Abstract
AIM: To propose a new endoscopic classification of achalasia for selecting patients appropriate for undergoing peroral endoscopic myotomy (POEM).
METHODS: We screened out the data of patients with achalasia examined from October 2000 to September 2011 at our Digestive Endoscopic Center with endoscopic pictures clear enough to reveal the morphology of middle and lower esophagus. After analyzing the correlation between the endoscopic morphology of the esophageal lumen and POEM, we proposed a new endoscopic classification (Ling classification) of achalasia according to three kinds of endoscopically viewed structures: multi-ring structure, crescent-like structure and diverticulum structure. There were three types based on the criteria of Ling classification: type I, smooth without multi-ring, crescent-like structure or diverticulum structure; type II, with multi-ring or crescent-like structure but without diverticulum structure; and type III, with diverticulum structure. Type II was classified into three subtypes: Ling IIa, Ling IIb and Ling IIc; and type III also had three subtypes: Ling IIIl, Ling IIIr and Ling IIIlr. Two endoscopists made a final decision upon mutual agreement through discussion if their separately recorded characteristics were different.
RESULTS: Among the 976 screened patients with achalasia, 636 patients with qualified endoscopic pictures were selected for the analysis, including 405 males and 231 females. The average age was 42.7 years, ranging from 6 to 93 years. Type I was the most commonly observed type of achalasia, accounting for 64.5% (410/636), and type III was the least commonly observed type of achalasia, accounting for 2.8% (18/636). And type II accounted for 32.7% (208/636) and subtype of Ling IIa, Ling IIb and Ling IIc accounted for 14.6% (93/636), 9.9% (63/636) and 8.2% (52/636), respectively. And subtype of Ling IIIl, Ling IIIr and Ling IIIlr accounted for 0.8% (5/636), 0.3% (2/636) and 1.7% (11/636), respectively.
CONCLUSION: A new endoscopic classification of achalasia is proposed that might help in determining the proper candidates for POEM.
Keywords: Endoscopy, Classification, Achalasia, Selection, Peroral endoscopic myotomy
INTRODUCTION
Treatments for achalasia include pharmacological therapy, endoscopic injection of botulinum toxin, endoscopic dilation, and laparoscopic or open surgery[1-5], among which laparoscopic surgery with fundoplication has been widely accepted as the primary therapy because of its low complication rate, durable symptom relief, and low incidence of postoperative gastroesophageal reflux[6-10]. However, a new alternative therapy named peroral endoscopic myotomy (POEM) has recently been reported to be effective clinically for esophageal achalasia without serious complications at least in a short term[11-13]. We have performed POEM since 2010, and found that not all the patients with achalasia were eligible to undergo POEM. If the esophageal lumen was too tortuous or if a diverticulum was formed in the middle or the lower part of the esophagus, to establish an appropriate submucosal tunnel would, to a great extent, cause a penetrative damage to the mucosa or the muscularis propria, which obviously destroyed the completeness of the submucosal tunnel, leading to a serious outcome such as mediastinitis if not successfully treated in time. Mucosal penetration at the gastric cardia has been firstly reported to occur respectively in 2 out of 5 and 2 out of 17 patients in two studies, although it did not cause serious consequences[12-14]. The occurrence of mucosal penetration at the cardia was also confirmed by several other studies[15-19]. Therefore, it is very important and necessary to make a precise judgment whether or not a patient with achalasia is a proper candidate for POEM. Inoune et al[12] suggested that a patient was not fit for a POEM therapy if a double-lumen sign was detected in the esophageal computed tomography (CT). However, no other studies have, to our best knowledge, reported the correlation between the morphology of the esophageal lumen and the indications of POEM. To better judge if a patient was suitable for POEM, we analyzed the correlation between the endoscopic morphology of the esophageal lumen and POEM, and proposed a new endoscopic classification of achalasia (Ling classification), hoping to assist in determining the indications of POEM.
MATERIALS AND METHODS
We reviewed the data of endoscopic examinations of patients diagnosed with achalasia from October 2000 to September 2011 at our Digestive Endoscopic Center and screened out the data of patients with endoscopic pictures clear enough to reveal the morphology of the middle and the lower parts of the esophagus. Two endoscopists (Li HK and Linghu EQ) independently recorded the characteristics of the morphology of the middle and the lower parts of the esophagus, which included three endoscopically detected intraluminal structures: multi-ring structure, crescent-like structure and diverticulum structure. There were three types according to the Ling classification[20]: type I, smooth without multi-ring , crescent-like structure or diverticulum structure; type II, with multi-ring or crescent-like structure but without diverticulum structure; and type III, with diverticulum structure (Figure 1). Type II was further divided into three subtypes: Ling IIa, Ling IIb and Ling IIc, and type III also had three subtypes: Ling IIIl, Ling IIIr and Ling IIIlr. The criteria for classifying subtypes II and III were as follows: Ling IIa, with multi-ring structure; Ling IIb, with crescent-like structure and the midpoint of its inner edge not larger than 1/3 of the esophageal lumen; Ling IIc, with crescent-like structure and the midpoint of its inner edge over 1/3 of the esophageal lumen; Ling IIIl, diverticulum structure in the left wall of esophagus; Ling IIIr, diverticulum structure in the right wall of esophagus; and Ling IIIlr, diverticulum structure in both the left and right walls of esophagus. If the two endoscopists recorded different characteristics, they would discuss together and made a final decision upon mutual agreement.
Figure 1.
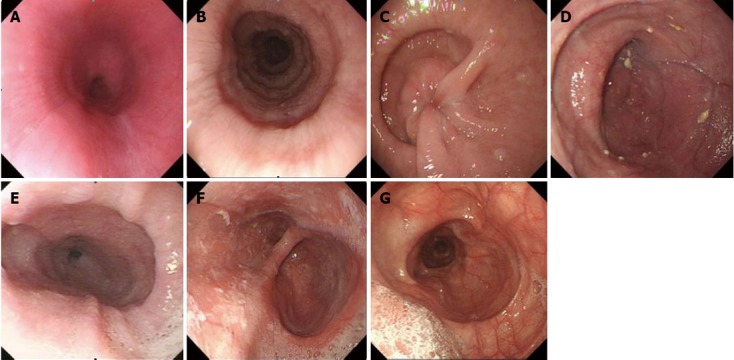
Typical pictures of each type or subtype in Ling classification. A: Type I; B: Type IIa; C: Type IIb; D: Type IIc; E: Type IIIl; F: Type IIIr; G: Type IIIlr.
RESULTS
Data of 976 patients with achalasia were collected and analyzed, and 636 of them were screened out with clear endoscopic pictures revealing the morphology of middle and lower esophagus, while 340 were excluded for unqualified pictures. Among the 636 patients, 405 were male and 231 were female. The average age was 42.7 years, ranging from 6 to 93 years.
We named our proposed classification Ling classification since Ling is short for Linghu, which is the family name of the corresponding author. As shown in Table 1, 64.5% (410/636) of the patients were classified as type I, which was the most common type of achalasia based on the Ling classification; 32.7% (208/636) of the patients were classified as type II; and only 2.8% (18/636) as type III. The typical pictures of each type or subtype are shown in Figure 1. The proportion of each type or subtype is described in Table 1 according to the Ling classification.
Table 1.
Proportion of each type or subtype according to Ling classification n (%)
| Type | Proportion |
| Ling I | 410 (64.5) |
| Ling II | 208 (32.7) |
| Ling IIa | 93 (14.6) |
| Ling IIb | 63 (9.9) |
| Ling IIc | 52 (8.2) |
| Ling III | 18 (2.8) |
| Ling IIIl | 5 (0.8) |
| Ling IIIr | 2 (0.3) |
| Ling IIIlr | 11 (1.7) |
DISCUSSION
As early as in 1980, Ortega et al[21] for the first time performed cutting esophageal muscles using the needle knife through the peroral endoscope, but few doctors followed them due to the possible mediastinal contamination. Until 2007, Pasricha et al[22] reported the possibility of POEM through a submucosal tunnel in a porcine model. In 2010, Inoue et al[12] started to use POEM to treat patients with achalasia after several refinements, including applications of endoscopic submucosal dissection technique, the triangle-tip knife, positive pressure ventilation and CO2 insufflations through the endoscope during POEM, and they reported a satisfactory short-term effects. Swanström et al[13] also reported their experience of POEM in patients with achalasia and esophageal motility disorders. Both of the above-mentioned clinical trials demonstrated that small mucosal penetration at the gastric cardia occurred respectively in 2 out of 5 and 2 out of 17 patients, but were treated differently. Inoue observed the penetrations without special treatment, while Swanström used traditional hemostatic clips to seal the penetrations. Even though no serious clinical outcomes were observed, we should keep alert about the incompleteness of the submucosal tunnel caused by mucosal penetration at the cardia, and we used fibrin sealant to treat this mucosal penetration[15]. If the penetrations were in situ, fluids from the stomach or the esophagus might flow into the tunnel, which might affect the healing of the incised inner circular muscles and further influence the effects of POEM.
We think that the reason why mucosal penetrations are more likely to occur in the cardia is that the working space in the submucosal tunnel near the cardia is narrower than in other parts, which makes a precise electrocautery without damaging the cardiac mucosa very difficult. Similarly, if POEM was performed in patients with a very tortuous esophagus, penetrations of mucosa or muscularis propria could happen where the working space is confined by the tortuousness of the esophagus. So, from the point of minimizing complications like penetrations of mucosa or muscularis propria, it is very important to make a precise judgment whether a patient with achalasia is or not a proper candidate for POEM. Inoune mentioned that a patient was not fit for a POEM therapy if a double-lumen sign was detected in the CT scan[12], however, no other studies on POEM have reported the correlation between the morphology of esophageal lumen and the indications of POEM[13-14,16-18]. We, therefore, proposed the endoscopic Ling classification of achalasia, hoping to assist in determining the indications of POEM after analyzing the correlation between the endoscopic morphology of the esophageal lumen and POEM.
After reviewing the endoscopic pictures of nearly 1000 patients, we screened out 636 patients with pictures clear enough to reveal the middle and lower esophagus and analyzed the characteristics of the morphology of esophagus. Because the submucosal tunnel established during POEM generally starts from the middle esophagus and ends at about 3 cm distal to the cardia[12,13], we focused on the morphology of the middle and lower esophagus. Based on the Ling classification, the esophagus of type I is very smooth and without multi-ring structure, crescent-like structure or diverticulum structure, so type I patients are the most safe type to undergo POEM. The esophagus of type Ling IIa with multi-ring structure was not so smooth as type I, but not much difficulties were encountered during establishment of the submucosal tunnel in our practice of POEM. The crescent-like structure present in type Ling IIb or Ling IIc actually reflexes the tortuousness of the esophageal lumen, and the degree of tortuousness is more severe in Ling IIc than in Ling IIb, and therefore to establish a submucosal tunnel across the tortuous point of the esophagus is more difficult and more likely to cause a penetration in Ling IIc than in Ling IIb. Diverticulum structure occurred in type III, making it the most challenging type to establish a submucosal tunnel across the diverticulum.
Location of the crescent-like structure or the diverticulum structure can greatly affect the success of a POEM therapy. Since we and other operators[12,13] preferred the establishment of submucosal tunnel in the right wall of the esophagus leading to the lesser curvature of stomach, the submucosal tunnel would be very difficult to be established if a crescent-like structure or diverticulum structure was located in the right wall of the esophagus. Otherwise, if a crescent-like structure or diverticulum structure was located in the left wall of the esophagus, the submucosal tunnel would be established with much less difficulty.
Based on our experiences, we suggest that type Ling I and Ling IIa patients are safe for POEM, and that Ling IIb patients can also be considered for POEM, but more cautions should be used to avoid damaging the mucosa or the muscularis propria when the submucosal tunnel is being established across the crescent-like structure. For Ling IIc and Ling III patients, POEM can be performed when the crescent-like structure is on the left side of the esophageal lumen, but it is not recommended when the crescent-like structure is on the right side. These suggestions may be modified in the future with improvement of technology. For example, when a new and safe technique to establish a tunnel across a crescent-like structure is available, a POEM therapy would be recommended for all the Ling II patients free of concerns of penetrations irrespective of the location of the crescent-like structures.
One classification of achalasia categorized by high-resolution manometry has been reported to be promising in predicting the efficacy of treatment of achalasia, such as balloon dilation[23-25]. But up to now, there has been no report about its usefulness for selecting candidates for POEM. And the relationship between the proposed endoscopic classification and manometric classification remains an interesting point worth further studying.
Since not all patients were eligible for undergoing POEM, we analyzed the characteristics of the esophageal lumen and proposed the Ling classification, hoping that Ling classification might help in determining the proper candidates for POEM, thus minimizing the complications such as penetration of mucosa or muscularis propria because other therapies such as endoscopic injection of botulinum toxin, endoscopic dilation or surgery would be recommended instead of POEM in patients with a severely tortuous esophagus. However, further prospective studies are needed to determine the usefulness of Ling classification for selecting candidates for POEM.
COMMENTS
Background
Peroral endoscopic myotomy (POEM) has been primarily confirmed to be effective for patients with achalasia in the short term by several studies since it was first clinically reported in 2010, but not all the patients with achalasia were eligible for a POEM therapy. If the esophageal lumen was too tortuous or a diverticulum was formed in the middle or the lower part of the esophagus, it would be quite challenging to establish a submucosal tunnel.
Research frontiers
Although no serious clinical outcomes of complications like mucosal perforation in the cardia has been reported, it is still of vital importance to select proper candidates for POEM so as to minimize those complications.
Innovations and breakthroughs
The authors proposed a new endoscopic classification of achalasia after analyzing the endoscopic pictures which clearly revealed the morphology of middle and lower esophagus and this new Ling classification of achalasia might assist in determining the indications of POEM.
Applications
The authors suggest the followings for choosing the candidates for POEM: Ling I and Ling IIa patients are safe for POEM, and Ling IIb patients can also be considered for POEM but more cautions should be used to avoid damaging the mucosa or the muscularis propria when the submucosal tunnel is being established across the crescent-like structure. For Ling IIc and Ling III patients, POEM can be performed when the crescent-like structure is on the left side of the esophageal lumen, but it is not recommended when the crescent-like structure is on the right side.
Terminology
POEM is a newly developed endoscopic therapy for achalasia by myotomy of the inner circular muscle of the lower esophagus, thus reducing the lower esophageal sphincter pressure and relieving symptoms of the patients.
Peer review
This study proposed a new endoscopic classification of achalasia based on the morphology of the middle and lower part of the esophagus, and role of the new classification in determining proper candidates for POEM was explored, and the authors suggested indications based on this new classification,which is very interesting. However, further prospective studies are needed to determine the validity of this Ling classification for selecting candidates for POEM.
Footnotes
P- Reviewers Patti MG, Traube M S- Editor Zhai HH L- Editor A E- Editor Xiong L
References
- 1.Roll GR, Rabl C, Ciovica R, Peeva S, Campos GM. A controversy that has been tough to swallow: is the treatment of achalasia now digested? J Gastrointest Surg. 2010;14 Suppl 1:S33–S45. doi: 10.1007/s11605-009-1013-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cheatham JG, Wong RK. Current approach to the treatment of achalasia. Curr Gastroenterol Rep. 2011;13:219–225. doi: 10.1007/s11894-011-0190-z. [DOI] [PubMed] [Google Scholar]
- 3.Gockel I, Sgourakis G, Drescher DG, Lang H. Impact of minimally invasive surgery in the spectrum of current achalasia treatment options. Scand J Surg. 2011;100:72–77. doi: 10.1177/145749691110000202. [DOI] [PubMed] [Google Scholar]
- 4.Leyden JE, Moss AC, MacMathuna P. Endoscopic pneumatic dilation versus botulinum toxin injection in the management of primary achalasia. Cochrane Database Syst Rev. 2006;(4):CD005046. doi: 10.1002/14651858.CD005046.pub2. [DOI] [PubMed] [Google Scholar]
- 5.Boeckxstaens GE, Annese V, des Varannes SB, Chaussade S, Costantini M, Cuttitta A, Elizalde JI, Fumagalli U, Gaudric M, Rohof WO, et al. Pneumatic dilation versus laparoscopic Heller’s myotomy for idiopathic achalasia. N Engl J Med. 2011;364:1807–1816. doi: 10.1056/NEJMoa1010502. [DOI] [PubMed] [Google Scholar]
- 6.Mikaeli J, Islami F, Malekzadeh R. Achalasia: a review of Western and Iranian experiences. World J Gastroenterol. 2009;15:5000–5009. doi: 10.3748/wjg.15.5000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Patti MG, Herbella FA. Achalasia and other esophageal motility disorders. J Gastrointest Surg. 2011;15:703–707. doi: 10.1007/s11605-011-1478-x. [DOI] [PubMed] [Google Scholar]
- 8.Wang L, Li YM, Li L. Meta-analysis of randomized and controlled treatment trials for achalasia. Dig Dis Sci. 2009;54:2303–2311. doi: 10.1007/s10620-008-0637-8. [DOI] [PubMed] [Google Scholar]
- 9.Moawad FJ, Wong RKh. Modern management of achalasia. Curr Opin Gastroenterol. 2010;26:384–388. doi: 10.1097/MOG.0b013e32833aaf4a. [DOI] [PubMed] [Google Scholar]
- 10.Gutschow CA, Töx U, Leers J, Schäfer H, Prenzel KL, Hölscher AH. Botox, dilation, or myotomy? Clinical outcome of interventional and surgical therapies for achalasia. Langenbecks Arch Surg. 2010;395:1093–1099. doi: 10.1007/s00423-010-0711-5. [DOI] [PubMed] [Google Scholar]
- 11.Inoue H, Minami H, Kaga M, Sato Y, Kudo SE. Endoscopic mucosal resection and endoscopic submucosal dissection for esophageal dysplasia and carcinoma. Gastrointest Endosc Clin N Am. 2010;20:25–34, v-vi. doi: 10.1016/j.giec.2009.08.005. [DOI] [PubMed] [Google Scholar]
- 12.Inoue H, Minami H, Kobayashi Y, Sato Y, Kaga M, Suzuki M, Satodate H, Odaka N, Itoh H, Kudo S. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy. 2010;42:265–271. doi: 10.1055/s-0029-1244080. [DOI] [PubMed] [Google Scholar]
- 13.Swanström LL, Rieder E, Dunst CM. A stepwise approach and early clinical experience in peroral endoscopic myotomy for the treatment of achalasia and esophageal motility disorders. J Am Coll Surg. 2011;213:751–756. doi: 10.1016/j.jamcollsurg.2011.09.001. [DOI] [PubMed] [Google Scholar]
- 14.Stavropoulos SN, Harris MD, Hida S, Brathwaite C, Demetriou C, Grendell J. Endoscopic submucosal myotomy for the treatment of achalasia (with video) Gastrointest Endosc. 2010;72:1309–1311. doi: 10.1016/j.gie.2010.04.016. [DOI] [PubMed] [Google Scholar]
- 15.Li H, Linghu E, Wang X. Fibrin sealant for closure of mucosal penetration at the cardia during peroral endoscopic myotomy (POEM) Endoscopy. 2012;44 Suppl 2 UCTN:E215–E216. doi: 10.1055/s-0032-1309358. [DOI] [PubMed] [Google Scholar]
- 16.Costamagna G, Marchese M, Familiari P, Tringali A, Inoue H, Perri V. Peroral endoscopic myotomy (POEM) for oesophageal achalasia: preliminary results in humans. Dig Liver Dis. 2012;44:827–832. doi: 10.1016/j.dld.2012.04.003. [DOI] [PubMed] [Google Scholar]
- 17.von Renteln D, Inoue H, Minami H, Werner YB, Pace A, Kersten JF, Much CC, Schachschal G, Mann O, Keller J, et al. Peroral endoscopic myotomy for the treatment of achalasia: a prospective single center study. Am J Gastroenterol. 2012;107:411–417. doi: 10.1038/ajg.2011.388. [DOI] [PubMed] [Google Scholar]
- 18.Zhou PH, Cai MY, Yao LQ, Zhong YS, Ren Z, Xu MD, Chen WF, Qin XY. [Peroral endoscopic myotomy for esophageal achalasia: report of 42 cases] Zhonghua Weichang Waike Zazhi. 2011;14:705–708. [PubMed] [Google Scholar]
- 19.Ren Z, Zhong Y, Zhou P, Xu M, Cai M, Li L, Shi Q, Yao L. Perioperative management and treatment for complications during and after peroral endoscopic myotomy (POEM) for esophageal achalasia (EA) (data from 119 cases) Surg Endosc. 2012;26:3267–3272. doi: 10.1007/s00464-012-2336-y. [DOI] [PubMed] [Google Scholar]
- 20.Linghu EQ, Li HK. A new endoscopic classification of achalasia. Zhonghua Qiangjing Waike Zazhi. 2011;4:8–10. [Google Scholar]
- 21.Ortega JA, Madureri V, Perez L. Endoscopic myotomy in the treatment of achalasia. Gastrointest Endosc. 1980;26:8–10. doi: 10.1016/s0016-5107(80)73249-2. [DOI] [PubMed] [Google Scholar]
- 22.Pasricha PJ, Hawari R, Ahmed I, Chen J, Cotton PB, Hawes RH, Kalloo AN, Kantsevoy SV, Gostout CJ. Submucosal endoscopic esophageal myotomy: a novel experimental approach for the treatment of achalasia. Endoscopy. 2007;39:761–764. doi: 10.1055/s-2007-966764. [DOI] [PubMed] [Google Scholar]
- 23.Pandolfino JE, Kwiatek MA, Nealis T, Bulsiewicz W, Post J, Kahrilas PJ. Achalasia: a new clinically relevant classification by high-resolution manometry. Gastroenterology. 2008;135:1526–1533. doi: 10.1053/j.gastro.2008.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pratap N, Kalapala R, Darisetty S, Joshi N, Ramchandani M, Banerjee R, Lakhtakia S, Gupta R, Tandan M, Rao GV, et al. Achalasia cardia subtyping by high-resolution manometry predicts the therapeutic outcome of pneumatic balloon dilatation. J Neurogastroenterol Motil. 2011;17:48–53. doi: 10.5056/jnm.2011.17.1.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Roman S, Zerbib F, Quenehervé L, Clermidy H, Varannes SB, Mion F. The Chicago classification for achalasia in a French multicentric cohort. Dig Liver Dis. 2012;44:976–980. doi: 10.1016/j.dld.2012.07.019. [DOI] [PubMed] [Google Scholar]


