Abstract
Objectives. We evaluated the association between the county sprawl index, a measure of residential density and street accessibility, and physical activity and body mass index (BMI).
Methods. We conducted a multilevel cross-sectional analysis in a sample of Nurses’ Health Study participants living throughout the United States in 2000 to 2001 (n = 136 592).
Results. In analyses adjusted for age, smoking status, race, and husband’s education, a 1-SD (25.7) increase in the county sprawl index (indicating a denser, more compact county) was associated with a 0.13 kilograms per meters squared (95% confidence interval [CI] = −0.18, −0.07) lower BMI and 0.41 (95% CI = 0.17, 0.65) more metabolic equivalent (MET) hours per week of total physical activity, 0.26 (95% CI = 0.19, 0.33) more MET hours per week of walking, and 0.47 (95% CI = 0.34, 0.59) more MET hours per week of walking, bicycling, jogging, and running. We detected potential effect modification for age, previous disease status, husband’s education level (a proxy for socioeconomic status), and race.
Conclusions. Our results suggest that living in a dense, compact county may be conducive to higher levels of physical activity and lower BMI in women.
The obesity epidemic in the United States is well documented,1,2 with estimates that 35.5% of adult women are obese.3 Only 60.4% of US women meet 2008 Department of Health and Human Services physical activity guidelines.4 Overweight and obesity are linked with numerous health outcomes, including cardiovascular diseases, arthritis, and stroke.5,6 Obesity has a multifactorial etiology, influenced by genetics, behavior, and environmental factors.7 Interventions at the environmental or neighborhood level, therefore, plausibly could change obesity-related behaviors and alter the distribution of overweight and obesity.
A growing literature links physical activity and obesity to the built environment.8 The built environment is defined as land-use patterns, transportation systems, and design features that provide opportunities for travel and physical activity.9,10 Attributes of the built environment, such as density, street connectivity, and land-use mix, have consistently been associated with increased walking and overall physical activity, as well as decreased body mass index (BMI).6,8,11–17 These factors create opportunities for walking, because homes, stores, and other destinations are closer, and influence access to recreational physical activity.18,19
Aspects of the built environment may have greater impact on women than on men for several reasons. Women bear a disproportionate burden for many of the outcomes associated with the built environment: they are more likely to be obese3 and less likely to meet physical activity guidelines.4,20 Women drive to places to exercise less frequently than do men and are more likely to walk for leisure activity, so walking in the neighborhood may be an important source of exercise.21,22 If the relationships between the built environment and health are truly causal, then interventions to improve the neighborhood built environment could have great impacts on the health of women.
Urban sprawl is defined as a process in which the “spread of development across the landscape far outpaces population growth.”23(p3) It is characterized by 4 dimensions: low residential density; rigidly separated homes, shops, and workplaces; roads with large blocks and poor access; and a lack of well-defined activity centers. These factors are thought to lead to decreased ability to walk from place to place and a lack of transportation choices. We used both individual health-related factors and county-level factors to examine the association between urban sprawl, physical activity, and BMI in a large sample of women living throughout the continental United States.
METHODS
The prospective Nurses’ Health Study (NHS) and NHS II follow large cohorts to assess an array of risk factors for chronic disease among women. For NHS, 121 700 female registered nurses aged 30 to 55 years from 11 states returned the initial questionnaire in 1976. The cohort has been continuously followed with biennial questionnaires. For the period of our study (2000–2001), 92% of the cohort still lived in their original states, although at least 10 participants resided in each of the 48 continental states. We geocoded all available addresses to the street or zip code level to obtain latitude and longitude.
The NHS II cohort, initiated in 1989, enrolled 116 686 female registered nurses aged 25 to 42 years from 14 states. As of 2001, 91% of the NHS II cohort still lived in these 14 states. The remainder of the cohort had relocated; at least 24 nurses resided in each of the 48 continental states. In both cohorts, response rates at each 2-year questionnaire cycle have consistently been approximately 90%. For both cohorts, return of the completed questionnaires implied consent to use the data in ongoing health research.
To assess the built environment, we used a standardized measure of urban sprawl, the county sprawl index, which has been associated with physical activity and BMI (defined as weight in kilograms divided by the square of height in meters).22,24 The county-level sprawl index was developed by Smart Growth America23 and calculated for all 952 metropolitan counties or statistically equivalent entities in the United States. We measured 2 characteristics of sprawl in each county, low residential density and poor street accessibility, derived from 6 variables in the 2000 US Census. Detailed information on the creation of the county sprawl index is available elsewhere.22 Higher county sprawl index values indicate a more compact county. We assigned an index value to each nurse according to the geocoded county of residence (in 2000 for NHS and 2001 for NHS II). We excluded from analysis all nurses who lived in counties where the sprawl index was not calculated.
Outcomes
We calculated BMI from self-reported weight in the 2000 NHS or 2001 NHS II questionnaire and self-reported height in the baseline questionnaire. A validation study of 184 NHS participants showed that self-reported weights were highly correlated with measured weights (r = 0.96; mean difference = 1.5 kg).25
The 2000 and 2001 questionnaires included a section on recreational physical activity during the past year, with questions on the average time per week spent walking or hiking outdoors, jogging (> 10 minutes per mile), running (≤ 10 minutes per mile), bicycling (including use of a stationary machine), lap swimming, playing tennis, playing squash or racquet ball, using a rowing machine, and engaging in calisthenics, aerobics, or aerobic dance. Each participant also reported the number of flights of stairs that she climbed daily and her usual walking pace. We multiplied the reported time spent weekly at each activity by its typical energy expenditure requirements expressed in metabolic equivalents (METs), then summed all the activity figures to yield a MET hours per week score.26 One MET, the energy expended while sitting quietly, is equivalent to 3.5 milliliters of oxygen uptake per kilogram of body weight per minute for a 70-kilogram adult. The following MET values were used for each activity: running, 12.0; playing squash or racquet ball, 9.0; climbing stairs, 8.0; jogging, bicycling, swimming, or playing tennis, 7.0; and calisthenics, aerobics, aerobic dance, or use of a rowing machine, 6.5. Walking was assigned a MET value corresponding to the reported pace: easy, 2.5; normal, 3.0; brisk, 4.0; or very brisk, 4.5.
In a validation study of 147 nurses who completed the same physical activity questionnaire, as well as quarterly 7-day activity diaries, the Pearson correlation coefficient between the MET scores from the questionnaires and the average of the diaries was 0.46. After adjustment for within-person variation in the diaries, the de-attenuated correlation was 0.56.27
We analyzed overall MET hours per week, walking MET hours per week, and a combined measure of MET hours per week for walking, bicycling, jogging, and running. We chose these combined activities because we hypothesized that they would be most closely related to the built environment.9
We included in our models correlates of physical activity and BMI that might also be correlated with urban sprawl: age, smoking (current, past, never), race (White, Black, Asian, other), and husband’s education as a proxy for individual socioeconomic status (SES; < high school, some high school, high school graduate, college graduate, graduate school).28 We also stratified analyses by previous disease status (reporting diabetes, cancer, or heart disease prior to 2000).
Statistical Analyses
We limited our analyses to respondents to the 2000 NHS or 2001 NHS II questionnaire who reported their weight, lived in a county where the sprawl index was estimated, were able to walk, and completed the physical activity questions. We conducted multilevel linear regression for physical activity or BMI on the county sprawl index and included a random county intercept to account for clustering of data among participants within a county. We expressed linear regression results as MET hours per week or BMI for each 1-SD increase in the sprawl index.
We also performed analyses with quartiles of sprawl. We conducted multilevel logistic regression by regressing the odds of being obese (BMI ≥ 30 kg/m2) or of achieving more than 500 MET minutes per week of physical activity (a value derived from the 2008 Physical Activity Guidelines for Americans29) on the county sprawl index. Consistent with the 2008 guidelines, we only included data on walking at moderate intensity or greater (> 3 MET) in our calculation for meeting guidelines for walking only. We analyzed effect modification by age, race, smoking status, husband’s education, and history of prior chronic diseases (cardiovascular disease, cancer, and diabetes) through modeling interaction terms, as well as through stratified analyses. In pooled analyses, we combined data from both NHS and NHS II, with adjustment for cohort. We conducted all statistical analyses with UNIX SAS version 9.1.3 (SAS Institute Inc, Cary, NC).
RESULTS
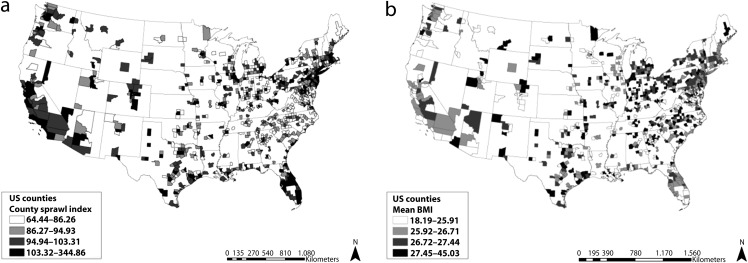
A total of 94 839 and 101 294 participants answered the 2000 NHS and 2001 NHS II questionnaires, respectively. After we excluded women who did not have data on BMI (NHS, n = 2487; NHS II, n = 6769), did not have a geocoded address or live in a county where the sprawl index was available (NHS, n = 12 134; NHS II, n = 13 676), could not walk (NHS, n = 966; NHS II, n = 305), or did not have complete information on physical activity (NHS, n = 9999; NHS II, n = 13 205), our sample comprised 69 253 women in NHS and 67 339 women in NHS II. The characteristics of our cohort are described in Table 1. Briefly, the mean county sprawl index in the 896 total counties for the combined cohorts was 109.5 and ranged from 62.6 to 352.1, with a SD of 25.7. This 1-SD increase equates to comparing Baltimore County, Maryland (Baltimore County sprawl index = 162.76), to Philadelphia County, Pennsylvania (Philadelphia County sprawl index = 187.78). The average age of NHS participants was 66 years (range = 53–81 years) and of NHS II participants was 46 years (range = 36–56 years). The majority were White, and most had husbands with at least a high school degree. Figure 1 shows the geographic distribution of the county sprawl index and the mean BMI across the counties in our analysis.
TABLE 1—
Participant and County Characteristics: United States, Nurses’ Health Study, 2000, and Nurses’ Health Study II, 2001
| NHS, No. (%) or Mean ±SD | NHS II, No. (%) or Mean ±SD | |
| Participants | 69 253 | 67 339 |
| Age, y | 66.4 ±7.1 | 46.2 ±4.7 |
| Race/ethnicity | ||
| White | 67 411 (97) | 62 233 (92) |
| Black | 1075 (2) | 1037 (2) |
| Asian | 598 (1) | 1043 (2) |
| Other | 169 (0.2) | 3026 (4) |
| Smoking status | ||
| Never | 30 429 (44) | 43 903 (65) |
| Past | 32 504 (47) | 17 762 (26) |
| Current | 6320 (9) | 5674 (8) |
| Husband’s educational level | ||
| < high school | 931 (< 1) | 361 (< 1) |
| Some high school | 2029 (3) | 9258 (14) |
| High school graduate | 20 139 (29) | 11 055 (16) |
| College graduate | 15 924 (23) | 18 654 (28) |
| Graduate school | 13 432 (19) | 18 359 (27) |
| Missing/not married | 16 798 (24) | 9652 (14) |
| BMI, kg/m2 | 26.7 ±5.3 | 26.8 ±6.3 |
| Physical activity, MET h/wk | 17.1 ±21.7 | 21.0 ±27.2 |
| Counties | 794 | 849 |
| County sprawl index | 109.5 ±23.1 | 109.4 ±28.0 |
Note. BMI = body mass index; MET = metabolic equivalent; NHS = Nurses' Health Study.
FIGURE 1—
County sprawl index and mean body mass index in participants and counties: United States, Nurses’ Health Study, 2000, and Nurses’ Health Study II, 2001.
After adjustment for age, smoking status, race, and husband’s education, a 1-SD increase in the county sprawl index (25.7 units) was associated with a 0.08 kilograms per meters squared lower average BMI (95% confidence interval [CI] = −0.14, −0.02) in NHS, −0.19 kilograms per meters squared (95% CI = −0.26, −0.11) in NHS II, and −0.13 kilograms per meters squared (95% CI = −0.18, −0.07) in the 2 cohorts combined. Analyses of the association between the county sprawl index and all of the physical activity outcomes showed a positive and statistically significant relationship in NHS and NHS II; these results were robust to adjustment for age, smoking, race, and husband’s education. Analyses of the 2 cohorts combined showed a 1-SD increase in the county sprawl index associated with an increase of 0.41 (95% CI = 0.17, 0.65) MET hours per week of total physical activity, 0.26 (95% CI = 0.19, 0.33) MET hours per week of walking, and 0.47 (95% CI = 0.34, 0.59) MET hours per week of combined walking, bicycling, jogging, and running in fully adjusted models. Analyses by quartile of the sprawl index indicated a dose–response relationship between the county sprawl index and both BMI and physical activity, with the strongest relationships generally seen in the highest quartile (Table 2).
TABLE 2—
Correlations Between Body Mass Index and Physical Activity by Quartiles of the County Sprawl Index: United States, Nurses’ Health Study, 2000, and Nurses’ Health Study II, 2001
| County Sprawl Index, quartilea | Age Adjusted, B (95% CI) | Fully Adjusted,b B (95% CI) |
| BMI, kg/m2 | ||
| 1 (Ref) | 1.00 | 1.00 |
| 2 | −0.17 (−0.32, −0.03) | −0.13 (−0.27, 0.00) |
| 3 | −0.36 (−0.52, −0.20) | −0.29 (−0.43, −0.14) |
| 4 | −0.43 (−0.61, −0.25) | −0.37 (−0.53, −0.20) |
| Total activity, MET h/wk | ||
| 1 (Ref) | 1.00 | 1.00 |
| 2 | 0.37 (−0.25, 0.99) | 0.20 (−0.39, 0.79) |
| 3 | 1.05 (0.38, 1.72) | 0.74 (0.11, 1.37) |
| 4 | 1.00 (0.24, 1.76) | 0.67 (−0.05, 1.39) |
| Walking, MET h/wk | ||
| 1 (Ref) | 1.00 | 1.00 |
| 2 | 0.02 (−0.18, 0.21) | −0.02 (−0.21, 0.18) |
| 3 | 0.16 (−0.05, 0.37) | 0.11 (−0.10, 0.31) |
| 4 | 0.38 (0.15, 0.62) | 0.33 (0.10, 0.56) |
| Combined walking, bicycling, jogging, and running, MET h/wk | ||
| 1 (Ref) | 1.00 | 1.00 |
| 2 | 0.32 (−0.02, 0.65) | 0.24 (−0.09, 0.56) |
| 3 | 0.62 (0.26, 0.98) | 0.49 (0.15, 0.84) |
| 4 | 0.86 (0.45, 1.27) | 0.72 (0.33, 1.12) |
Note. BMI = body mass index; CI = confidence interval; MET = metabolic equivalent.
Quartile 1: from Jackson County, GA (62.55), to Allen County, IN (97.44); quartile 2: from Lawrence County, OH (97.44), to Lancaster County, NE (106.62); quartile 3: from Monongalia County, WV (106.62), to Contra Costa County, CA (115.77); quartile 4: from Santa Barbara County, CA (115.77), to New York County, NY (352.07).
Adjusted for age, smoking, race, and husband’s education.
Consistent with our multilevel linear regression analyses, fully adjusted multilevel logistic models revealed that a 1-SD increase in the county sprawl index was associated with a 2% decrease in the odds of being obese (95% CI = 1%, 3%) in NHS and a 5% decrease in NHS II (95% CI = 4%, 6%). Similarly, a 1-SD-higher country sprawl index was associated with a 5% increase in NHS (95% CI = 4, 6%) and 6% increase in NHS II (95% CI = 5%, 7%) in the odds of meeting the physical activity guidelines through walking and an increase in the odds of meeting the guidelines through walking, jogging, running, or bicycling of 4% in NHS (95% CI = 3%, 5%) and 7% in NHS II (95% CI = 6%, 7%).
Our stratified analyses yielded similar results for NHS and NHS II (data for NHS is shown in Table 3). We found little evidence of effect modification by smoking. In both NHS and NHS II participants, we found stronger associations between county sprawl and BMI in women with previous disease than in those with no previous disease. The relationship between the county sprawl index and both total physical activity and walking, jogging or running, or bicycling was stronger in younger women in both cohorts and in women whose husbands had a college education or higher in NHS. Overall, we detected little evidence of effect modification by race, although we did find a positive effect of the sprawl index on walking among Whites, with no associations among Black women or women whose race was categorized as other.
TABLE 3—
Correlations Between Body Mass Index and Physical Activity by 1-SD Change in Average County Sprawl Index, Stratified by Potential Effect Modifiers: United States, Nurses’ Health Study, 2000
| Modifier | No. | Total Activity, B (95% CI) | P for Interaction | Walking, B (95% CI) | P for Interaction | Combined Walking, Bicycling, Jogging, and Running, B (95% CI) | P for Interaction | BMI, B (95% CI) | P for Interaction |
| Age, y | <.001 | .141 | <.001 | .926 | |||||
| 53.5–60.4 | 17 272 | 0.44 (0.01, 0.87) | 0.27 (0.10, 0.44) | 0.45 (0.22, 0.68) | –0.07 (–0.18, 0.04) | ||||
| 60.5–66.1 | 17 029 | 0.76 (0.31, 1.22) | 0.32 (0.15, 0.49) | 0.49 (0.25, 0.72) | –0.10 (–0.19, 0.00) | ||||
| 66.2–72.5 | 17 633 | –0.12 (–0.54, 0.30) | 0.23 (0.07, 0.39) | 0.22 (0.00, 0.44) | –0.08 (–0.18, 0.01) | ||||
| 72.6–81.3 | 17 319 | –0.23 (–0.57, 0.11) | 0.17 (0.02, 0.31) | 0.08 (–0.11, 0.28) | –0.10 (–0.19, –0.01) | ||||
| Race | .054 | .023 | .111 | .824 | |||||
| White | 67 411 | 0.34 (0.06, 0.61) | 0.27 (0.17, 0.37) | 0.36 (0.22, 0.50) | –0.08 (–0.14, –0.02) | ||||
| Black | 1 075 | 0.02 (–0.77, 0.81) | –0.02 (–0.35, 0.31) | 0.16 (–0.23, 0.55) | –0.04 (–0.24, 0.16) | ||||
| Asian | 598 | –0.27 (–1.60, 1.06) | 0.04 (–0.53, 0.60) | –0.04 (–0.84, 0.76) | –0.21 (–0.44, 0.02) | ||||
| Other | 169 | –0.19 (–4.23, 3.85) | 1.28 (–0.40, 2.97) | 1.22 (–0.76, 3.21) | –0.33 (–1.10, 0.44) | ||||
| Husband’s educational level | .004 | .729 | .025 | .948 | |||||
| ≤ high school | 23 099 | –0.32 (–0.66, 0.03) | 0.15 (0.01, 0.29) | 0.08 (–0.11, 0.26) | –0.02 (–0.11, 0.07) | ||||
| ≥ College | 29 356 | 0.19 (–0.18, 0.56) | 0.31 (0.18, 0.45) | 0.34 (0.15, 0.52) | –0.13 (–0.20, –0.05) | ||||
| Smoking status | .074 | .486 | .136 | .797 | |||||
| Never | 30 429 | 0.44 (0.11, 0.77) | 0.25 (0.13, 0.38) | 0.42 (0.24, 0.59) | –0.09 (–0.17, –0.01) | ||||
| Past | 32 504 | 0.01 (–0.33, 0.34) | 0.23 (0.10, 0.36) | 0.21 (0.04, 0.38) | –0.09 (–0.17, –0.02) | ||||
| Current | 6 320 | 0.05 (–0.51, 0.62) | 0.22 (–0.01, 0.45) | 0.35 (0.05, 0.65) | –0.05 (–0.19, 0.08) | ||||
| Previous cancer, diabetes, or heart disease | .071 | .204 | .212 | .013 | |||||
| No | 50 863 | 0.44 (0.15, 0.74) | 0.23 (0.12, 0.34) | 0.39 (0.23, 0.54) | –0.06 (–0.12, 0.00) | ||||
| Yes | 18 390 | –0.10 (–0.45, 0.25) | 0.33 (0.19, 0.47) | 0.22 (0.02, 0.41) | –0.16 (–0.27, –0.06) |
Note. BMI = body mass index; CI = confidence interval; Models adjusted for age, smoking, race, and husband’s education, except where they were the stratifying variable.
DISCUSSION
We found an inverse relationship between the county sprawl index and BMI and positive associations between the county sprawl index and physical activity, indicating that women who lived in denser counties with more accessible street designs had lower BMIs and were more active. Our findings add to the literature because they were derived from a large, geographically diverse sample and focus on a broad age range of adult women, who are at the highest risk of inactivity.4 We also examined multiple effect modifiers and potential confounders. We analyzed data from a cohort of mostly White nurses, giving us fewer concerns about confounding by SES or race.
Our findings are consistent with other studies that examined associations between urban sprawl, BMI, and physical activity. A study of Behavioral Risk Factor Surveillance System data on 206 992 adults from 448 counties in the United States found that the county sprawl index was positively associated with minutes walked and negatively associated with obesity, BMI, and hypertension.22 The effect sizes for these outcomes were stronger in adults aged 65 years and older, whereas we found stronger associations for 2 physical activity outcomes among younger women. Similar results were observed in the National Longitudinal Survey of Youth, where the county sprawl index was negatively associated with risk for overweight and obesity.24 The authors did not find statistically significant relationships in their longitudinal analyses, although coefficients suggested that BMI decreased when participants moved to denser areas.
Plantinga and Bernell attempted to isolate a causal relationship between the county sprawl index and obesity in the National Longitudinal Survey of Youth and found that moving to a denser county led to decreases in BMI (P = .04).30 Cross-sectional analyses in a study of 4997 older men showed that a higher county sprawl index was associated with more walking and meeting physical activity recommendations by walking, as well as with lower prevalence of overweight; however, these associations were not found in longitudinal analyses.31 Several studies have analyzed the relationship between other measures of the built environment and physical activity or BMI and generally have had findings consistent with ours.14,32–36
We found some evidence of effect modification by age, disease status, husband’s education (a proxy of SES), and race. Effect modification by age may be attributable to differential effects of the built environment on behavior over the life course: surroundings may have more influence on physical activity among younger individuals, and older individuals’ levels of physical activity likely are determined by other factors. The associations between sprawl, walking, and BMI were stronger in those with previous cancer, diabetes, or heart disease, which is a unique finding. This may be because persons with prior disease find it easier to engage in low-impact physical activity or to obtain health counseling in denser and more connected areas.
Consistent with our results, other authors have observed potential effect modification by race37 and SES.38 Possibly neighborhood safety is inferior in low-SES and minority neighborhoods, and this drives walking behavior more than the built environment. Other factors, such as levels of automobile access and use among different socioeconomic groups, may explain effect modification by SES. Joshu et al. examined the relationship between the county sprawl index and BMI and observed results similar to ours.39 They assessed potential effect modification by personal barriers to physical activity (e.g., no safe place to exercise) and found that these barriers have less impact on BMI in more compact counties, indicating that living in a denser county may diminish the negative impact of personal barriers on BMI.
Limitations
The questionnaire did not specifically ask whether physical activity took place indoors or outdoors, and it is unclear what impact this outcome misclassification had on our results. When we restricted our outcome to the activities most likely to be affected by the built environment (instead of our total physical activity measure), our associations were strengthened. This lends support to the theory that the built environment is driving these specific behaviors.
Participants were asked to report on recreational physical activities as opposed to physical activity that might be related to active transportation. The walking item specified “walking for exercise or walking to work.” However, it is likely that other types of utilitarian or transportation-related physical activity, such as walking or bicycling to do errands, were underreported. That we still saw statistically significant results despite this underreporting is a novel finding because it suggests that denser and more connected built environments have the potential to increase opportunities for recreational physical activity.
We assessed the built environment at the county level, leading to concerns over exposure misclassification. The scale at which the built environment potentially operates on physical activity behaviors is unknown, and a county-level metric may be too large. In addition, the county sprawl index is only available in metropolitan counties, and therefore results may not be generalizable to women in rural counties or other regions not represented in the sample. However, because policies are often made at the county level, these results may be relevant for decision-makers in crafting healthy land-use policy.
Because the majority of our participants were White, our sample lacked racial diversity. This constrained understanding of the effect of the built environment on other races. In addition, all participants at one time worked as a nurse. This does not imply that the results are only applicable to nurses; however, it is possible that they can only be generalized to women of similar SES. We addressed confounding by SES to the best of our ability by adjusting our models by the measure of husband’s highest achieved educational degree. We believe that this measure explains the majority of variation in SES among female nurses of the age and period of our cohorts. Unfortunately, NHS asked very few further questions about SES, limiting our ability to investigate this issue in detail.
The cross-sectional design of the study diminished our ability to establish temporality. Therefore, we cannot preclude that reverse causation accounted for the relationships we observed; that is, people who participated in physical activity chose to live in denser and more connected counties. Finally, it is unclear by what mechanism sprawl correlates with physical activity and BMI. Density and street accessibility may be markers for other factors that drive physical activity and BMI; therefore, no definitive statements on causal relationships can be based on our results alone.
Conclusions
Because the majority of the US population is exposed to some type of sprawl, even small effect sizes may be of large public health importance through their effects on the population distributions of physical activity and BMI. Healthy People 2020 objectives are to increase the prevalence of those achieving physical activity guidelines from 43.5% to 47.9%.40 The increased odds of 4% to 7% for meeting physical activity recommendations found in our analysis are therefore meaningful.
Our findings contribute to our understanding of the associations between sprawl, BMI, and physical activity in adult women. Our findings indicate statistically significant associations between BMI, recreational physical activity, and residential density and street accessibility, as measured by the county sprawl index. Our study builds on the existing literature regarding the effects of the built environment on women over a broad age range through a nationally distributed sample and a large sample size.
Acknowledgments
This research was supported by the National Cancer Institute (grants R21 CA125078-01 A1, P01 CA87969, and R01 CA50385).
Human Participant Protection
The Brigham and Women’s Hospital institutional review board approved the study protocol. Participants’ return of the completed questionnaires implied consent to use the data in ongoing health research.
References
- 1.Centers for Disease Control and Prevention Obesity and overweight for professionals: data and statistics: US obesity trends. 2009. Available at: http://www.cdc.gov/obesity/data/trends.html. Accessed November 18, 2009
- 2.Mokdad AH, Ford ES, Bowman BAet al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA. 2003;289(1):76–79 [DOI] [PubMed] [Google Scholar]
- 3.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303(3):235–241 [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention Prevalence of self-reported physically active adults—United States, 2007. MMWR Morb Mortal Wkly Rep. 2008;57(48):1297–1300 [PubMed] [Google Scholar]
- 5.Must A, Spadano J, Coakley EH, Field AE, Colditz G, Dietz WH. The disease burden associated with overweight and obesity. JAMA. 1999;282(16):1523–1529 [DOI] [PubMed] [Google Scholar]
- 6.Patterson RE, Frank LL, Kristal AR, White E. A comprehensive examination of health conditions associated with obesity in older adults. Am J Prev Med. 2004;27(5):385–390 [DOI] [PubMed] [Google Scholar]
- 7.National Heart, Lung, and Blood Institute Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults. Bethesda, MD: National Institutes of Health; 1998. NIH publication 98–4083 [Google Scholar]
- 8.Feng J, Glass TA, Curriero FC, Stewart WF, Schwartz BS. The built environment and obesity: a systematic review of the epidemiologic evidence. Health Place. 2009;16(2):175–190 [DOI] [PubMed] [Google Scholar]
- 9.Committee on Physical Activity, Health, Transportation, and Land Use, Transportation Research Board, Institute of Medicine Does the Built Environment Influence Physical Activity? Examining the Evidence. Washington, DC: National Academies Press; 2005. Special report 282 [Google Scholar]
- 10.Brownson RC, Hoehner CM, Day K, Forsyth A, Sallis JF. Measuring the built environment for physical activity: state of the science. Am J Prev Med. 2009;36(4 suppl):S99–S123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Frumkin H, Frank L, Jackson R. Urban Sprawl and Public Health: Designing, Planning, and Building for Healthy Communities. Washington, DC: Island Press; 2004 [Google Scholar]
- 12.Papas MA, Alberg AJ, Ewing R, Helzlsouer KJ, Gary TL, Klassen AC. The built environment and obesity. Epidemiol Rev. 2007;29:129–143 [DOI] [PubMed] [Google Scholar]
- 13.Michael Y, Beard T, Choi D, Farquhar S, Carlson N. Measuring the influence of built neighborhood environments on walking in older adults. J Aging Phys Act. 2006;14(3):302–312 [DOI] [PubMed] [Google Scholar]
- 14.Berke EM, Koepsell TD, Moudon AV, Hoskins RE, Larson EB. Association of the built environment with physical activity and obesity in older persons. Am J Public Health. 2007;97(3):486–492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fisher KJ, Li F, Michael Y, Cleveland M. Neighborhood-level influences on physical activity among older adults: a multilevel analysis. J Aging Phys Act. 2004;12(1):45–63 [DOI] [PubMed] [Google Scholar]
- 16.Cunningham GO, Michael YL. Concepts guiding the study of the impact of the built environment on physical activity for older adults: a review of the literature. Am J Health Promot. 2004;18(6):435–443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ewing R, Cervero R. Travel and the built environment. J Am Plann Assoc. 2010;76(3):265–294 [Google Scholar]
- 18.Sallis JF. Measuring physical activity environments: a brief history. Am J Prev Med. 2009;36(4 suppl):S86–S92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Handy S. Critical assessment of the literature on the relationships among transportation, land use, and physical activity. In: Committee on Physical Activity, Health, Transportation, and Land Use, Transportation Research Board, Institute of Medicine. Does the Built Environment Influence Physical Activity? Examining the Evidence. Washington, DC: National Academies Press; 2005:Appendix A. Special report 282.
- 20.Troiano RP, Freedson PS. Promises and pitfalls of emerging measures of physical activity and the environment. Am J Prev Med. 2010;38(6):682–683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Handy SL. Community design and travel behavior: exploring the implications for women. : Transportation Research Board, Conference on Research on Women's Issues in Transportation Chicago, IL: National Academies Press; 2006:29–38 [Google Scholar]
- 22.Ewing R, Schmid T, Killingsworth R, Zlot A, Raudenbush S. Relationship between urban sprawl and physical activity, obesity, and morbidity. Am J Health Promot. 2003;18(1):47–57 [DOI] [PubMed] [Google Scholar]
- 23.Smart Growth America Measuring sprawl and its impact: the character and consequences of urban expansion. 2002. Available at: http://www.smartgrowthamerica.org/resources/measuring-sprawl-and-its-impact. Accessed May 4, 2010
- 24.Ewing R, Brownson RC, Berrigan D. Relationship between urban sprawl and weight of United States youth. Am J Prev Med. 2006;31(6):464–474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Willett W, Stampfer MJ, Bain Cet al. Cigarette smoking, relative weight, and menopause. Am J Epidemiol. 1983;117(6):651–658 [DOI] [PubMed] [Google Scholar]
- 26.Ainsworth BE, Haskell WL, Leon ASet al. Compendium of physical activities: classification of energy costs of human physical activities. Med Sci Sports Exerc. 1993;25(1):71–80 [DOI] [PubMed] [Google Scholar]
- 27.Wolf AM, Hunter DJ, Colditz GAet al. Reproducibility and validity of a self-administered physical activity questionnaire. Int J Epidemiol. 1994;23(5):991–999 [DOI] [PubMed] [Google Scholar]
- 28.Lee S, Kawachi I, Berkman LF, Grodstein F. Education, other socioeconomic indicators, and cognitive function. Am J Epidemiol. 2003;157(8):712–720 [DOI] [PubMed] [Google Scholar]
- 29.The 2008 Physical Activity Guidelines for Americans. Washington, DC: US Department of Health and Human Services; 2008 [Google Scholar]
- 30.Plantinga AJ, Bernell S. The association between urban sprawl and obesity: is it a two-way street? J Reg Sci. 2007;47(5):857–879 [Google Scholar]
- 31.Lee IM, Ewing R, Sesso HD. The built environment and physical activity levels: the Harvard Alumni Health Study. Am J Prev Med. 2009;37(4):293–298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lopez R. Urban sprawl and risk for being overweight or obese. Am J Public Health. 2004;94(9):1574–1579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Frank LD, Schmid TL, Sallis JF, Chapman JF, Saelens BE. Linking objectively measured physical activity with objectively measured urban form: findings from SMARTRAQ. Am J Prev Med. 2005;28(2 suppl 2):117–125 [DOI] [PubMed] [Google Scholar]
- 34.Li F, Fisher KJ, Brownson RC, Bosworth M. Multilevel modelling of built environment characteristics related to neighbourhood walking activity in older adults. J Epidemiol Community Health. 2005;59(7):558–564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Li F, Harmer PA, Cardinal BJet al. Built environment, adiposity, and physical activity in adults aged 50–75. Am J Prev Med. 2008;35(1):38–46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Garden FL, Jalaludin BB. Impact of urban sprawl on overweight, obesity, and physical activity in Sydney, Australia. J Urban Health. 2009;86(1):19–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Scott MM, Dubowitz T, Cohen DA. Regional differences in walking frequency and BMI: what role does the built environment play for Blacks and Whites? Health Place. 2009;15(3):882–887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lovasi GS, Hutson MA, Guerra M, Neckerman KM. Built environments and obesity in disadvantaged populations. Epidemiol Rev. 2009;31:7–20 [DOI] [PubMed] [Google Scholar]
- 39.Joshu CE, Boehmer TK, Brownson RC, Ewing R. Personal, neighbourhood and urban factors associated with obesity in the United States. J Epidemiol Community Health. 2008;62(3):202–208 [DOI] [PubMed] [Google Scholar]
- 40.US Department of Health and Human Services Healthy people 2020—improving the health of Americans. 2012. Available at: http://www.healthypeople.gov/2020/default.aspx. Accessed April 25, 2012