Laparoscopic appendectomy reduced the rate of unnecessary appendectomies and postoperative length of stay.
Keywords: Laparoscopy, Appendectomy, Nigeria
Abstract
Objective:
Laparoscopic appendectomy in a setting where resources are poor is still controversial. This study evaluates the impact of laparoscopy on the early outcome of acute appendicitis in a developing country.
Methods:
All patients who underwent appendectomy from January 2010 through June 2011 at the Obafemi Awolowo University Teaching Hospitals Complex, Ile-Ife, Nigeria were recruited for this study.
Results:
Of the 139 patients with acute appendicitis within the study period, 83 (59.7%) had open appendectomy (OA), 19 (13.7%) whose clinical and radiological findings suggested complicated appendicitis at presentation had laparotomy, while 37 (26.6%) had laparoscopic procedures. In the laparoscopy group, initial diagnostic laparoscopy in 4 (10.8%) patients revealed a normal appendix along with other findings that precluded appendectomy. Laparoscopic appendectomy (LA) was then performed in 33 (23.7%) patients with 2 of these (6.1%) requiring conversion to open laparotomy. Mean time for the LA procedure was higher than that observed for OA (56.2 vs 38.9 min). Patients in the LA group had a shorter mean postoperative stay (1.8 vs 3.0). Wound infection occurred in 2 (6.5%) patients from the LA group and 8 (9.6%) from OA.
Conclusion:
Laparoscopic appendectomy reduced the rate of unnecessary appendectomy and postoperative hospital stay in our patients, potentially reducing crowding in our surgical wards. We advocate increased use of laparoscopy especially in young women.
INTRODUCTION
Acute appendicitis is one of the most common procedures worldwide, with appendectomy accounting for up to one-third of all emergency surgeries performed in both developing and developed countries.1 For several decades, open appendectomy (OA) has been the gold standard with acceptable outcome in most published series.2 The introduction of laparoscopic appendectomy (LA) was therefore greeted with initial reluctance, skepticism, or outright rejection by many surgeons. Surgeons were discouraged by the disadvantages of the laparoscopic approach, including longer duration of operation, increased cost to the patient, and reports of complications.3,4 Nearly 3 decades later, large series of randomized controlled trials have shown significant evidence in favor of LA in many centers across the world.5,6 Despite published studies showing several advantages, the validity of this procedure in developing countries has not been confirmed.7
In many developing countries like Nigeria, the challenges posed by the burden of communicable diseases and other primary healthcare concerns have limited government support for development of modern tertiary healthcare facilities. Indeed, laparoscopic surgery is practiced in only a few tertiary hospitals across the country. Our hospital is located in a semiurban part of Southwestern Nigeria with a large agricultural population. We have recently introduced laparoscopic surgery into our general surgical practice.8 The present study was conducted to evaluate the impact of laparoscopy on the diagnosis and treatment of patients with acute appendicitis in our setting.
PATIENTS AND METHODS
We studied patients with a clinical diagnosis of uncomplicated acute appendicitis at the Ife Hospital Unit of the Obafemi Awolowo University Teaching Hospitals Complex, Ile-Ife, Osun State, Nigeria over a 1-y period from January 2010 through June 2011. The socio-demographic data of the patients were obtained along with detailed records of clinical presentation. Investigations were conducted and comorbidities identified. A clinical diagnosis of acute appendicitis was made based on clinical presentation and findings on abdomino-pelvic ultrasonography. When the diagnosis was inconclusive, such patients were usually selected for diagnostic laparoscopy. Pneumoperitoneum was created in each patient by inserting a Veress needle at the umbilicus. An 11-mm trocar was then inserted at the same site for initial diagnostic laparoscopy. Before conducting an LA, a 5-mm port was introduced in the suprapubic region and another one in the right upper quadrant. The appendix was identified and freed from any adhesions by a combination of blunt and sharp dissection. The mesoappendix was then serially divided after coagulation with bipolar electrocautery, and the base of the appendix was secured using synthetic absorbable sutures by extracorporeal knotting. The specimen was extracted by drawing the appendix into the 11-mm port and extracting it under vision. There were few instances of markedly enlarged or purulent specimens and a retrieval bag was used. Conventional OA was performed traditionally.
All patients received pre- and postoperative doses of antibiotics. A nonsteroidal anti-inflammatory agent was used for postoperative analgesia in all patients. Postoperative administration was evaluated according to patient tolerance and signs such as nausea or vomiting.
Data regarding the operative findings and its duration, postoperative requirement for analgesia, postoperative length of stay and complications were recorded. Data were analyzed using Statistical Package for Social Sciences version 16. Comparison between the 2 groups was made using χ2 and Student t tests. Statistical significance was set at P < .05.
RESULTS
The study included 139 patients with acute appendicitis. Open surgery was performed directly in 102 (73.4%) patients including OA in 83 (59.7%) patients and laparotomy in 19 (13.7%) patients presenting with complicated appendicitis following clinical and radiological examination. Two of the patients undergoing OA (2.4%) were converted to laparotomy due to difficulties with delivering the appendix through a Lanz incision. Within the study time period, 37 (26.6%) patients had laparoscopic procedures. In the laparoscopy group, initial diagnostic laparoscopy in 4 patients revealed a normal appendix along with other significant findings. LA was then performed in 33 (23.7%) patients with 2 (6.1%) conversions to open laparotomy, due to findings of a complex inflammatory mass in one patient and an extensive retrocecal abscess in another patient. Two other patients with perforated appendixes and another 2 with phlegmon surrounding the appendix successfully underwent laparoscopy.
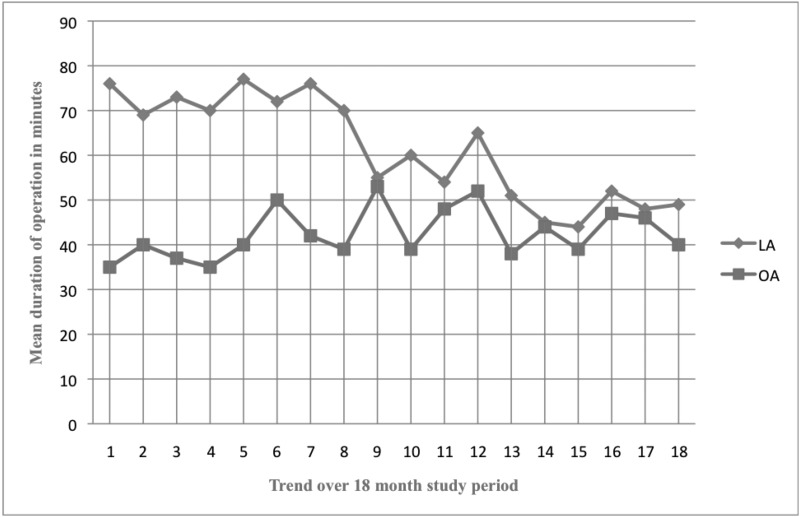
Patients in the laparoscopy group were aged 15 to 51 y with a mean of 29 y, while patients in the OA group were aged 14 to 68 y with a mean of 25.2 y, as shown in Table 1. A larger number of female patients were selected for the laparoscopic approach, compared with the OA group, both groups being equally matched for sex distribution. Preoperative abdominal ultrasound scan revealed features suggesting acute appendicitis in 51.7% and 73.4% of patients in the LA and OA groups, respectively. Intraoperative findings in the LA group included a grossly inflamed appendix in 62.2% of patients with a normal appendix in 4 patients (10.8%) with pathologies, such as ileacacal adhesions in 9 (24.3%), ovarian pathologies in 5 (13.5%), and perforated appendix in 2 (5.4%) patients. The mean time for LA surgery was higher than that for OA (56.2 vs 38.9 min), with a reduction in time for LA, as depicted in Figure 1. Postoperatively, a prolonged ileus extending beyond 48 h was recorded in 4 (10.8%) patients in the OA. Patients in the LA group were discharged between the first and third day after surgery (mean 1.8) as compared to 2 to 4 (mean 3.0) days for the OA group. Postoperative superficial wound infection occurred in the port sites of 2 (6.4%) LA patients, while similar superficial infection occurred in 4, deep SSI in 2 and residual abscess in 1 patient from the OA group. Histopathological report confirmed appendicitis in all patients (96.8%) but 1 in the LA and 84.3% patients in the OA group.
Table 1.
Comparing Laparoscopic and Open Appendectomy in a Nigerian Hospital
| Laparoscopic Appendectomy (n=31) | Open Appendectomy (n=83) | ||
|---|---|---|---|
| Demographic Features | |||
| Age Range (years) | 15–51 | 14–68 | |
| Mean age (years) | 27.0 | 25.2 | |
| Sex Distribution (M:F) | 7:24 | 44:39 | |
| Clinical Features & Investigation Findings | |||
| RLQ Pain | 31/31 | 83/83 | |
| Nausea | 20/31 | 56/83 | |
| Vomiting | 2/31 | 19/83 | |
| Fever | 4/31 | 13/83 | |
| Guarding | 6/31 | 39/83 | |
| Ultrasound findings | 16/31 | 47/64 | |
| Outcome | |||
| Duration of surgery, Range (mean) | 38–78 min (56.2 min) | 29–67 min (38.9 min) | X2=12.343 |
| df=1; p=0.032 | |||
| Prolonged ileus. | 0/31 | 4/83 | |
| Length of stay, Range (mean) | 1–3(1.8) | 2–4(3.0) | X2=15.333 |
| df=1; p=0.049 | |||
| Postoperative surgical site infection | 2/31 | 7/83 | X2=2.312 |
| df=2; p=0.632 | |||
| Histopathological confirmation | 31/31 | 70/83 |
Figure 1.
Mean duration of time for laparoscopic and open appendectomy.
DISCUSSION
Surgical procedures for acute appendicitis and its complications are one of the commonest emergency surgeries performed in our center. Previous studies across Nigeria have reported a high incidence of complications in need of immediate laparotomy.9–11 In this study, 13.9% patients presented with complications that required immediate laparotomy, while 6 from the LA group had complications requiring open laparotomy. This high incidence of complications is partly due to patients utilizing overthe-counter drugs at the onset of the symptoms while for others there may have been a delay in referral from their primary care physicians.
Most the procedures (102 of 139) were performed by the open approach. This is because most residents performing these procedures are not yet experienced in laparoscopic surgery, especially in the emergency department setting. Patients selected for the laparoscopic approach included young females in the reproductive age group with suspected pelvic conditions, patients presenting with signs not specific to appendicitis, and older patients with features of acute appendicitis. We found dense adhesions between pelvic organs and terminal ileum in 1 patient, a solid ovarian mass in a 23-y-old female patient and ruptured ovarian cysts with limited hemoperitoneum in another 2. The appendix in these 4 patients appeared normal; hence, they were not eligible for laparoscopic appendectomy. Earlier reports have highlighted several benefits of initial diagnostic laparoscopy in these group of patients.12–14 In Nigeria, negative appendectomy rate ranges between 15% and 30% and is more common among women.9,15,16 We believe that LA, if embraced across Nigeria and other similar developing settings, would reduce this incidence of negative appendectomy.
The mean duration of operation time was significantly longer in the laparoscopy group compared with the open group (P = .032). The initial period of our learning curve contributed significantly to the longer duration of the procedure in the early period of this study. This, however, declined considerably over time as reported in Figure 1. The mean operation time for LA in our study is similar to that reported in other countries.7,17,18
Postoperatively, 4.8% of patients who had OA developed prolonged ileus lasting beyond 48 h, while this was not observed in the LA group. This factor probably contributed to a statistically significant difference observed in the duration of hospital stay between the 2 groups.
Different studies have shown that wound infection rates are lower following LA compared with OA.19,20 A meta-analysis of randomized controlled trials found a slightly higher incidence of intraabdominal abscesses in LA patients.5 In this study, surgical site infection was recorded in 6.4% of LA patients compared with 10.8% of the OA group. This difference was not statistically significant though the grades of infection were higher in the OA group. The 2 port-site infections recorded in the LA group were superficial, but deep SSI were recorded in 4 patients along with 2 incidences of residual abscesses in the OA group. This may be because most patients with urgent need for surgery were immediately offered the open option. The percentage of postoperative wound infections following OA ranged between 8% and 26% as reported in hospitals throughout Nigeria.9,15
The present study has its limitations. To adequately compare the outcome of these 2 groups in our setting, a randomized study would have been ideal. As more surgeons and trainees in our center become more proficient in laparoscopic surgery, we will be able to design a randomized comparison of the 2 procedures, without the inherent selection bias of the current study. A number of studies have also compared the cost implications of OA and LA in different settings.21,22 Our study is unable to offer such a detailed comparison, because the LA procedure is currently subsidized in our hospital. The cost of laparoscopy in our center has reduced drastically with the adoption of reuseable instruments as well as alternatives to reduce the number of consumables required for surgery. For instance, a tray of disposable hand instruments for one laparoscopic cholecystectomy was purchased by our hospital for the equivalent of 1050 US Dollars. A set of reuseable hand instruments purchased for the equivalent of 3800 US Dollars have been used for approximately 200 different procedures with minimal additional costs for resterilization. Our supply of preformed endoloop sutures was irregular and also added to the direct cost of the procedure. This prompted us to adopt routine extracorporeal ligation of the appendix base. We also limited the use of retrieval bags in patients with inflamed or purulent specimens, while in other cases we have drawn the appendix into the 11-mm trocar for extraction. Another inexpensive option is a simple tripolar forceps with a blade that can be activated to divide between the bipolar ends of the electrocautery and aid the division of the mesoappendix. A number of authors from other developing settings have described different modifications and improvisations that could reduce cost and encourage the feasibility of LA in such situations.7,23
For this study, we have also focused on training the surgical team in laparoscopic procedures. While a number of surgeons in our hospital have been exposed to training in laparoscopic surgery outside Nigeria, many residents, nurses and other support staff had no prior exposure to the procedures. Internal training of our staff has had a positive impact on the success of our laparoscopy cases. We are currently introducing the use of laparoscopy in the operative management of patients with complicated appendicitis as well as those with generalized peritonitis. We believe that through constant evolution of laparoscopy and other forms of minimally invasive surgery patient outcome will continue to improve.
CONCLUSION
The present study shows successful outcomes in performing laparoscopic appendectomy. LA reduced postoperative hospital stay in our patients potentially reducing crowding in our surgical wards. We advocate the use of diagnostic laparoscopy in young women with suspected acute appendicitis, as well as in those with atypical presentations in our developing economy.
Contributor Information
Adewale O. Adisa, Department of Surgery, Obafemi Awolowo University and Obafemi Awolowo University Teaching Hospitals Complex, Ile Ife, Nigeria..
Olusegun I. Alatise, Department of Surgery, Obafemi Awolowo University and Obafemi Awolowo University Teaching Hospitals Complex, Ile Ife, Nigeria..
Olukayode A. Arowolo, Department of Surgery, Obafemi Awolowo University and Obafemi Awolowo University Teaching Hospitals Complex, Ile Ife, Nigeria..
Oladejo O. Lawal, Department of Surgery, Obafemi Awolowo University and Obafemi Awolowo University Teaching Hospitals Complex, Ile Ife, Nigeria..
References:
- 1. Addis DG, Shaffer N, Fowler BS, Tauxe RV. The epidemiology of acute appendicitis and appendectomy in the United States. Am J Epidemiol. 1990;132:910–925 [DOI] [PubMed] [Google Scholar]
- 2. Fitz RH. Perforating inflammation of the vermiform appendix: with special reference to its early diagnosis and treatment. Am J Med Sci. 1886;92:321–346 [Google Scholar]
- 3. Fischer CP, Castaneda A, Moore F. Laparoscopic appendectomy: indications and controversies. Semin Laparosc Surg. 2002;9:32–39 [PubMed] [Google Scholar]
- 4. Golub R, Siddiqui F, Pohl D. Laparoscopic versus open appendectomy: A meta-analysis. J Am Coll Surg. 1998;186:545–553 [DOI] [PubMed] [Google Scholar]
- 5. Li X, Zhang J, Sang L, et al. Laparoscopic versus conventional appendectomy – a meta-analysis of randomized controlled trials. BMC Gastroenterology. 2010;10:129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Sauerland S, Jaschinski T, Neugebauer EA. Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev. 2010;10:CD001546. [DOI] [PubMed] [Google Scholar]
- 7. Ali R, Khan MR, Pishori T, Tayeb M. Appendectomy for acute appendicitis: Is this a feasible option for developing countries? Saudi J Gastroenterol. 2010;16(1):25–29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Adisa AO, Arowolo OA, Salako AA, Lawal OO. Preliminary experience with laparoscopic surgery in Ile-Ife, Nigeria. Afr J Med Med Sc. 2009;38:351–356 [PubMed] [Google Scholar]
- 9. Edino ST, Mohammed AZ, Ochichia O, Anumah M. Appendicitis in Kano, Nigeria: A 5-year review of pattern, morbidity and mortality. Annals of African Medicine. 2004;3(1):38–41 [Google Scholar]
- 10. Okafor PI, Orakwe JC, Chianakwana GU. Management of appendiceal masses in a peripheral hospital in Nigeria: review of thirty cases. World J Surg. 2003;27(7):800–803 [DOI] [PubMed] [Google Scholar]
- 11. Osifo OD, Ogiemwonyi SO. Peritonitis in children: our experience in Benin-City, Nigeria. Surg Infect (Larchmt). 2011;12(2):127–130 [DOI] [PubMed] [Google Scholar]
- 12. Larsson PG, Henriksson G, Olsson M, et al. Laparoscopy reduces unnecessary appendicectomies and improves diagnosis in fertile women. Surg Endosc. 2001;15:200–202 [DOI] [PubMed] [Google Scholar]
- 13. Van den Broek WT, Bijnen AB, van Eerten PV, de Ruiter P, Gouma DJ. Selective use of diagnostic laparoscopy in patients with suspected appendicitis. Surg Endosc. 2000;14:938–941 [DOI] [PubMed] [Google Scholar]
- 14. Tzovaras G, Liakou P, Baloyiannis I, et al. Laparoscopic appendectomy: Differences between male and female patients with suspected acute appendicitis. World J Surg. 2007;31:409–413 [DOI] [PubMed] [Google Scholar]
- 15. Fashina IB, Adesanya AA, Atoyebi OA, Osinowo OO, Atimomo CJ. Acute appendicitis in Lagos: a review of 250 cases. Niger Postgrad Med J. 2009;16(4):268–273 [PubMed] [Google Scholar]
- 16. Mangete ED, Kombo BB. Acute appendicitis in Port Harcourt, Nigeria. Orient Journal of Medicine. 2004;16(1):1–3 [Google Scholar]
- 17. Wei H, Huang JL, Zheng Z, et al. Laparoscopic versus open appendectomy: a randomized comparison. Surg Endosc. 2010;24:266–269 [DOI] [PubMed] [Google Scholar]
- 18. Kim SY, Hong SG, Roh HR, Park SB, Kim YH, Chae GB. Learning Curve for a laparoscopic appendectomy by a surgical trainee. J Korean Soc Coloproctol. 2010;26(5):324–328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Khan MN, Fayyad T, Cecil TD, Moran BJ. Laparoscopic versus open appendectomy: the risk of postoperative infectious complications. JSLS. 2007;11:363–367 [PMC free article] [PubMed] [Google Scholar]
- 20. Swank HA, Eshuis EJ, van Berge Henegugouwen MI, Bemelman WA. Short and long-term results of open versus laparoscopic appendectomy. World J Surg. 2011;35(6)1221–1226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Adler S, Scherrer M, Ruckauer KD, Daschner FD. Comparison of economic and environmental impacts between disposable and reuseable instruments used for laparoscopic cholecystectomy. Surg Endosc. 2005;19:268–272 [DOI] [PubMed] [Google Scholar]
- 22. Apelgren KN, Blank ML, Slomski CA, Hadjis NS. Reusable instruments are more cost effective than disposable instruments for laparoscopic cholecystectomy. Surg Endosc. 1994;8:32–34 [DOI] [PubMed] [Google Scholar]
- 23. Ali IV, Maliekkal JI. Laparoscopic appendicectomy using Endo-Ring applicator and Fallope Rings. Saudi J Gastroenterol. 2009;15(1):39–41 [DOI] [PMC free article] [PubMed] [Google Scholar]