Results of this study suggest that the incidence of vaginal cuff dehiscence after robotic-assisted total laparoscopic hysterectomy compares favorably to total abdominal and vaginal hysterectomies.
Keywords: Vaginal cuff dehiscence, Robotic-assisted total laparoscopic hysterectomy, Evisceration
Abstract
Study Objective:
The aim of this study was to estimate the cumulative incidence of vaginal cuff dehiscence in robotic-assisted total hysterectomies in our patients and to provide recommendations to decrease the incidence of vaginal cuff dehiscence.
Methods:
This was an observational case series, Canadian Task Force Classification II-3 conducted at an academic and community teaching hospital. A total of 654 patients underwent robotic-assisted total laparoscopic hysterectomy for both malignant and benign reasons from September 1, 2006 to March 1, 2011 performed by a single surgeon. The da Vinci Surgical System was used for robotic-assisted total laparoscopic hysterectomy.
Results:
There were 3 cases of vaginal cuff dehiscence among 654 robotic-assisted total laparoscopic hysterectomies, making our cumulative incidence of vaginal cuff dehiscence 0.4%. The mean time between the procedures and vaginal cuff dehiscence was 44.3 d (6.3 wk). All patients were followed up twice after surgery, at 3 to 4 wk and 12 to 16 wk.
Conclusion:
In our study, the incidence of vaginal cuff dehiscence after robotic-assisted total laparoscopic hysterectomy compares favorably to that of total abdominal and vaginal hysterectomy. Our study suggests that the incidence of vaginal cuff dehiscence is more likely related to the technique of colpotomy and vaginal cuff suturing than to robotic-assisted total hysterectomy per se. With proper technique and patient education, our vaginal dehiscence rate has been 0.4%, which is 2.5 to 10 times less than the previously reported vaginal cuff dehiscence rate in the literature.
INTRODUCTION
The da Vinci Surgical System (Intuitive Surgical, Sunnydale, CA) was FDA-approved for gynecologic surgery in April 2005 and has been used increasingly for benign and malignant gynecologic conditions, including total hysterectomy. Robotic technology has been found to improve the visualization, ergonomics, autonomy of camera control, and performance of complex laparoscopic maneuvers, such as suturing and knot tying.
Vaginal cuff dehiscence is a rare, but potentially devastating complication of total hysterectomy. The incidence of cuff dehiscence after a hysterectomy varies according to the surgical approach. Recent reviews report that the incidence of vaginal cuff dehiscence increases disproportionately in robotic hysterectomies compared to that in abdominal and vaginal hysterectomies.1–5
Vaginal cuff dehiscence requires prompt surgical management. In general, the incidence of vaginal cuff dehiscence is increased due to risk factors like poor wound healing, increased intraabdominal pressure, smoking, hematoma, vaginal trauma such as intercourse, and pelvic floor defects.3,6–16 However in most cases, investigators cannot define any risk factors.6,7 Our study is designed to review our experience of encountering vaginal cuff dehiscence in patients who have undergone laparoscopic total hysterectomy performed with the da Vinci Robotic System (Intuitive Surgical). Given the limited data, the aim of our study was to describe the rate of vaginal cuff dehiscence in a large series of consecutive robotic-assisted total hysterectomies for both benign and malignant reasons, and describe the characteristics of the patients with this complication. We also aim to provide recommendations to decrease the incidence of vaginal cuff dehiscence in robotic-assisted total hysterectomies.
METHODS
The Institutional Review Board at our institutions approved this study. We conducted a retrospective analysis of 654 consecutive patients, who underwent robotic-assisted total laparoscopic hysterectomy for both benign and malignant indications from September 1, 2006 to March 1, 2011 in a single surgeon's teaching practice in 2 hospitals. The division is a referral base for gynecologic oncology cases, complicated surgeries, and morbidly obese patients. All women who underwent robotic-assisted total laparoscopic hysterectomy, including radical hysterectomies were included in the study. We excluded all other robotic procedures including supracervical hysterectomies. The data were extracted from a database that had been prospectively maintained and included patient demographics, body mass index (BMI), hospital stay duration, surgical indication and procedure, duration of procedure, estimated blood loss, laparotomy conversion rate, intraoperative and postoperative complications, readmissions, and reoperations. The database was created using data from the electronic medical record, including records from the operating room, anesthesia, and pathology. The outpatient clinical records were used to obtain information for follow-up visits. All this information was entered into the database by the minimally invasive fellow and updated on a regular basis.
We defined vaginal cuff dehiscence as any palpable or visible separation of the vaginal incision with or without abdominal or pelvic organ eviscerating through the opening. All procedures were teaching cases and were performed either by the single teaching surgeon, fellow, or rotating gynecology residents with the teaching surgeon's direct supervision. Postoperatively, patients were seen at least twice, at 3 to 4 wk and 12 to 16 wk, and every effort was made to assure that any vaginal cuff dehiscence was reported to the surgeon who performed the procedure. Prophylactic antibiotics were given before all the procedures. All robotic operations were completed using the 4-arm da Vinci Surgical System (Intuitive Surgical, Mountain View, CA) model S or Si with a 5-port technique. The variations in surgical technique were minimal. In most patients, a sponge stick with the Colpo-pneumo Occluder balloon was inserted in the vagina. In a minority of patients, a Koh Colpotomizer System (Cooper Surgical, Trumbull, CT) in conjunction with a RUMI Uterine Manipulator (Cooper Surgical, Trumbull, CT) and a Colpo-pneumo Occluder balloon were inserted before port placement. In most the cases, the ports were placed in a sunrise distribution centered around the camera port (Figure 1). After insertion of the laparoscopic ports, the patients were tilted in a steep Trendelenburg position, the small bowel was brought out of the pelvis, and the distal ileum was flipped on its mesentery to help keep bowel above the pelvic brim. Subsequently, Trendelenburg was reduced to minimal, enough to keep small bowel out of the pelvis, and the da Vinci System was docked. The robot was positioned between the patients' legs, and once the robot was docked, the surgeon sat at the console and performed the operation. EndoWrist instruments were attached to each arm. The usual robotic instruments used were Hot Shears (monopolar curved scissor) with tip cover accessory at power setting of 45W in arm 1, fenestrated bipolar forceps with power setting of 45W in arm 2, and Pro Grasp forceps for arm 3. Vascular pedicles were coagulated and transected by the scrubbed assistant with a 5-mm or 10-mm LigaSure Atlas sealer/divider (Valleylab, Boulder, CO). The assistant also performed suction and irrigation (Suction Irrigator, Vital Concepts, Grand Rapids, MI) and retraction to expose the operative field. Hysterectomy was started with coagulation and transection of the round ligament. In all the cases, the retroperitoneum was exposed and ureters were identified. After isolation, ligation, and transection of the utero-ovarian ligament or infundibulopelvic ligament, uterine vessels, cardinal and uterosacral ligaments, a circumferential colpotomy was made using monopolar scissors in the cutting mode at 45 W. The specimen was then removed through the vagina. In patients with a large myomatous uterus, most specimens were vaginally morcellated, and in a minority of cases a laparoscopic morcellator was used. The bladder was then dissected further away from the edge of the vaginal cuff until at least 10 mm of healthy and pink vaginal edge was available for suturing. The vaginal cuff closure was always performed vertically in a running, single-layer nonlocking fashion using number 0 braided absorbable suture (Polysorb, Covidien) on a taper GS-21 needle (Figure 2). The vaginal cuff closure was begun at the middle of anterior wall of the vagina at 12 o'clock and continued vertically with at least one stitch in front of the uterine vessels and one stitch behind the uterine vessels. The uterosacral ligaments were incorporated in the closure (Figure 3). Knots were tied intracorporeally.
Figure 1.

Port placement, sunrise distribution.
Figure 2.
Vaginal cuff closure starts at 12 o'clock by passing the needle through the loop and continuing vertically.
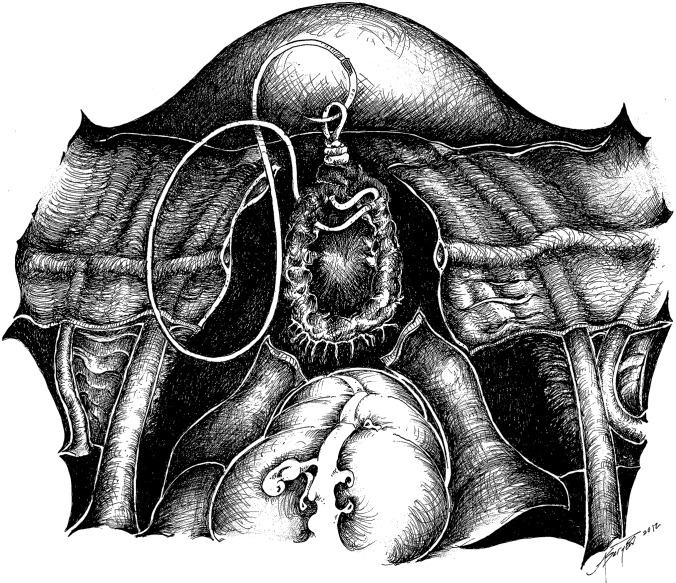
Figure 3.
Vertical vaginal cuff closure with bilateral uterosacral ligament vaginal vault suspension.
To bypass the tissue effect of thermal damage, special care was taken to incorporate at least 10 mm of tissue from the vaginal edges and to incorporate the vaginal mucosa along with paravaginal tissue. We put a loop at the end of our suture to save time and passed the needle through the loop rather than tying it at the start of suturing. A follow-up visit was scheduled in 3 to 4 wk and 12 to 16 wk after the surgery. In both of these routine follow-up visits and at most other indicated visits, pelvic examination, including a speculum examination, was performed. All patients were advised to postpone intercourse with deep penetration for at least 6 wk postoperatively. All patients were strongly advised to return to our clinic for any postoperative complications. All referring physicians were advised to notify us of any complications including vaginal cuff dehiscence.
RESULTS
During the study period, from September 1, 2006 to March 1, 2011, 654 patients underwent robotic-assisted total laparoscopic hysterectomy (RTLH) for both benign and malignant indications. The division is a referral center for gynecologic oncology cases, complicated surgeries, and morbidly obese patients. Many patients had additional procedures, such as lysis of adhesions, pelvic floor repair, lymph node dissection, omentectomy, treatment of endometriosis, ureterolysis, and cystoscopy. Data from 654 consecutive robotic-assisted total laparoscopic hysterectomies were collected including general gynecologic indications for hysterectomy, such as abnormal bleeding, pelvic mass, pelvic pain, genetic predisposition (including BRCA mutation and Lynch syndrome), pelvic organ prolapse and cervical dysplasia. Oncologic indications included endometrial hyperplasia, endometrial cancer, cervical cancer, and ovarian cancer. We did not exclude any patient from the study because of advanced cancer. Fifty-one percent of patients underwent hysterectomy for benign conditions and 49% for malignant indications. All patients had 2 routine postoperative vaginal examinations at 3 to 4 wk and 12 to 16 wk after surgery.
Three cases of vaginal cuff dehiscence occurred, making the cumulative incidence of vaginal cuff dehiscence 0.4% in 654 consecutive patients. The interval between the initial hysterectomy and the onset of dehiscence was 44.3 d (range, 13 to 86). Mean age was 53.6 (range, 51 to 58). The presenting symptoms were leakage of fluid, protruding mass from the vagina, and abdominal pain. Two patients underwent RTLH for symptomatic leiomyoma, and one underwent RTLH, BSO, and lymph node dissection for borderline ovarian tumor. Mean BMI was 30.5 (range, 22.4 to 37.2). Intercourse was the triggering event for the first patient, which occurred 86 d after RTLH. The second occurrence was 34 d after RTLH with the triggering event of straining during defecation. There was no triggering event for the third one. The omentum was the eviscerated organ in the first patient. She had moderate abdominal tenderness without any rebound or guarding. The eviscerated omentum was found to be adherent to the edge of vaginal cuff. A combined approach was used; the patient underwent exploratory laparoscopy and was found to have small bowel and omental adhesions to the edge of vaginal cuff. These adhesions were released with sharp and blunt dissection, and a small amount of necrotic tissue on the vaginal edge was debrided. The vaginal cuff was then closed transvaginally by using interrupted figure-of-eight stitches with number 0 Vicryl suture. The prolapsed organ was the small bowel in the second patient. The bowel was irrigated with sterile warm saline solution and inspected for viability. Once this was established, it was replaced into the peritoneal cavity, and the defect was repaired transvaginally. The third patient presented with a complaint of watery vaginal discharge 13 d after surgery and was found to have a 3-cm vaginal cuff defect as well as a left lower ureterovaginal fistula. There was no prolapsed organ and possibly the small opening in the vaginal cuff was due to the ureterovaginal fistula. The patient underwent examination under anesthesia with a cystoscopy, left retrograde pyelogram, and left ureteral stent placement. The vaginal cuff was repaired at the same time transvaginally by using interrupted figure-of-eight stitches with number 0 Vicryl suture. A Foley catheter was placed. Two months later, the stent was removed and the patient recovered from both the ureterovaginal fistula and the vaginal cuff dehiscence. The patient resumed normal activity including intercourse 3 mo after vaginal cuff repair. Two patients required debridement of the vaginal edge before repair. The vaginal cuff was closed transvaginally using interrupted figure-of-eight stitches with number 0 Vicryl suture in all 3 patients. The patients' recovery was uneventful, and all 3 recovered very well after the first repair with no recurrence of cuff dehiscence.
DISCUSSION
Recent reports have suggested that vaginal cuff dehiscence might be more common in robotic-assisted total laparoscopic hysterectomy.1–5 Depending on the authors, the incidence of vaginal cuff dehiscence after robotic-assisted total hysterectomies varied between 0.98% and 4.1%. Kho et al.3 reported a 4.1% incidence of vaginal cuff dehiscence among robotic procedures involving colpotomy, including hysterectomy, trachelectomy, and vaginectomy. A retrospective review of 2,399 hysterectomies performed at the Mayo Clinic in Scottsdale, Arizona, of which 15% were performed robotically and 9% with traditional laparoscopy, reported the vaginal cuff dehiscence rate to be 2.87% for robotic hysterectomy and 0.47%, 0.13%, and 0.99% for TLH, TVH, and TAH respectively.1 Dauterive et al.2 reported 7 of their 268 patients who underwent RALH for nonmalignant reasons had vaginal cuff dehiscence with a cumulative incidence of 2.61%. They reported that all except 1 of 7 cuff dehiscences occurred within the surgeon's first 25 cases. Visco et al.5 reported on robotic hysterectomy with a deshicence incidence of 1.27% among their patients. Robinson et al.4 reported 2 cases of vaginal cuff dehiscence among 205 robotic TLHs performed between December 2007 and January 2009, with an incidence of 0.98%. Nezhat et al.17 published in 1996 the first case series of 3 women with vaginal evisceration after total laparoscopic hysterectomy, 2 to 5 mo postoperatively and questioned whether vaginal evisceration is especially common after total laparoscopic hysterectomy. Hur et al.6 showed that the cumulative incidence of vaginal cuff dehiscence was 4.93% among total laparoscopic hysterectomies (TLH), 0.29% among total vaginal hysterectomies (TVH), and 0.12% among total abdominal hysterectomies (TAH) during a 15-mo period. They reported that the relative risk of a vaginal cuff dehiscence complication after TLH compared with TVH and TAH was 21.0 and 53.2, respectively.
Our data revealed a cumulative incidence of vaginal cuff dehiscence after RALH of 0.4%. This compares favorably to reported vaginal cuff dehiscence in total abdominal and vaginal hysterectomy. This is much lower than reported dehiscence rate after RALH in other studies. Moreover, in 49% of our patients, malignancy was the indication for surgery. These patients may be at increased risk for vaginal cuff dehiscence, because of advanced age and multimodal treatment, including chemotherapy and radiation, that may impair wound healing and increase the vaginal cuff dehiscence rate. Furthermore in many cases, lymph node dissection was performed which can potentially cause pelvic fluid accumulation and delay vaginal cuff healing. Traditionally, thermal damage due to the use of electrocautery at the time of colpotomy has been the main hypothesis behind the high incidence of vaginal cuff dehiscence after minimally invasive hysterectomies.6,17 In our patients, we used monopolar curved scissors in the cutting mode of 45 W. We try to have minimal tissue contact in order to create a clean cut with a minimal coagulation effect for the colpotomy. Cuff hemostasis is obtained with suturing instead of electrocoagulation. To bypass the tissue effect of thermal damage, special care was taken to incorporate at least 10 mm of pink tissue from full-thickness vaginal edges, and to incorporate the vaginal mucosa. The other explanation might be that the quality of knot tying in robotic surgery is not as good as that in hand tying. Muffly et al.18 report that the knot is stronger if it is directly maintained using the hand compared to the robotic arms. Their study showed that a mean force of 57.4 N was needed to untie 5 square knots performed by the robot, but for manual tying the force needed was 112.2 N (P < .001). We start our suture with a loop that has been placed at the end of the suture extracorporeally before introduction into the abdominal cavity. We used square knots with instrument tie at the end of suture and believe well-constructed square knots with flat throws are less likely to slip. The suture should be tightened sufficiently to approximate the vaginal edges without constricting the tissue. Knots were tied intracorporeally at the end of vaginal closure.
Magnified views by the camera in robotic surgery may mislead the surgeon to place sutures too close to the vaginal edge or not to include full thickness as reported by Uccella et al.19 We used a robotic large needle driver with a jaw length of 10 mm or a Mega needle driver with a jaw length of 13 mm as a reference and included at least 10 mm of full thickness of vaginal cuff including the mucosa.
Our method of vertical vaginal cuff closure increases posthysterectomy vaginal length and may contribute to decreased vaginal cuff rupture after intercourse. A randomized trial comparing methods of vaginal cuff closure at vaginal hysterectomy and the effect on vaginal length by Vassallo et al.20 revealed that closing the vaginal cuff vertically is superior to horizontal closure for the purpose of preserving vaginal length. In many studies cited earlier, the specific technique of vaginal cuff closure was not mentioned. However traditionally, vaginal cuff closure is done horizontally. In the Kho et al.3 study with an incidence rate of 4.1% of vaginal cuff dehiscence, the technique of vaginal cuff closure consisted of 2 transverse nonlocking running sutures of polyglactin 1-0 on a CT-1 needle with absorbable polydioxanone clips secured at each end. In our study, the vaginal cuff closure was always begun at the middle of the anterior wall of the vagina at 12 o'clock and continued vertically in a running, single-layer nonlocking fashion using number 0 braided absorbable suture (Polysorb, Covidien) on a taper GS-21 needle. Uterosacral ligaments were incorporated in the closure (Figure 3). In our experience, vertical closure facilitated the bilateral uterosacral ligament vaginal vault suspension, and vaginal length was increased with no evidence of upper vaginal narrowing. However, a vertical vaginal cuff closure may potentially increase the risk of ureteral kinking if the bladder is not dissected off the vagina adequately.
Other potential risk factors for vaginal cuff dehiscence include vaginal trauma such as intercourse soon after surgery in premenopausal patients.7–11,17 Hur et al.6 reported that the most common trigger of cuff dehiscence was coitus. To reduce the incidence of vaginal cuff dehiscence, we recommend that our patients avoid vaginal intercourse with deep penetration for at least for 6 wk postoperatively.
Somkuti et al.11 described several other factors that may contribute to vaginal cuff dehiscence including postoperative cuff infection and cuff hematoma. Although we minimize the use of electrocautery for cuff hemostasis, we make sure we obtain excellent hemostasis with suturing to prevent cuff hematoma.
Larsson et al.21 reported that pre- and postoperative treatment for at least 4 d with metronidazole rectally significantly reduced vaginal cuff infection among women with abnormal vaginal flora who underwent total abdominal hysterectomy. We also treat any vaginitis including bacterial vaginosis before surgery and postoperatively look for signs and symptoms of cuff cellulitis.
In several studies,12–13 pelvic organ prolapse is mentioned as a contributing factor for vaginal cuff dehiscence after hysterectomy in postmenopausal patients. We routinely reattach the uterosacral ligament to the vaginal cuff to prevent future vaginal cuff prolapse (Figure 3).
We designed the mnemonic “Dehiscence” to assist remembering the principals of vaginal cuff dehiscence prevention. Please see Addendum.
Management of vaginal cuff dehiscence begins with evaluation and stabilization of the patient's condition. A pelvic examination is essential for diagnosis. We irrigate the eviscerated organ with sterile warm saline solution. We recommend placement of the patient in Trendelenburg's position and place a sterile moist gauze over the eviscerated organ and separate it from the vagina. The route of repair should be individualized based on findings at the time of presentation of vaginal cuff dehiscence. If examination reveals that the bowel is viable with active peristalsis and not in need of resection, the patient is a candidate for transvaginal repair. If any adhesion to the vaginal cuff is suspected, the prolapsed organ cannot be reduced, exposure is poor, or there is an acute abdomen, we suggest a combined laparoscopic-vaginal approach. We consider imaging including CT scan of the pelvis and abdomen for any signs of hematoma, abscess, or bowel obstruction or any suspicion of other injuries such as ureteral injury. We start intravenous hydration and broad-spectrum antibiotics. The primary goal of surgery is to remove any necrotic tissue and close the vaginal cuff without any tension using an interrupted closure. We usually repair the vaginal cuff using interrupted figure-of-eight stitches with number 0 delayed absorbable sutures. Any underlying comorbid condition that increases intraabdominal pressure should be treated actively. We advise delaying intercourse at least 6 wk postoperatively.
CONCLUSION
Vaginal cuff dehiscence is a rare but serious complication and requires prompt recognition and surgical correction. The reported incidence of vaginal cuff dehiscence after robotic-assisted total laparoscopic hysterectomies varies between 0.98% and 4.1%. Among our patients who underwent robotic-assisted total laparoscopic hysterectomy (n = 654), the cumulative incidence of cuff dehiscence was 0.4%. This is 2.5 to 10 times less than the reported dehiscence rate after the same procedure in others studies. To our knowledge our study represents the largest published experience that estimates the incidence of vaginal cuff dehiscence in robotic-assisted total laparoscopic hysterectomy in 654 consecutive patients and includes both benign and malignant cases. This rate in our patients is comparable to or lower than the reported vaginal cuff dehiscence after total abdominal or vaginal hysterectomy. The reported incidence of vaginal cuff dehiscence after total abdominal and vaginal hysterectomy is 0.12% to 0.99%.1,6
The incidence of vaginal cuff dehiscence after robotic-assisted total laparoscopic hysterectomy is probably related to preoperative and postoperative preparation, the surgical technique, and vaginal cuff suturing rather than with robotic-assisted total hysterectomy per se.
The results of our study suggest that colpotomy and vaginal closure technique may contribute to decreasing the vaginal cuff dehiscence rate after robotic-assisted total laparoscopic hysterectomy. Our data may also suggest the important role of prolonged pelvic rest especially in high risk groups.
We acknowledge that a limitation our study is the fact that all cases were performed or supervised by a single experienced gynecologic oncologist who has vast experience in laparotomy, laparoscopy, and robotic surgery; therefore, this may not be representative of general practice. Further randomized studies may be necessary to fully assess contributing factors in vaginal cuff dehiscence in robotic-assisted total laparoscopic hysterectomy. Until then, we suggest emphasis on prevention of vaginal cuff dehiscence based on information that is available thus far.
Addendum
We designed the mnemonic “Dehiscence” to assist remembering the principals of vaginal cuff dehiscence prevention;
D for defect. Any pelvic floor defect should be recognized and appropriately repaired at the time of robotic hysterectomy. We routinely close the vaginal cuff vertically and do bilateral uterosacral ligament vaginal vault suspension in all of our robotic hysterectomies.
E for Education. Patients should be given careful instructions to avoid intercourse, heavy lifting with increased intrapelvic pressure, or putting any object inside the vagina for at least 6 wk after surgery. Patients may resume sexual activity earlier if speculum examination shows complete healing of the vaginal cuff.
H for hormone replacement. If atrophy coexists, one may consider estrogen vaginal cream.
I for infection. Prophylactic antibiotic was given before all procedures. We treat any symptomatic bacterial vaginosis prior to hysterectomy to prevent cuff infection after RALH.
S for symptoms. Recognize the symptoms of vaginal cuff dehiscence. Early diagnosis decreases the serious sequelae, including peritonitis, bowel injury, and necrosis. Patients most commonly present with vaginal bleeding and a sudden gush of watery vaginal discharge.
C for cuff closure. Vertical vaginal cuff closure increases posthysterectomy vaginal length, which may contribute to decrease of vaginal cuff rupture with intercourse. This is especially useful in radical hysterectomy in which the vagina will be short secondary to removal of 3cm to 5cm of upper vagina.
E for evisceration. Evisceration was reported in 60% of cases. Small bowel is the most common organ that prolapsed through the vagina. Prompt recognition and surgical correction of evisceration may prevent bowel incarceration, perforation, peritonitis, and sepsis.
N for no tension. The suture should be tightened sufficiently to approximate the vaginal edges without constricting the tissue.
C for cutting current rather than coagulation current with minimum tissue contact and low voltage. Minimizing the use of thermal energy may result in less tissue damage to the vaginal cuff.
E for edge. Magnified views by the camera in robotic surgery may mislead the surgeon to place sutures too close to the vaginal edge or not to include full thickness. We use the robotic needle driver as a reference and make sure to include at least 10 mm of full thickness of the vaginal cuff including the mucosa.
Contributor Information
Shabnam Kashani, Department of Obstetrics & Gynecology, Minimally Invasive Gynecologic Surgery Fellowship Program, Yale New Haven Health/Bridgeport Hospital, New Haven, CT, USA..
Taryn Gallo, Department of Obstetrics & Gynecology, Minimally Invasive Gynecologic Surgery Fellowship Program, Yale New Haven Health/Bridgeport Hospital, New Haven, CT, USA..
Anita Sargent, Department of Obstetrics, Gynecology & Reproductive Sciences, Division of Gynecology Oncology, Yale University School of Medicine, New Haven, CT, USA..
Karim ElSahwi, Department of Obstetrics, Gynecology & Reproductive Sciences, Division of Gynecology Oncology, Yale University School of Medicine, New Haven, CT, USA..
Dan-Arin Silasi, Department of Obstetrics, Gynecology & Reproductive Sciences, Division of Gynecology Oncology, Yale University School of Medicine, New Haven, CT, USA..
Masoud Azodi, Department of Obstetrics, Gynecology & Reproductive Sciences, Division of Gynecology Oncology, Yale University School of Medicine, New Haven, CT, USA..
References:
- 1. Akl MN. Robotic hysterectomy more likely to result in vaginal cuff dehiscence. Annual Meeting of the Society of Gynecologic Surgeons; 2008 [Google Scholar]
- 2. Dauterive E, Morris IV, G Incidence and characteristics of vaginal cuff dehiscence in robotic-assisted and traditional total laparoscopic hysterectomy. J Robot Surg. 2012;6:149–154 [DOI] [PubMed] [Google Scholar]
- 3. Kho RM, Akl MN, Cornella JL, Magtibay PM, Wechter ME, Magrina JF. Incidence and characteristics of patients with vaginal cuff dehiscence after robotic procedures. Obstet Gynecol. 2009;114:231–235 [DOI] [PubMed] [Google Scholar]
- 4. Robinson BL, Liao JB, Adams SF, Randall TC. Vaginal cuff dehiscence after robotic total laparoscopic hysterectomy. Obstet Gynecol. 2009;114:369–371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Visco AG, Advincula AP. Robotic gynecologic surgery. Obstet Gynecol. 2008;112:1369–1384 [DOI] [PubMed] [Google Scholar]
- 6. Hur HC, Guido RS, Mansuria SM, Hacker MR, Sanfilippo JS, Lee TT. Incidence and patient characteristics of vaginal cuff dehiscence after different modes of hysterectomies. J Minim Invasive Gynecol. 2007;14:311–317 [DOI] [PubMed] [Google Scholar]
- 7. Iaco PD, Ceccaroni M, Alboni C, et al. Transvaginal evisceration after hysterectomy: is vaginal cuff closure associated with a reduced risk? Eur J Obstet Gynecol Reprod Biol. 2006;125:134–138 [DOI] [PubMed] [Google Scholar]
- 8. Hall BD, Phelan JP, Pruyn SC, Gallup DG. Vaginal evisceration during coitus: a case review. Am J Obstet Gynecol. 1978;131:115–116 [DOI] [PubMed] [Google Scholar]
- 9. Haney AF. Vaginal evisceration after forcible coitus with intraabdominal ejaculation. J Reprod Med. 1978;21:254–26 [PubMed] [Google Scholar]
- 10. Cardosi RJ, Hoffman MS, Roberts WS, Spellacy WN. Vaginal evisceration after hysterectomy in premenopausal women. Obstet Gynecol. 1999;94:859. [DOI] [PubMed] [Google Scholar]
- 11. Somkuti SG, Vieta PA, Daugherty JF, Hartley LW, Blackmon EB., Jr Transvaginal evisceration after hysterectomy in premenopausal women: a presentation of three cases. Am J Obstet Gynecol. 1994;171:567–568 [DOI] [PubMed] [Google Scholar]
- 12. Croak AJ, Gebhart JB, Klingele CJ, Schroeder G, Lee RA, Podratz KC. Characteristics of patients with vaginal rupture and evisceration. Obstet Gynecol. 2004;103:572–576 [DOI] [PubMed] [Google Scholar]
- 13. Kowalski LD, Seski JC, Timmins PF, Kanbour AI, Kunschner AJ, Kanbour-Shakir A. Vaginal evisceration: presentation and management in postmenopausal women. J Am Coll Surg. 1996;183:225–229 [PubMed] [Google Scholar]
- 14. Yüce K, Dursun P, Gültekin M. Posthysterectomy intestinal prolapse after coitus and vaginal repair. Arch Gynecol Obstet 2005;272:80–81 [DOI] [PubMed] [Google Scholar]
- 15. Purakal J, Moyer G, Burke W. Vaginal cuff dehiscence after hysterectomy in a woman with systemic lupus erythematosus: a case report. J Reprod Med. 2008;53:305–37 [PubMed] [Google Scholar]
- 16. Ramirez PT, Klemer DP. Vaginal evisceration after hysterectomy: a literature review. Obstet Gynecol Surv. 2002;57:462–467 [DOI] [PubMed] [Google Scholar]
- 17. Nezhat CH, Nezhat F, Seidman DS, Nezhat C. Vaginal vault evisceration after total laparoscopic hysterectomy. Obstet Gynecol. 1996;87:868–870 [PubMed] [Google Scholar]
- 18. Muffly T, McCormick TC, Dean J, Bonham A, Hill RF. An evaluation of knot integrity when tied robotically and conventionally. Am J Obstet Gynecol. 2009;200:e18–20 [DOI] [PubMed] [Google Scholar]
- 19. Uccella S, Ghezzi F, Mariani A, et al. Vaginal cuff closure after minimally invasive hysterectomy: our experience and systematic review of the literature. Am J Obstet Gynecol. 2011;205:119.e1–12 [DOI] [PubMed] [Google Scholar]
- 20. Vassallo BJ, Culpepper C, Segal JL, Moen MD, Noone MB. A randomized trial comparing methods of vaginal cuff closure at vaginal hysterectomy and the effect on vaginal length. Am J Obstet Gynecol. 2006;195:1805–1808 [DOI] [PubMed] [Google Scholar]
- 21. Larsson PG, Carlsson B. Does pre- and postoperative metronidazole treatment lower vaginal cuff infection rate after abdominal hysterectomy among women with bacterial vaginosis? Infect Dis Obstet Gynecol. 2002;10:133–140 [DOI] [PMC free article] [PubMed] [Google Scholar]