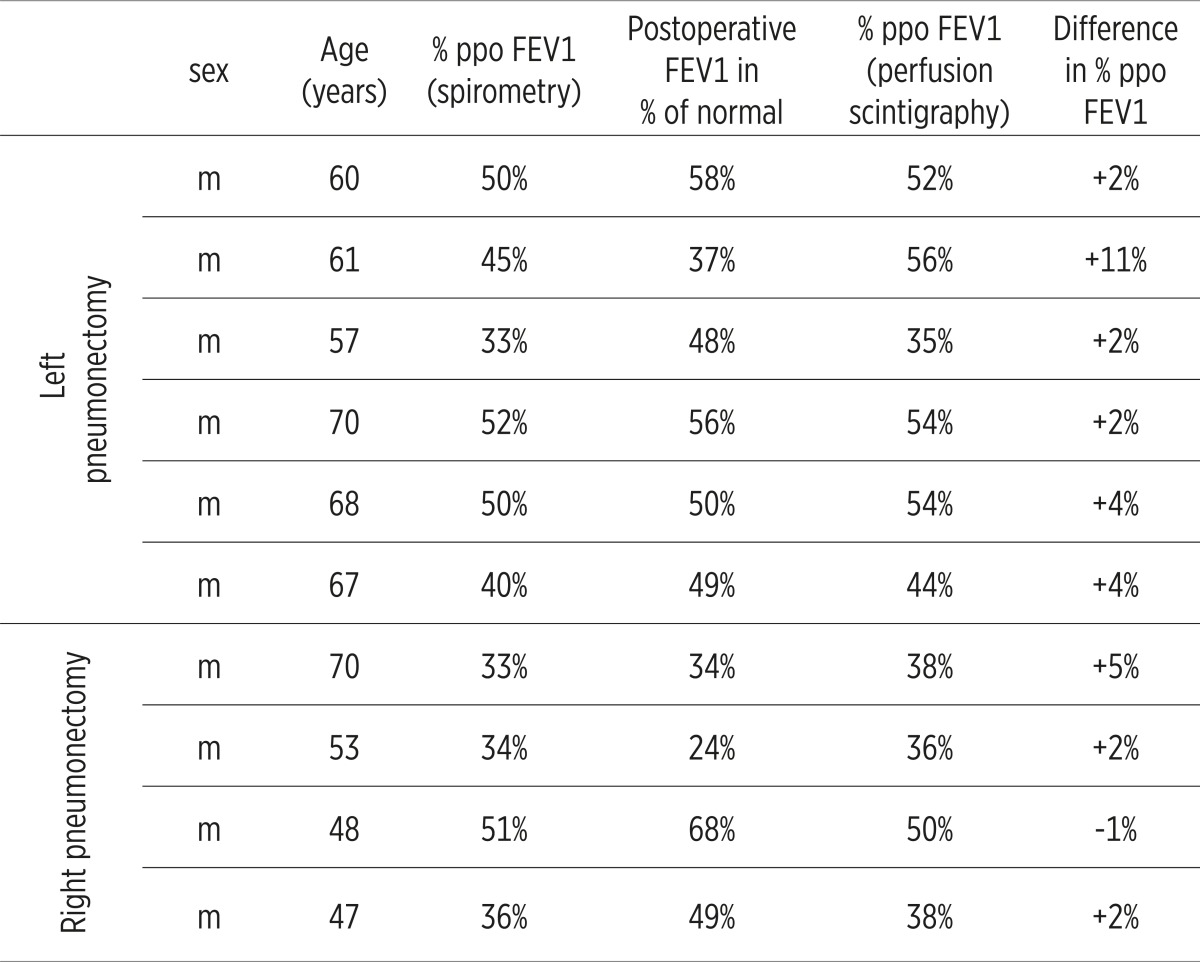 |
Advances in surgery and anesthesiology made the operations possible and in patients with severe associated cardiopulmonary diseases who previously were not given an approval for surgery (25). Two issues are raised during the preoperative functional assessment and so: a) whether the cardiopulmonary reserve is sufficient to enable the patient to survive the operation, and b) whether the patient be chronically incapable for daily life due to insufficient pulmonary function (26). The potential benefits of the surgery – pulmonary resection should be balanced in relation to postoperative morbidity and mortality. Nowadays the most common diseases that require resection of lung are malignant. But the question, asked already by Gass GD and Olsen GN in 1986th, stayed open – “what is the acceptable surgical mortality for the disease that is 100% fatal if not operated?” (25). All patients planned for lung surgical resection should be assessed preoperatively whether they can endure the maximal resection i.e. pneumonectomy if during the operation it is seen that planned lower resections i.e. lobectomy or bilobectomy will not give the satisfactory result. Various methods are recommended for preoperative evaluation of postoperative lung function. One of them is the simple calculation according to the number of lung segments planned to be resected, and one is the calculation from lung perfusion scintigraphy. Different authors give the different recommendations but great number of them recommend both methods to be done in planned pneumonectomy.
Prediction of postoperative pulmonary function can be done in different ways: the use of ventilation scintigraphy (10, 19, 20), perfusion scintigraphy (1, 2, 3, 10, 19, 20, 21, 22), quantitative CT (computed tomography) (19) and a simple calculation according to the number of lung segments planned to be removed (1, 3, 5, 22, 27, 28). All these methods provide similar quantitative estimates of the value of postoperative lung function (1, 2, 3, 16, 22, 24, 27, 29, 30, 31, 32).
All patients according to BTS and ACCP (2, 3) guides should have full lung function tests, and quantitative isotope perfusion scan if pneomonectomy is considered. Perfusion lung scintigraphy is an easy, available efficient test for prediction of postoperative lung function. The predicted postoperative FEV1 is in good correlation with actual values. In this test radionucleotid emission detected in any part of the lung can be expressed as a percentage of the total emission detected by gamma cameras that are placed over each hemi thorax (11). Perfusion, so and ventilation scintigraphy may be used to assess the residual lung function (20, 30, 31) as non-invasive methods to evaluate the contribution of each lung to the total ventilation and perfusion. Ventilation/perfusion studies have shown that the loss of function after pneumonectomy is approximately proportional to the percentage of the contribution of each lung to the total lung function. In our study in 10 patients planned for pneumonectomy we did ventilationperfusion scintgraphy but took into consideration only the result of perfusion.
In our study in 10 patients scheduled for pneumonectomy predicted postoperative pulmonary function is calculated not only by formula based on the number of segments to be removed but also by perfusion lung scintigraphy in order to compare the predictive value of these two methods,. It was found that the ppoFEV1 values calculated by the two methods did not differ significantly and in both methods we did not find the significant differences between predicted and achieved values. The biggest difference was found in one patient with left pneomonectomy where the calculated % ppoFEV1 by perfusion scintigraphy was 11% higher than that calculated by spirometry.
6. CONCLUSION
For many patients with lung diseases, including lung cancer present as localized disease, surgical resection is the only potentially curative option that provides the best perspective for long-term survival. It is necessary to predict the probably post-resection lung function to prevent complications during and after surgery and chronic pulmonary insufficiency. The potential benefits of the surgery–pulmonary resection should be balanced in relation to postoperative morbidity and mortality.
All patients planned for lung surgical resection, whether pneumonectomy is planned or not, should be assessed preoperatively whether they can endure the maximal resection, i.e. pneumonectomy if during the operation it is seen that planned lower resections will not give the satisfactory result.
Postoperative pulmonary function after pneumonectomy can be predicted by use of simple calculation according to the number of lung segments planned to be removed or by perfusion scintigraphy.
Predicted – prognosticated values of postoperative pulmonary function obtained by these two methods do not differ significantly, and there are no significant differences between predicted and achieved values in both methods.
Conflict of interest
None declared.
REFERENCES
- 1.Kearney DJ, Lee T, Reilly J, DeCamp M, Surgabaker DJ. Assessment of operative risk in patients undergoing lung resection. Importance of predicted pulmonary function. Chest. 1994;105:753–759. doi: 10.1378/chest.105.3.753. [DOI] [PubMed] [Google Scholar]
- 2.British Thoracic Society, Society of Cardiothoracic Surgeons of Great Britain and Ireland Working Party. BTS guidelines on the selection of patients with lung cancer for surgery. Thorax. 2001;56:89–108. doi: 10.1136/thorax.56.2.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beckles MA, Spiro SG, Colice GL, Rudd RM American College of Chest Physicians. The physiologic evaluation of patients with lung cancer being considered for resectional surgery. Chest. 2003;(Suppl 1):105S–114S. doi: 10.1378/chest.123.1_suppl.105s. [DOI] [PubMed] [Google Scholar]
- 4.Markos J, Mullan BP, Hillman DR. Preoperative assessment as a predictor of mortality and morbidity after lung resection. Am Rev Respir Dis. 1989;139:902–910. doi: 10.1164/ajrccm/139.4.902. [DOI] [PubMed] [Google Scholar]
- 5.Putnam JB, Colon R, McMutray MJ, All MK, Roth JA. Predicted pulmonary function and survival after pneumectomy for primary lung carcinoma. Ann Thorac Surg. 1990;49:909–914. doi: 10.1016/0003-4975(90)90864-3. [DOI] [PubMed] [Google Scholar]
- 6.Nakahara K, Ohno K, Hashimoto J. Prediction of postoperative respiratory failure in patients undergoing lung resection for lung cancer. Ann Thorac Surg. 1988;46:549–552. doi: 10.1016/s0003-4975(10)64694-2. [DOI] [PubMed] [Google Scholar]
- 7.Segal JJ, Buterworthh BA. Ventilatory capacity in chronic bronchitis in relation to carbon dioxide retention. Scand J Resp Dis. 1966;47:215–220. [PubMed] [Google Scholar]
- 8.Andjelic B, Milicevic B, Major Z. Preoperativno ispitivanje plucne funkcije. Najnovija shvatanja. Pneumon. 2000;38(1-20):95–99. [Google Scholar]
- 9.Le Roy Ladurie M, Ranson- Bitker B. Uncertainties in the expected value for forced expiratory volume in one second after surgery. Chest. 1986;90:223. doi: 10.1378/chest.90.2.222. [DOI] [PubMed] [Google Scholar]
- 10.Miller JI. Physiologic evaluation of pulmonary function in the candidate for lung resection. J Thorac Cardiovasc Surg. 1993;105:347, 351. [PubMed] [Google Scholar]
- 11.Celli BR. What is the value of preoperative pulmonary function testing? Medical clinics of North America. Medical Consultation. 1993;77:309–325. doi: 10.1016/s0025-7125(16)30253-x. [DOI] [PubMed] [Google Scholar]
- 12.Lockwood P. The principles of predicting risk of post-thoracotomy- function-related complications in bronchogenic carcinoma. Respiration. 1973;30:329–331. doi: 10.1159/000193048. [DOI] [PubMed] [Google Scholar]
- 13.Hamzagic H. U: Savremene mogucnosti klinicke fiziologije disanja. Sarajevo: Univerzitetska knjiga; 1999. Ocjena operabilnosti bolesnika; pp. 327–333. [Google Scholar]
- 14.Win T, Jackson A, Shraples L, Groves A, Wells FC, Ritchie AJ. Relationship between pulmonary function and lung cancer surgical outcome. Eur Respir J. 2005;25:594–599. doi: 10.1183/09031936.05.00077504. [DOI] [PubMed] [Google Scholar]
- 15.Tissi GM. Preoperative evaluation of pulmonary function. Am Rev Respir Dis. 1979;119:293–310. doi: 10.1164/arrd.1979.119.2.293. [DOI] [PubMed] [Google Scholar]
- 16.Pierce RJ, Copland KS, Barter CE. Preoperative risk evaluation for lung cancer. Predicted postoperative product as a predictor of surgical mortality. Am J Respir Crit Care Med. 1994;150:947–955. doi: 10.1164/ajrccm.150.4.7921468. [DOI] [PubMed] [Google Scholar]
- 17.Ninan M, Summers KE, Landreneau RJ. Standardised exercise oxymetry predicts postpneumonectomy outcome. Ann Thorac Surg. 1997;64:328. doi: 10.1016/S0003-4975(97)00474-8. [DOI] [PubMed] [Google Scholar]
- 18.Fergusson MK, Reader LB, Mick R. Optimising selection of patients for major lung resection. J Thorac Cardiovasc Surg. 1995;109:275–283. doi: 10.1016/S0022-5223(95)70389-6. [DOI] [PubMed] [Google Scholar]
- 19.Hill S, Newall C. Practical handbook of respiratory function testing. Stoke-on-Trent. Association of respiratory technology and physiology. 1999 [Google Scholar]
- 20.Olsen GN, Block AJ, Swenson EV, Castle JR, Wynne JW. Pulmonary function evaluation of the lung resection candidate: a prospective study. Am Rev Respir Dis. 1975;111:379–387. doi: 10.1164/arrd.1975.111.4.379. [DOI] [PubMed] [Google Scholar]
- 21.Boushy SF, Bligg DM. Clinical course related to preoperative and postoperative pulmonary function in patients with bronchogenic carcinoma. Chest. 1971;59:383–391. doi: 10.1378/chest.59.4.383. [DOI] [PubMed] [Google Scholar]
- 22.Wernly JA, DeMeester TR, Kircher PT. Clinical value of quantitative ventilation-perfusion lung scans in the surgical management of bronchogenic carcinoma. J Thorac Cardiovasc Surg. 1980;80:535–543. [PubMed] [Google Scholar]
- 23.Karliner JS, Coomaraswamy R, Williams MH. Relationship between preoperative pulmonary function studies and prognosis of patients undergoing pneumectomy for carcinoma in the lung. Chest. 1968;54:112–118. doi: 10.1378/chest.54.2.112. [DOI] [PubMed] [Google Scholar]
- 24.Gerson G. Preoperative respiratory function tests and postoperative mortality. A study of patients undergoing surgery for carcinoma of the bronchus. Br. J Anesth. 1969;41:967–971. doi: 10.1093/bja/41.11.967. [DOI] [PubMed] [Google Scholar]
- 25.Gass GD, Olsen GN. Preoperative pulmonary function testing to predict postoperative morbidity and mortality. Chest. 1986;89:127–135. doi: 10.1378/chest.89.1.127. [DOI] [PubMed] [Google Scholar]
- 26.Berchard D. In: Pulmonary function testing in diagnostic procedures for thoracic diseases. III. LoCicero J, editor. Philadelphia: WB Saunders; 1992. [Google Scholar]
- 27.Pate P, Tenholder MF, Griffin JP. Preoperative assessment of the high risk patient for lung resection. Ann Thorac Surg. 1996;61:1494–1500. doi: 10.1016/0003-4975(96)00087-2. [DOI] [PubMed] [Google Scholar]
- 28.Bolliger CT, Guckel S, Engel H. Prediction of functional reserves after lung resection: comparison between quantitative computed tomography, scintigraphy and anatomy. Respiration. 2002;69:482–489. doi: 10.1159/000066474. [DOI] [PubMed] [Google Scholar]
- 29.Intal B, Frost N. A comparison between measured and calculated changes in the lung function after operation for pulmonary cancer. Acta Anesth Scand. 1975;57(suppl.1):39–45. doi: 10.1111/j.1399-6576.1975.tb05411.x. [DOI] [PubMed] [Google Scholar]
- 30.Villa G, Zoccola R, Salio M. 99m Tc-DTPA ventilation and 99m Tc-MAA perfusion in preoperative evaluation of CA patients. Nuel Med Commun. 1990;11:96. [Google Scholar]
- 31.Cukic V, Baljic R. The Most Common Detected Risk and Etiologic Factors of Pulmonary Thromboembolism. Mat Soc Med. 2012 Dec;24(4):223–226. doi: 10.5455/msm.2012.24.223-226. doi: 10.5455/msm.2012.24.223-226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Alli MK, Mountain CF, Miller JM. Regional pulmonary function before and after pneumonectomy using xanon- 133. Chest. 1975;68:288–296. doi: 10.1378/chest.68.3.288. [DOI] [PubMed] [Google Scholar]