Abstract
Background
Improvements in patient-reported health-related quality of life (HRQoL) are important goals of cardiac rehabilitation (CR). In patients undergoing coronary angiography for angina and with documented coronary artery disease (CAD), the present study compared HRQoL over 6 months in CR participants and non-participants. Clinical predictors of CR participants were also assessed.
Methods
A total of 221 consecutive patients undergoing angiography for angina with documented CAD and who were eligible for a CR program were recruited. CR participants were enrolled in a six-week Phase II outpatient CR course (31%, n = 68) within 2 months following angiography and the non-participants were included as a control. At baseline (angiography), one and six months post angiography, clinical and HRQoL data were obtained including the Short Form-36 (SF-36) and the Seattle Angina Questionnaire (SAQ). The response rate for the HRQoL assessment was 68% (n = 150). Cross sectional comparisons were age-adjusted and performed using logistic or linear regression as appropriate. Longitudinal changes in HRQoL were assessed using least squares regression. Finally, a multiple logistic regression was fitted with CR participant as the final outcome.
Results
At angiography, the CR non-participants were older, and age-adjusted analyses revealed poorer physical (angina limitation: 54 ± 25 versus 64 ± 22, p <0.05) and mental HRQoL (significant psycho-social distress: 62%, n = 95 versus 47%, n = 32, p <0.05) compared to the CR participants. In addition, the CR participants were more likely to have undergone angiography for myocardial infarction (OR = 2.8, 95% CI 1.5-5.3, p = 0.001). By six months, all patients showed an improvement in HRQoL indices, however the rate of improvement did not differ between the controls and CR participants.
Conclusion
Following angiography, CAD patients reported improvements in both generic and disease-specific HRQoL, however CR participation did not influence this outcome. This may be explained by biases in CR enrollment, whereby acute patients, who may be less limited in HRQoL compared to stable, chronic patients, are targeted for CR participation. Further investigation is required so CR programs maximize the quality of life benefits to all potential CR patients.
Keywords: Coronary artery disease, Cardiac rehabilitation, Health-related quality of life
Background
Cardiac rehabilitation (CR) programs are recognized as an effective component for the management of patients with coronary artery disease (CAD) [1,2]. Two systematic reviews of almost 50 randomised controlled trials showed a 20% reduction in all cause mortality and a 27% reduction in cardiac mortality at two to five years [3,4]. However, the impact of CR on health-related quality of life (HRQoL) has been inconclusive [4] due to the limited studies and the methodologies employed.
Previous CR studies have largely targeted patients with a recent MI, coronary revascularisation or cardiac failure. However all patients with CAD could potentially benefit from CR, especially those with chronic diseases who are more likely to be significantly disabled. Despite this, it appears that patients with chronic angina are less likely to participate in these programs [5], especially if they are female [6] or do not undergo revascularisation procedures.
This study evaluated CAD patients undergoing diagnostic angiography to ascertain (i) the clinical characteristics and HRQoL of patients undergoing CR as compared to those who do not, (ii) to assess the clinical predictors of CR participants, and (iii) compare the 6-month HRQoL progress following angiography in those that do and do not receive CR.
Methods
This prospective, observational study recruited patients undergoing diagnostic angiography at the Queen Elizabeth Hospital (QEH) (Adelaide, Australia) between April 2003 and May 2007 and followed their progress over a 6-month period. The QEH is a tertiary hospital that provides cardiac care to the North-Western suburbs of Adelaide as well as diagnostic angiographic facilities for rural communities and smaller metropolitan hospitals. The Hospital provides Phase II CR services only for those patients residing within its local health care jurisdiction. This study was approved by the Central Northern Adelaide Health Service Ethics of Human Research Committee.
Study patients
Inclusion criteria for study enrollment included patients presenting for (i) invasive coronary angiography undertaken for the investigation of chest pain, (ii) angiographically documented obstructive CAD (≥ 50% stenosis in at least one epicardial coronary artery), and (iii) eligibility for Phase II CR at QEH (defined by residential location in the Western suburbs of Adelaide, Australia).
The study exclusion criteria were (a) non-coronary disorders such as aortic valve disease, and (b) inability to communicate in English/unable to complete written questionnaires.
Cardiac rehabilitation program
The QEH Phase II CR program comprises of biweekly visits held over a 6-week period. The course incorporates counseling and education on overall heart health and risk factor identification, nutrition, smoking cessation and weight loss. In addition, relaxation techniques and stress management for both patients and their partners or carers are included. A structured exercise program with an individualized exercise prescription was incorporated into each session.
Study protocol
Patients scheduled for coronary angiography for the investigation of chest pain were approached prior to the procedure and informed consent was obtained. At this time, a detailed clinical history was attained via standardized medical case-note review (conducted by clinical nurses and medical staff). At time of consent, all patients underwent a short interview with clinical nurses or trained research assistants assessing cardiovascular risk profile, and angina severity which was graded according to the Canadian Cardiovascular Society Classification (CCSC). This was followed by HRQoL assessment utilizing the self-administered Short-Form 36 (SF-36) [7] and the Seattle Angina Questionnaires (SAQ) [8] instruments. At 1 and 6 months post-angiography, patients were re-assessed by: (a) SF-36 and SAQ mailed out for completion, (b) review of hospital administrative system for hospital admissions/presentations and (2) follow-up phone calls made assessing angina status, medication use and clinical events.
Parameters assessed
Participation in CR was strictly defined as completion of the Phase II CR program as identified by the hospital CR services medical record system. The CR records were reviewed to identify patients who were documented as having completed the CR program at the hospital. The CR records at a second hospital, outside the local health care jurisdiction, were also reviewed to verify if any patients included in the study underwent CR at another nearby facility. Clinical data was obtained by medical case note review and patient interview. Socio-economic status was defined by the Australian Bureau of Statistics’ Socio-Economic Indexes for Areas scores, an accepted proxy measure for socio-economic status based on regional analyses in Australia [9]. HRQoL was assessed using both a generic (SF-36) and disease specific (SAQ) questionnaire. The SF-36 is a well-established measure [7], and has been shown to have good reliability, validity and responsiveness in patients with CAD [10], and also in a CR setting [11]. Elevated psychosocial distress was identified by the SF-36 Mental Summary Score (MCS) of ≤45 [12]. The SAQ is a disease-specific functional status measure quantifying five clinically relevant domains related to angina: physical limitation, angina stability, angina frequency, treatment satisfaction & quality of life [8]. It is reported to be the most appropriate disease-specific instrument for CAD [13].
Statistical analysis
Comparisons were made between patients who completed the Phase II CR program and those who did not participate in the program. Cross-sectional analyses between the CR participants and non-participants, for categorical or continuous variables were performed using either logistic or linear regression respectively, and age adjusted where appropriate. Longitudinal changes in SF-36 and SAQ scores from baseline to 6 months between the CR groups were compared utilising either random effects generalised least square or fixed effects ordinary least squares regression [14]. A multiple logistic regression was fitted with CR attendance as the final outcome. Variables identified for the multivariate analysis were selected following univariate tests significant at a p value level of 0.25. The final model was obtained using automatic backward elimination, and the final odds ratios (ORs) with 95% CIs and p values are reported. All analyses were performed with STATA (Version 11, StataCorp, Texas, USA).
Missing HRQoL data management
Follow-up HRQoL data over the 6 months was available in 68% of patients undergoing coronary angiography. To account for possible missing value bias, multiple imputation techniques [15] were used, conditioned upon the available SAQ and SF-36 scores. Imputation was performed by chained equations utilising switching regression, an iterative multivariable regression technique [16]. The data analysis was then repeated using the above-described methods but no significant deviation from the original models were observed. The HRQoL results presented below are those from the imputed data analysis.
Results
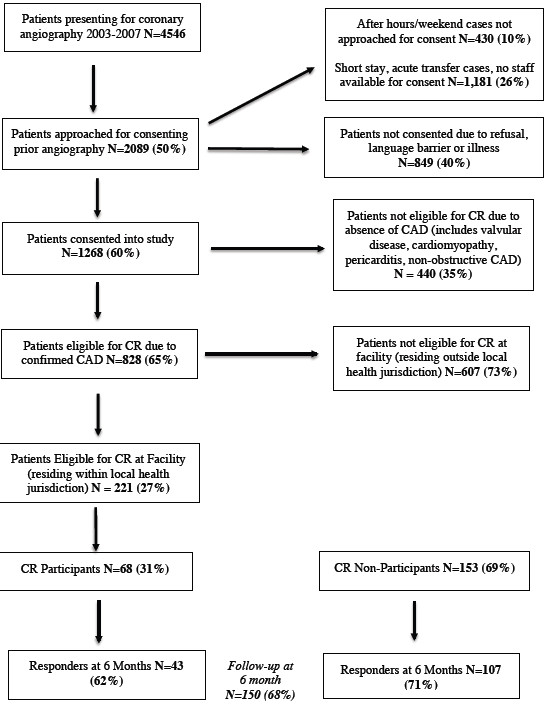
Between 28th April 2003 and 11th April 2007, 828 patients with angiographic evidence of CAD were identified and consented. Of these, 221 (27%) were eligible for referral to TQEH Phase II cardiac rehabilitation services and were recruited into the study. Figure 1 shows the Study Flow Diagram. Of these patients, 68 (31%) participated and completed the Phase II CR with almost 70% (n = 46) commencing the program within one month of coronary angiography. The mean waiting time for enrolment was 1.7 months (SD = 2.15, 95% CI 1.16-2.22).
Figure 1.
Flow Chart Describing Patients Presenting for Coronary Angiography and Eligible for Cardiac Rehabilitation at the Queen Elizabeth Hospital. Study flow diagram describing (a) the number of patients undergoing coronary angiography during the recruitment period, (b) the number of patients who were approached for consent, (c) reasons for no consent and exclusion, (d) the number of patients with confirmed CAD, (e) the number of patients who were eligible for CR program and (f) the response rate of CR participants and non-participants.
Baseline characteristics of study patients
Demographic and clinical features
Patients attending Phase II CR were significantly younger compared to patients who did not attend CR and thus subsequent analyses were age-adjusted. In relation to socioeconomic status, 24% (n = 37) of CR patients were identified as belonging to low, which was comparable to 16% (n = 11) in the CR non-participants (Table 1). The CR patients were more likely to have undergone angiography following an admission with an acute coronary syndrome (ACS) (Table 2), with 41% (n = 62) having experienced a recent myocardial infarction compared with 17% (n = 12) who did not have CR (p < 0.001). Despite this, the extent of angiographic disease was similar between groups as was the initial therapy although there was a slight trend towards medical therapy for those not participating in CR (Table 2).
Table 1.
Baseline clinical characteristics between CR participants and non-Participants
| n |
No CR n = 153 |
n |
CR n = 68 |
Total N = 221 |
||
|---|---|---|---|---|---|---|
| %/Mean ± SD | %/Mean ± SD | %/Mean ± SD | ||||
|
Cardiovascular Risk Factors | ||||||
| Age (years) |
153 |
65 ± 12* |
68 |
60 ± 12** |
221 |
63 ± 12 |
| Female |
153 |
31% |
68 |
24% |
221 |
29% |
| Current Smoker |
148 |
18% |
68 |
21% |
216 |
19% |
| Ex-smoker |
147 |
45% |
68 |
34% |
215 |
41% |
| Hypertension |
152 |
63% |
67 |
55% |
219 |
61% |
| Diabetes Mellitus |
149 |
33% |
67 |
28% |
216 |
31% |
| Hypercholesterolaemia |
149 |
74% |
68 |
71% |
217 |
73% |
|
Co-morbidities | ||||||
| Previous Myocardial Infarct |
152 |
32% |
68 |
32% |
220 |
32% |
| Prior Revascularisation |
153 |
28% |
68 |
24% |
221 |
27% |
| Cerebrovascular disease |
149 |
10% |
63 |
2% |
212 |
8% |
| Chronic obstructive pulmonary disease |
149 |
28% |
63 |
13%* |
212 |
24% |
| Peripheral arterial disease |
149 |
7% |
63 |
3% |
212 |
6% |
| Gastroesophageal disorders |
149 |
41% |
65 |
32% |
214 |
38% |
| Musculoskeletal disease |
149 |
14% |
63 |
22% |
212 |
17% |
| Psychiatric disorders |
147 |
25% |
64 |
17% |
211 |
23% |
|
Indication for Angiography | ||||||
| Recent Acute Coronary Syndrome |
150 |
41% |
66 |
65%** |
216 |
49% |
| Chronic Stable Angina |
150 |
55% |
66 |
33%** |
216 |
51% |
|
Low Socioeconomic status |
153 |
24% |
68 |
16% |
221 |
22% |
| CCS II-IV at Angiography | 141 | 61% | 63 | 51% | 204 | 58% |
** p < 0.01.
*p < 0.05, age adjusted.
Table 2.
Baseline cardiac history & HRQoL characteristics between CR participants and non-Participants
| n | No CR (n = 153) | n | CR (n = 68) | |
|---|---|---|---|---|
|
Pre-Angiography Cardioprotective Therapy | ||||
| Anti-platelet |
153 |
84% |
68 |
82% |
| Beta-blockers |
153 |
35% |
68 |
19% |
| Statins |
153 |
67% |
68 |
66% |
| ACE-inhibitor |
153 |
42% |
68 |
40% |
| Angiotensin Receptor Blocker |
153 |
18% |
68 |
13% |
|
Obstructive CAD Findings | ||||
| Single Vessel Disease |
153 |
29% |
68 |
32% |
| Double Vessel Disease |
|
39% |
|
32% |
| Triple Vessel Disease |
|
32% |
|
35% |
|
Initial Treatment Strategy | ||||
| Medical Therapy |
153 |
56% |
68 |
41% |
| Coronary Angioplasty/stent |
|
30% |
|
43% |
| Coronary bypass graft |
|
14% |
|
16% |
|
Seattle Angina Questionnaire | ||||
| Physical Limitation |
153 |
54±25 |
68 |
64±22* |
| Angina Stability |
153 |
37±31 |
68 |
40±34 |
| Angina Frequency |
153 |
59±27 |
68 |
66±27 |
| Treatment Satisfaction |
153 |
90±16 |
68 |
89±18 |
| Quality of Life |
153 |
42±22 |
68 |
44±24 |
|
Short-Form 36 | ||||
| Physical Summary Score |
153 |
34±11 |
68 |
38±11 |
| Mental Summary Score |
153 |
42±11 |
68 |
43±11 |
| Elevated Psychosocial Distress | 153 | 62% | 68 | 47%* |
*p < 0.05, **p < 0.01, age adjusted.
HRQoL indices
Scores on the HRQoL indices indicated the CR patients had a better quality of life in terms of both general health status and angina-specific morbidity at baseline (Table 2). Scores on the physical limitation domain of the SAQ were significantly higher in the CR patients compared to CR non-participants. The angina frequency domain was also higher (indicating less angina) in the CR patients, however this was not statistically significant. Consistent with this, scores on the SF-36 PCS tended to be higher in the CR patients. In addition, elevated psychosocial distress as identified by the SF-36 MCS, was lower in the CR patients (Table 2).
Predictors of CR participation
Predictors of CR participation were assessed in the overall group of patients presenting for angiography who were potentially eligible for referral. Following univariate analysis, backward elimination retained the following predictors: age, recent myocardial infarction and a prior history of musculoskeletal disease. In the final model, only recent myocardial infarction (OR = 2.8, 95% CI 1.5-5.3, p = 0.001) remained as a significant predictor of CR participation.
Six month outcomes in study patients
Clinical outcomes
At 6 months following angiography, at which time the CR patients had completed their rehabilitation programme, there were no differences between groups in relation to cardiac events (Table 3). Furthermore there were no differences between groups in changes in medical therapy or angina limitations as assessed via the CSCC system (Table 3).
Table 3.
Clinical progress over 6 months following angiography
| n |
No CR |
n |
CR |
n |
Total |
p
|
|
|---|---|---|---|---|---|---|---|
| % | % | % | Age adjusted | ||||
|
CCS Class II-IV 6 Months |
78 |
17% |
34 |
21% |
112 |
18% |
0.593 |
|
Medication Changes | |||||||
| Any Changes |
126 |
68% |
60 |
68% |
186 |
68% |
0.965 |
| Started Nitrates |
125 |
22% |
60 |
25% |
185 |
23% |
0.562 |
| Started CCB |
126 |
22% |
60 |
13% |
186 |
19% |
0.165 |
| Started Beta Blocker |
126 |
14% |
60 |
13% |
186 |
14% |
0.929 |
| Started Any Anti-anginal |
126 |
44% |
60 |
45% |
186 |
44% |
0.757 |
|
Cardiac Endpoints | |||||||
| ED Chest Pain Presentation |
128 |
16% |
59 |
10% |
187 |
14% |
0.263 |
| Chest pain re-admission |
127 |
16% |
59 |
10% |
186 |
14% |
0.345 |
| Myocardial infarction |
127 |
2% |
59 |
0% |
186 |
2% |
|
| Repeat angiography |
127 |
4% |
59 |
3% |
186 |
4% |
0.646 |
| PCI |
126 |
13% |
60 |
20% |
186 |
15% |
0.401 |
| CABG |
126 |
24% |
59 |
22% |
185 |
23% |
0.905 |
| Mortality |
153 |
2% |
68 |
1% |
221 |
2% |
0.844 |
| MI/Mortality | 153 | 3% | 68 | 1% | 221 | 3% | 0.659 |
HRQoL indices
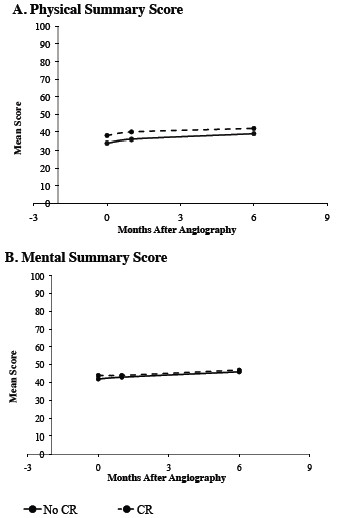
Figures 2 and 3 summarise the HRQoL indices over the 6-month period for the 2 study groups. The HRQoL indices were measured at 1 and 6 months although at the 1-month assessment time point, only 70% (n = 46) of the CR participants had commenced the program and none had completed the 6-week program. By 6 months, all the CR participants had completed the CR program. The SAQ-derived physical limitation, angina frequency, and quality of life scales all showed significant improvement over the 6-month study period. Both study groups also demonstrated statistically significant improvements in the SF-36 PCS and MCS over the 6-month period. However, no differences were observed in the rate of improvement from baseline over 6 months between the two groups in SAQ and SF-36 scores (Figures 2 and 3). Furthermore, cross-sectional analysis on the 1 and 6 month endpoints revealed no significant differences for both the SAQ and SF-36 scales between the two groups.
Figure 2.
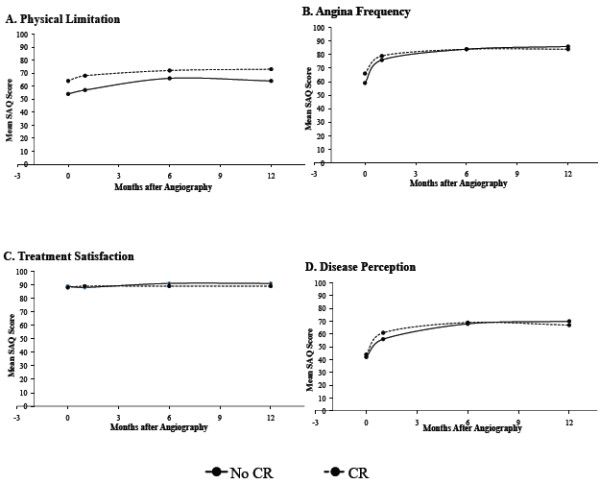
A-D. SAQ Domain Scores Over Six Months in CR Participants and Non-Participants. SAQ domain scores from baseline to six months compared between cardiac rehabilitation participants and non-participants. Longitudinal analysis revealed no significant differences in the rate or extent of improvement in the scores between CR participants and non-participants.
Figure 3.
A and B.SF-36 Summary Scores Over Six Months. SF-36 Physical (A) and Mental Summary Score (B) from baseline to six months compared between cardiac rehabilitation participants and non-participants. Longitudinal analysis revealed no significant differences in the rate or extent of improvement in the scores between CR participants and non-participants.
Discussion
This case–control study assessed the clinical characteristics of patients with angiographically-documented CAD who underwent CR and assessed their subsequent clinical and HRQoL progress over a 6-month period. The key findings from this study are (i) patients who undertake CR are younger and most likely to have experienced a recent myocardial infarction; and (ii) in the 6-month follow-up period, all patients showed an improvement in HRQoL indices independent of whether or not they had CR with no significant incremental benefit found in those who did have CR.
Patient selection for cardiac rehabilitation
Typically, CR has been targeted towards CAD patients who have experienced a recent MI [17] or undergone revascularisation therapies [18]. In this study, two-thirds of the CR patients had experienced a recent ACS, and this was the defining clinical characteristic of the cohort. Although it is paramount that all patients with an ACS be offered CR, it is equally important that stable patients with documented CAD should be offered CR. Indeed, as shown in our study, those who did not undertake CR were more chronically disabled, older, more physically disabled, more frequently identified with psychosocial distress and more often had a history of chronic stable angina (Table 1). Hence those who did not undertake CR may potentially have benefited more than those who did. Unfortunately this study does not provide insights into why patients did/did not participate in the Phase II CR program, thus it may reflect a selection bias by the health care system or patient choice.
Regardless of the reason, the findings of this study suggest that patients with chronic stable angina need to be targeted for enrolment to a CR program and this may be best undertaken at the time of diagnostic angiography. Targeting CR to patients undergoing revascularisation therapies is important and will provide CR to some chronic stable angina patients. However this study showed that those who did not receive CR tended to be managed with medical therapy (Table 2). Moreover, CR in stable angina patients has been shown to be superior to percutaneous coronary intervention in increasing exercise capacity and reducing hospital readmissions [19]. Thus an active program to target CR for disabled chronic stable angina patients needs to be considered.
The impact of cardiac rehabilitation on HRQoL
Improvement in HRQoL following CR has not been consistently documented as highlighted in a meta-analysis, which demonstrated that improvement in HRQoL with CR was better than in controls in only two of 12 trials [4]. However, comparing HRQoL findings in CR research is difficult due to the diversity of the instruments used. Earlier studies often used psychosocial well-being measures [5,6,20] rather than established generic and disease-specific instruments. Although more recent trials have increasingly employed the SF-36, there are still conflicting accounts concerning the influence of CR on HRQoL [21-24]. In addition, only few studies have used a disease-specific measure, however the choice of instrument has varied, and have included the MacNew [25,26], the Cardiac Quality of Life Index [27], and Quality of Life after Myocardial Infarction [28]. Hofer et al [29] highlights that a consistent application of a single disease-specific measure is warranted in CR research. Although the SAQ is an established and arguably the best disease-specific measure for CAD [13], the present study is the first to utilize the SAQ in a CR setting.
Study implications for cardiac rehabilitation
The failure of CR to impact on HRQoL in this and other studies warrants further consideration as it may reflect nuances relating to these studies rather than CR being ineffective. These include factors relating to the patient, the CR therapy and the study design.
Patient factors
As discussed above and reported in previous studies [30], the patients who did not participate in CR were the most disabled and thus may well have been those that would have derived the most benefit. Five patient-related factors may have influenced the findings in this study and should be closely considered in further studies. Firstly, CR efficacy in relation to impact on HRQoL has been shown to be age-dependent with previous studies reporting that younger (i.e. <41 years) and older (>65 years) patients benefitting the most from CR with no benefits observed in those 41–65 years [21,29]. In this study, the average age of the CR participants was 60 years, which may have influenced the findings. Secondly, almost half of the CR patients were identified as experiencing elevated psychosocial distress and this has a major impact on HRQoL. Thus if the CR program also focused on the treatment of psychosocial distress, an incremental improvement in HRQoL may have also been achieved. Thirdly, the CR study population predominantly underwent this therapy following a recent myocardial infarct. Muller-Nordhorn et al [21] showed that only patients undergoing CR following revascularisation procedures showed improvement in their SF-36 scores whereas recent myocardial infarct patients did not. Fourthly, patient participation in CR was 31%, which is comparable to rates reported by other studies, which have shown 14-43% of potential cardiac patients participate in CR programs [31-33]. Although all the study patients were eligible for CR, why the non-participants did not avail themselves to this opportunity is unclear. The focus by the health workers on the acute presentation [34,35] may have under-emphasized the importance in chronic conditions and thus education of both health care workers and patients is required. Logistic factors may have also influenced patient participation, such as transport availability/cost and session times. Finally, although all the CR patients completed the program, the commitment they made to the therapy was not assessed.
The CR therapy
CR programs are heterogeneous in content although professional societies are developing guidelines with core components to standardize the therapy [36,37]. Hence the findings from this study may not be applicable to other CR programs. In particular, tailored programs for different CAD presentations or populations may be useful to maximize benefits for patients, as suggested by Piepoli et al [38]. For example, tailored gender-specific programs have been shown to provide increased quality of life improvement for women [39]. Other aspects that require further considerations include CR program delivery and duration. The hospital-based CR program in this study may be better delivered as a telephone or on-line program, which may assist in patient participation and provide long-term access to all. This is important since recent studies have shown that a continued intervention following CR is effective in improving cardiovascular outcomes [40,41]. Also the duration of the CR program in this study was only 6 weeks whereas Piepoli [38] highlights that such short-term approaches are unlikely to yield long-term benefits or impact on quality of life.
Study design
The current study was a longitudinal case–control design and the limitations of this design may have influenced the findings. Firstly, the non-randomised allocation to CR therapy may have been influenced by a selection bias although the two groups were similar in their baseline HRQoL indices. Secondly, the study period was limited to 6 months and longer follow-up periods may have influenced the results. Of note, a meta-analysis of CR therapies showed improvement in all-cause mortality only at 3-year follow-up and not earlier [42]. Thirdly, important information such as referral and drop out rates, reasons for non-inclusion in CR, such as ambulation, were not available in this study. The lack of standardized data collection and thus insufficient program information causes difficulty when assessing biases [43]. Lastly, although the study was powered to detect a difference of 6 points on the SF-36 PCS, the total sample size was relatively small; larger studies are required and should investigate smaller but clinically relevant differences in HRQoL. It should also be noted that HRQoL assessment is best undertaken by patient interview where possible as opposed to mail-out surveys to increase response rate.
Conclusion
The importance of CR in reducing cardiac events amongst patients with established CAD has been previously established, however its benefit in improving HRQoL is less clear and has not been affirmed in this study. This study has shown that those CAD patients who do not undergo CR are usually more disabled with chronic disorders and thus may potentially be those who would derive the most benefit from this therapy. Thus further studies are required to identify which patients will receive the optimal benefit from CR therapy rather than simply targeting those who have experienced a recent ACS.
Competing interests
The authors declare that they have not competing interests.
Authors’ contributions
JB conceived the study, and participated in its design and helped draft the manuscript. RT participated in the study design, carried out the patient assessments, performed the statistical analysis and drafted the manuscript. Each author has read and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Contributor Information
Rosanna Tavella, Email: rosanna.tavella@adelaide.edu.au.
John F Beltrame, Email: john.beltrame@adelaide.edu.au.
Acknowledgement
The authors wish to acknowledge Renee Henthorn, Sue Sierp, the Lyell McEwin and Queen Elizabeth Hospitals Cardiac Rehabilitation teams for their valuable assistance in undertaking this study.
Funding and support
Professor John Beltrame is supported by a South Australian Cardiovascular Research Development Program Fellowship.
Rosanna Tavella is supported by The Queen Elizabeth Hospital Research Foundation Postgraduate Scholarship.
References
- Ades PA. Cardiac rehabilitation and secondary prevention of coronary heart disease. N Engl J Med. 2001;345:892–902. doi: 10.1056/NEJMra001529. [DOI] [PubMed] [Google Scholar]
- Dalal HM, Zawada A, Jolly K, Moxham T, Taylor RS. Home based versus centre based cardiac rehabilitation: Cochrane systematic review and meta-analysis. BMJ. 2010;340:b5631. doi: 10.1136/bmj.b5631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jolliffe JA, Rees K, Taylor RS, Thompson D, Oldridge N, Ebrahim S. Exercise-based rehabilitation for coronary heart disease. Cochrane Database Syst Rev. 2001. pp. 1–62. CD001800. [DOI] [PubMed]
- Taylor RS, Brown A, Ebrahim S. et al. Exercise-based rehabilitation for patients with coronary heart disease: systematic review and meta-analysis of randomized controlled trials. Am J Med. 2004;116:682–692. doi: 10.1016/j.amjmed.2004.01.009. [DOI] [PubMed] [Google Scholar]
- Daly J, Sindone AP, Thompson DR, Hancock K, Chang E, Davidson P. Barriers to participation in and adherence to cardiac rehabilitation programs: a critical literature review. Prog Cardiovasc Nurs. 2002;17:8–17. doi: 10.1111/j.0889-7204.2002.00614.x. [DOI] [PubMed] [Google Scholar]
- Ades PA, Waldmann ML, Polk DM, Coflesky JT. Referral patterns and exercise response in the rehabilitation of female coronary patients aged greater than or equal to 62 years. Am J Cardiol. 1992;69:1422–1425. doi: 10.1016/0002-9149(92)90894-5. [DOI] [PubMed] [Google Scholar]
- Ware JE, Snow KK, Kosinski M, Gandek B. SF-36 health survey: manual and interpretation guide. Boston: The Health Institute, New England Medical Center; 1993. [Google Scholar]
- Spertus JA, Winder JA, Dewhurst TA. et al. Development and evaluation of the Seattle Angina Questionnaire: a new functional status measure for coronary artery disease. J Am Coll Cardiol. 1995;25:333–341. doi: 10.1016/0735-1097(94)00397-9. [DOI] [PubMed] [Google Scholar]
- ABS. Socio-economic indexes for areas, Australia, 2001. Canberra: Australian Bureau of Statistics; 2003. [Google Scholar]
- McHorney CA, Ware JE Jr, Lu JF, Sherbourne CD. The MOS 36-item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care. 1994;32:40–66. doi: 10.1097/00005650-199401000-00004. [DOI] [PubMed] [Google Scholar]
- Jette DU, Downing J. Health status of individuals entering a cardiac rehabilitation program as measured by the medical outcomes study 36-item short-form survey (SF-36) Phys Ther. 1994;74:521–527. doi: 10.1093/ptj/74.6.521. [DOI] [PubMed] [Google Scholar]
- Tavella R, Air T, Tucker G, Adams R, Beltrame JF, Schrader G. Using the Short Form-36 mental summary score as an indicator of depressive symptoms in patients with coronary heart disease. Qual Life Res. 2010;19:1105–1113. doi: 10.1007/s11136-010-9671-z. [DOI] [PubMed] [Google Scholar]
- Dougherty CM, Dewhurst T, Nichol WP, Spertus J. Comparison of three quality of life instruments in stable angina pectoris: Seattle Angina Questionnaire, Short Form Health Survey (SF-36), and Quality of Life Index-Cardiac Version III. J Clin Epidemiol. 1998;51:569–575. doi: 10.1016/S0895-4356(98)00028-6. [DOI] [PubMed] [Google Scholar]
- Stock J, Waston M. In: Introduction to econometrics. Stock J, Watson M, editor. Boston: Addison Wesley Higher Education; 2003. Regression with panel data. [Google Scholar]
- Rubin D. Multiple imputation for Non-response in surveys. New York: Wiley; 1987. [Google Scholar]
- van Buuren S, Boshuizen HC, Knook DL. Multiple imputation of missing blood pressure covariates in survival analysis. Stat Med. 1999;18:681–694. doi: 10.1002/(SICI)1097-0258(19990330)18:6<681::AID-SIM71>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- Ades PA, Huang D, Weaver SO. Cardiac rehabilitation participation predicts lower rehospitalization costs. Am Heart J. 1992;123:916–921. doi: 10.1016/0002-8703(92)90696-S. [DOI] [PubMed] [Google Scholar]
- Hedback B, Perk J, Hornblad M, Ohlsson U. Cardiac rehabilitation after coronary artery bypass surgery: 10-year results on mortality, morbidity and readmissions to hospital. J Cardiovasc Risk. 2001;8:153–158. doi: 10.1097/00043798-200106000-00006. [DOI] [PubMed] [Google Scholar]
- Hambrecht R, Walther C, Mobius-Winkler S. et al. Percutaneous coronary angioplasty compared with exercise training in patients with stable coronary artery disease: a randomized trial. Circulation. 2004;109:1371–1378. doi: 10.1161/01.CIR.0000121360.31954.1F. [DOI] [PubMed] [Google Scholar]
- Bunker S, McBurney H, Cox H, Jelinek M. Identifying participation rates at outpatient cardiac rehabilitation programs in Victoria, Australia. J Cardiopulm Rehabil. 1999;19:334–338. doi: 10.1097/00008483-199911000-00001. [DOI] [PubMed] [Google Scholar]
- Muller-Nordhorn J, Kulig M, Binting S. et al. Change in quality of life in the year following cardiac rehabilitation. Qual Life Res. 2004;13:399–410. doi: 10.1023/B:QURE.0000018473.55508.6a. [DOI] [PubMed] [Google Scholar]
- Hawkes AL, Nowak M, Speare R. Short Form-36 Health Survey as an evaluation tool for cardiac rehabilitation programs: is it appropriate? J Cardiopulm Rehabil. 2003;23:22–25. doi: 10.1097/00008483-200301000-00005. [DOI] [PubMed] [Google Scholar]
- Pasquali SK, Alexander KP, Coombs LP, Lytle BL, Peterson ED. Effect of cardiac rehabilitation on functional outcomes after coronary revascularization. Am Heart J. 2003;145:445–451. doi: 10.1067/mhj.2003.172. [DOI] [PubMed] [Google Scholar]
- Izawa K, Hirano Y, Yamada S, Oka K, Omiya K, Iijima S. Improvement in physiological outcomes and health-related quality of life following cardiac rehabilitation in patients with acute myocardial infarction. Circ J. 2004;68:315–320. doi: 10.1253/circj.68.315. [DOI] [PubMed] [Google Scholar]
- Benzer W, Platter M, Oldridge NB. et al. Short-term patient-reported outcomes after different exercise-based cardiac rehabilitation programmes. Eur J Cardiovasc Prev Rehabil. 2007;14:441–447. doi: 10.1097/HJR.0b013e32802bf7ae. [DOI] [PubMed] [Google Scholar]
- Yohannes AM, Doherty P, Bundy C, Yalfani A. The long-term benefits of cardiac rehabilitation on depression, anxiety, physical activity and quality of life. J Clin Nurs. 2010;19:2806–2813. doi: 10.1111/j.1365-2702.2010.03313.x. [DOI] [PubMed] [Google Scholar]
- Kennedy MD, Haykowsky M, Daub B, Van Lohuizen K, Knapik G, Black B. Effects of a comprehensive cardiac rehabilitation program on quality of life and exercise tolerance in women: a retrospective analysis. Curr Control Trials Cardiovasc Med. 2003;4:1. doi: 10.1186/1468-6708-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oldridge N, Guyatt G, Jones N. et al. Effects on quality of life with comprehensive rehabilitation after acute myocardial infarction. Am J Cardiol. 1991;67:1084–1089. doi: 10.1016/0002-9149(91)90870-Q. [DOI] [PubMed] [Google Scholar]
- Hofer S, Kullich W, Graninger U. et al. Cardiac rehabilitation in Austria: long term health-related quality of life outcomes. Health Qual Life Outcomes. 2009;7:99. doi: 10.1186/1477-7525-7-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harlan WR 3rd, Sandler SA, Lee KL, Lam LC, Mark DB. Importance of baseline functional and socioeconomic factors for participation in cardiac rehabilitation. Am J Cardiol. 1995;76:36–39. doi: 10.1016/S0002-9149(99)80797-8. [DOI] [PubMed] [Google Scholar]
- Bethell HJ, Turner SC, Evans JA, Rose L. Cardiac rehabilitation in the United Kingdom. How complete is the provision? J Cardiopulm Rehabil. 2001;21:111–115. doi: 10.1097/00008483-200103000-00008. [DOI] [PubMed] [Google Scholar]
- Kotseva K, Wood D, De Backer G, De Bacquer D, Pyorala K, Keil U. EUROASPIRE III: a survey on the lifestyle, risk factors and use of cardioprotective drug therapies in coronary patients from 22 European countries. Eur J Cardiovasc Prev Rehabil. 2009;16:121–137. doi: 10.1097/HJR.0b013e3283294b1d. [DOI] [PubMed] [Google Scholar]
- Blackburn GG, Foody JM, Sprecher DL, Park E, Apperson-Hansen C, Pashkow FJ. Cardiac rehabilitation participation patterns in a large, tertiary care center: evidence for selection bias. J Cardiopulm Rehabil. 2000;20:189–195. doi: 10.1097/00008483-200005000-00007. [DOI] [PubMed] [Google Scholar]
- Corra U, Piepoli MF, Carre F. et al. Secondary prevention through cardiac rehabilitation: physical activity counselling and exercise training: key components of the position paper from the Cardiac Rehabilitation Section of the European Association of Cardiovascular Prevention and Rehabilitation. Eur Heart J. 2010;31:1967–1974. doi: 10.1093/eurheartj/ehq236. [DOI] [PubMed] [Google Scholar]
- Cortes O, Arthur HM. Determinants of referral to cardiac rehabilitation programs in patients with coronary artery disease: a systematic review. Am Heart J. 2006;151:249–256. doi: 10.1016/j.ahj.2005.03.034. [DOI] [PubMed] [Google Scholar]
- Balady GJ, Ades PA, Comoss P. et al. Core components of cardiac rehabilitation/secondary prevention programs: A statement for healthcare professionals from the American Heart Association and the American Association of Cardiovascular and Pulmonary Rehabilitation Writing Group. Circulation. 2000;102:1069–1073. doi: 10.1161/01.CIR.102.9.1069. [DOI] [PubMed] [Google Scholar]
- British Association for Cardiovascular Prevention and Rehabilitation. The BACPR Standards and Core Components for Cardiovascular Disease Prevention and Rehabilitation 2012. 2nd. United Kingdom; 2012. [Google Scholar]
- Piepoli MF, Corra U, Benzer W. et al. Secondary prevention through cardiac rehabilitation: from knowledge to implementation. A position paper from the cardiac rehabilitation section of the European association of cardiovascular prevention and rehabilitation. Eur J Cardiovasc Prev Rehabil. 2010;17:1–17. doi: 10.1097/HJR.0b013e3283313592. [DOI] [PubMed] [Google Scholar]
- Beckie TM, Beckstead JW, Schocken DD, Evans ME, Fletcher GF. The effects of a tailored cardiac rehabilitation program on depressive symptoms in women: A randomized clinical trial. Int J Nurs Stud. 2010;48:3–12. doi: 10.1016/j.ijnurstu.2010.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giannuzzi P, Temporelli PL, Marchioli R. et al. Global secondary prevention strategies to limit event recurrence after myocardial infarction: results of the GOSPEL study, a multicenter, randomized controlled trial from the Italian Cardiac Rehabilitation Network. Arch Intern Med. 2008;168:2194–2204. doi: 10.1001/archinte.168.20.2194. [DOI] [PubMed] [Google Scholar]
- Wood DA, Kotseva K, Connolly S. et al. Nurse-coordinated multidisciplinary, family-based cardiovascular disease prevention programme (EUROACTION) for patients with coronary heart disease and asymptomatic individuals at high risk of cardiovascular disease: a paired, cluster-randomised controlled trial. Lancet. 2008;371:1999–2012. doi: 10.1016/S0140-6736(08)60868-5. [DOI] [PubMed] [Google Scholar]
- Chew DP, Aroney CN, Aylward PE. et al. 2011 Addendum to the national heart foundation of Australia/cardiac society of Australia and New Zealand guidelines for the management of acute coronary syndromes (ACS) 2006. Heart Lung Circ. 2011;20:487–502. doi: 10.1016/j.hlc.2011.03.008. [DOI] [PubMed] [Google Scholar]
- Davies P, Taylor F, Beswick A. et al. Promoting patient uptake and adherence in cardiac rehabilitation. Cochrane Database Syst Rev. 2010;7:1–39. doi: 10.1002/14651858.CD007131.pub2. CD007131. [DOI] [PMC free article] [PubMed] [Google Scholar]