This study suggests that training improves laparoscopic suturing skills in experienced as well as inexperienced laparoscopic surgeons.
Keywords: Laparoscopic suturing, Training, Trained surgeons, Novice surgeons
Abstract
Background:
Laparoscopic suturing is a difficult skill to master but can be acquired with extensive training outside the operating room. This study was done with the primary aim of assessing whether prior exposure to laparoscopic surgery helped trainees in acquiring laparoscopic suturing skills more quickly than trainees with no prior exposure to laparoscopic surgery.
Materials and Methods:
Twenty laparoscopy-exposed and 20 laparoscopy-naïve surgeons performed 5 laparoscopic gastrojejunostomies each on a phantom porcine model. The performance was evaluated for operation time, overall anastomotic score (calculated by adding scores of anastomotic leak, size of the anastomosis, suture placement, and mucosal approximation), and the level of difficulty. The performance at the beginning of training (baseline) was compared to the performance at the end of training.
Results:
All participants showed statistically significant improvement in operation time, overall anastomotic score, and difficulty level. Laparoscopy-exposed surgeons had a significantly better operation time than laparoscopy-naïve surgeons at the beginning of training; however, the difference became insignificant by the end of training. The difference in overall anastomotic score was not significant between laparoscopy-exposed and naïve-surgeons. Laparoscopy-exposed surgeons showed significant improvements in anastomotic leak rate and size of the anastomosis, whereas laparoscopy naïve surgeons showed improvements in all the parameters, although these were not significant statistically.
Conclusion:
Training improves the laparoscopic suturing skills of laparoscopy-exposed as well as laparoscopy-naïve surgeons. Prior experience in laparoscopic surgery does not seem to influence the acquisition of laparoscopic suturing skills as laparoscopic-naïve surgeons manage to catch up with the skills of the laparoscopy-exposed surgeons.
INTRODUCTION
With advances in technology, laparoscopic surgery has replaced open surgery in many surgical operations. Advanced surgical operations are now being done laparoscopically, and more reconstructive procedures are being performed. The skill of laparoscopic suturing is very important for performance of these advanced laparoscopic procedures.
Laparoscopic suturing skills are probably the most difficult skills to master in the minimally invasive environment because of the limitations of laparoscopic surgery, such as altered depth perception, 2-diminsional vision, counterintuitive movements, dependence on visual-spatial skills, and small working field.1,2 Though difficult, laparoscopic suturing skills can be acquired with extensive training, and acquisition of laparoscopic suturing skills is based on the principle of modeling, repetitive practice, and formative feedback.3,4
There is an ongoing debate in the literature whether prior exposure to laparoscopic surgery helps trainees in acquiring laparoscopic suturing skills faster. It has been shown in a few studies that previous laparoscopic experience is not necessary for the acquisition of laparoscopic suturing skills.4,5 As a result, many residency programs have included this as an essential skill in their curriculum.6,7 Even the Society of American Gastrointestinal Endoscopic Surgeons (SAGES) has introduced laparoscopic suturing in their Fundamentals of Laparoscopic Surgery (FLS) program.6,8
There are no studies in the literature in which trainees have done a full anastomosis and the acquisition of laparoscopic skills assessed on the basis of the anastomosis. This prospective study was done to assess the acquisition of laparoscopic suturing skills in a short-term training program in performance of laparoscopic gastrojejunostomy on a porcine phantom model and to compare whether prior exposure to laparoscopic surgery helped the trainees in acquiring laparoscopic suturing skills faster in comparison to trainees who had no previous exposure to laparoscopic surgery.
MATERIALS AND METHODS
This prospective study was conducted as a part of a 3-d intensive training in laparoscopic suturing skills for general surgery residents. Institute Ethics Committee clearance was obtained prior to the start of the study. Forty general surgery residents participating voluntarily who gave informed written consent for participation in the study were divided into 2 groups. General surgery residents who had more than 2 y experience in laparoscopic surgery and who had performed a laparoscopic cholecystectomy (generally residents in their fourth or fifth year of residency) were included in group 1 as laparoscopy-exposed surgeons. General surgery residents who had little or no exposure to laparoscopic surgery were included in group 2 as laparoscopy-naïve surgeons.
The Course
The participants were given 3 d of intensive training in laparoscopic suturing on a Tuebingen Trainer with integrated porcine organs.9–11 Each course consisted of 6 participants, and participants from both the groups were randomly allotted to a course. The course consisted of a video demonstration on principles of laparoscopic suturing that was followed by 2 h of practicing laparoscopic suturing on a cloth model with the help of instructors.
The trainees performed 5 laparoscopic gastrojejunostomies on a porcine phantom model in the Tuebingen Trainer.9–11 The trainees in both the groups were given no verbal or physical help to complete the anastomosis. The performance in the first case was taken as the baseline performance, and performance in the fifth case was taken as the final score. The results of the first and fifth cases were compared.
Preparation of the Model
Porcine organs (stomach and 15 cm of jejunum) taken from the slaughter house were integrated into the Tuebingen trainer after being prepared (irrigated, washed, frozen, and thawed). A 2-cm longitudinal anterior gastrostomy and enterotomy were made extracorporeally, and the organ was fixed in the Tuebingen trainer in the anatomical position. The participants were then shown a video of a laparoscopic gastrojejunostomy on the porcine model, and each participant performed 5 laparoscopic gastrojejunostomies on this model. A 30° 10-mm telescope was mounted on a Martin's Arm, and the trainee could adjust the camera according to their requirements. The gastrojejunostomy was performed in a single layer of inverting continuous suture using 2-0 Vicryl on a 30-mm half circle, round body needle and a thread length of 15 cm. The posterior layer was sutured before the anterior layer, starting from the right corner. At the end, the anterior and posterior sutures were tied together at the left corner. The technique of anastomosis, suturing, and knot tying was similar for each candidate and for each case.
Assessment
The performance of the candidates was recorded for every case. The operation time for each procedure was noted. The evaluation of the anastomosis was done extracorporeally. The quality of anastomosis was evaluated by assessing anastomotic leak, size of the anastomosis, suture placement, and mucosal approximation. The anastomotic leak was assessed by occluding both limbs of the jejunum and 1 end of the stomach with clamps (Figure 1a). The stomach was then filled with water from the open end, and any leak was scored as explained in the Table 1. The jejunum was split open along its mesenteric border to visualize the inside of the anastomosis for the evaluation of the size of the anastomosis, suture placement, and mucosal approximation, and these were assessed as shown in the Table 1 (Figure 1b). The score for anastomotic leak, size of the anastomosis, suture placement, and mucosal approximation were added to achieve the overall anastomotic score for each participant. The level of difficulty of the procedure was graded by each participant at the end of the procedure on a Likert scale from 1 to 4. The performance was assessed from case 1 to case 5, and the acquisition of laparoscopic suturing skills was compared between the 2 groups on various parameters as previously described.
Figure 1.
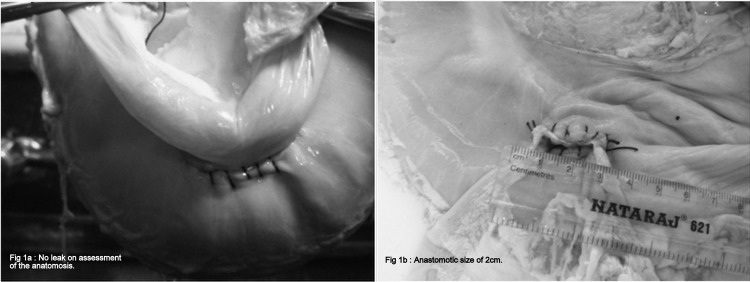
a. Extracorporeal assessment of anastomotic leak by filling the jejunum and stomach with water. b. Extracorporeal assessment of size of anastomosis, suture placement and mucosal approximation.
Table 1.
Assessment Criteria for Performance
| 1. Operative Time | Measured in Minutes | |||
| 2. Quality of the Anastomosis | Score 1 | Score 2 | Score 3 | Score 4 |
| A. Anastomotic Leak | Major Leak | Minor Leak | No Leak | — |
| B. Size of the anastomosis | Complete closure | <1 cm | ≥1 cm–<2 cm | 2 cm |
| C. Suture Placement | <0.5 | >1 cm | 0.5–1 cm | — |
| D. Mucosal approximation | Poor | Satisfactory | — | — |
| Anastomotic Score | Total of A, B, C, D | |||
| 3. Difficulty level | Difficult | Not Difficult | Not Easy | Easy |
Statistical Analysis
Statistical analysis was done using Stata/S.E 9.1 software. Improvement from case 1 to case 5 was analyzed using Friedman's test (for anastomotic leak, suture placement, and difficulty level), Cochran's Q test (for mucosal approximation), and Wilcoxon signed rank test (for operation time and size of the anastomosis). The performance of trained and novice surgeon was compared using the Pearson χ2 test for anastomotic leak, suture placement, and difficulty level. The Mann-Whitney test was used to compare operation time and the size of the anastomosis. Correlation of continuous variables with age and experience was assessed with the Spearman's rank correlation test. Correlation of discrete variables with age and experience were assessed with the Karl-Pearson correlation test. P<.05 was considered statistically significant.
RESULTS
The age of the participants ranged from 22 y to 36 y with a mean age of 28.2±3.4. There was a significant difference in the mean age between the 2 groups (30.9±2.5 y vs 25.5±1.8 y, P=.001). There were 38 male and 2 female participants. All the participants were right-handed surgeons. The participants belonged to various levels of residency from postgraduate year (PGY) 1 to 6 (Table 2). None of the participants admitted having any prior skill or practice in laparoscopic suturing techniques. The average number of procedures performed by the trainees is given in Table 3.
Table 2.
Demographic Profile–Age Distribution (years)
| Group I N(%) | Group II N(%) | |
|---|---|---|
| Age | 30.9±2.5 (27–36) | 25.5±1.8 (22–28) |
| PGY 1 | 0 | 18 (45%) |
| PGY 2 | 0 | 2 (5%) |
| PGY 3 | 3 (7.5%) | 0 |
| PGY 4 | 3 (7.5%) | 0 |
| PGY 5 | 9 (22.5%) | 0 |
| PGY 6 | 5 (12.5%) | 0 |
PGY = Post Graduate Year.
Table 3.
Exposure to Laparoscopic Surgery
| Procedure | Group I |
Group II |
P Valuea | ||
|---|---|---|---|---|---|
| Assisted | Performed | Assisted | Performed | ||
| Diagnostic Lap | 40.0±109.2 (0–500) | 2.8±3.5 (0–10) | 1.5±2.8 (0–10) | 0 | 0.001 |
| Lap Cholecystectomy | 62.5±45.3 (0–200) | 13.5±16.1 (0–55) | 5.3±4.9 (0–15) | 0 | 0.0006 |
| Lap Appendectomy | 9.1±5.5 (3–20) | 1.3±1.9 (0–5) | 0.2±0.4 (0–2) | 0 | 0.004 |
| Lap ventral hernia repair | 20.1±12.5 (2–50) | 0.6±1.4 (0–3) | 1.6±2.3 (0–5) | 0 | 0.06 |
| Lap inguinal hernia repair | 24.5±19.5 (6–100) | 0.6±1.4 (0–5) | 1.7±2.3 (0–5) | 0 | 0.06 |
| Open bowel anastomosis | 73.4±103.9 (0–400) | 21.5±31.7 (0–150) | 2.2±3.1 (0–10) | 0 | 0.004 |
P value calculated by unpaired t-test for laparoscopic surgeries performed.
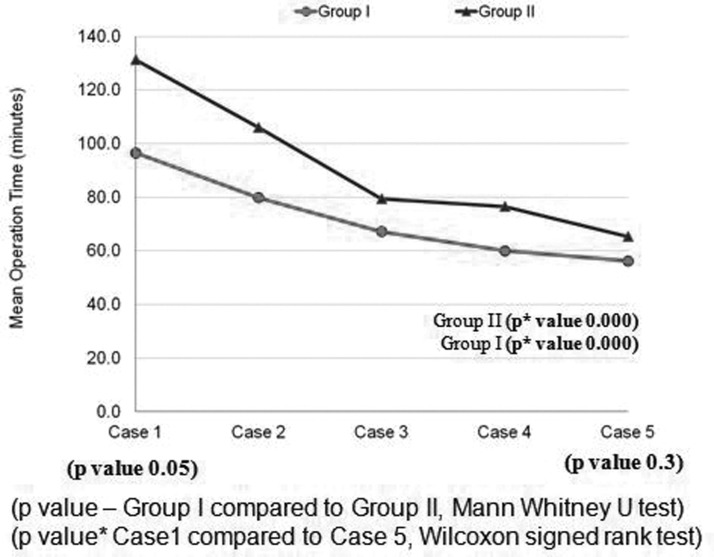
The trainees showed a statistically significant improvement in the mean operation time (113.8±55.4 min to 60.7±20.6 min, P<.0001) from the baseline evaluation to the final score. Participants in group 1 took significantly less operative time at the baseline evaluation. It was observed that with training the difference between the 2 groups that existed at the baseline evaluation (P=.05) disappeared by the fifth case (final score)(P=.3, Figure 2). The tasks were also performed by 2 senior consultants, and their mean operative time was 42.6 min with a range of 35 to 55 min.
Figure 2.
Comparison of mean operation time (Minutes).
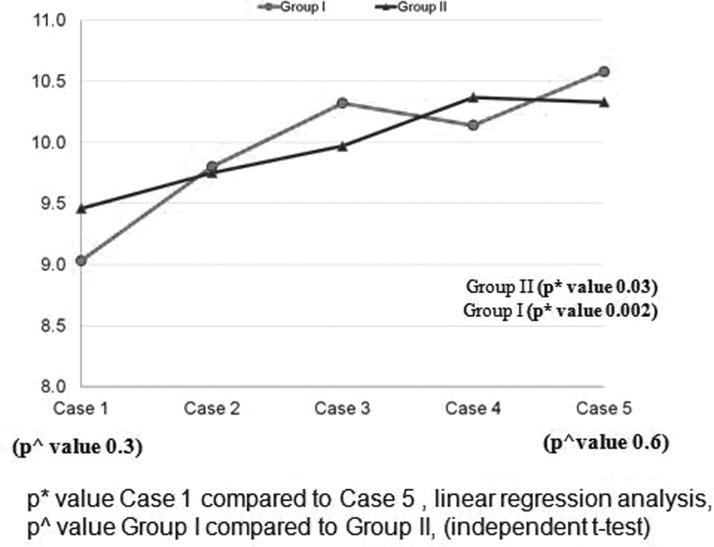
The study group showed a significant improvement in the overall anastomotic score from the baseline evaluation to the final evaluation (9.2 vs 10.4, P=.001, Figure 3). Laparoscopy-exposed surgeons had a better anastomotic score at the baseline evaluation, (9.46 vs 9.03, P=.3); however, the laparoscopy-naïve surgeons managed to catch up on their skills at the time of final evaluation, and the difference between the 2 groups narrowed (10.58 vs 10.33, P=.6).
Figure 3.
Comparison of overall anastomotic score.
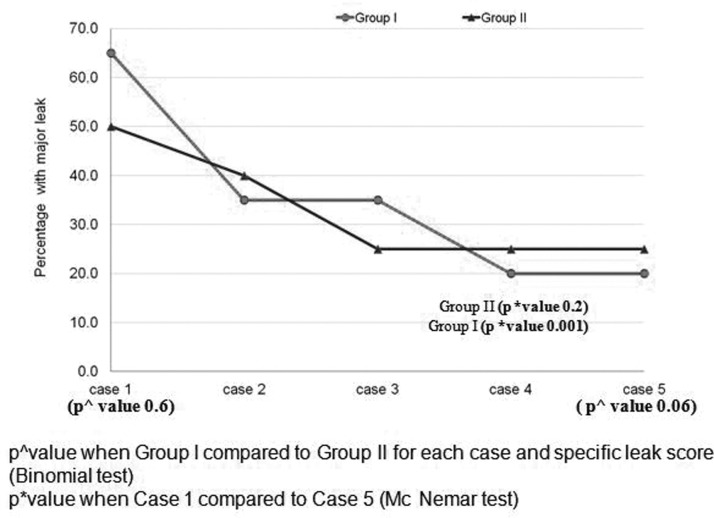
All the participants showed a significant improvement in major anastomotic leak rate (P=.003) and size of the anastomosis (P=.002). Although there was an improvement in adequate suture placement and satisfactory mucosal approximation, the improvement was not statistically significant (P=.6 and P=.3, respectively).
Considering each parameter individually for quality of anastomosis, laparoscopy-exposed surgeons had a significant improvement from the baseline to the end of training in major anastomotic leak rate (P=.001) (Figure 4) and size of the anastomosis (P=.01). The improvement in mucosal approximation and suture placement was not significant. On the other hand, although laparoscopy-naïve surgeons had significant improvement in the overall quality of anastomosis with training, the improvement was not significant for any parameter individually.
Figure 4.
Comparison of anastomotic leak.
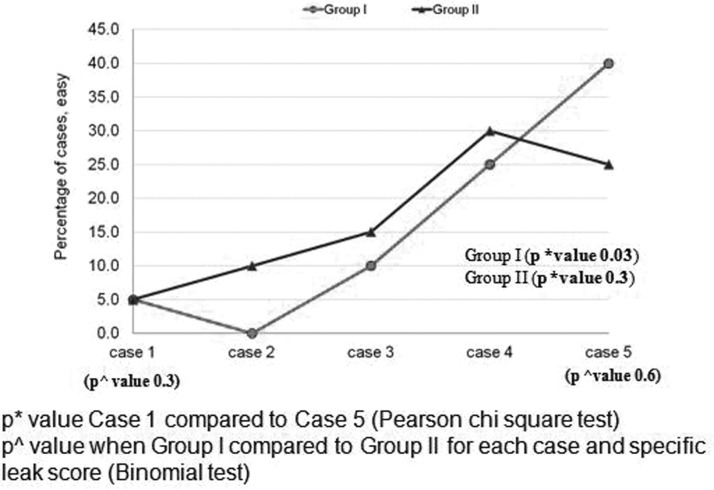
Each participant assessed the level of difficulty at the end of each case (Figure 5). The assessment of the level of difficulty of laparoscopic gastrojejunostomy improved with training for the entire study population (P<.001). The assessment of the level of difficulty was not found to be significantly different between the 2 groups at any time during the training.
Figure 5.
Comparison of assessment of difficulty level (percentage).
Another significant observation in our study was a negative correlation of mean operation time with age (correlation=−0.2233, P=.015) and experience (correlation=−0.2515, P=.0003) and a positive correlation of mucosal approximation with experience (correlation=0.1557, P=.0289). Significant correlation of age with experience (correlation=0.8839, P=.0001) (Table 4) was also noted.
Table 4.
Correlation with Age and Experience
| Age |
Experience |
|||
|---|---|---|---|---|
| Correlationa | P Valuea | Correlationa | P Valuea | |
| Operation Time | −0.2233 | 0.0015 | −0.2515 | 0.0003 |
| Anastomotic leak | 0.0861 | 0.2255 | 0.0588 | 0.4117 |
| Size of the anastomosis | −0.0180 | 0.8023 | −0.0488 | 0.4959 |
| Suture placement | 0.006 | 0.9328 | −0.0091 | 0.8990 |
| Mucosal approximation | 0.0766 | 0.2811 | 0.1557 | 0.0289 |
| Age with experience | 0.8839 | .0001 | ||
Karl Pearson correlation for continuous variables and Spearman's rank correlation for discrete variables.
DISCUSSION
Laparoscopic suturing skill is probably the most difficult skill to master in the minimally invasive environment.1,12 Despite the difficulty, studies reveal that these skills can be acquired with extensive training outside the operating room.2,5,7,8,13 However, the baseline skills required by the subject to learn laparoscopic suturing skills have not been defined, though many studies have found that previous laparoscopic exposure is not required for the acquisition of laparoscopic skills.
The method to assess acquisition of laparoscopic suturing skill varies among studies and has not been uniform. They vary from assessment of single intracorporeal knotting to 100 consecutive knots.3,14 No previous study has assessed the laparoscopic suturing skills of surgical trainees in the performance of bowel anastomosis on a porcine model in an almost real scenario. This is possibly the first study where laparoscopic suturing skills acquisition has been assessed by operation time, anastomotic leak, and size of the anastomosis, suture placement, mucosal approximation, and difficulty level.
Operation time is a significant parameter to assess the laparoscopic skills of a surgeon. It has been used as an objective measure of the acquisition of laparoscopic skills by many studies such as those done by Rosser et al.15 Vossen et al.16 Chung et al.17 Risucci et al.18 and Dubrowski et al.6 These studies reveal that as the surgeon becomes more skillful, operation time decreases and reaches a minimum level that is similar to that of the experts.19–21 In the present study, training resulted in significant improvement in mean operation time for all the participants. It was the first and the most significant parameter to improve after training. The difference in the operation time between the laparoscopy-exposed and laparoscopy-naïve surgeons also decreased significantly after the training course, signifying that training definitely shortens the learning curve for laparoscopic suturing skills for both the laparoscopy-exposed and laparoscopy-naïve surgeons and that the laparoscopy-naïve surgeons manage to catch up with the laparoscopy-exposed surgeons after training.
However, the trainees in our program could not reach the level of experts possibly because laparoscopic suturing is a very difficult task to master, and although they showed significant improvement in operative time, they still need more practice to reach the level of experts. The trainees showed a significant improvement in the overall anastomotic score from the baseline to the postcourse evaluation, which signifies that training helped them in acquiring the skills of laparoscopic suturing. The laparoscopy-naïve surgeons also had a significant improvement in the anastomotic score.
Similar improvement in laparoscopic suturing skills with training was also observed by Kanumuri et al.13 who found that third-year medical students improved task completion rate and time with training. Botden et al.22 observed statistically significant improvement in 18 novice medical students from the second knot to the top of the performance. Vossen et al.16 observed 100 consecutive intracorporeal suturings after a training and found that the quality of the knots increased when the first 10 were compared to the last 10 knots.
Few studies have shown that experience in laparoscopic procedures is not a prerequisite for trainees to learn laparoscopic suturing techniques and that novice surgeons can acquire complex skills of laparoscopic suturing in a shorter and similar time as compared to the trained surgeons. Aggarwal et al.4 who compared the performance of 9 senior operative residents (PGY 4 and 5; course A) with 14 junior operative resident (PGY 2 and 3) at an identical 2-d laparoscopic suturing course, had similar observations. In a study done by Stefanidis et al.23 novices demonstrated a 22-fold increase in performance after uniformly achieving proficiency in a reasonable (5.6 h) amount of time. Risucci et al.18 found significant and similar improvement in both the resident and attending surgeons from suturing trials 1 to 3 and trials 8 to 15.
The observations in our study are similar to the above-mentioned studies. Laparoscopy-naïve surgeons, despite the limitation of their minimal previous laparoscopic surgery experience and even exposure to open bowel anastomosis, were capable of learning basic laparoscopic skills as effectively and efficiently as the trained surgeons. It was seen that though the laparoscopy-exposed surgeons were faster than the laparoscopy-naïve surgeons in the beginning of the study, this difference in mean operation time between the 2 groups decreased significantly after training.
Many studies have shown variable effect of age and experience on acquisition of laparoscopic suturing skills. Rissuci et al.18 and Kroeze et al.3 demonstrated a positive relationship between laparoscopic suturing skill and experience. Our study also suggests that as age increases mean operation time decreases and as experience increases the mean operation time decreases and the mucosal approximation improves. Thus, with age, experience increases and both lead to better acquisition of laparoscopic suturing skills. However, Vossen et al.16 and Aggarwal et al.4 had observed that performance was not related to experience or age, respectively. The application and transfer of these skills in the operating theater directly on patients has not been studied and the sustainability and transfer of the skills acquired was not assessed due to logistical problems of retesting the individuals.
Though the relation of experience to acquisition of laparoscopic suturing skills is controversial, there may be some benefit to having previous experience in laparoscopic or open surgical procedures. One explanation is that laparoscopy-naïve surgeons had to first overcome the basic skills of laparoscopy, such as bimanual dexterity, depth perception, absence of haptic feedback, and other such things, accounting for their initially prolonged operative time. However, once they overcame this, they made significant improvement in the operative time and also the overall anastomotic score. Laparoscopy-exposed surgeons were able to achieve significant improvements in anastomotic leak rate and size of the anastomosis apart from the mean operation time. The overall anastomotic score was greater than that of the laparoscopy-naïve surgeons; however, the difference was not statistically significant. Our observations suggest that this group of participants acquired knowledge of the methods for laparoscopic suturing and were able to apply this knowledge without difficulty. Further, their experience in performing a secure anastomosis in open surgical procedures may have benefitted them. On the other hand, laparoscopy-naïve surgeons had to acquire knowledge of basic laparoscopic skills, laparoscopic suturing, bowel anastomosis, and dexterity during the 3-d course and hence could not achieve further improvement in mean operative time and other parameters. Since laparoscopic suturing is a complex skill involving several tasks, the mental workload threshold of participants, along with the short duration of training, probably prevented the laparoscopy-exposed surgeons from improving on their performance. Hence, it can be deduced from our study that training leads to improvement in skills in all the residents irrespective of their previous exposure to laparoscopic surgery. Laparoscopy-naïve surgeons can acquire skills comparable to that of the trained surgeons.
The findings of this study need to be tested on a larger scale with a greater number of trainees, and if the findings are proven and the skills are identical between the 2 groups, then it can have important implications in the training requirements of laparoscopy-naïve residents whereby it may become mandatory for laparoscopy-naïve as well as practicing surgeons to undergo training before they are exposed to the operating theater environment.
CONCLUSION
It may be inferred from our study that training improves the laparoscopic suturing skills of laparoscopy-exposed as well as laparoscopy-naïve surgeons and definitely helps in decreasing the learning curve. Prior experience in laparoscopic surgery does not seem to influence the acquisition of laparoscopic suturing skills, as laparoscopy-naïve surgeons catch up with the skills of the laparoscopy-exposed surgeons.
Acknowledgments
The laparoscopic equipment in the Minimally Invasive Surgery Training Centre, All India Institute of Medical Sciences, New Delhi, India was donated by Richard Wolf, Knittlingem, Germany as one time educational grant, and technical support for establishing this training centre was provided by Prof GF Buess and Mrs Lilo Mailander, Section for Minimally Invasive Surgery, Eberhard-Karls University Tuebingen, Tuebingen, Germany.
Contributor Information
Virinder Kumar Bansal, Department of Surgical Disciplines, All India Institute of Medical Sciences, New Delhi, India..
Tseten Tamang, Department of Surgical Disciplines, All India Institute of Medical Sciences, New Delhi, India..
Mahesh C. Misra, Department of Surgical Disciplines, All India Institute of Medical Sciences, New Delhi, India..
Pradeep Prakash, Department of Surgical Disciplines, All India Institute of Medical Sciences, New Delhi, India..
Karthik Rajan, Department of Surgical Disciplines, All India Institute of Medical Sciences, New Delhi, India..
Hemanga K. Bhattacharjee, Department of Surgical Disciplines, All India Institute of Medical Sciences, New Delhi, India..
Subodh Kumar, Department of Surgical Disciplines, All India Institute of Medical Sciences, New Delhi, India..
Amit Goswami, Department of Surgical Disciplines, All India Institute of Medical Sciences, New Delhi, India..
References:
- 1. Gurusamy K, Aggarwal R, Palanivelu L, Davidson BR. Systematic review of randomized controlled trials on the effectiveness of virtual reality training for laparoscopic surgery. Br J Surg. 2008;95:1088–1097 [DOI] [PubMed] [Google Scholar]
- 2. Moorthy K, Munz Y, Dosis A, Bello F, Chang A, Darzi A. Bimodal assessment of laparoscopic suturing skills. Surg Endosc. 2004;18:1608–1612 [DOI] [PubMed] [Google Scholar]
- 3. Kroeze GCS, Mayer EK, Chopra S, Aggarwal R, Darzi A, Patel A. Assessment of laparoscopic suturing skills of urology residents: a pan-European study. Eur Urol. 2009;56:865–873 [DOI] [PubMed] [Google Scholar]
- 4. Aggarwal R, Hance J, Undre S, et al. Training junior operative residents in laparoscopic suturing skills is feasible and efficacious. Surgery. 2006;139:729–734 [DOI] [PubMed] [Google Scholar]
- 5. Brown DC, Miskovic D, Tang B, Hanna GB. Impact of established skills in open surgery on the proficiency gain process for laparoscopic surgery. Surg Endosc. 2010;24:1420–1426 [DOI] [PubMed] [Google Scholar]
- 6. Dubrowski A, Park J, Moulton C, Larmer J, MacRae H. A comparison of single and multiple stage approaches to teaching laparoscopic suturing. Am J Surg. 2007;193:269–273 [DOI] [PubMed] [Google Scholar]
- 7. Nguyen PH, Acker CE, Heniford BT, Stefanidis D. What is the cost associated with the implementation of the FLS program into a general surgery residency? Surg Endosc. 2010;24:3216–3220 [DOI] [PubMed] [Google Scholar]
- 8. Rosenthal ME, Ritter EM, Goova MT, et al. Proficiency-based Fundamentals of laparoscopic surgery skills training results in durable performance improvement and a uniform certification pass rate. Surg Endosc. 2010;24:2453–2457 [DOI] [PubMed] [Google Scholar]
- 9. Bansal VK, Panwar R, Misra MC, Bhattacharjee HK, Jindal V, Loli A, Goswami A, Krishna A, Tamang T. Are short-term focused training courses on a phantom model using porcine gall bladder useful for trainees in acquiring basic laparoscopic skills? Surg Laparosc Endosc Percutan Tech. 2012;22:154–60 PMID:22487631 [DOI] [PubMed] [Google Scholar]
- 10. Waseda M, Inaki N, Mailender L, Buess GF. An innovative trainer for surgical procedures using animal organs. Minim Invasive Ther Allied Technol. 2005;14:262–266 [DOI] [PubMed] [Google Scholar]
- 11. Raestrup H, Mailender L, Roth K, Mannche K. Phantom training courses in Tuebingen. Minim Invasive Ther Allied Technol. 2000;9:311–314 [Google Scholar]
- 12. Misra MC, Bansal VK, Bhowate P, Bhattacharya H. Training in laparoscopic surgery. JIMSA. 2007;20:15–19 [Google Scholar]
- 13. Kanumuri P, Ganai S, Wohaibi EM, Bush RW, Grow DR, Seymour NE. Virtual reality and computer-enhanced training devices equally improve laparoscopic surgical skills in novices. JSLS. 2008;12:219–226 [PMC free article] [PubMed] [Google Scholar]
- 14. Pearson AM, Gallagher AG, Rosser JC, Satava RM. Evaluation of structured and quantitative training methods for teaching intracorporeal knot tying. Surg Endosc. 2002;6:130–137 [DOI] [PubMed] [Google Scholar]
- 15. Rosser JC, Rosser LE, Savalgi RS. Skill acquisition and assessment for laparoscopic surgery. Arch Surg. 1997;132:200–204 [DOI] [PubMed] [Google Scholar]
- 16. Vossen C, Ballaer PV, Shaw RW, Koninckx PR. Effect of training on endoscopic intracorporeal knot tyring. Hum Reprod. 1997;12:2658–2663 [DOI] [PubMed] [Google Scholar]
- 17. Chung SY, Landsittel D, Chon CH, Ng CS, Fuchs GJ. Laparoscopic skills training using a webcam trainer. J Urol. 2005;173:180–183 [DOI] [PubMed] [Google Scholar]
- 18. Risucci D, Geiss A, Gellman L, Pinard B, Rosser J. Surgeon-specific factors in the acquisition of laparoscopic surgical skills. Am J Surg. 2001;181:289–293 [DOI] [PubMed] [Google Scholar]
- 19. Gallagher AG, Lederman AB, McGlade K, Satava RM, Smith CD. Discriminative validity of the Minimally Invasive Surgical Trainer in Virtual Reality (MIST-VR) using criteria levels based on expert performance. Surg Endosc. 2004;18:660–665 [DOI] [PubMed] [Google Scholar]
- 20. Grantcharov TP, Kristiansen VB, Bendix J. Randomized clinical trial of virtual reality simulation for laparoscopic skills training. Br J Surg. 2004;91:146–150 [DOI] [PubMed] [Google Scholar]
- 21. Seymour NE, Gallagher AG, Roman SA. Virtual reality training improves operating room performance: results of a randomized double blinded study. Ann Surg. 2002;236:458–463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Botden SM, de Hingh IH, Jakimowicz JJ. Suturing training in augmented reality: gaining proficiency in suturing skills faster. Surg Endosc. 2009;23:2131–2137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Stefanidis D, Korndorffer JR, Sierra R, Touchard C, Dunne B, Scott DJ. Skill retention following proficiency-based laparoscopic simulator training. Surgery. 2005;138:165–170 [DOI] [PubMed] [Google Scholar]