Abstract
This study investigates the 10-year course and impact of AA-related helping (AAH), step-work, and meeting attendance on long-term outcomes. Data were derived from 226 treatment-seeking alcoholics recruited from an outpatient site in Project MATCH and followed for 10 years post-treatment. Alcohol consumption, AA participation, and other-oriented behavior were assessed at baseline, end of the 3-month treatment period, and one year, three years, and 10 years post-treatment. Controlling for explanatory baseline and time-varying variables, results showed significant direct effects of AAH and meeting attendance on reduced alcohol outcomes and a direct effect of AAH on improved other-oriented interest.
Keywords: Alcoholics Anonymous, Project MATCH, Meeting Attendance, Step-work, AA-related helping
INTRODUCTION
Alcoholics Anonymous (AA) has distinguished itself within the alcohol problems arena through its membership size and geographical dispersion (more than 2.1 million members and 100,766 groups in 150 countries), its influence on the modern treatment of alcohol use disorders, and through the volume and growing methodological rigor of research studies on the effects of AA participation (1–3). Meta-analytic reviews of the effects of AA involvement report a positive association between AA participation and abstinence across diverse populations as well as reductions in substance-related health care costs (4–8). Efforts to date to isolate the active ingredients of AA participation have focused primarily on meeting attendance, step-work, and service (9,10). Meeting attendance has been associated with abstinence and a higher number of sober friends (11–13). More step-work at a 3-year follow-up has been associated with decreased alcohol consumption at a 10-year follow-up (14) AA-related helping activities (AAH) are associated with greater abstinence at 1-year and 3-year follow-ups and reduced depression (15–20).
There are several theoretical interpretations of the evolution of service within the 12-step program. First, AAH can be viewed as an application of Riesman’s “helper therapy principle (HTP)”; one’s own problems diminish through the process of helping others (21). AAH applies the long “wounded healer” tradition whereby survivors of a life-altering disorder or experience develop special sensitivities, insights, and skills to be uniquely helpful to others with the same condition (22,23) —a process AA’s co-founder Bill Wilson characterized as “the sublime paradox of strength coming out of weakness”(24). Second, just as an evolutionarily adaptive gene may promote the replication and survival of a particular species (25), AA’s primary purpose, to stay sober and help other alcoholics, may have evolved to sustain the program’s survival. Service positions such as chairperson or secretary further ongoing AA group functioning. Third, AAH can also be understood within AA’s posited theory of self-centeredness as a central factor in the development and maintenance of alcoholism. AA’s main textbook is filled with admonitions of the dangers of selfishness, self-centeredness, self-absorption, self-justification, self-pity, and self-deception. The collective experience of AA’s original 100 members acknowledges self-knowledge, self-reliance, self-control, and self-sufficiency as failed paths to sustaining sobriety (26). Whereas mutual aid alcoholic societies in the 19th century viewed self-assertion as liberating the alcoholic from the disease (27,28), AA’s founders characterized the illness as stemming from the “bondage of self” (26) which could only be broken by personal surrender and self-transcendence.
AA’s main textbook emphasizes key exercises for ego reduction, which others reference as the foundation of recovery (29,30). The AA recovery process involves: a) surrender--admission of powerlessness and personal limitations (Step 1) (“…we had to quit playing God”); b) transcendence of self via reliance on a power greater than self (Step 2); c) witnessed confession of wrongs done to others (Step 5); d) repair of family and social relationships through making amends (Step 9); e) carrying a message of hope to other alcoholics (Step 12), which is often done in ritualized storytelling within a community of recovering people; and f) personal anonymity as a spiritual principle--a metaphoric and literal shedding of self (Tradition 4) (31). Seen in this light, AA is not a “self-help” program but a mutual-help program that rests on the premonition that sustained sobriety cannot be achieved alone (32). AAH enacts many of these exercises designed to increase other-orientation and self-transcendence which occurs quickly for some and slowly for others.
Long-term, prospective study of the course of AA participation across major programmatic activities and impact on behavior is limited. Of the few studies with 5-years or more follow-up post-treatment, Kaskutas and colleagues (33) delineated four long-term patterns regarding AA meeting attendance: 1) low, 2) medium, 3) descending, and 4) high, with highest meeting attendance occurring in the first year following treatment. Long-term participation patterns in other program activities such as step-work and AAH are less clear. While higher meeting attendance in the initial post-treatment period is associated with more improved drinking outcomes (7,34–49), few have studied the long-term influence of other major components on decreased substance use. Further, long-term alcohol investigations of AA’s impact on clinical outcomes beyond drinking are rare. A handful of early studies considered the potential effect of AA participation on a transformation from self-centeredness to increased other-orientation (29,50). Reinert and colleagues (51,52) hypothesized a decline in self orientation with increased years in recovery, but did not find such declines over short periods of time in a sample of AA members. However, increased other-regard, if it occurs through such mechanisms as step-work or AAH, may span years of AA participation.
This paper builds upon prior prospective AAH research to explore the course and impact of AA participation across three major programmatic activities: meeting attendance, step-work, and AAH. In this study, we examine: 1) the 10-year course of AA participation, drinking, and other-oriented behavior, 2) the influence of 12-step facilitated treatment (TSF) on AA programmatic activities and outcomes over time, and 3) the influence of time-varying participation in AA programmatic activities on subsequent drinking and other-oriented behavior.
METHODS
Participants
Data were derived from Project MATCH, a prospective longitudinal investigation of the efficacies of three behavioral treatments for alcohol use disorders delivered over a 3-month treatment period (53). Project MATCH recruited subjects from 4 aftercare sites (n = 774; 80% male) and 5 outpatient sites (n = 952; 72% male). This report presents 10-year outcome data collected at one outpatient site in Project MATCH (n = 226). At intake, the clinical profile of the study sample was similar to other outpatient site samples in Project MATCH, with exception to being younger at intake (P < .0001), less education (P < .0001), and greater Hispanic representation (P < .0001, Table 1). During follow-up, over 85% of the original 952 outpatients in Project MATCH was retained in the three years post-treatment, with no significant site differences in attrition (54,55).
Table 1.
Baseline Characteristics of Outpatient Sites in Project MATCH
| Outpatient Site | |||||
|---|---|---|---|---|---|
| Variable | Albuquerque | Buffalo | Farmington | Milwaukee | West Haven |
|
| |||||
| 226 (24%) | 200 (21%) | 201 (21%) | 178 (19%) | 147 (15%) | |
| Male | 166 (73%) | 140 (70%) | 145 (72%) | 115 (65%) | 122 (83%) |
| Caucasian | 120 (53%) | 173 (87%) | 190 (95%) | 165 (93%) | 135 (92%) |
| Hispanic | 103 (46%)*** | 2 (1%) | 3 (1%) | 4 (2%) | 4 (3%) |
| Married | 44 (19%)*** | 72 (36%) | 98 (49%) | 59 (33%) | 68 (46%) |
| Employed Fulltime | 95 (42%) | 79 (40%) | 125 (62%) | 103 (58%) | 83 (56%) |
| ASPD | 28 (14%) | 14 (7%) | 11 (6%) | 21 (12%) | 7 (6%) |
| Treatment Assignment | |||||
| CBT | 72 (32%) | 67 (33%) | 61 (30%) | 51 (29%) | 50 (34%) |
| MET | 79 (35%) | 72 (36%) | 66 (33%) | 55 (31%) | 44 (30%) |
| TSF | 75 (33%) | 61 (31%) | 74 (37%) | 72 (40%) | 53 (36%) |
| Age (M, SD) | 33.25 (8.50)*** | 40.17 (10.62) | 41.93 (10.07) | 37.53 (10.66) | 43.25 (11.01) |
| Education (M,SD) | 12.70 (1.90)*** | 13.50 (2.09) | 14.16 (2.16) | 13.50 (2.13) | 13.49 (2.24) |
| PDA (M,SD) | 36.45 (8.47) | 31.25 (6.93) | 28.49 (7.60) | 43.50 (7.07) | 31.83 (9.40) |
| Prior Treatment (M, SD) | 1.11 (2.89) | 0.83 (1.67) | 0.82 (1.32) | 1.17 (1.75) | 1.30 (1.92) |
| AA Attendance (M,SD) | 0.03 (0.08) | 0.02 (0.06) | 0.04 (0.12) | 0.02 (0.07) | 0.05 (0.14) |
P<.05,
P<.01,
P<.001,
P<.0001
Extensive attritional analyses also compared study participants who did and did not complete a 10-year interview, which was completed on average 117 months (SD = 9.54) post-randomization. Of the original 226 outpatient subjects, 23 (10%) did not provide consent for the 10-year follow-up interview and 22 (10%) had died since the 39-month interview, confirmed by obituaries death certificates from the New Mexico Office of Medical Records. Of the surviving, eligible subjects (n = 181), 148 (82%) completed a 10-year follow-up interview, 28 (15%) were unable to be located, and 5 (3%) refused to participate. There were no significant differences between study participants with and without 10-year evaluations (Table 2).
Table 2.
Baseline Characteristics of Outpatient Sample by 10-Year Interview Status
| Participant Status at 10-Year Interview | |||||
|---|---|---|---|---|---|
| Variable | Interview Completed | Ineligible | Refused | Deceased | Unable to Schedule |
|
| |||||
| 148 (66%) | 23 (10%) | 5 (2%) | 22 (10%) | 28 (2%) | |
| Male | 104 (70%) | 19 (83%) | 4 (80%) | 17 (77%) | 22 (79%) |
| Caucasian | 71 (48%) | 13 (57%) | 4 (80%) | 16 (73%) | 16 (57%) |
| Hispanic | 75 (51%) | 10 (43%) | 1 (20%) | 6 (27%) | 11 (39%) |
| Married | 35 (24%) | 4 (17%) | 1 (20%) | 1 (6%) | 368 (11%) |
| Employed Fulltime | 65 (44%) | 10 (43%) | 3 (60%) | 7 (32%) | 10 (36%) |
| ASPD | 16 (13%) | 7 (35%) | 1(20%) | 3 (16%) | 1 (4%) |
| Treatment Assignment | |||||
| CBT | 49 (33%) | 8 (35%) | 0 (0%) | 6 (27%) | 9 (32%) |
| MET | 48 (33%) | 11 (48%) | 4 (80%) | 7 (32%) | 9 (32%) |
| TSF | 51 (34%) | 4 (17%) | 1 (20%) | 9 (41%) | 10 (36%) |
| Age (M, SD) | 33.12 (8.56) | 32.43 (9.00) | 37.60 (10.41) | 36.18 (7.77) | 31.54 (11.01) |
| Education (M,SD) | 12.72 (1.97) | 12.57 (1.78) | 11.80 (0.45) | 12.91 (2.27) | 12.68 (1.47) |
| PDA (M,SD) | 36.21 (8.72) | 33.27 (9.59) | 44.11 (4.85) | 29.45 (9.00) | 43.29 (5.60) |
| Prior Treatment (M, SD) | 1.11 (3.43) | 1.09 (1.65) | 1.00 (1.73) | 1.50 (1.26) | 0.79 (1.07) |
| Meeting Attendance (M,SD) | 0.02 (0.07) | 0.03 (0.06) | 0.12 (0.23) | 0.04 (0.13) | 0.04 (0.07) |
|
| |||||
The general aims, research design, and organization of Project MATCH can be read about in detail elsewhere (56). The study procedures were approved by the Human Subjects Review Committee at University of New Mexico, written informed consent was obtained in accordance with the standards of the Committee on Human Experimentation with the Helsinki Declaration of 1975 (54,57), and a Certificate of Confidentiality from the National Institute on Alcohol Abuse and Alcoholism was obtained.
Measures
Background characteristics were assessed at baseline. Time-varying variables (percent days abstinent, 3 indices of AA participation, other-oriented interest) were assessed at baseline, 3-, 15-, 39-, and 120-months post-randomization.
Background Characteristics
Baseline demographic and clinical characteristics included gender, race, marital status, full-time employment status, age, years of education, anti-social personality disorder (ASPD), chemical dependency treatment history, and receipt of Twelve-step Facilitation (TSF). Receipt of TSF versus no TSF (Cognitive Behavioral Therapy, Motivational Enhancement Therapy) was ascertained from Project MATCH’s randomized treatment assignment (42).
Alcohol Use
Alcohol use was defined as percent days abstinent (PDA) using the semi-structured Form 90 (59). The Form 90 is a calendar-based daily drinking estimation method that incorporates a grid-averaging approach to provide a comprehensive and efficient assessment of a person’s drinking over a designated period of time (90 days in this study). It has demonstrated test-retest reliability for treatment-seeking alcoholics (60) and problem use of illicit drugs (61). Given the negatively skewed distribution, PDA variables received an arcsine transformation, as was done in the primary MATCH outcome analyses (54).
AA Participation
Three indices of AA participation variables were measured: 1) AAH, 2) AA meeting attendance (MTG), and 3) step-work. AAH was assessed with the 13-item Alcoholics Anonymous Involvement (AAI) questionnaire (62), a well-validated measure of AA affiliation developed for use in Project MATCH (62). Using criterion from prior work (9), AAH was defined by endorsement of two AAI items: being a sponsor and/or completion of the 12th step in the last 90 days. MTG was assessed from one item on the Form 90, “How many AA meetings have you attended in the past 90 days?” and converted into percent of days attending AA (number of days attending AA/ number of days in the assessment period), for a score ranging from .00–1.00. Because of a positively skewed distribution, MTG was log transformed. Step-work was measured from the continuous AAI item ascertaining completed steps (0–11) in the assessment period, and summed. Using Cohen’s effect size r estimates (63), there was a small correlation between AAH and MTG at any assessment (r = .18–.24, P < .001), a moderate correlation between AAH and step-work (r = .26–.43, P < .001), and a moderate correlation between MTG and step-work (r = .42–.60, P < .001).
Other-Oriented Interest (OOI)
One item from the Beck Depression Inventory (BDI;64) was used as an index of AA’s espoused behavior towards others (i.e., “…trying each day to be a little more thoughtful and considerate to those with whom we came in contact” (65; p356). With regard to interest in others in the past week, participants rated the OOI item from 0 (no loss of interest) to 3 (lost all interest). Similar single-item measures have been used in other alcohol investigations (66,67).
Statistical Analysis
Statistical analyses were performed using SAS version 9.1.3 (SAS Institute Inc., 2004). Depending on the type of variables (continuous or discrete), the Fisher’s Exact Test for binary variables or Kruskal-Wallis Chi-Square Test for continuous variables was performed to evaluate demographic and clinical differences between subjects. We used hierarchal linear modeling (HLM) to examine the course of time-varying variables (AA variables, outcomes). Variables were mean centered to reduce multi-collinearity (68).
We used pairs of time points in which time-varying AA covariates (AAH, meeting attendance, step-work) were analyzed in relation to lagged time-varying outcomes (e.g., AAH at 3-months predicting PDA at 15-months, AAH at 15-months predicting PDA at 39-months, and AAH at 39-months predicting PDA at 120-months). We used HLM to predict PDA, with adjustments for lack of independency among the multiple observations for each person. We used generalized estimation equations (GEE) methods to predict OOI, with an unstructured correlation matrix and correction for over-dispersion (69). A non-significant linear time co-efficient between data collected in the initial three years and at the ten year interview suggested no marked change in slope to raise concern of the interval time lag. All models controlled for baseline assessments of AA variables and the dependent variable. In addition, to help rule out the possibility that variables other than AA were responsible for improved outcomes, we included baseline covariates linked to treatment outcomes: gender, age, marital status (married/not married), race/ethnicity, full-time employment (yes/no), ASPD diagnosis (yes/no), and prior treatments (14,16). To achieve this, we used an empirical backward elimination procedure to test whether baseline covariates were related to outcomes. Results revealed that age, marital status, full-time employment, and prior treatments were significantly related to study outcomes, and thus, were maintained as control variables. To limit hypothesis testing and to maintain the recommended 15:1 predictor/subject ratio (70), we first evaluated evidence of direct effects of TSF and time-varying AA variables on outcomes at any time during the study. Analytic models were then rerun to include all interaction terms between TSF, the time-varying AA variable, and time.
Although missing data patterns were non-monotone (i.e. intermittently missing), and importantly, not associated with PDA or OOI outcomes, we used the Markov Chain Monte Carlo (MCMC) method for multiple imputation (71,72). For any given assessment through month 39, data reconstruction for independent variables ranged from 4–6% for study participants. These rates are similar to those constructed for other outpatient samples in Project MATCH (73). The statistics reported for variables in our analyses are the averaged results across the ten imputations performed. The degrees of freedom for the reported t-statistics for each regression coefficient vary from analysis to analysis given the recommended use of adjusted degrees of freedom (74). When multicollinearity diagnostics of the two fitted models were examined, tolerances were .50 and above, indicating low concern of multicollinearity (69). We reported all two-tailed tests with significance values greater than 95% (P < .05).
RESULTS
Table 1 shows the demographic and clinical characteristics of the outpatient sample at baseline. The majority of participants were male (76%) and single (76%). Approximately half of the sample were Caucasian (48%), Hispanic (51%), and employed full-time (44%). On average, subjects were 33 years old (M = 33.12 years), had a high school diploma (M = 12.73 years of education), and 13% met diagnostic criteria for ASPD. Participants entered treatment with low PDA, few prior treatments, and low prior exposure to AA. Thirty-three percent (n = 75) of the outpatient sample was randomly assigned to TSF.
Course of Outcomes
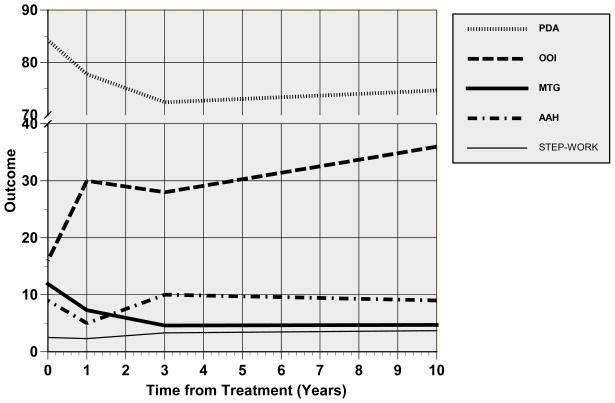
Figure 1 shows the population-averaged estimates of the 10-year course of PDA and OOI. A significant direct effect for time was found for PDA (F = 40.15, P < .0001) but not for OOI scores (F = 2.11, P = .15). The average PDA at the three month interview approximately doubled from baseline and declined thereafter. At no assessment did the rate of abstinence exceed 13%, a rate similar to other long-term investigations of problem drinkers (34). The proportion of subjects reporting some to all lost interest in others was lowest at the 3-month interview (16%), and returned to pre-treatment levels by the 120-month interview (36%). At any assessment, there was a small, negative correlation between PDA and OOI scores (rs = −0.16 thru −0.20, P < .001).
Figure 1. 10-Year Course of Outcomes and AA Participation.
NOTES:
aPDA = percent days abstinent in the assessment period; bOOI = other-oriented interest, proportion endorsing some to all lost OOI in the assessment period; cAAH = AA-related helping; dMTG = percent days attending AA in the assessment period; eSTEP-WORK = number of steps worked among participants working 1+ steps in the assessment period.
Course of AA Participation
The 10-year course of MTG, step-work, and AAH following the index treatment is shown in Figure 1. Significant fluctuations in MTG were observed over time (F = 10.82, P < .0001); as shown in Figure 1, MTG at the 3-month interview (0 years in Figure 1) more than doubled from baseline, declined by 6% at the 15-month interview (1 yr on Figure 1), further declined at the 39-month interview (3 years on Figure 1) to a level that was relatively constant at the 120-month interview. In contrast, the average number of steps completed remained low over the decade following the index treatment (F = 2.01, P = 0.11); notably, approximately two-thirds of the sample were not working any steps at any point. However, as shown in Figure 1, those who worked at least one step during the index treatment continued to progress in step-work over time (F = 10.21, P < .0001). The rate of AAH was also relatively constant over time (F = 2.62, P = .06); approximately 9–10% of the population were AAH participants at any point during follow-up. At the 15-month interview, however, only 5% of the outpatient sample was participating in AAH.
TSF and Course of AA Participation
During the 3-month treatment period, TSF recipients had greater participation in AAH (15% vs. 6%; χ2=5.17, p<.05), step-work (1+ steps worked, 68% vs. 29%; χ2 = 29.90, P < .0001), and MTG (M = 23.73 vs. M = 5.93, F = 38.81, P < .0001). At the 15-month interview, this pattern continued in TSF recipients in terms of greater participation in AAH (10% vs. 1%; χ2=10.54, p<.001), step work (1+ steps worked, 53% vs. 26%, χ2= 11.98, P < .001), but not MTG (F = 0.61, P = .23). However, TSF did not distinguish long-term AA participation patterns beyond the 15-month interview. Unrelated to TSF, AAH initiation steadily increased from 3% at the 15-month interview to 11% at each subsequent assessment. At any point in the study, AAH participants versus non-AAH participants had higher levels of MTG (F = 5.03, P < .0001) and step-work (F = 11.54, P < .0001).
AA Participation and Outcomes Over Time
Table 3 shows the parameter estimates of baseline covariates and time-varying covariates (variables assessed at each follow-up) in relation to PDA over time. Controlling for baseline covariates, results showed significant direct effects of MTG (P < .01) and AAH (P < .05) on PDA outcomes. Results also revealed age, prior treatment, and being married approached significance (P < .10). Similar to prior results found in Project MATCH (75), there was no significant direct effect of TSF nor interaction with time to indicate greater efficacy of TSF vs. other treatments on PDA during or following the index treatment episode.
Table 3.
Estimates and p values for final model of percent days abstinent over time in an outpatient sample in Project MATCHa
| Variable | β | CI Lower | CI Upper | t | P |
|---|---|---|---|---|---|
| Time-varying Covariates | |||||
| Follow-up Month1 | 0.027 | −0.313 | 0.170 | 1.04 | 0.299 |
| AAH2 | −0.041 | 0.059 | 0.380 | 1.81 | 0.033 |
| Meeting Attendance | 0.144 | 0.026 | 0.216 | 2.60 | 0.009 |
| Step-work3 | 0.045 | −0.086 | 0.176 | 0.65 | 0.519 |
| TSF Assignment | 0.095 | −0.102 | 0.294 | 0.95 | 0.341 |
| AAH X Month | 0.093 | −0.030 | 0.216 | 1.50 | 0.137 |
| Meeting Attendance X Month | −0.069 | −0.155 | 0.017 | −1.44 | 0.128 |
| Step-work X Month | −0.054 | −0.123 | 0.016 | −1.54 | 0.129 |
| TSF X Month | −0.068 | −0.154 | 0.017 | −1.48 | 0.122 |
| Baseline Covariates | |||||
| PDA4 | 0.263 | 0.146 | 0.380 | 4.43 | <.0001 |
| AAH | −0.117 | −0.313 | 0.169 | −0.58 | 0.562 |
| Meeting Attendance | −0.025 | −0.123 | 0.073 | −0.51 | 0.613 |
| Step-work | 0.047 | −0.101 | 0.194 | 0.63 | 0.531 |
| Age | −0.010 | −0.014 | −0.002 | −1.81 | 0.067 |
| Prior Treatment | 0.013 | 0.001 | 0.026 | 1.65 | 0.059 |
| Married | −0.103 | −0.216 | 0.011 | −1.78 | 0.077 |
Notes: Lagged-panel HLM results with multiple imputation;
Follow-up month after intake: 3-month, 15-month, 39-month, 120-month;
AAH = AA-related helping;
Step-work = no. of steps worked (1–11);
PDA=percent days abstinent.
Results also demonstrated significant direct effects of MTG (P < .05) and AAH (P < .05) on OOI outcomes (Table 4). The significant coefficient for AAH (−0.37) indicated an adjusted odds ratio of 0.69 (i.e., exp (−0.37)), the reciprocal of which translated into a 50% increased likelihood for AAH participants versus non-participants to be in the lower OOI category (i.e. higher interest in others), controlling for explanatory variables in the model. The coefficient for MTG (−0.126) revealed that with each one-unit increase in MTG, the odds of being in a lower OOI category rose by 13% (i.e. 100[exp(−.126)−1]. Prior treatment was significantly related to OOI (P < .05), whereas being married and TSF receipt approached significance (P < .10).
Table 4.
Estimates and p values for final model of other-oriented interest over time in an outpatient sample in Project MATCHa
| Variable | β | CI Lower | CI Upper | t | P |
|---|---|---|---|---|---|
| Time-varying Covariates | |||||
| Follow-up Month1 | 0.003 | −0.072 | 0.032 | 0.08 | 0.938 |
| AAH2 | −0.371 | −0.772 | −0.036 | −2.81 | 0.013 |
| Meeting Attendance | −0.126 | −0.252 | −0.026 | −2.00 | 0.033 |
| Step-work3 | −0.080 | −0.263 | 0.103 | −0.86 | 0.391 |
| TSF Assignment | −0.222 | −0.475 | 0.032 | −1.73 | 0.096 |
| AAH X Month | −0.052 | −0.227 | 0.122 | −0.59 | 0.556 |
| Meeting Attendance X Month | 0.031 | −0.057 | 0.119 | 0.68 | 0.496 |
| Step-work X Month | 0.043 | −0.043 | 0.129 | 0.99 | 0.323 |
| TSF X Month | 0.097 | −0.026 | 0.219 | 1.57 | 0.122 |
| Baseline Covariates | |||||
| OOI4 | 0.229 | 0.125 | 0.333 | 4.36 | <.0001 |
| AAH | −0.049 | −0.198 | 0.099 | −0.65 | 0.514 |
| Meeting Attendance | 0.005 | −0.122 | 0.134 | 0.90 | 0.368 |
| Step-work | 0.011 | −0.120 | 0.142 | 0.17 | 0.866 |
| Age | 0.001 | −0.007 | 0.009 | 0.28 | 0.783 |
| Prior Treatment | 0.013 | 0.001 | 0.025 | 2.20 | 0.028 |
| Married | 0.073 | −0.085 | 0.231 | 0.67 | 0.095 |
Notes:
Lagged-panel GEE results with multiple imputation;
Follow-up month after intake: 3-month, 15-month, 39-month, 120-month;
AAH = AA-related helping;
Step-work = no. of steps worked (1–11);
OOI = other-oriented interest.
DISCUSSION
This study provides a snapshot of what can be expected of outpatients’ AA participation in the decade following their index treatment and highlights the importance of meeting attendance and AAH to long-term behavioral change. Meeting attendance during treatment and in the following decade parallels patterns reported in other prospective 12-step investigations (76,77) meeting attendance was highest during treatment and steadily declined thereafter. In contrast, a relatively stable rate of AAH (9%) and low levels of step-work were observed during and following treatment. Despite a lowered rate of AAH at the 15-month assessment, AAH participants did more step-work and attended more meetings than non-AAH participants at any study interval. TSF treatment significantly boosted AAH participation and step-work relative to the other treatment conditions, but effects were lost after the initial year post-treatment. Extended effects of TSF beyond the initial year post-treatment may be seen with coordination of other 12-step facilitation approaches such as “Bridging the Gap” (78,79), or periodic booster sessions post-treatment, such as Case Monitoring (R01 AA009907; 80).
We next explored the relationship between participation in 3 AA programmatic activities on subsequent drinking and other-oriented behavior over time. Consistent with prior work (6–8,15,16,62), results showed direct effects of meeting attendance and AAH on greater abstinence across time, but not differential benefit of TSF. Controlling for pretreatment levels of OOI, those engaged in AAH were significantly more likely to report higher interest in others. These findings suggest the importance of meeting attendance to abstinence as a newcomer and in long-term recovery, and support AA’s suggestion to help others as way to stave off an urge to drink and increase interest in others.
There are several limitations of this study that warrant attention. This outpatient sample was representative of other outpatient sites in Project MATCH with exception to age and education. Findings may not generalize to non treatment-seeking populations or those with more severe addiction. However, alcohol consumption patterns were similar to 10-year course patterns observed in other samples of problem drinkers (34). Second, treatment effects in this study are limited to the randomized index treatment. Third, our estimates of AAH and OOI are likely to be on the low end of true rates given their 1–2 item assessments.
Limitations aside, this study is the first to explore the 10-year course of meeting attendance, step-work, and AAH and their concurrent influence on long-term outcomes. Psychometrically sound measures employed in Project MATCH were consistently collected at each study interval, with 10-years of month-to-month estimates of drinking outcomes reliably assessed with the Form-90. Other strengths of this study include: a high representation of Hispanic problem drinkers seeking outpatient treatment; an 82% retention rate at 10-years post-treatment; and advanced statistical techniques including multiple imputation that produced robust parameter estimates. The HLM methods employed controlled for all stable measured and unmeasured characteristics of subjects correlated with model covariates (69), thereby eliminating potentially large sources of bias.
Treatment provides a time-limited opportunity during which patients may be receptive to professional input and advice. The significant correlation in our study between worse alcohol outcomes and less interest in others suggests that clients may benefit from increasing other-oriented behaviors as part of their recovery program. The current practice of encouraging meeting attendance could be honed by encouraging service involvement at meetings that do not require extended sobriety time (e.g. helping setup chairs, tables, or coffee). Step-work activity during and following treatment was low; on average, two out of three alcoholics worked no steps during treatment and in the decade following. Formal step-work exercises, a common practice of treatment programs, may require more clinician guidance to increase clients’ understanding of steps worked and their completion. Future studies are warranted to explore the impact of working all 12-steps on behavioral change as well as sequencing of AAH activities in relation to length of time sober.
Acknowledgments
We would like to thank Stefan Padfield for his helpful comments regarding this manuscript. The authors acknowledge that the reported results are, in whole or in part, based on analyses of the Project MATCH Public Data Set and 10-year outcomes collected by an outpatient site in Project MATCH. These data were collected as part of a multisite clinical trial of alcoholism treatments, which was supported by a series of grants from NIAAA, and were made available to the authors by the Project MATCH Research Group. This paper was not reviewed or endorsed by the Project MATCH Research Group and does not necessarily represent the opinions of its members, who are not responsible for the contents.
This research was funded in part by a John Templeton Foundation grant awarded to Dr. Pagano, and National Institute on Alcohol Abuse and Alcoholism (NIAAA) grants awarded to Drs. Pagano (K01 AA015137), Stout and Kelly (R21 AA016762), and Tonigan (K02 AA00326).
Contributor Information
Maria E. Pagano, Email: mxp123@case.edu, Case Western Reserve University School of Medicine, Department of Psychiatry, Division of Child Psychiatry, WO Walker Building, 10524 Euclid Ave., Cleveland, OH, 44106
William L. White, Chestnut Health Systems, 3329 Sunset Key Circle #203, Punta Gorda, FL, 33955
John F. Kelly, Center for Addiction Medicine, Department of Psychiatry, Harvard Medical School, 60 Staniford St., Boston, MA, 02114
Robert L. Stout, Decision Sciences Institute, Pacific Institute for Research Evaluation, 1005 Main Street Pawtucket, RI, 02860
Rebecca R. Carter, Case Western Reserve University School of Medicine, Department of Psychiatry, Division of Child Psychiatry, WO Walker Building, 10524 Euclid Ave., Cleveland, OH, 44106.
J. Scott Tonigan, The University of New Mexico, Center on Alcoholism, Substance Abuse, and Addiction, 2650 Yale SE, Albuquerque, NM, 87106
References
- 1.Humphreys K. Circles of recovery: Self-help organizations for addictions. Cambridge, UK: Cambridge University Press; 2004. [Google Scholar]
- 2.Kelly JF, Yeterian J. Mutual-help groups. In: O’Donohue W, Cunningham JR, editors. Evidence-based adjunctive treatments. New York: Elsevier; 2008. pp. 61–106. [Google Scholar]
- 3.White W. Peer-based Addiction Recovery Support: History, Theory, Practice, and Scientific Evaluation. Chicago, IL: Great Lakes Addiction Technology Transfer Center and Philadelphia Department of Behavioral Health and Mental Retardation Services; 2009. [Google Scholar]
- 4.Emrick CD, Tonigan JS, Montgomery HA, Little L. Alcoholics Anonymous: what is currently known? In: McCrady BS, Miller WR, editors. Research on Alcoholics Anonymous: Opportunities and alternatives. Piscataway, NJ: Rutgers Center of Alcohol Studies; 1993. pp. 41–76. [Google Scholar]
- 5.Forcehimes A, Tonigan JS. Self-efficacy to remain abstinent and substance abuse: a meta-analysis. Alcoholism Treatment Quarterly. 2008;26:480–489. [Google Scholar]
- 6.Kelly J, Stout RL, Zywiak W, Schneider R. A 3-year study of addiction mutual-help group participation following intensive outpatient treatment. Alcoholism: Clinical and Experimental Research. 2006;30:1381–1392. doi: 10.1111/j.1530-0277.2006.00165.x. [DOI] [PubMed] [Google Scholar]
- 7.Moos RH, Moos BS. Participation in treatment and Alcoholics Anonymous: a 16-year follow-up of initially untreated individuals. Journal of Clinical Psychology. 2006;65:383–391. doi: 10.1002/jclp.20259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tonigan JS, Toscova R, Miller WR. Meta analysis of the literature on Alcoholics Anonymous: sample and study characteristics with moderate findings. Journal of Studies on Alcohol and Drugs. 1996;57:65–72. doi: 10.15288/jsa.1996.57.65. [DOI] [PubMed] [Google Scholar]
- 9.Moos RH. Active ingredients of substance use-focused self-help groups. Addiction. 2008;103:387–396. doi: 10.1111/j.1360-0443.2007.02111.x. [DOI] [PubMed] [Google Scholar]
- 10.Morgenstern J, Bux DA, Labouvie E, Morgan T, Blanchard KA, Muench F. Examining mechanisms of action in 12-Step community outpatient treatment. Drug and Alcohol Dependence. 2003;72:237–247. doi: 10.1016/j.drugalcdep.2003.07.002. [DOI] [PubMed] [Google Scholar]
- 11.Humphreys K, Mankowski ES, Moos RH, Finney JW. Do enhanced friendship networks and active coping mediate the self-help groups on substance abuse? Annals of Behavioral Medicine. 1999;21:54–60. doi: 10.1007/BF02895034. [DOI] [PubMed] [Google Scholar]
- 12.Morgenstern J, Kahler CW, Frey RM, Labouvie E. Modeling therapeutic response to 12-step treatment: optimal responders, nonresponders, and partial responders. Journal of Substance Abuse. 1996;8:45–59. doi: 10.1016/s0899-3289(96)90079-6. [DOI] [PubMed] [Google Scholar]
- 13.Zemore SE, Kaskutas LA. Helping, spirituality, and Alcoholics Anonymous in recovery. Journal of Studies on Alcohol and Drugs. 2004;65:383–391. doi: 10.15288/jsa.2004.65.383. [DOI] [PubMed] [Google Scholar]
- 14.Tonigan JS, Miller WR. AA practicing subtypes: are there multiple AA fellowships [abstract]? Alcoholism: Clinical and Experimental Research. 2005;29:384. [Google Scholar]
- 15.Pagano ME, Friend KB, Tonigan JS, Stout RL. Helping other alcoholics in Alcoholics Anonymous and drinking outcomes: findings from Project MATCH. Journal of Studies on Alcohol and Drugs. 2004;65:766–773. doi: 10.15288/jsa.2004.65.766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pagano ME, Zemore SE, Onder CC, Stout RL. Predictors of initial AA-related helping: findings from Project MATCH. Journal of Studies on Alcohol and Drugs. 2009;70:117–125. doi: 10.15288/jsad.2009.70.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tonigan JS, Rice SL. Is it beneficial to have an alcoholics anonymous sponsor? Psychology of Addictive Behaviors. 2010;24:397–403. doi: 10.1037/a0019013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zemore SE. Helping as healing among recovering alcoholics. Southern Medical Journal. 2007;100:447–450. doi: 10.1097/SMJ.0b013e31803175da. [DOI] [PubMed] [Google Scholar]
- 19.Zemore SE, Kaskutas LE, Ammon LN. In 12-Step groups, helping helps the helper. Addiction. 2004;99:1015–1023. doi: 10.1111/j.1360-0443.2004.00782.x. [DOI] [PubMed] [Google Scholar]
- 20.Pagano ME, Krentzman AR, Onder CC, et al. Service to Others in Sobriety (SOS) Alcoholism Treatment Quarterly. 2010;28:111–127. doi: 10.1080/07347321003656425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Riessman F. The ‘helper’ therapy principle. Social Work. 1965;10:27–32. [Google Scholar]
- 22.Jackson SW. The wounded healer. Bulletin of the History of Medicine. 2001;75:1–36. doi: 10.1353/bhm.2001.0025. [DOI] [PubMed] [Google Scholar]
- 23.White W. The History of Recovered People as Wounded Healers: from native America to the rise of the modern alcoholism movement. Alcoholism Treatment Quarterly. 2000;18:1–23. [Google Scholar]
- 24.Wilson W. Yale University, Laboratory of Applied Physiology, School of Alcohol Studies. Alcohol, Science and Society: Twenty-nine Lectures with Discussions as Given at the Yale Summer School of Alcohol Studies. New Haven, NY: Quarterly Journal of Studies on Alcohol; 1945. The fellowship of Alcoholics Anonymous; pp. 461–473. [Google Scholar]
- 25.Dawkins R. The Selfish Gene. New York City: Oxford University Press; 1976. [Google Scholar]
- 26.Alcoholics Anonymous. Alcoholics Anonymous: The Story of How More Than One Hundred Men Have Recovered from Alcoholism. New York: Works Publishing Company; 1939. [Google Scholar]
- 27.White W. Pathways from the Culture of Addiction to the Culture of Recovery: A Travel Guide for Addiction Professionals. 2. Center City, MN: Hazelden; 1996. [Google Scholar]
- 28.White W. Pre-AA alcoholic mutual aid societies. Alcoholism Treatment Quarterly. 2001;19:1–21. [Google Scholar]
- 29.Tiebout HM. Alcoholics Anonymous: an experiment of nature. Quarterly Journal of Studies on Alcohol. 1961;22:52–68. [PubMed] [Google Scholar]
- 30.Reinart DF. Effects of participation in alcohol self-help groups on surrender and narcissism among adult male [doctoral dissertation] Dissertation Abstracts International. 1992;53:3827B. [Google Scholar]
- 31.Alcoholics Anonymous. Twelve steps and twelve traditions. New York: Alcoholics Anonymous World Services, Inc; 2002. [Google Scholar]
- 32.Miller W, Kurtz E. Models of alcoholism used in treatment: contrasting AA and other perspectives with which it is often confused. Journal of Studies on Alcohol. 1994;55:159–166. doi: 10.15288/jsa.1994.55.159. [DOI] [PubMed] [Google Scholar]
- 33.Kaskutas LA, Bond J, Avalos LA. 7-year trajectories of Alcoholics Anonymous attendance and associations with treatment. Addictive Behaviors. 2009;34:1029–1035. doi: 10.1016/j.addbeh.2009.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Delucchi KL, Kaskutas LA. Following problem drinkers over eleven years: understanding changes in alcohol consumption. Journal of Studies on Alcohol and Drugs. 2010;71:831–836. doi: 10.15288/jsad.2010.71.831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gossop M, Stewart D, Marsden J. Attendance at Narcotics Anonymous and Alcoholics Anonymous meetings, frequency of attendance and substance use outcomes after residential treatment for drug dependence: a 5-year follow-up study. Addiction. 2007;103:199–225. doi: 10.1111/j.1360-0443.2007.02050.x. [DOI] [PubMed] [Google Scholar]
- 36.Moos RH, Moos BS. Help-seeking careers: connections between participation in professional treatment and Alcoholics Anonymous. Journal of Substance Abuse Treatment. 2004;26:167–173. doi: 10.1016/S0740-5472(03)00190-9. [DOI] [PubMed] [Google Scholar]
- 37.Moos RH, Moos BS. Long-term influence of duration and frequency of participation in Alcoholics Anonymous on individuals with alcohol use disorders. Journal of Consulting and Clinical Psychology. 2004;72:81–90. doi: 10.1037/0022-006X.72.1.81. [DOI] [PubMed] [Google Scholar]
- 38.Moos RH, Moos BS. Paths of entry into Alcoholics Anonymous: consequences for participation and remission. Alcoholism: Clinical and Experimental Research. 2005;29:1858–1868. doi: 10.1097/01.alc.0000183006.76551.5a. [DOI] [PubMed] [Google Scholar]
- 39.Moos RH, Moos BS. The interplay between help-seeking and alcohol-related outcomes: divergent processes for professional treatment and self-help groups. Drug and Alcohol Dependence. 2004;75:155–164. doi: 10.1016/j.drugalcdep.2004.01.016. [DOI] [PubMed] [Google Scholar]
- 40.Moos RH, Moos BS. Sixteen-year changes and stable remission among treated and untreated individuals with alcohol use disorders. Drug and Alcohol Dependence. 2005;80:337–347. doi: 10.1016/j.drugalcdep.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 41.Moos RH, Moos BS. Protective resources and long-term recovery from alcohol use disorders. Drug and Alcohol Dependence. 2007;86:46–54. doi: 10.1016/j.drugalcdep.2006.04.015. [DOI] [PubMed] [Google Scholar]
- 42.Moos RH, Moos BS. Gender, treatment and self-help in remission from alcohol use disorders. Clinical Medicine & Research. 2006;3:163–174. doi: 10.3121/cmr.4.3.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kelly J, Brown S, Abrantes A, Kahler C, Myers MG. Social recovery model: an 8-year investigation of adolescent 12-step group involvement following inpatient treatment. Alcoholism: Clinical and Experimental Research. 2008;32:1468–1478. doi: 10.1111/j.1530-0277.2008.00712.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ritsher JB, McKeller JD, Finney JW, Otilingam PG, Moos RH. Psychiatric comorbidity, continuing care and mutual help as predictors of five-year remission from substance use disorders. Journal of Studies on Alcohol and Drugs. 2002;63:709–715. doi: 10.15288/jsa.2002.63.709. [DOI] [PubMed] [Google Scholar]
- 45.Timko C, DeBennedetti A, Moos BS, Moos RH. Predictors of 16-year mortality among individuals initiating help-seeking for an alcoholic use disorder. Alcoholism: Clinical and Experimental Research. 2006;30:1171–1720. doi: 10.1111/j.1530-0277.2006.00206.x. [DOI] [PubMed] [Google Scholar]
- 46.Timko C, Moos RH, Finney JW, Lesar MD. Long-term outcomes of alcohol use disorders: Comparing untreated individuals with those in Alcoholics Anonymous and formal treatment. Journal of Studies on Alcohol and Drugs. 2000;61:529–540. doi: 10.15288/jsa.2000.61.529. [DOI] [PubMed] [Google Scholar]
- 47.Vaillant GE. What can long-term follow-up teach us about relapse and prevention of relapse in addiction? British Journal of Addiction. 1988;83:1147–1157. doi: 10.1111/j.1360-0443.1988.tb03021.x. [DOI] [PubMed] [Google Scholar]
- 48.Vaillant GE. A 60-year follow-up of alcoholic men. Addiction. 2003;98:1043–1051. doi: 10.1046/j.1360-0443.2003.00422.x. [DOI] [PubMed] [Google Scholar]
- 49.Vaillant GE, Clark W, Cyrus C, et al. Prospective study of alcoholism treatment: eight-year follow-up. American Journal of Medicine. 1983;75:455–463. doi: 10.1016/0002-9343(83)90349-2. [DOI] [PubMed] [Google Scholar]
- 50.Turnbull L. Narcissism and the potential for self-transformation in the Twelve Steps. Health. 1997;1:149–165. [Google Scholar]
- 51.Reinert DF, Allen JP, Fenzel LM, Estadt BK. Alcohol recovery in self-help groups: surrender and narcissism. Journal of Religion and Health. 1993;32:299–308. doi: 10.1007/BF00990956. [DOI] [PubMed] [Google Scholar]
- 52.Reinert DF, Estadt BK, Fenzel LM, Allen JP, Gilroy FD. Relationship of surrender and narcissim to involvement in alcohol recovery. Alcoholism Treatment Quarterly. 1995;12:49–58. [Google Scholar]
- 53.Longabaugh R, Wirtz P. Project MATCH hypotheses: results on causal change analyses. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2001. [Google Scholar]
- 54.Project MATCH Research Group. Matching alcoholism treatments to client heterogeneity: Project MATCH posttreatment drinking outcomes. Journal of Studies on Alcohol and Drugs. 1997;58:7–29. [PubMed] [Google Scholar]
- 55.Project MATCH Research Group. Matching alcoholism treatments to client heterogeneity: Project MATCH three year drinking outcomes. Alcoholism: Clinical and Experimental Research. 1998;22:1300–1311. doi: 10.1111/j.1530-0277.1998.tb03912.x. [DOI] [PubMed] [Google Scholar]
- 56.Del Boca FK, Mattson ME, Fuller R, Babor TF. Planning a multisite matching trial: organization structure and research design. In: Babor TF, Boca FKD, editors. Treating matching in alcoholism. New York: Cambridge University Press; 2003. pp. 15–28. [Google Scholar]
- 57.Project MATCH Research Group. Project MATCH: Rationale and methods for a multisite clinical trial matching patients to alcoholism treatment. Alcoholism: Clinical and Experimental Research. 1993;17:1130–1145. doi: 10.1111/j.1530-0277.1993.tb05219.x. [DOI] [PubMed] [Google Scholar]
- 58.Miller WR, Zweben A, DiClemente CC, Rychtarik RG. Motivational enhancement therapy manual: a clinical research guide for therapists treating individuals with alcohol abuse and dependence. Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 1992. [Google Scholar]
- 59.Miller WR. Form 90: a structured assessment interview of drinking and related behaviors. Washington, DC: Government Printing Office; 1996. [Google Scholar]
- 60.Tonigan JS, Miller WR, Brown JM. The reliability of Form 90: an instrument for assessing alcohol treatment outcome. Journal of Studies on Alcohol and Drugs. 1997;58:358–364. doi: 10.15288/jsa.1997.58.358. [DOI] [PubMed] [Google Scholar]
- 61.Westerberg VS, Tonigan JS, Miller WR. Reliability of Form 90D: an instrument for quantifying drug use. Substance Abuse: Research and Treatment. 1998;19:179–189. doi: 10.1080/08897079809511386. [DOI] [PubMed] [Google Scholar]
- 62.Tonigan JS, Connors GJ, Miller WR. The Alcoholics Anonymous Involvement (AAI) scale: reliability and norms. Psychology of Addictive Behaviors. 1996;10:75–80. [Google Scholar]
- 63.Cohen J. Statistical power analysis for the behavioral sciences. Mawah, NJ: Lawrence Erlbaum; 1988. [Google Scholar]
- 64.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 65.Alcoholics Anonymous. Alcoholics Anonymous: The Story of how Many Thousands of Men and Women have Recovered from Alcoholism. 4. New York: Alcoholics Anonymous World Services, Inc; 2001. [Google Scholar]
- 66.Pagano ME, Phillips KA, Stout RL, Menard W, Piliavin JA. The impact of helping behaviors on the course of substance use disorders in individuals with body dysmorphic disorder. Journal of Studies on Alcohol and Drugs. 2007;68:291–295. doi: 10.15288/jsad.2007.68.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Pagano ME, Murphy JM, Pedersen M, et al. Screening for psychosocial problems in 4–5 year olds during routine EPSDT examinations; validity and reliability in a Mexican-American sample. Clinical Pediatrics. 1996;35:139–146. doi: 10.1177/000992289603500305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Aiken LS, West SG. Multiple Regression: Testing and interpreting interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- 69.Allison P. Logistic regression using SAS: theory and application. Cary, NC: SAS Institute; 1999. [Google Scholar]
- 70.Pedhazur EJ. Multiple regression in behavioral research: Explanation and prediction. Fort Worth, TX: Harcourt Brace College Publishers; 1997. p. 207. [Google Scholar]
- 71.Gilks WR, Richardson S, Speigelhalter DJ. Markov Chain Monte Carlo in practice: interdisciplinary statistics. London: Chapman and Hall; 1996. [Google Scholar]
- 72.Little RJA, Rubin DB. Statistical analysis with missing data. Hoboken, NJ: Wiley & Sons; 2002. [Google Scholar]
- 73.Kelly J, Stout R, Tonigan JS, Magill M, Pagano ME. Negative affect, relapse, and Alcoholics Anonymous: does AA work by reducing anger? Journal of Studies on Alcohol and Drugs. 2010;71:434–444. doi: 10.15288/jsad.2010.71.434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Barnard J, Rubin DB. Small-sample degrees of freedom with multiple imputation. Biometrika. 1999;86:948–955. [Google Scholar]
- 75.Babor TF, Del Boca FK. Treatment matching in alcoholism. Cambridge, UK: Cambridge University Press; 2003. [Google Scholar]
- 76.Timko C, Moos RH, Finney JW, Connell EG. Gender differences in help-utilization and the 8-year course of alcohol abuse. Addiction. 2002;97:887–889. doi: 10.1046/j.1360-0443.2002.00099.x. [DOI] [PubMed] [Google Scholar]
- 77.Blonigen DM, Timko C, Moos BS, Moos RH. Treatment, Alcoholics Anonymous, and 16-year changes in impulsivity and legal problems among men and women with alcohol use disorders. Journal of Studies on Alcohol and Drugs. 2009;70:714. doi: 10.15288/jsad.2009.70.714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Caldwell PE. Fostering client connections with Alcoholics Anonymous: A framework for social workers in various practice settings. Social Work Health Care. 1999;28:45–61. doi: 10.1300/J010v28n04_04. [DOI] [PubMed] [Google Scholar]
- 79.Alcoholics Anonymous. Bridging the gap between treatment and AA through temporary contact programs. New York: Alcoholics Anonymous World Services, Inc; 1991. [Google Scholar]
- 80.Zweben A, Rose SJ, Stout RL, Zywiak WH. Case monitoring and motivational style brief interventions. In: Hester RK, Miller WR, editors. Handbook of Alcoholism Treatment Approaches: Effective Alternatives. 3. Boston, MA: Allyn & Bacon; 2003. pp. 113–130. [Google Scholar]