Abstract
Among substance-dependent individuals comorbid major depressive disorder (MDD) is associated with greater severity and poorer treatment outcomes, but little research has examined mediators of post-treatment substance use outcomes within this population. Using latent growth curve models we tested relationships between individual rates of change in 12-step involvement and substance use, utilizing post-treatment follow-up data from a trial of group Twelve-Step Facilitation (TSF) and Integrated Cognitive-Behavioral Therapy (ICBT) for veterans with substance dependence and MDD. While TSF patients were higher on 12-step affiliation and meeting attendance at end-of-treatment as compared to ICBT, they also experienced significantly greater reductions in these variables during the year following treatment, ending at similar levels as ICBT. Veterans in TSF also had significantly greater increases in drinking frequency during follow-up, and this group difference was mediated by their greater reductions in 12-step affiliation and meeting attendance. Patients with comorbid depression appear to have difficulty sustaining high levels of 12-step involvement after the conclusion of formal 12-step interventions, which predicts poorer drinking outcomes over time. Modifications to TSF and other formal 12-step protocols or continued therapeutic contact may be necessary to sustain 12-step involvement and reduced drinking for patients with substance dependence and MDD.
Keywords: 12-step involvement, comorbidity, mediation
Introduction
Among individuals diagnosed with substance dependence, major depressive disorder (MDD) is a common and problematic psychiatric comorbidity, affecting an estimated 22% of persons with alcohol dependence and 40% with drug dependence (1). Compared to individuals without comorbidity, those with MDD have a poorer long-term course of substance use (2), greater risk of suicide (3), and greater treatment costs (4,5). In clinical settings the prevalence of comorbid MDD is even greater, exceeding 50% in some settings (6), and these patients typically have poorer outcomes from inpatient (7) or outpatient treatment (8–10). Given the vast prevalence and complications associated with comorbid substance dependence and MDD, there is a clear need to better understand processes that contribute to long-term outcomes in these chronically-disabled patients, and to develop treatments that better sustain long-term change.
Researchers have recently stressed the importance of identifying mechanisms of behavior change (11,12), the factors that explain why and how treatments work. Some of the most prominent mediating variables in this line of research have been those related to 12-step involvement, such as attendance at 12-step meetings and affiliation with 12-step principles. Greater levels of 12-step affiliation and attendance have been consistently associated with reduced alcohol and drug use in general samples (13,14), but fewer studies have examined these relations in patients with psychiatric comorbidity. Similar levels of participation (6) and degree of benefit from 12-step meetings (15) have been found for patients with psychiatric conditions, but other studies found reduced long-term benefits (16) for patients with comorbid MDD. Given the inconsistent and limited body of research, further studies are needed to clarify the importance of post-treatment 12-step affiliation and meeting attendance for patients with comorbid substance dependence and MDD.
The extent to which specific interventions can produce sustained levels of 12-step involvement in comorbid patients is also relatively unknown. Treatments designed specifically to increase 12-step attendance and affiliation can achieve these goals in substance-dependent patients (17,18), including those with greater psychiatric severity (19). Similar results were found in our sample of veterans with comorbid MDD, where patients receiving group Twelve-Step Facilitation (TSF) had increased levels of 12-step affiliation during treatment (20). However, it is not known whether comorbid patients can sustain high levels of 12-step participation after the conclusion of TSF therapy, and if any changes in long-term participation will impact substance use. Surprisingly few studies of substance-dependent samples have directly examined post-treatment change in 12-step involvement, but some investigations have found no decline in 12-step attendance or affiliation in the first six months (21) or one year (18) following treatment. Patients with comorbid MDD could have greater difficulty sustaining 12-step involvement, possibly due to persistent depressive symptoms interfering with meeting attendance, difficulty making social connections with group members, or group resistance to the use of psychotropic medication (22). Difficulty sustaining 12-step involvement may contribute to the poorer long-term treatment outcomes for patients with comorbid MDD, but to date this question has not been examined empirically.
This study involves secondary analyses of a sample of veterans enrolled in a 6-month trial of group TSF and Integrated Cognitive Behavioral Therapy (ICBT) for treatment of comorbid substance dependence and major depression (23,24). Utilizing latent growth curve models (LGMs) which explicitly model individual patterns of change in specified variables, we had three primary aims related to 12-step involvement and post-treatment substance use during the one-year follow-up period. First, we aimed to describe the post-treatment trajectories of 12-step affiliation and meeting attendance separately for the TSF and ICBT groups. Secondly, we examined if the post-treatment trajectories of 12-step affiliation and meeting attendance differed between TSF and ICBT, hypothesizing that patients in TSF would have difficulty sustaining within-treatment levels of 12-step affiliation and attendance and evince greater decline in these variables during follow-up. Thirdly, we examined if post-treatment change in 12-step affiliation and meeting attendance predicted post-treatment change in drinking and drug use. We hypothesized that greater reductions in 12-step affiliation and meeting attendance would predict greater increases in drinking and drug use, and that these effects would mediate the superior long-term treatment effects observed for the ICBT condition.
Methods
Subjects
The sample for this study includes 201 veterans who participated in a trial of outpatient group psychotherapy for comorbid substance dependence and MDD (23,24). We included all participants from the trial who completed at least one follow-up assessment from end-of-treatment (Month 6) to the one-year follow-up (Month 18). Demographics of the sample are presented in Table 1. Study inclusion criteria were lifetime dependence on alcohol, cannabis, or stimulants with recent (past 90 day) use, and major depressive disorder with at least one episode occurring independently of substance use. Exclusion criteria included opiate dependence with intravenous administration, bipolar or psychotic disorder, residing excessively far (≥ 50 miles) from the research facility, or memory impairments prohibiting accurate recall in study assessments.
Table 1.
Demographic and clinical characteristics of veterans with substance dependence and major depression (N = 201).
| TSF n =113 | ICBT n =129 | |
|---|---|---|
| Male | 90.4 % | 89.7 % |
| Caucasian | 71.3 % | 78.5 % |
| Mean age (SD) | 49.2 (7.6) | 48.9 (7.8) |
| Mean years of education (SD) | 13.6 (2.2) | 13.4 (2.1) |
| Employed | 21.3 % | 16.0 % |
| Married | 7.6 % | 17.0 % |
| Alcohol dependence | 86.7 % | 91.9 % |
| Stimulant dependence | 55.2 % | 54.4 % |
| Cannabis dependence | 28.7 % | 31.1 % |
TSF: Twelve-Step Facilitation; ICBT: Integrated Cognitive-Behavioral Therapy
Procedures
The procedures for this study were approved by the University of California, San Diego and VA San Diego Healthcare System (VASDHS) Institutional Review Boards. Participant referrals were obtained from the VASDHS dual diagnosis clinic by research study staff, who conducted brief screenings prior to meeting with eligible veterans to explain study procedures and obtain informed consent. Participating veterans consented to 6 months of group psychotherapy, recording of sessions, psychotropic medication management appointments, random urine screens, and research assessments conducted at intake and at 3-month intervals for an 18-month period. Veterans agreed to receive no other formal treatment for substance use or depression for the duration of group psychotherapy. Participation in other formal intervention was allowed during follow-up.
Group Treatments
Group psychotherapy was initiated on a rolling basis, with starts occurring every 2 weeks. After completing the intake assessment participants were sequentially allocated to the treatment condition with the next start date. For Twelve-Step Facilitation (TSF) we modified the TSF protocol from Project MATCH (25) to allow group delivery and discussion of multiple substances. For development of Integrated Cognitive-Behavioral Therapy (ICBT), material was adapted from two empirically-supported treatments: group cognitive-behavioral therapy for depression (26) and cognitive-behavioral relapse prevention from Project MATCH (27). The two treatments were identically structured with a series of three modules, with each module designed to cover a specific 12-step (e.g., Steps 1–3) or cognitive-behavioral (e.g., modifying thoughts) topic. Group sessions occurred twice/week for the first 3 months of group treatment, when each topic was covered in a one-month block. Topics were reviewed in the next 3 months during weekly group sessions. The mean session attendance was similar (M = 22 sessions) across groups. Interventions were co-delivered by senior clinicians (e.g., clinical staff or post-doctoral fellows) and doctoral students trained via manual review, direct observation, and weekly supervision. Therapists were rotated across treatment conditions on a regular basis (every 6–12 months), and adherence to protocol was assessed via videotape review.
Measures
Measures utilized in this study were obtained at end-of-treatment (Month 6) and at 3-month intervals until the one-year follow-up (Month 18).
12-step meeting attendance and affiliation
We used the Alcoholics Anonymous Affiliation Scale (28) to measure 12-step affiliation and meeting attendance in the past month. Analytical models examined 12-step affiliation and meeting attendance separately, as prior research has found differences in their prediction of substance use (29). The number of 12-step meetings attended in the past month was measured by a single ordinal item, while 12-step affiliation was measured with the sum of four binary items (e.g., having a sponsor, reading literature, doing service, having a spiritual awakening). We utilized the 12-step variables from Months 6, 9, 12, 15, and 18.
Frequency of alcohol and drug use
Alcohol and drug use during the prior 90 days was assessed with the Timeline Follow-Back (TLFB (30)), a reliable and valid calendar-assisted interview (31). In this study the TLFB was utilized to separately examine percent days drinking (PDD) and percent days using drugs (PDDRG) during the previous 90 days. Our analyses included all measures of PDD and PDDRG from end-of-treatment (Month 6) and the 12-month follow-up period (Months 9, 12, 15, and 18).
Statistical methods
Our longitudinal analyses utilized latent growth modeling (LGM) in the structural equation modeling framework. In LGM a series of repeated measures (e.g., PDD at Months 6 through 18) are used to indicate each individual’s underlying latent “growth curve” (i.e., trajectory) on one or more variables. This process creates separate growth curves for each individual, described by “growth factors” such as latent intercept (starting level) and latent slope (rate of change over time). Estimates of the sample mean and variance are obtained for each growth factor, and covariates can be used to predict individual differences in the initial level or rate of change over time. One distinct advantage of LGM is the ability to examine relations between the rates of change in multiple longitudinal processes, as warranted by the aims of this study. Because we were primarily concerned with the 12-month follow-up period, the end-of-treatment (Month 6) time point served as the initial level for each LGM. Thus, in each LGM the latent intercept represents the level at end-of-treatment, while latent slopes represent rates of increase or decrease during the 12 months of follow-up (Month 6 to Month 18).
For each study variable we first fit unconditional (i.e., no predictors) growth models to determine the optimal shape of the growth trajectory, before incorporating treatment group as a predictor in conditional models. This allowed us to test whether treatment condition predicted variability in the intercepts and slopes. In the final LGMs for PDD and PDDRG we specified growth curve mediation models (see Figure 1), to determine if the slope of 12-step affiliation or meeting attendance mediated the relationship between treatment group and the slope of PDD or PDDRG. To test the significance of mediated effects we used asymmetric 95% confidence intervals obtained with the bias-corrected bootstrap procedure (32), which has shown greater power to detect mediated effects than other formal mediation tests (33). All LGMs utilized the maximum likelihood procedure, which incorporates all available data from each participant under the assumption of missing at random.
Figure 1.
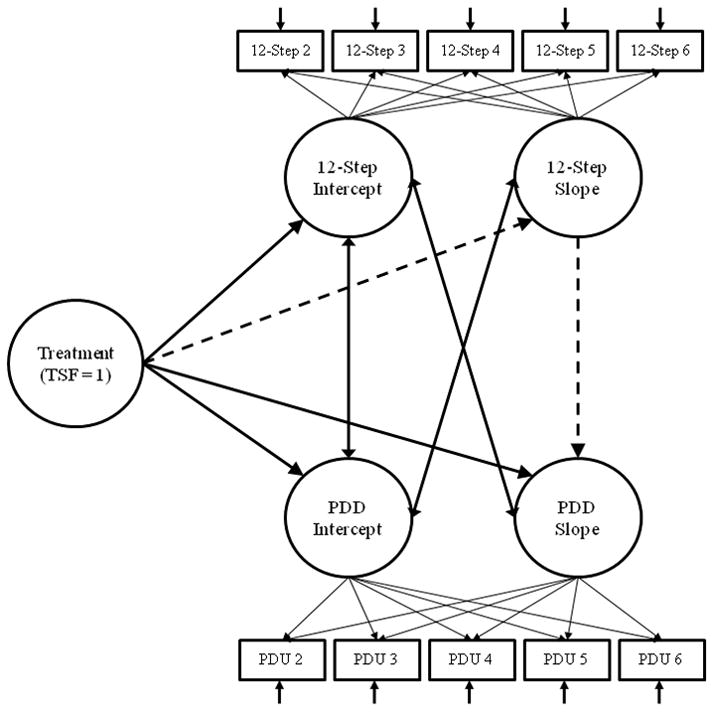
Latent growth curve mediation model with treatment group predicting post-treatment change in 12-step involvement, which in turn predicts post-treatment change in percent days drinking (PDD). Dotted line represents mediation path.
Results
12-step Meeting Attendance and Affiliation
As shown in Figure 2, the ICBT and TSF groups differed in their longitudinal patterns of 12-step meeting attendance and affiliation from Month 6 to Month 18. We used LGMs to estimate the mean pattern of change and variability in 12-step variables separately for TSF and ICBT. For the TSF group, a quadratic LGM was an excellent fit to the data for 12-step affiliation (χ2(6, N = 91) = 2.76, p = .84, CFI = 1.00, RMSEA <.01) and attendance (χ2(6, N = 91) = 5.37, p = .50, CFI = 1.00, RMSEA < .01). At the mean level, the TSF group exhibited a significant decline in 12-step affiliation and meeting attendance from Month 6 to 18, with a significant deceleration in that decline as indicated by a positive, statistically significant quadratic slope (see Table 2). This nonlinear decline was likely due to a steep descent in the first 6 months following treatment (Month 6 to Month 12) with little change thereafter. There was significant individual variability in the intercept, linear slope, and quadratic slope for 12-step affiliation, but variability was significant only in the intercept for 12-step meeting attendance. For the ICBT group, a linear LGM was a good fit to the data for 12-step affiliation (χ2(10, N = 105) = 12.26, p = .27, CFI = 0.99, RMSEA = .05) and attendance (χ2(10, N = 105) = 8.52, p = .58, CFI = 1.00, RMSEA = .05). In contrast to TSF, the ICBT group exhibited no significant increase or decrease in 12- step affiliation or meeting attendance, and no significant individual variability in the intercept or slope for either 12-step model (see Table 2).
Figure 2.

Group means of 12-step affiliation, 12-step attendance, drinking frequency, and drug use frequency for Twelve-Step Facilitation (TSF) and Integrated Cognitive-Behavioral Therapy (ICBT).
Table 2.
Results from unconditional latent growth curve models of 12-step affiliation and meeting attendance separately for Twelve-Step Facilitation and Integrated Cognitive-Behavioral Therapy.
| TSF | ICBT | |||
|---|---|---|---|---|
|
| ||||
| Mean (SE) | Variance (SE) | Mean (SE) | Variance (SE) | |
| 12-step affiliation | ||||
| Latent intercept | 2.54 (.15)*** | 1.74 (.46)*** | 1.86 (.13)*** | 1.15 (.23)*** |
| Linear slope | −.61 (.15)*** | 1.11 (.37)** | −.06 (.03) | .01 (.02) |
| Quadratic slope | .11 (.03)** | .05 (.02)* | - | - |
| 12-step attendance | ||||
| Latent intercept | .44 (.03)*** | .07 (.02)** | .26 (.03)*** | .05 (.01)*** |
| Linear slope | −.13 (.02)*** | .006 (.01) | −.002 (.008) | .002 (.001) |
| Quadratic slope | .02 (.005)*** | .000 (.001) | - | - |
TSF: Twelve-Step Facilitation; ICBT: Integrated Cognitive-Behavioral Therapy
p < .05,
p < .01,
p < .001.
To examine whether patients in the TSF and ICBT groups differed significantly in their longitudinal patterns of 12-step affiliation and attendance, we conducted conditional LGMs with the full sample, using a dummy-coded treatment group variable (ICBT = 0, TSF = 1) as a predictor of 12-step affiliation and attendance growth factors. The linear LGM was an adequate fit for 12-step affiliation (χ2(13, N = 196) = 36.21, p < .01, CFI = .94, RMSEA = .09) and a good fit for meeting attendance (χ2(13, N = 196) = 20.65, p = .08, CFI = .98, RMSEA = .06). Compared to ICBT, individuals in TSF had significantly greater intercepts of 12-step affiliation (b = .45, SE = .20, p = .02) and meeting attendance (b = .14, SE = .04, p = .001). However, TSF also predicted significantly greater decline in 12-step affiliation (b = −.11, SE = .05, p = .03) and attendance (b = −.04, SE = .01, p = .003) from Month 6 to Month 18. These results indicate that while veterans in TSF had greater levels of 12-step involvement at end-of-treatment, their 12-step affiliation and meeting attendance declined to a greater extent than the ICBT group during the 12 months of follow-up.
Alcohol and Drug Use Outcomes
To examine changes in alcohol and drug use, we first estimated separate unconditional LGMs for percent days drinking (PDD) and percent days using drugs (PDDRG) from Month 6 to Month 18. The linear LGM was an excellent fit to the data for PDD (χ2(7, N = 201) = 5.025, p < .001, CFI = 1.00, RMSEA < .01) and PDDRG (χ2(8, N = 201) = 12.85, p = .12, CFI = .98, RMSEA = .06). At the mean level there was a significant increase from Month 6 to Month 18 in PDD but no significant change in PDDRG (see Table 3). The variance estimates for growth factors (e.g., intercept, linear slope) revealed significant individual variability in the intercept and slope for PDD and PDDRG. Thus, while the mean pattern of change was an increase in alcohol use and no change in drug use, there was considerable individual variability in the initial level and change over time in frequency of drinking and drug use.
Table 3.
Results from latent growth curve models of percent days drinking and percent days using drugs from Month 6 (End of treatment) to Month 18 for veterans with substance dependence and major depression.
| % Days Drinking | % Days Using Drugs | |||
|---|---|---|---|---|
| Intercept | Slope | Intercept | Slope | |
|
|
|
|||
| Unconditional model | ||||
| Mean | 8.70*** | 0.99* | 3.28*** | 0.46 |
| Variance | 217.67*** | 20.45*** | 74.78*** | 5.61*** |
| Conditional models | b or r (SE) | b or r (SE) | b or r (SE) | b or r (SE) |
| Treatment group (TSF vs. ICBT) | −.10 | .20* | −.002 | .09 |
| 12-step affiliation model | ||||
| Treatment group (TSF vs. ICBT) | −.10 | −.15 | −.003 | −.07 |
| 12-step affiliation intercept | −.40*** | .25 | −.09 | −.03 |
| 12-step affiliation slope | .57* | −.93** | .14 | −.43 |
| 12-step attendance model | ||||
| Treatment group (TSF vs. ICBT) | −.10 | −.07 | −.003 | −.08 |
| 12-step attendance intercept | −.29** | .10 | −.09 | −.05 |
| 12-step attendance slope | .37* | −.63** | .26 | −.42 |
TSF: Twelve-Step Facilitation; ICBT: Integrated Cognitive-Behavioral Therapy
p < .05,
p < .01,
p < .001.
In the conditional model there were no treatment group differences in PDD intercepts, but TSF predicted significantly greater PDD slopes over time (see Table 3). Treatment group did not significantly predict PDDRG intercepts or slopes. These results indicated that patients in TSF increased in drinking frequency more than patients in ICBT during the year-long follow-up, and that there were no group differences in the end-of-treatment drinking frequency, end-of-treatment drug use frequency, or rate of change in drug use over time.
Changes in 12-step involvement predicting alcohol and drug use
We then used the LGMs for 12-step and affiliation to predict individual differences in the end-of-treatment level (intercept) and rate of change in alcohol and drug use (linear slope) from Month 6 to Month 18. In separate models the slopes for 12-step affiliation and meeting attendance were utilized as mediating variables between treatment group and the slopes for PDD and PDDRG (see dashed lines in Figure 1), to test whether the greater increases in PDD over time for TSF patients were explained by greater decreases in 12-step variables. Results from these analyses are presented in Table 3. The PDD intercept was significantly and negatively correlated with the intercepts for 12-step affiliation and meeting attendance, indicating that individuals with greater levels of affiliation and meeting attendance at end-of-treatment were also drinking less frequently at end-of-treatment. The PDD intercept was significantly and positively correlated with the slopes for 12-step affiliation and attendance, indicating that individuals with lower PDD at end-of-treatment had greater decreases in their 12-step affiliation and attendance during follow-up. Finally, the slopes for 12-step affiliation and meeting attendance were strongly, negatively predictive of PDD slope. This indicated that individuals with greater decreases in 12-step affiliation and meeting attendance from Month 6 to Month 18 had greater increases in PDD over time. As shown by asymmetric 95% confidence intervals obtained via the bias-corrected bootstrap procedure, the indirect effects of treatment group on PDD through slopes of 12-step affiliation (ab = 3.30, 95% CI [.67, 16.54]) and meeting attendance (ab = 2.41, 95% CI [.47, 6.47]) were statistically significant. These results indicate that the greater relative increases in PDD for the TSF patients were mediated by (and possibly attributable to) their greater relative decreases in 12-step affiliation and meeting attendance. There were no significant relations between intercepts and slopes of the 12-step variables and PDDRG (see Table 3), indicating that the end-of-treatment level and change during follow-up for drug use frequency was unrelated to end-of-treatment level or change during follow-up for 12-step affiliation or meeting attendance.
Discussion
This study examined post-treatment change in 12-step affiliation and meeting attendance and related effects on substance use outcomes in a sample of veterans with comorbid substance dependence and major depression who received six months of group treatment with TSF or ICBT. Because fewer studies of mediating variables have focused on substance-dependent patients with psychiatric comorbidity, there is relatively less knowledge about processes that sustain long-term change in their substance use outcomes. This study adds to the existing literature by examining post-treatment trajectories of change in 12-step affiliation and attendance in comorbid patients, determining whether treatment condition predicts individual differences in these trajectories, and reporting the mediational effects of reduced 12-step involvement on long-term substance use outcomes.
Veterans in the TSF condition had greater levels of 12-step affiliation and meeting attendance at end-of-treatment than those in ICBT. This is consistent with prior studies of this sample (20,34) and shows that a professionally-delivered TSF intervention can enable greater levels of 12-step involvement than other psychotherapies during active treatment. However, veterans in TSF also evinced a significant nonlinear decline in both 12-step affiliation and meeting attendance during the one year follow-up, while those in ICBT had no significant change. Previous studies of non-comorbid patients found no post-treatment decline in affiliation or meeting attendance following 12-step interventions (18,21). Our contrasting findings suggest comorbid MDD may interfere with continued attendance at 12-step meetings and affiliation with prescribed 12-step behaviors, even when patients are relatively successful at achieving these goals during active TSF. Potential explanatory mechanisms behind this finding are beyond our current scope, but could be related to persistent depressive symptoms and related low motivation, the sudden absence of accountability provided by a formal treatment group, or difficulty in establishing firm social bonds in 12-step meetings for patients with comorbid MDD. Some patients were evidently successful at sustaining 12-step affiliation as revealed by significant individual variance estimates, but modifications to TSF or continued contact may be necessary to achieve the desired long-term results in the majority of patients with comorbid MDD.
Independent of treatment condition, individuals with greater decreases in 12-step affiliation and meeting attendance also had greater increases in drinking frequency during the one-year follow-up. As evidenced by strong standardized coefficients in our latent growth curve models, post-treatment change in 12-step involvement likely plays a large role in determining whether patients with comorbid substance dependence and MDD experience post-treatment increases in drinking. Similar to a prior report of follow-up substance use outcomes in this sample (24), the current study found patients in TSF had greater post-treatment increases in drinking frequency than those in the ICBT condition. We also determined this group difference was mediated through reductions in 12-step affiliation and meeting attendance, which provides a possible explanation for the worse outcomes over time for TSF and supports the long-term efficacy of ICBT. During follow-up the ICBT group as a whole did not increase or decrease in 12-step affiliation or meeting attendance, but their mean levels of attendance and affiliation remained consistently greater than zero. Although it was not a prescribed element of treatment, there is apparently a subset of patients in ICBT who continue 12-step involvement. Superior long-term patterns in other mediating variables (e.g., self-efficacy, social support) may have also occurred for the ICBT condition, and future studies will explore other potential factors related to their superior post-treatment drinking outcomes.
Limitations of this study include the restricted demographic characteristics of the veteran sample (e.g., heavily male, mostly Caucasian) which curtails the immediate generalizability of these findings. Because we tested relations between concurrent changes in 12-step involvement and substance use, we cannot make conclusions about causal relationships, but other elements of our design and findings (e.g., mediation testing, dose-response relationship) enhance the plausibility of causal conclusions (35). Our measures did not differentiate between different types of 12-step meetings (e.g., Alcoholics vs. Narcotics Anonymous), which could have helped explain the lack of findings for drug use outcomes, and future work might benefit from more detailed measures of 12-step involvement. Also, because our 12-step measures were relatively brief, there may have been important aspects of these behaviors we did not consider. Finally, while the results have important implications for the broader population of individuals with substance dependence and MDD, replication in other samples and settings is needed.
Footnotes
Clinical trials registration: Clinicaltrials.gov identifiers NCT00108407 and NCT00018655.
Declarations of interest: Research funded by Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Clinical Sciences Research & Development Merit Review Awards to Dr. Sandra A. Brown and Dr. Susan R. Tate, and by National Institute on Drug Abuse fellowship grant (F31DA030861) awarded to Matthew J. Worley.
Contributor Information
Matthew J. Worley, San Diego State University/University of California, San Diego Joint Doctoral Program in Clinical Psychology
Susan R. Tate, San Diego Veterans Affairs Healthcare System and University of California, San Diego
John R. McQuaid, San Francisco Veterans Affairs Medical Center
Eric L. Granholm, San Diego Veterans Affairs Healthcare System and University of California, San Diego, Department of Psychiatry
Sandra A. Brown, University of California, San Diego
References
- 1.Grant BF, Stinson FS, Dawson DA, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: Results from the national epidemiologic survey on alcohol and related conditions. Archives of General Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- 2.Hasin D, Liu X, Nunes E, McCloud S, Samet S, Endicott J. Effects of major depression on remission and relapse of substance dependence. Archives of General Psychiatry. 2002;59:375–380. doi: 10.1001/archpsyc.59.4.375. [DOI] [PubMed] [Google Scholar]
- 3.Bolton JM, Pagura J, Enns MW, Grant B, Sareen J. A population-based longitudinal study of risk factors for suicide attempts in major depressive disorder. Journal of psychiatric research. 2010;44:817–826. doi: 10.1016/j.jpsychires.2010.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mark TL. The costs of treating persons with depression and alcoholism compared with depression alone. Psychiat Serv. 2003;54:1095–1097. doi: 10.1176/appi.ps.54.8.1095. [DOI] [PubMed] [Google Scholar]
- 5.Druss BG, Rosenheck RA. Patterns of health care costs associated with depression and substance abuse in a national sample. Psychiat Serv. 1999;50:214–218. doi: 10.1176/ps.50.2.214. [DOI] [PubMed] [Google Scholar]
- 6.Chi FW, Satre DD, Weisner C. Chemical dependency patients with cooccurring psychiatric diagnoses: service patterns and 1-year outcomes. Alcoholism: Clinical and Experimental Research. 2006;30:851–859. doi: 10.1111/j.1530-0277.2006.00100.x. [DOI] [PubMed] [Google Scholar]
- 7.Curran GM, Flynn HA, Kirchner J, Booth BM. Depression after alcohol treatment as a risk factor for relapse among male veterans. Journal of substance abuse treatment. 2000;19:259–265. doi: 10.1016/s0740-5472(00)00107-0. [DOI] [PubMed] [Google Scholar]
- 8.Gamble SA, Conner KR, Talbot NL, Yu Q, Tu XM, Connors GJ. Effects of pretreatment and posttreatment depressive symptoms on alcohol consumption following treatment in Project MATCH. Journal of Studies on Alcohol and Drugs. 2010;71:71–77. doi: 10.15288/jsad.2010.71.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Levin FR, Bisaga A, Raby W, et al. Effects of major depressive disorder and attention-deficit/hyperactivity disorder on the outcome of treatment for cocaine dependence. Journal of substance abuse treatment. 2008;34:80–89. doi: 10.1016/j.jsat.2006.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Glasner-Edwards S, Marinelli-Casey P, Hillhouse M, Ang A, Mooney LJ, Rawson R. Depression among methamphetamine users: association with outcomes from the Methamphetamine Treatment Project at 3-year follow-up. Journal of Nervous and Mental Disease. 2009;197:225–231. doi: 10.1097/NMD.0b013e31819db6fe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Longabaugh R. The search for mechanisms of change in behavioral treatments for alcohol use disorders: a commentary. Alcoholism: Clinical and Experimental Research. 2007;31:21s–32s. doi: 10.1111/j.1530-0277.2007.00490.x. [DOI] [PubMed] [Google Scholar]
- 12.Longabaugh R, Donovan DM, Karno MP, McCrady BS, Morgenstern J, Tonigan JS. Active ingredients: How and why evidence-based alcohol behavioral treatment interventions work. Alcoholism: Clinical and Experimental Research. 2005;29:235–247. doi: 10.1097/01.alc.0000153541.78005.1f. [DOI] [PubMed] [Google Scholar]
- 13.Ouimette PC, Moos RH, Finney JW. Influence of outpatient treatment and 12-step group involvement on one-year substance abuse treatment outcomes. Journal of Studies on Alcohol. 1998;59:513–522. doi: 10.15288/jsa.1998.59.513. [DOI] [PubMed] [Google Scholar]
- 14.Tonigan JS, Toscova R, Miller WR. Meta-analysis of the literature on Alcoholics Anonymous: sample and study characteristics moderate findings. Journal of Studies on Alcohol. 1996;57:65–72. doi: 10.15288/jsa.1996.57.65. [DOI] [PubMed] [Google Scholar]
- 15.Bogenschutz MP, Geppert CM, George J. The role of twelve-step approaches in dual diagnosis treatment and recovery. Am J Addiction. 2006;15:50–60. doi: 10.1080/10550490500419060. [DOI] [PubMed] [Google Scholar]
- 16.Kelly JF, McKellar JD, Moos R. Major depression in patients with substance use disorders: Relationship to 12-Step self-help involvement and substance use outcomes. Addiction. 2003;98:499–508. doi: 10.1046/j.1360-0443.2003.t01-1-00294.x. [DOI] [PubMed] [Google Scholar]
- 17.Timko C, Debenedetti A, Billow R. Intensive referral to 12-Step self-help groups and 6-month substance use disorder outcomes. Addiction. 2006;101:678–688. doi: 10.1111/j.1360-0443.2006.01391.x. [DOI] [PubMed] [Google Scholar]
- 18.Walitzer KS, Dermen KH, Barrick C. Facilitating involvement in Alcoholics Anonymous during out-patient treatment: a randomized clinical trial. Addiction. 2009;104:391–401. doi: 10.1111/j.1360-0443.2008.02467.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Subbaraman MS, Kaskutas LA, Zemore S. Sponsorship and service as mediators of the effects of Making Alcoholics Anonymous Easier (MAAEZ), a 12-step facilitation intervention. Drug and Alcohol Dependence. 2011;116:117–124. doi: 10.1016/j.drugalcdep.2010.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Glasner-Edwards S, Tate SR, McQuaid JR, Cummins K, Granholm E, Brown SA. Mechanisms of action in integrated cognitive-behavioral treatment versus twelve-step facilitation for substance-dependent adults with comorbid major depression. Journal of Studies on Alcohol and Drugs. 2007;68:663–672. doi: 10.15288/jsad.2007.68.663. [DOI] [PubMed] [Google Scholar]
- 21.Kahler CW, Read JP, Ramsey SE, Stuart GL, McCrady BS, Brown RA. Motivational enhancement for 12-step involvement among patients undergoing alcohol detoxification. Journal of Consulting and Clinical Psychology. 2004;72:736–741. doi: 10.1037/0022-006X.72.4.736. [DOI] [PubMed] [Google Scholar]
- 22.Rychtarik RG, Connors GJ, Dermen KH, Stasiewicz PR. Alcoholics Anonymous and the use of medications to prevent relapse: an anonymous survey of member attitudes. Journal of Studies on Alcohol. 2000;61:134–138. doi: 10.15288/jsa.2000.61.134. [DOI] [PubMed] [Google Scholar]
- 23.Brown SA, Glasner-Edwards SV, Tate SR, McQuaid JR, Chalekian J, Granholm E. Integrated cognitive behavioral therapy versus twelve-step facilitation therapy for substance-dependent adults with depressive disorders. Journal of Psychoactive Drugs. 2006;38:449–460. doi: 10.1080/02791072.2006.10400584. [DOI] [PubMed] [Google Scholar]
- 24.Lydecker KP, Tate SR, Cummins KM, McQuaid J, Granholm E, Brown SA. Clinical outcomes of an integrated treatment for depression and substance use disorders. Psychology of Addictive Behaviors. 2010;24:453–465. doi: 10.1037/a0019943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Project Match Research Group. Matching Alcoholism Treatments to Client Heterogeneity: Project MATCH posttreatment drinking outcomes. Journal of Studies on Alcohol. 1997;58:7–29. [PubMed] [Google Scholar]
- 26.Muñoz RF, Ying Y-W. The Prevention of Depression: Research and Practice. Baltimore: Johns Hopkins University Press; 1993. [Google Scholar]
- 27.Kadden RM. Cognitive-behavioral coping skills therapy manual: a clinical research guide for therapists treating individuals with alcohol abuse and dependence. Rockville, Md: U.S. Dept. of Health and Human Services, Public Health Service, National Institutes of Health, National Institute on Alcohol Abuse and Alcoholism; 1995. [Google Scholar]
- 28.Humphreys K, Kaskutas LA, Weisner C. The Alcoholics Anonymous Affiliation Scale: Development, reliability, and norms for diverse treated and untreated populations. Alcoholism: Clinical and Experimental Research. 1998;22:974–978. doi: 10.1111/j.1530-0277.1998.tb03691.x. [DOI] [PubMed] [Google Scholar]
- 29.Weiss RD, Griffin ML, Gallop RJ, et al. The effect of 12-step self-help group attendance and participation on drug use outcomes among cocaine-dependent patients. Drug and Alcohol Dependence. 2005;77:177–184. doi: 10.1016/j.drugalcdep.2004.08.012. [DOI] [PubMed] [Google Scholar]
- 30.Sobell LC, Sobell MB. Timeline follow-back: A technique for assessing self-reported alcohol consumption. In: Litten RZ, Allen JP, editors. Measuring alcohol consumption: Psychosocial and biochemical methods. Totowa, NJ: Humana Press; 1992. pp. 41–72. [Google Scholar]
- 31.Maisto SA, Sobell MB, Sobell LC. Reliability of self-reports of low ethanol consumption by problem drinkers over 18 months of follow-up. Drug and Alcohol Dependence. 1982;9:273–278. doi: 10.1016/0376-8716(82)90066-7. [DOI] [PubMed] [Google Scholar]
- 32.MacKinnon DP. Introduction to statistical mediation analysis. New York: Lawrence Erlbaum Associates; 2008. [Google Scholar]
- 33.MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological methods. 2002;7:83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Worley MJ, Tate SR, Brown SA. Mediational Relations between 12-step Meeting Attendance, Depression, and Substance Use during and after Treatment for Comorbidity. doi: 10.1111/j.1360-0443.2012.03943.x. under review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nock MK. Conceptual and design essentials for evaluating mechanisms of change. Alcoholism: Clinical and Experimental Research. 2007;31:4s–12s. doi: 10.1111/j.1530-0277.2007.00488.x. [DOI] [PubMed] [Google Scholar]


