1. Introduction
Alcohol use and especially misuse substantially contributes to global rates of premature deaths and disease (World Health Assembly 2005). It is estimated that alcohol use is associated with about 4% of deaths, and that alcohol use is one of the most avoidable risk factors for death. The financial burden associated with alcohol misuse in the US is estimated to be $837 per head in the US, with the poor disproportionately sharing the burden of those costs (Rehm, Mathers, & Filmore 2009).
Harmful levels of alcohol use have been associated with increased risk for injury, increased risk for alcohol impaired driving, and poorer psychosocial and health outcomes (Brewer & Swahn 2005; Quinlan, Brewer et al. 2005; Marczinski, Combs et al. 2007; Standerwick, Davies, Tucker, & Sheron,. 2007). These negative consequences are affected not only by the amount of alcohol use, but also by the pattern of alcohol use (Plant, Miller, Thornton, Plant, & Bloomfield, 2000). Of particular concern is binge drinking, which is defined as consuming four or more drinks for females or five or more drinks for males on an occasion. Binge drinking has also been cited as a significant risk factor for sexually transmitted disease, sexual assaults and unplanned pregnancies (Standerwick et al., 2007).
Marijuana is the most frequently reported illicit drug and is the most commonly used illicit drug in developed countries (Degenhardt, Hall, & Lynskey. 2001a). Conjoint use of alcohol and marijuana is frequently found with impaired driving (Soderstrom, Dischinger, Kerns, & Trifills, 1995; Longo, Hunter, Lokan, White, & White, 2000) and conjoint use is associated with injury and other negative consequences as well as more binge alcohol use (Woolard, Baird, Mello, Nirenberg, & Longabaugh, 2009). Conjoint alcohol and marijuana use increases the likelihood of alcohol abuse, with the odds increasing as levels of marijuana use increase (Degenhardt, Hall, & Lynskey 2001b).
1.1 The emergency department
Visits to the emergency department (ED) are often associated with substance use. In 2007 there were over 116 million visits to US EDs, and it is estimated that nearly two million of these visits were for reasons directly related to alcohol use in association with drug use, with marijuana being a frequent drug used in association with alcohol (Substance Abuse and Mental Health Services Administration and Office of Applied Studies 2010). Injured and uninjured ED patients experience high rates of past and future alcohol related injuries (Cherpitel 1998), with conjoint alcohol and marijuana use found in many injured ED patients and motor vehicle crash fatalities (Soderstrom, Dischinger, Kerns & Trifills, 1995; Longo, et al., 2000).
The ED is more likely than any other health care setting to deal with the immediate negative health consequences, such as injury associated with substance misuse, and the Substance Abuse Task Force of the Society for Academic Emergency Medicine (SAEM) has advocated that EDs should provide a system of referral to treatment for those seeking help with alcohol misuse problems (D'Onofrio & Bernstein, 1998a; D'Onofrio & Bernstein,, 1998b). Despite this position by SAEM, a mechanism for achieving this important aim has yet to be uniformly applied across EDs.
Brief therapeutic interventions (BI) are increasingly utilized to address substance use problems of individuals who present in a variety of health care settings. However, exactly what constitutes a BI has been a source of some debate. The label BI has been applied to interventions which can differ in duration, approach, and content, and can be delivered to disparate client groups such as treatment seekers or non-treatment seekers, dependent or non-dependent drinkers, and those with other health problems (Smith, Hodgson, Bridgeman & Shepherd, 2003). While BI can be based on several different therapeutic approaches, motivational interviewing techniques have become common (Dunn, Deroo, & Rivara, 2001).
Brief interventions for alcohol use have been shown to decrease alcohol consumption when delivered in a variety of settings, including the ED and primary care settings. Studies in of BI in primary care settings report intervention related reductions of alcohol consumption on average of 13–34% compared with control groups (Whitlock, et al. 2004). The Cochrane library’s drugs and alcohol group reviewed 29 controlled trials; 24 from primary care and 5 from emergency departments. There were more than 7,000 participants in these studies who drank on average over 30 drinks per week on entry. After one year or more, people in the BI group drank about 4 drinks less per week than controls (Kaner, et al 2009). Even with this modest effect size, another analysis concluded that BI for alcohol delivered in the primary care setting could reduce mortality rates among problem drinkers by 23–26% (Cuijpers, Riper, & Lemmers, 2004).
Compared to other interventions, the modest time and resource investment needed (Smith et al. 2003) is considered strength. Even in a busy ED it is feasible to implement a BI during a visit for treatment of an acute medical condition, and BI delivered in the ED for alcohol use has been shown to reduce negative consequences of use (such as injury), although often in the absence of a significant corresponding reduction in alcohol consumption (Longabaugh et al., 2001; Nilsen et al., 2008; Havard, Shakeshaft, & Sanson-Fischer, 2008).
Brief Intervention has recently been tested specifically for cannabis use and demonstrated potential for reducing use and related risk and harm when compared with untreated controls (Benyamina, Lecacheux, Blecha, Reynaud, & Lukasiewcz, 2008; McRae, & Brady 2003; Nordstrom & Levin, 2007). While not as effective as multi-session cognitive-behavioral treatment, BI is more cost-effective (Copeland & Swift, 2009; Denis, Lavie, Fatseas, & Auriacombe, 2006, McRae & Brady, 2003, Martin & Copeland, 2008, McCambridge, Slym, & Strang, 2008 ; Walker, Roffman, Stephens, Berghuis, & Wakana, 2006). Studies of BI for cannabis have relied on a variety of new and old intervention designs (e.g., in-person, written materials, multi-media approaches) (Lang, Engelander, & Brooke, 2000; Stephens, Roffman, Fearer, Williams, & Burke, 2007). Most studies of BI for marijuana have been conducted outside the ED setting and have shown BI to be effective (Fischer et al. (2012). There has been only one smalls scale research study demonstrating effectiveness of a BI delivered in the ED to increase abstinence from marijuana and reduction of days of marijuana use among adolescent and young adult ED patients (Bernstein et al. 2009).
While alcohol or marijuana use has been subject to BI, interventions focused on both have not been published. Previous research conducted by this group of investigators with hazardous drinkers who visited the ED with an injury showed that almost half (47%) were also marijuana users (Woolard, Nirenberg, & Longabaugh, 2002). ED patients who admit both marijuana and alcohol use report more negative consequences of use such as injuries, but they also report high levels of motivation to change (Woolard, et al., 2009). While there are many users of alcohol who use marijuana, a BI designed for both alcohol and marijuana use has not been explored in a research trial.
1.3 Goals of this investigation
Project Reduce, a randomized controlled trial funded by the National Institute on Alcohol Abuse and Alcoholism, was conducted to evaluate the effectiveness of a two session brief face-to-face brief intervention delivered to ED patients who reported both alcohol and marijuana use (the BI group) in comparison to patients who received only an assessment and standard emergency medical care (the SC group). It was hypothesized that BI in comparison to the SC group would reduce alcohol and marijuana use three and 12-months after being enrolled in the study, and that a corresponding difference in the reduction of alcohol and marijuana negative consequences would also be found. The research hypotheses concerning the anticipated results at three and 12 month post recruitment were:
The intervention group (receiving BI) would reduce alcohol use and binge drinking significantly more than the control group (receiving standard ED care; SC) at three and twelve-months post randomization.
The BI group would reduce marijuana use significantly more than the SC group at three and twelve-months post randomization.
The BI group would reduce conjoint alcohol and marijuana use significantly more than the SC group at three and twelve-months post randomization.
The BI group would reduce psychosocial negative consequences and injuries associated with alcohol, marijuana and conjoint use significantly more than the SC group at 12-months post randomization.
2. Methods
2.1 Study design
The study site was the emergency department (ED) at Rhode Island Hospital in Providence, Rhode Island. This is an urban level I trauma center ED that has over 100,000 annual patient visits. Trained research assistants (RAs) were employed in the ED to recruit, consent and conduct the baseline assessment survey with participants. Screening and study recruitment took place during the day and evening shifts across all days of the week. The RAs screened potentially eligible ED patients for study inclusion and eligible participants signed a written consent to participate in the study. Participants were informed that the study would offer assessment and intervention for alcohol and marijuana users, but the random assignment was not conducted until after the baseline assessment. Following the baseline assessment the participant was randomized to receive either the standard care (SC) or brief intervention (BI). Participants were not informed of of the hypotheses being tested in this study.
Each participant was allocated a study identification number and closed envelopes containing the randomized assignment of that participant, which was opened by the RA after the participant had completed the baseline assessment. If the participant randomized into the BI group the RA contacted the interventionist. After the RA conducted a ‘warm handover (i.e. introduced the interventionist to the participant), the interventionist conducted the BI. After completing the first BI, the interventionist scheduled the booster session, within a two-week period of the first BI. The same interventionist conducted the baseline and second BI session.
If the participant was in the SC group the RA scheduled the follow-up assessment appointments. In the standard care condition participants received routine emergency care for their presenting medical complaint during and after completing the baseline assessment. Participants assigned to the BI condition also received standard emergency medical care. All study participants were offered information on local treatment resources for substance misuse either following the BI or after the baseline assessment for the SC group. Follow up assessments were conducted by telephone at three and twelve months post recruitment by RAs blinded as to the patient’s original treatment condition. The baseline and follow-up assessments each took between 30–45 minutes to administer. Participants were compensated $25.00 for baseline and three month assessments and $50.00 for twelve month assessments. This study was approved by the Institutional Review Board at Rhode Island hospital and a Certificate of Confidentiality was obtained from NIAAA. This study has been registered with Clinical Trials.gov.
2.2 Participants
Patients who were not critically ill or injured were first screened for alcohol and marijuana use using the Wellness questionnaire (see section 2.3). Patients who were 18 or older and reported alcohol use in the prior month and marijuana uses in the prior year were invited to participate. Patients were excluded from study recruitment if they: were admitted to the hospital; in treatment for substance use or psychiatric disorders; were not English speaking; in police custody; unable to consent or too medically unstable to participate in the research.
2.3 Measures
Wellness Questionnaire (Baird, & Harrington, 2004)
This ten item screening instrument was administered to ED patients to determine potential study eligibility. Patients were asked general questions about their health with questions about quantity and frequency of alcohol (over the past month) and frequency of marijuana use (over the past year).
Demographic Questionnaire
Participants were asked questions about age, gender, ethnicity, race, marital relationship, education and employment. Participants were also asked about their reason for the ED visit, coded as a visit for an injury or illness.
Alcohol Use Disorders Inventory Test (Saunders, Aasland, Babor, De La Fuente, & Grant, 1993)
This is a ten question self-report instrument of frequency of alcohol use, binge use and experience of alcohol related negative consequences. AUDIT scores of 8 or greater are indicative of hazardous alcohol use and the probability of alcohol abuse and dependency increases with scores above 16. The AUDIT was administered at baseline (AUDIT scores range from 0 to 40) to describe the severity of alcohol use among the participants. The AUDIT has established internal consistency, alpha = .80 and can reliably distinguish participants with positive and negative alcohol drinking histories (Saunders et al., 1993). Cherpitel (1995) reported that, in ED populations, an AUDIT cutoff score of 8 produces 85% sensitivity and 88% specificity for hazardous drinking and 83% sensitivity and 89% specificity for alcohol dependence. The AUDIT was administered at the baseline to determine the alcohol severity level of this sample
Alcohol, Marijuana and Drug Use Index (AMD) (Nirenberg, & Lee, 2003)
The AMD has 7 questions about the past 30 days use of alcohol, marijuana and other drugs. This included frequency and quantity questions, including binge alcohol questions (4 or more for females, 5 or more for males). Since a quantity of marijuana that would define excessive use could not be obtained from the literature, we asked participants to report their subjective level of being ‘high’ on the days that they used marijuana. For the data analysis, being high was defined as the report of being “somewhat high” or “very high” on a day when marijuana was used. The AMD was administered at the baseline, three and twelve month assessments. Five variables were created from the AMD; alcohol use days, binge drinking days, marijuana use days, marijuana high days, and conjoint marijuana and alcohol use days. Cronbach’s alpha was calculated on these five variables to determine the levels of internal consistency of these items as a scale. The calculated alpha of .74 shows that this is an acceptable scale.
Noteworthy Index of Problems (Longabaugh, 2003) (NIP)
The NIP was developed and adapted from the Drinkers Inventory of Consequences Forcehimes, Tonigan, Miller, Kenna, & Baer, 2007). The NIP asks about the frequency of occurrence of 19 events (e.g., job loss) related to either alcohol use, marijuana use, or conjoint use, in the past three months. Three summary variables were created: 1.alcohol negative consequences, 2. Marijuana negative consequences, and 3. conjoint use related negative consequences. Cronbach’s alpha as a measure of internal consistency was calculated on these summary variables. The calculated values (alcohol negative consequences = .93, marijuana = .92, conjoint = .89), showed excellent reliability. The NIP was administered at the baseline, three and twelve month assessments.
Injury Behavior Checklist (IBC)
The IBC is an adaptation of an injury checklist developed for children and adolescents (Speltz, Gonzales, Sulzbacker, & Quan, 1990) and validated on an ED patient population The original injury checklist had acceptable reliability with a Cronbach’s alpha of .87 The IBC asks participants how often each of 17 injuries has occurred in the past 12 months. If a participant affirms that an injury had happened, subsequent questions are asked about the use of alcohol, marijuana or both prior to their injury are asked. Three variables were created; total injuries, total alcohol-related injuries and total marijuana-related injuries. Conjoint use related injury was reported too infrequently to be used in the analysis. The IBC was administered at the baseline and twelve month assessments.
2.4 Brief Interventions
The BIs were conducted by trained interventionists who held PhD or Masters Degrees in mental health related disciplines and completed an initial 2 week course in motivational interviewing (MI). Those randomized to BI were counseled based on the principles of MI as described by Miller & Rollnick (2002) and the MATCH MET treatment manual (Miller, Zweben, DiClemente, & Rychtarik 1995). Participants received two BI sessions. The model of delivering two sessions of BI was decided based on the REIS study (Longabaugh et al., 2001) which showed that only participants who received two sessions of BI reduced alcohol related negative consequences and injuries. The first BI session lasted between 20 to 60 minutes, and the second 15 to 40 minutes.
The goal of the first BI session was to engage the participant in reflection upon the pros and cons of alcohol and marijuana use. The intervention incorporated elements of MI used in BIs with problem drinkers (Bien, Miller, Miller, Boroughs, 1993). These include: l) feedback; 2) emphasis on personal responsibility for change; 4) advice with permission, 4) a menu of alternative change options; 4) an empathic interventionist style; and 5) fostering patient self-efficacy. The interventionist provided direct feedback concerning the participant’s alcohol and marijuana use compared to community norms. The participant and interventionist developed a change plan that addressed changes the participant wanted to make, usually focused on reduction of substance use. If the participant was not ready to change substance use the interventionist worked with the participant to increase motivation for change. The interventionists discussed with participants the pros and cons of alcohol and marijuana use and also explored their conjoint use, and the effect that conjoint use had on the reported pros and cons. For example if a patient reported that alcohol made him aggressive, the interventionist would probe to find out if aggression was mitigated or intensified if marijuana had also been used. The focus of the second BI session was to review and reinforce the change plan for those who had one, or to increase motivation for change and create a change plan with those who had not made a change plan in the first session.
2.4.1 Treatment fidelity
All clinical interventionists were trained and certified in MI by a MI trainer, who was a member of the motivational interviewers’ network of trainers (MINT). The weekly clinical supervision sessions with the interventionists were conducted by a licensed clinical psychologist with MI expertise. BI sessions were audio recorded and prior to conducting these weekly meetings the clinical supervisor reviewed a random sample of these tapes. No formal scoring of these tapes was undertaken. However, at these meetings the tape reviews were discussed. Discussions focused on avoiding drift from the tenets of MI, the clinical issues that needed to be addressed in the booster session, and any performance problems.
2.5 Data analysis
2.5.1 Sample size and data management
Sample size was calculated using the effect size (d = 0.28–0.30) from a previous randomized clinical trial at our institution (Longabaugh, et al. 2001). Using Cohen’s procedure for calculating sample size, with a power of .80 and an alpha of .05, and with an estimated attrition rate of 20%, 260 participants were recruited to each treatment condition to enable the main study hypotheses to be tested (Lipsey, 1990). Data were initially collected on paper, then using double data entry to assure accuracy, transferred to an electronic database (Illume 2.2, DatStat, Seattle, WA). The database was electronically checked for inconsistent entries and transferred to SAS version 9.1 (SAS Institute, Inc., Cary, NC) for analysis.
Prior to data analyses, the distribution of raw scores was assessed and transformations of data were conducted when appropriate. The untransformed data is reported in the appropriate tables. A mixed model procedure was used to handle clustering of data and to model variables across the three time points of interest (baseline, three and twelve-months). The variation in individuals within a treatment condition was modeled as a random effect. Means, standard deviations and/or confidence intervals (CI) at the 95% significance level are reported.
3. Results
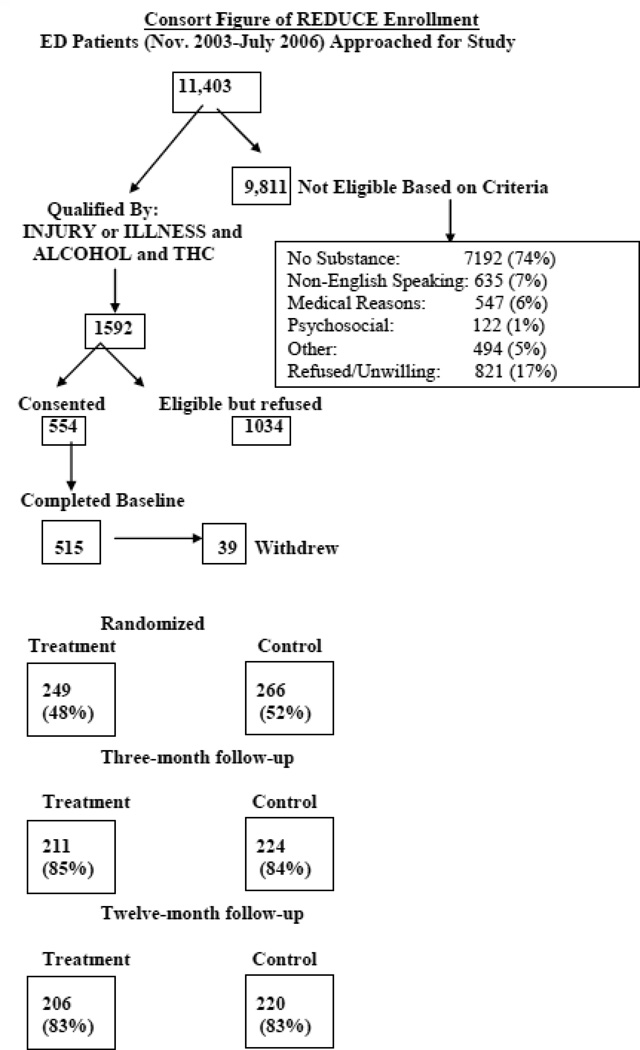
During the time that the study was conducted in the ED, 11,403 patients were approached to be screened for eligibility. Of these patients 1,592 (13.6 %) met eligibility criteria; admitting use of both alcohol in the last month and marijuana use in the past year. As shown on the CONSORT diagram, (Figure 1), 1034 were eligible but refused to participate and 554 agreed to participate. During the consent or assessment process 39 participants withdrew and 515 completed the baseline assessment; this represents 33% of eligible patients agreeing to participate and being randomized into a treatment condition. During the study, 85% of all recruited patients (N=435) participated in the three-month and 83% (N=426) in the 12 month follow-up. There was no differential attrition across treatment groups (SC N=224 at three-month and 211 at 12-month assessments, BI N=220 at three-month and 206 at 12-month assessments). Fifty-one percent of participants assigned to BI returned for the second BI session. Intent to treat analyses was conducted using the assigned treatment condition as the independent variable irrespective of the number of BI sessions received.
FIG. 1.
3.1 Demographics
There were no significant differences in baseline characteristics by treatment group assignment (see Table 1). Across the sample 68% were White and 17% were Hispanic or Latino. There were approximately equal proportions of uninjured (52%) and injured (48%) in the SC and BI groups. Using the AUDIT as a measure of alcohol use severity, there was no significant difference in baseline AUDIT scores between the SC (M = 11.15) and BI groups (M = 10.70). However, these values indicate that both the SC and BI groups were on average using alcohol at harmful levels, as defined by AUDIT scores ≥8 for males and ≥ 6 for females. At baseline there were no significant differences between the SC and BI groups on measures of past 30 days alcohol and marijuana use, conjoint alcohol/marijuana use, binge use of alcohol and marijuana, negative consequences and injuries related to alcohol or marijuana use (Tables 2).
Table 1.
Demographic characteristics
| Demographics | SC | BI | Statistic |
|---|---|---|---|
| Age | M = 28.3 (SD=9.1) | M = 28.4 (SD=8.9) | t (509) = −0.15; p =.88 |
| Gender | Female = 16% | Female = 17% | Χ2 (1) = 0.33; p =.53 |
| Education level in years | M = 12.3 (SD= 2.1) | M = 12.5 (SD= 2.4) | t (509) = −1.03; p =.31 |
| AUDIT total | M = 11.15 (SD = 1.30) | M = 10.7 (SD = 1.51) | t (509) = 0.84; p =.40 |
Table 2.
Baseline, three and 12-month alcohol and marijuana use and negative consequences.
| Outcome | Baseline | Three months | Twelve Months | |||
|---|---|---|---|---|---|---|
| SC (N = 260) |
BI (N = 249) |
SC (N = 224) |
BI (N= 211) |
SC (N = 220) |
BI (N = 206) |
|
| Days alcohol | M = 8.7 | M = 7.8 | M =6.05 | M =4.58 | M = 5.90 | M =4.08 |
| use in past 30 | 95% CI: 7.8- | 95% CI: | 95% CI:5.11- | 95% CI: | 95% CI: 4.88- | 95% CI: |
| days (AMD) | 9.6 | 6.84–8.76 | 7.08 | 3.69–5.57 | 7.02 | 3.24–5.02 |
| Days THC | M = 12.4 | M = 12.8 | M =10.6 | M =10.7 | M=10.0 | M =9.4 |
| use in past 30 | 95% CI: | 95% CI: | 95% CI:9.03- | 95% CI: | 95% CI: 8.43- | 95% CI: |
| days (AMD) | 10.98–13.82 | 11.35–14.25 | 12.17 | 9.07–12.33 | 11.57 | 7.78–11.02 |
| Days conjoint | M = 6.2 | M = 6.5 | M =2.69 | M =2.01 | M =2.16 | M = 1.25 |
| alcohol and | 95% CI: 5.41- | 95% CI: | 95% CI: 1.90- | 95% CI : | 95% CI : | 95% CI : |
| THC use in | 6.99 | 5.66–7.34 | 3.61 | 1.25–2.96 | 1.56–2.86 | 0.81–1.54 |
| past 30 days | ||||||
| (AMD) | ||||||
| Days alcohol | M = 3.4 | M = 3.1 | M = 1.28 | M = 0.64 | M = 1.77 | M = 0.72 |
| binge use in | 95% CI: 2.88- | 95% CI: | 95% CI:0.82- | 95% CI: | 95% CI: 1.19- | 95% CI: |
| past 30 days | 3.92 | 2.54–3.66 | 1.82 | 0.29–1.12 | 1.57 | 0.36–1.21 |
| (AMD) | ||||||
| Days THC | M = 4.9 | M = 5.3 | M =3.50 | M = 4.75 | M =3.61 | M 3.24 |
| heavy use in | 95% CI: 4.19- | 95% CI:4.45- | 95% CI: 2.34- | 95% CI: | 95% CI:2.46- | 95% CI: |
| past 30 days | 5.61 | 6.15 | 4.84 | 3.42–6.30 | 4.97 | 2.16–4.54 |
| (AMD) | ||||||
| Total negative | M = 3.3 | M = 3.1 | M =2.8 | M =2.5 | M = 2.3 | M =2.1 |
| consequences | 95% CI: 3.05- | 95% CI: | 95% CI: 2.51- | 95% CI: | 95% CI: 2.01- | 95% CI: |
| (NIP) | 3.54 | 2.83–3.37 | 3.09 | 2.18–2.82 | 2.59 | 1.80–2.40 |
| Alcohol | M = 2.5 | M = 2.4 | M =2.1 | M =1.8 | M = 1.9 | M =1.6 |
| negative | 95% CI: 2.30- | 95% CI: | 95% CI : | 95% CI : | 95% CI: 1.65- | 95% CI: |
| consequences | 2.70 | 2.16–2.64 | 1.85–2.35 | 1.53–2.07 | 2.15 | 1.35–1.85 |
| (NIP) | ||||||
| THC negative | M = 1.7 | M = 1.6 | M = 1.3 | M =1.4 | M =0.97 | M =1.0 |
| consequences | 95% CI: 1.51- | 95% CI: | 95% CI: 1.09- | 95% CI: | 95% CI: 0.78- | 95% CI: |
| (NIP) | 1.89 | 1.39–1.81 | 1.51 | 1.17–1.63 | 1.16 | 0.78–1.22 |
3.2 Alcohol and marijuana use
There were significant changes across groups in substance use, negative consequences and injuries over the study (see Table 2). As compared to the baseline, past 30 days alcohol use, alcohol binge use, marijuana and conjoint use decreased from baseline to the three and twelve month assessments for both groups. To determine the effects of group assignment (2 levels), time (3 levels) and the interaction between group assignment and time we conducted a repeated measures analysis using a generalized linear model. We examined each group’s relative change over time. For each consumption outcome the time effect was significant.
As can be seen in Tables 2 and 3, the BI group had a significantly lower binge use of alcohol at three (BI M =0.64, SC M = 1.28) and twelve months (BI M = 0.72, SC M = 1.77). Compared to baseline levels, these reductions associated with BI would be expected to reduce binge drinking days by 2.4 per month, or 29 days a year; the SC group would reduce by 1.7 days per month, or 20 days a year. This is a 74% reduction from baseline for the BI group and a 50% reduction for the SC group. Using an arcsine transformation, this difference in the reduction between the groups is a moderate effect size (d= 0.52). The BI group also had a significantly greater reduction in conjoint alcohol and marijuana use days at three (BI M = 2.01, SC M =2.6) and at twelve months (BI M = 1.25, SC M = 2.16). This results in approximately 5 fewer conjoint use days per month for the BI group, or 60 days a year; and 1.25 fewer conjoint use days per month, or 15 days per year for the SC group. This is an 81% reduction from baseline for the BI group and a 33% for the SC group. Using an arcsine transformation, this difference in reduction between the groups is a large effect size (d= 1.12).
Table 3.
Modeling changes in substance use and negative consequences baseline to three and 12-months post recruitment
| Measure | Effect | DF | Statistic |
|---|---|---|---|
| Days alcohol use in past | Group | 1, 397 | F=6.12; p = .01 |
| 30 days (AMD)* | Time | 2,798 | F = 27.37; p < .001 |
| Group*Time | 2,798 | F = 2.67; p = .07 | |
| Days THC use in past 30 | Group | 1, 397 | F=0.12; p = .73 |
| days (AMD)* | Time | 2,798 | F = 13.36; p < .001 |
| Group*Time | 2,798 | F = 0.18; p = .83 | |
| Days conjoint alcohol and | Group | 1, 331 | F=7.77; p = .01 |
| THC use in past 30 days | Time | 2,662 | F = 10.77; p < .001 |
| (AMD)* | Group*Time | 2,662 | F = 3.78; p = .02 |
| Days alcohol binge in | Group | 1, 397 | F=6.33; p = .01 |
| past 30 days (AMD)* | Time | 2,798 | F = 9.91; p < .001 |
| Group*Time | 2,798 | F = 3.07; p = .05 | |
| Days THC heavy use in | Group | 1, 257 | F=0.01; p = .93 |
| past 30 days (AMD)* | Time | 2,514 | F = 9.48; p < .001 |
| Group*Time | 2,514 | F = 1.21; p = .30 | |
| Total negative | Group | 1,348 | F=0.70; p = .40 |
| consequences (NIP)* | Time | 2,696 | F = 39.99; p < .001 |
| Group*Time | 2,698 | F = 0.14; p = .86 | |
| Alcohol negative | Group | 1,348 | F=2.18; p = .14 |
| consequences (NIP)* | Time | 2,696 | F = 32.82; p < .001 |
| Group*Time | 2,698 | F = 0.25; p = .77 | |
| THC negative | Group | 1,348 | F=0.24; p = .62 |
| consequences (NIP)* | Time | 2,696 | F = 28.67; p < .001 |
| Group*Time | 2,698 | F = 0.49; p = .61 |
square root transformation
Although the difference in reduction in days of any alcohol use between the two groups (a mean reduction of 3.7 for BI and 2.1 for SC in drinking days per month) did not reach significance (p = .07), it is a trend that is worth noting.
3.3 Negative psychosocial consequences
The occurrence of negative psychosocial events that could be associated with alcohol and/or marijuana use was measured at baseline, and at the three and twelve follow up using the NIP. As can be seen from Tables 3 and 4, overall negative consequences, and negative consequences associated with alcohol and marijuana use significantly decreased from baseline to the three month follow up, and from the three to twelve month follow up. However, there was no significant difference between BI and SC groups (Total negative consequences Group* Time F (2,698) =0.14; p = .86; Alcohol negative consequences Group * Time F(2,698) = 0.25; p = .77; THC negative consequences Group * Time F(2,698) = 0.49; p = .61).
3.4 Injuries
Both the SC and BI groups significantly decreased their report of total injuries measured by the IBC (SC baseline M = 2.7; SC 12 months = M =1.4; BI baseline M = 2.9; BI 12 months M = 1.7) and injuries related to alcohol (SC baseline M = 2.1; SC 12 months M =1.4; BI baseline M = 2.6; BI 12 months M = 1.8) and marijuana use over time (SC baseline M = 2.5; SC 12 months M =1.5; BI baseline M = 2.8; BI 12 months M = 1.7) but these reductions did not significantly differ between the groups.
4. Discussion
There were significant reductions in the pattern of substance use within and between the BI and SC groups over time. There were significant reductions in both groups from baseline to 12 months in all measures of substance use, negative consequences and injuries. There was no differential group by time effects for days of alcohol use, days of marijuana use, and days of heavy marijuana use, negative consequences associated with alcohol and marijuana use or injuries. However, the BI group had significantly greater reduction in binge alcohol days and conjoint alcohol, and marijuana use days. It was of interest that days of alcohol use, while not significant, did show a trend toward the BI group having greater reductions. It appears that overall the study population benefited from the research protocol, as all measures of substance use showed significant reductions over time.
Changes in both treatment and control groups have been reported in other ED studies of BI. Their cause has been hypothesized as either assessment reactivity or regression to the mean (Clifford, Maisto, & David, 2007). Studies focusing on injured ED patients have also speculated that having a substance-related injury might also be a factor in reductions observed. The present study does not support this explanation, as both injured and ill patients were included in the sample, and presenting condition did not moderate responsiveness to treatment condition. More recent studies of BI in the ED have included a minimal assessment group in addition to the assessment and intervention groups. These studies will help determine if the cause of improvements seen in the ED study populations are the result of assessment reactivity which can occur when the assessment serves as an effective counseling treatment.
The reduction in days of binge alcohol use for the BI group is encouraging and may be of clinical significance. At the 12-month assessment, on average the SC group reported 1.77 binge use days in a 30 day period and the BI group reported an average of 0.72 binge use days in the past 30 day period. This could be an important reduction annualizing to 29 less binge episode days per year for the BI group. As binge drinking is associated with many risk behaviors (e.g. aggression, risky sex), the BI could significantly reduce harm for this population.
The BI group also reduced conjoint marijuana and alcohol use days more than the SC group. This reduction annualized to approximately 60 less days of conjoint use each year for the BI group. Conjoint use of alcohol and marijuana has been associated with increased binge drinking, injury, risk behaviors and negative consequences (Woolard, et al. 2002). In this study there was no differential reduction in negative consequences or injuries with our Reduce BI. Many ED studies have reported that BI reduces negative consequences of alcohol without reducing the amount of alcohol use.(Nilsen, et al., 2008). A few ED studies have found reduced alcohol consumption with BI and others have found no effects of BI on either alcohol use or alcohol related negative consequences (D'Onofrio, Pantalon et al. 2008). We theorized a causal sequence, changes in substance use first and subsequent changes in consequences. While we showed reductions in alcohol and marijuana consequences in the entire study population over time, we did not demonstrate these reductions in the BI group to a greater extent than in the SC group. It may be that the further reductions in substance use pattern, alcohol binge and conjoint use, that we found with our Reduce BI would be associated with future reductions in negative consequences and injury over a longer time frame (beyond 12 months). One year follow up may be too short a time to detect small but important changes in negative consequences and injuries. One criticism of studies of BI has been this lack of long term follow up. Perhaps longer follow up to 2 years would demonstrate reductions in consequences in the Reduce BI group.
The BI was associated with a specific treatment effect on binge drinking and conjoint use of marijuana and alcohol with a trend toward reduction in alcohol use, but no reduction in measures of marijuana use. Given the client-centered non-directional approach of BI, the actual change plan was chosen by the participant. It may have been that participants considered binge drinking more problematic and focused their efforts on reducing this behavior. Similarly, it may be that social and peer support for the participant favor changing binge drinking rather than moderating overall levels of alcohol or marijuana use. Conjoint alcohol and marijuana use may have been reduced because of its association with binge drinking. The anecdotal reports from interventionists suggest that participants were more ready to discuss changing binge drinking than moderating overall alcohol or marijuana use. Indeed, there was frequent anecdotal reporting by the interventionists that participants would be able to list the cons of binge drinking and conjoint use but had more difficulty in reporting the cons of moderate alcohol or marijuana use.
5. Limitations
As with many studies that are conducted on a non-treatment seeking population, the high participant refusal rate (67%) among ED patients limits the generalizability of the results. No data are available concerning those who refused to participate. Hence whether those that refused are a distinct group from the studied population is unknown. We speculate that those refusing could be less motivated to change behavior than the group studied. A daunting challenge for BI in research and clinical practice is to find an avenue for enlisting the participation of patients who misuse substances placing themselves at risk, when they refuse intervention. Our results can only be applied to those ED patients who admit alcohol and marijuana use and accept an intervention to respond to questions about their alcohol and marijuana use and participate in the BI sessions.
In contrast to our earlier REIS study (Longabaugh et al., 2001) which had 67% of patients return for their booster session, only 51% of participants in the BI group returned for the booster session in the present study. We used an intention to treat model in our data analysis, and since not all BI participants received the booster session, this may have impacted our findings, resulting in an underestimation of the potential treatment effect. If more participants had 2 sessions, this may have changed the direction of our findings by increasing the BI effects on the negative consequences and injuries outcomes. A challenge for ED practice which was experienced in this study as well, is improving patient attendance at follow up referral. The lack of a formal rating of the tapes of the BI session is a limitation. This data would have enabled us to show the consistency between interventionists in treatment fidelity.
The data collected were self-reported, which is subject to potential bias by poor recall and the desire to conform to perceived expectations. However in general self-reported data has been accepted in alcohol studies, as self-report has been validated in prior studies (Hesselbrock, Babor, Hesselbrock, Meyer, & Workman, 1983). In particular, interventions have not been found to be associated with a bias toward under reporting of alcohol use (Babor, Stephens, & Marlatt, 1987).
In interpreting our findings, it should be noted that we studied an ED population in a particular region of the country where both alcohol and marijuana are readily available. Use of marijuana varies by state and city, and the ED patients recruited into this study may have more marijuana users than other EDs. Our study also excluded critically ill and injured patients and those requiring hospital admissions, many of whom may have more profound substance use problems.
6. Conclusion
Irrespective of treatment condition participants showed substantial reductions in all alcohol and marijuana consumption variables, as well as negative consequences attributed to alcohol and THC. Reductions observed from baseline to 3 months were sustained over the 12 month follow up period. BI had an added incremental sustained effect only on frequency of binge drinking and conjoint alcohol and marijuana use. These two variables were primary targets of the BI intervention and it is encouraging that these showed the differential effects of receiving the BI. It is disappointing though those reductions in these high risk substance use behaviors did not result in longer term treatment-related reductions in negative consequences or injuries. This may be attributable to measurement insensitivity and/or insufficient time at risk for differential consequences to emerge, or the limited effect of the BI in these areas.
Identifying high-risk patients in the ED by asking them about their alcohol and marijuana use and offering BI should be encouraged. A substantial number will admit alcohol and marijuana use and a third of these are open to receiving a BI. If the REDUCE protocol were translated into practice in the study ED, 4 to 5 patients who do not presently get counseling would be counseled for their substance misuse daily. Irrespective of whether they received a BI, patients receiving assessment could be expected to report sustained reductions in substance use and consequences a year later. If they received BI they would also report even further sustained reductions in days of binge drinking and conjoint alcohol and THC use, two high risk behaviors.
Acknowledgments
Role of Funding Sources
This study was supported by grant funding from NIAAA (1R01AA13709-01A1). NIAAA had no direct involvement in the study design, collection of data, analysis and interpretation of data, writing of this report, or in the decision to submit the paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Babor T, Stephens R, Marlatt G. Verbal report methods in clinical research on alcoholism: Response bias and its minimization. Journal of Studies on Alcohol. 1987;48:410–424. doi: 10.15288/jsa.1987.48.410. [DOI] [PubMed] [Google Scholar]
- Baird J, Harrington M. Wellness Questionnaire: Unpublished Survey. 2004 [Google Scholar]
- Benyamina A, Lecacheux M, Blecha L, Reynaud M, Lukasiewcz M. Pharmacotherapy and psychotherapy in cannabis withdrawal and dependence. Expert Review of Neurotherapeutics. 2008;8:479–491. doi: 10.1586/14737175.8.3.479. [DOI] [PubMed] [Google Scholar]
- Bernstein E, Edwards E, Dorfman D, Heeren T, Bliss C, Bernstein J. Screening and brief intervention to reduce marijuana use among youth and young adults in a pediatric emergency department. Academic Emergency Medicine. 2009;16(11):1174–1185. doi: 10.1111/j.1553-2712.2009.00490.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bien TH, Miller WR, Boroughs JM. Motivational interviewing with alcohol outpatients. Behavioural and Cognitive Psychotherapy. 1993;21(4):347–356. [Google Scholar]
- Brewer RD, Swahn MH. Binge drinking and violence. Jama. 2005;294(5):616–618. doi: 10.1001/jama.294.5.616. [DOI] [PubMed] [Google Scholar]
- Cherpitel CJ. Analysis of cut points for screening instruments for alcohol problems in the emergency room. Journal of Studies On Alcohol. 1995;56(6):695–700. doi: 10.15288/jsa.1995.56.695. [DOI] [PubMed] [Google Scholar]
- Cherpitel CJ. Drinking patterns and problems and drinking in the injury event: an analysis of emergency room patients by ethnicity. Drug Alcohol Rev. 1998;17(4):423–431. doi: 10.1080/09595239800187261. [DOI] [PubMed] [Google Scholar]
- Clifford PR, Maisto SA, David CM. Alcohol treatment research assessment exposure subject reactivity effects: part I. Alcohol use and related consequences. Journal of Studies on Alcohol and Drugs. 2007;68(4):519–528. doi: 10.15288/jsad.2007.68.519. [DOI] [PubMed] [Google Scholar]
- Copeland J, Swift W. Cannabis use disorder: Epidemiology and management. International Review of Psychiatry. 2009;21:96–103. doi: 10.1080/09540260902782745. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, Riper H, Lemmers L. The effects on mortality of brief interventions for problem drinking: A meta-analysis. Addiction. 2004;99:839–845. doi: 10.1111/j.1360-0443.2004.00778.x. [DOI] [PubMed] [Google Scholar]
- Denis C, Lavie E, Fatséas M, Auriacombe M. Psychotherapeutic interventions for cannabis abuse and/or dependence in outpatient settings. Cochrane Database of Systematic Reviews. 2006;19:111–116. doi: 10.1002/14651858.CD005336.pub2. [DOI] [PubMed] [Google Scholar]
- D'Onofrio G, Bernstein E. Patients with alcohol problems in the emergency department, Part 1: improving detection. SAEM Substance Abuse Task Force. Society for Academic Emergency Medicine. Academic Emergency Medicine. 1998a;5(12):1200–1209. doi: 10.1111/j.1553-2712.1998.tb02696.x. [DOI] [PubMed] [Google Scholar]
- D'Onofrio G, Bernstein E. Patients with alcohol problems in the emergency department, part 2: intervention and referral. SAEM Substance Abuse Task Force. Society for Academic Emergency Medicine. Academic Emergency Medicine. 1998b;5(12):1210–1217. doi: 10.1111/j.1553-2712.1998.tb02697.x. [DOI] [PubMed] [Google Scholar]
- D'Onofrio G, Pantalon MV, et al. Brief intervention for hazardous and harmful drinkers in the emergency department. Annals of Emergency Medicine. 2008;51(6):742–750. doi: 10.1016/j.annemergmed.2007.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degenhardt L, Hall W, Lynskey M. Alcohol, cannabis and tobacco use among Australians: a comparison of their associations with other drug use and use disorders, affective and anxiety disorders, and psychosis. Addiction. 2001a;96(11):1603–1614. doi: 10.1046/j.1360-0443.2001.961116037.x. [DOI] [PubMed] [Google Scholar]
- Degenhardt L, Hall W, Lynskey M. The relationship between cannabis use and other substance use in the general population. Drug Alcohol Depend. 2001b;64(3):319–327. doi: 10.1016/s0376-8716(01)00130-2. [DOI] [PubMed] [Google Scholar]
- Dunn C, Deroo L, Rivara FP. The use of brief interventions adapted from motivational interviewing across behavioral domains: A systematic review. Addiction. 2001;96(12):1725–1742. doi: 10.1046/j.1360-0443.2001.961217253.x. [DOI] [PubMed] [Google Scholar]
- Fischer B, Dawe M, McGuire F, Shuper P, Capler R, Bilsker D, Bilsker D. Feasibility and impact of brief interventions for frequent cannabis users in Canada. Journal of Substance Abuse Treatment. 2012 doi: 10.1016/j.jsat.2012.03.006. Available online 18 April 2012. [DOI] [PubMed] [Google Scholar]
- Forcehimes AA, Tonigan JS, Miller WR, Kenna GA, Baer JS. Psychometrics of the Drinker Inventory of Consequences (DrInC) Addictive Behaviors. 2007;32(8):1699–1704. doi: 10.1016/j.addbeh.2006.11.009. [DOI] [PubMed] [Google Scholar]
- Havard A, Shakeshaft A, Sanson-Fisher R. Systematic review and meta-analyses of strategies targeting alcohol problems in emergency departments: interventions reduce alcohol-related injuries. Addiction. 2008;103(3):368–376. doi: 10.1111/j.1360-0443.2007.02072.x. [DOI] [PubMed] [Google Scholar]
- Hesselbrock M, Babor T, Hesselbrock V, Meyer R, Workman K. Never Believe an Alcoholic? On the Validity of Self-Report Measures of Alcohol Dependence and Related Constructs. Substance Use & Misuse. 1983;18(5):593–609. doi: 10.3109/10826088309027359. [DOI] [PubMed] [Google Scholar]
- Kaner EF, Dickinson HO, Beyer F, Pienaar E, Schlesinegr C, Campbell F, Saunders JB, Burnand B, Heather N. Effectiveness of brief alcohol interventions in primary care populations. The Cochrane Library. 2009;7 doi: 10.1002/14651858.CD004148.pub3. OCT. www.thecochranelibrary.com. [DOI] [PubMed] [Google Scholar]
- Lang E, Engelander M, Brooke T. Report of an integrated brief intervention with self-defined problem cannabis users. Journal of Substance Abuse Treatment. 2000;19:111–116. doi: 10.1016/s0740-5472(99)00104-x. [DOI] [PubMed] [Google Scholar]
- Lipsey MW. Design sensitivity: Statistical power for experimental research. Newbury Park, CA: Sage Publications; 1990. [Google Scholar]
- Longabaugh R. Noteworthy Index of Problems: Unpublished Survey. 2003 [Google Scholar]
- Longabaugh R, Woolard R, Nirenberg T, Minugh AP, Becker B, Clifford PR, Carty K, Sparadeo F, Gogineni A. Evaluating the effects of a brief motivational intervention for injured drinkers in the emergency department. Journal of Studies on Alcohol. 2001;62(6):806–816. doi: 10.15288/jsa.2001.62.806. [DOI] [PubMed] [Google Scholar]
- Longo MC, Hunter CE, Lokan RT, White JM, White MA. The prevalence of alcohol, cannabinoids, benzodiazepines and stimulants amongst injured drivers and their role in driver culpability: Part I: The prevalence of drug use in drive the drug-positive group. Accident Analysis and Prevention. 2000;32(5):613–622. doi: 10.1016/s0001-4575(99)00111-6. [DOI] [PubMed] [Google Scholar]
- Marczinski C, Combs S, Filmore MT. Increased sensitivity to the disinhibiting effects of alcohol in binge drinkers. Psychology of Addictive Behaviors. 2007;21(3):346–354. doi: 10.1037/0893-164X.21.3.346. [DOI] [PubMed] [Google Scholar]
- Martin G, Copeland J, Swift W. The adolescent cannabis check-up: Feasibility of a brief intervention for young cannabis users. Journal of Substance Abuse Treatment. 2005;29:207–213. doi: 10.1016/j.jsat.2005.06.005. [DOI] [PubMed] [Google Scholar]
- Martin G, Copeland J. The adolescent cannabis check-up: Randomized trial of a brief intervention for young cannabis users. Journal of Substance Abuse Treatment. 2008;34:407–414. doi: 10.1016/j.jsat.2007.07.004. [DOI] [PubMed] [Google Scholar]
- McCambridge J, Slym R, Strang J. Randomized controlled trial of motivational interviewing compared with drug information and advice for early intervention among young cannabis users. Addiction. 2008;103:1809–1818. doi: 10.1111/j.1360-0443.2008.02331.x. [DOI] [PubMed] [Google Scholar]
- McRae A, Budney A, Brady K. Treatment of marijuana dependence: A review of the literature. Journal of Substance Abuse Treatment. 2003;24:369–376. doi: 10.1016/s0740-5472(03)00041-2. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. New York, NY: Guilford Press; 2002. [Google Scholar]
- Miller WR, Zweben A, DiClemente CC, Rychtarik R. Motivational Enhancement Therapy Manual National Institute on Alcohol Abuse and Alcoholism. U.S. Department of Health and Human Services. 1995 [Google Scholar]
- Nilsen P, Baird J, Mello MJ, Nirenberg T, Woolard R, Bendsten P, Longabaugh R. A systematic review of emergency care brief alcohol interventions for injury patients. Journal of Substance Abuse Treatment. 2008;35(2):184–201. doi: 10.1016/j.jsat.2007.09.008. [DOI] [PubMed] [Google Scholar]
- Nirenberg T, Lee C. Alcohol, Marijuana and Drug Use Index: Unpublished Survey. 2003 [Google Scholar]
- Nordstrom B, Levin F. Treatment of cannabis use disorder: A review of the literature. American Journal of Addiction. 2007;16:331–342. doi: 10.1080/10550490701525665. [DOI] [PubMed] [Google Scholar]
- Plant M, Miller P, Thornton C, Plant M, et al. Life Stage, Alcohol Consumption Patterns, Alcohol-Related Consequences, and Gender. Substance Abuse. 2000;21(4):265–281. doi: 10.1080/08897070009511438. [DOI] [PubMed] [Google Scholar]
- Quinlan KP, Brewer RD, Siegel P, Sleet DA, Mokdad AH, Shults RA, Flowers N. Alcohol-Impaired Driving Among U.S. Adults 1993–2002. American Journal Of Preventive Medicine. 2005;28(4):346–350. doi: 10.1016/j.amepre.2005.01.006. [DOI] [PubMed] [Google Scholar]
- Rehm J, Mathers C, et al. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet. 2009;373(9682):2223–2233. doi: 10.1016/S0140-6736(09)60746-7. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, De La fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption--II. Addiction. 1993;88(6):791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Smith AJ, Hodgson RJ, Bridgeman KK, Shepherd JP. A randomized controlled trial of a brief intervention after alcohol-related facial injury. Addiction. 2003;98(1):43–52. doi: 10.1046/j.1360-0443.2003.00251.x. [DOI] [PubMed] [Google Scholar]
- Soderstrom CA, Dischinger PC, Kerns TJ, Trifills Al. Marijuana and other drug use among automobile and motorcycle drivers treated at a trauma center. Accidident Analysis and Prevention. 1995;27(1):131–135. doi: 10.1016/0001-4575(94)00043-l. [DOI] [PubMed] [Google Scholar]
- Speltz ML, Gonzales N, Sulzbacker S, Quan L. Assessment of injury risk in young children: a preliminary study of the injury behavior checklist. Journal of Pediatric Psychology. 1990;15(3):373–383. doi: 10.1093/jpepsy/15.3.373. [DOI] [PubMed] [Google Scholar]
- Standerwick K, Davies C, Tucker L, Sheron N. Binge drinking, sexual behaviour and sexually transmitted infection in the UK. International Journal of STD & AIDS. 2007;18:810–813. doi: 10.1258/095646207782717027. [DOI] [PubMed] [Google Scholar]
- Stephens R, Roffman R, Fearer S, Williams C, Burke R. The marijuana Check-up: Promoting change in ambivalent marijuana users. Addiction. 2007;102:947–957. doi: 10.1111/j.1360-0443.2007.01821.x. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration and Office of Applied Studies. Rockville, MD: 2010. National Estimates of Drug-Related Emergency Department Visits: 2007, Drug Abuse Warning Network. [Google Scholar]
- Walker D, Roffman R, Stephens R, Berghuis J, Wakana K. Motivational enhancement therapy for adolescent marijuana users: A preliminary randomized controlled trial. Journal of Consulting and Clinical Psychology. 2006;74:628–632. doi: 10.1037/0022-006X.74.3.628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitlock EP, Polen MR, Green CA, et al. Behavioral counseling interventions in primary care to reduce risky/harmful alcohol use by adults: A summary of the evidence for the U.S. Preventive Services Task Force. Annals of Internal Medicine. 2004;140:557–568. doi: 10.7326/0003-4819-140-7-200404060-00017. [DOI] [PubMed] [Google Scholar]
- Woolard R, Baird J, Mello MJ, Nirenberg T, Longabaugh R. Injuries, negative consequences, and risk behaviors among both injured and uninjured emergency department patients who report using alcohol and marijuana. Journal of Emergency Trauma Shock. 2009;2(1):23–28. doi: 10.4103/0974-2700.44679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolard R, Nirenberg T, Longabaugh R. Alcohol, marijuana, and injury in the emergency department. Medicine and Health Rhode Island. 2002;85(10):306–308. [PubMed] [Google Scholar]
- World Health Assembly. Public health problems caused by harmful use of alcohol. Genva, Switzerland: World Health Organization; 2005. [Google Scholar]