Abstract
Background
Smoking marijuana has been reported to increase risk of myocardial infarction (MI) immediately after use, but less is known about the long-term impact of marijuana use among patients with established coronary disease.
Methods
The Determinants of MI Onset Study (MIOS) is a multicenter inception cohort study of MI patients enrolled in 1989–1996 and followed for mortality using the National Death Index. In an initial analysis of 1935 MI survivors followed for a median of 3.8 years, we found an increased mortality rate among marijuana users. The current paper includes 3886 MIOS patients followed for up to 18 years. We used Cox proportional hazards models to calculate the hazard ratio and 95% confidence interval for the association between marijuana use and mortality and a propensity score matched analysis to further control confounding.
Results
Over up to 18 years of follow-up, 519 patients died, including 22 of the 109 reporting marijuana use in the year prior to their MI. There was no statistically significant association between marijuana use and mortality. Compared to non-users, the mortality rate was 29% higher (95% confidence interval 0.81 to 2.05, p=0.28) among those reporting any marijuana use.
Conclusions
Habitual marijuana use among patients presenting with acute MI was associated with an apparent increased mortality rate over the following 18 years that did not reach nominal statistical significance. Larger studies with repeated measures of marijuana use are needed to definitively establish whether there are adverse cardiovascular consequences of smoking marijuana among patients with established coronary heart disease.
Introduction
Marijuana is the most commonly used illicit drug in the United States, and it is becoming increasingly popular over time. In 2009, it was estimated that 16.7 million (6.6%) people ages 12 and older had used marijuana in the past month. Between 2002 and 2009, the rate of current illicit drug use increased from 2.7 to 6.2% among adults ages 50 to 59.1 Despite the common and increasing use, few studies have examined the long-term impact of marijuana use, a question that is of particular public health interest with the aging of the baby boomers who are now at risk for cardiovascular disease or who already are known to have coronary artery disease.
Cannabanoids are associated with both harmful2–4 and protective effects.7 The main active constituent of marijuana, tetrahydrocannabinol (THC), is a mixed agonist for cannabinoid 1 and 2 receptors (CB1 and CB2).7 Activation of CB1 receptors may increase lipid resistance and promote chronic cardiovascular dysfunction in obesity3 and diabetes2; on the other hand activation of CB2 receptors may suppress the inflammatory response5 and in turn, reduce atherosclerosis progression.6 In terms of short-term effects, marijuana can acutely lead to cardiac ischemia in susceptible individuals by causing a catecholamine release that in turn increases resting heart rate, ischemia, and arrhythmias. Additionally, smoking marijuana decreases vascular resistance leading to orthostatic hypotension, limits oxygen uptake by increasing levels of carboxyhemoglobin, and may delay the treatment of chest pain because of the analgesic properties of THC.8 Furthermore, marijuana use has been associated with a short-term increased risk of myocardial infarction in adults9 and children.4
Little is known about the association between marijuana use and survival, particularly among those at highest cardiovascular risk, such as those who have survived an MI. We previously showed that the rate of myocardial infarction (MI) is 4.8 times greater (95% confidence interval [CI] 2.4 to 9.5) in the hour following marijuana use compared to other times.9 Regarding the risk from habitual marijuana use, several studies have reported that there is a relationship between heavy cannabinoid use and all-cause mortality10–13 and some14–16, but not all, studies have shown that there is a higher mortality rate associated with cannabinoid use in the general population. In a preliminary analysis of 1913 MIOS study participants including 52 people reporting marijuana use in the year prior to MI that were followed for a median of 3.8 years,19 we found that compared with nonusers, using marijuana less than once per week was associated with a 2.5-fold (95% CI 0.9 to 7.3) higher rate of mortality, and the corresponding hazard ratio for using marijuana once or more per week was 4.2 (95% CI 1.2 to 4.3). It remains unclear whether marijuana use is associated with increased mortality among MI survivors over longer follow-up times. Therefore, we extended our previous analysis of the MIOS study19 to include a larger sample size (3886 participants, including 109 marijuana users) with up to 18 years of follow-up. We hypothesized that compared to no use, self-reported marijuana use would be associated with a higher rate of all-cause mortality among patients who sustained an MI, and that there would be a dose-response relationship with higher mortality rates for greater frequency of marijuana use.
Methods
Enrollment and Data Collection
The Determinants of MI Onset Study (MIOS) is a multicenter study of MI patients enrolled in 1989–1996 and followed for mortality using the National Death Index. Altogether, 3886 patients hospitalized in 64 centers nationwide were interviewed a median of 4 days (range 0 to 30 days) after sustaining an MI. As described previously,9 trained interviewers identified eligible patients by reviewing coronary care unit admission logs and patient charts. For inclusion, patients were required to have a creatine kinase level above the upper limit of normal for each center, positive MB isoenzymes, an identifiable onset of symptoms of infarction, and the ability to complete a structured interview. The institutional review board of each center approved the protocol and each participant gave informed consent. Subsequent approval was obtained from the Beth Israel Deaconess Medical Center Committee on Clinical Investigations to search publically available mortality records.
Exposure and Covariate Assessment
Trained research personnel conducted a standardized interview to obtain information about the time, place, and quality of MI pain and other symptoms. In addition, patients were asked about several possible triggers including, “Have you used marijuana, cocaine, or amphetamines in the past year?”. If the person answered affirmatively, they were asked, “how often do you use it?” and “when did you last use it?”. We categorized responses for marijuana use in the year preceding MI as any use, less than weekly, or marijuana use once per week or more. One person reported smoking marijuana in the year before MI, but he did not report how often he smoked marijuana, so he is included in the analyses of risk from any marijuana but not the analysis of weekly and monthly marijuana use. Research personnel reviewed medical charts to collect information including age, sex, marital status, medication use, history of hypertension, diabetes, heart failure, MI and non-cardiac comorbidities including respiratory disease, renal failure, cancer or stroke. Height and weight were self-reported and used to derive body mass index. Usual frequency of physical activity was assessed with a validated scale developed for the study.20 We used 2000 U.S. Census data on median household income at the block group level.
Outcome Assessment
All participants were administratively censored on December 31, 2007 or date of death, whichever came first. We searched the National Death Index for deaths of Onset Study participants and requested death certificates from state offices of vital records for all probable matches using a previously validated algorithm that included name, date of birth, sex, race, marital status, and state.23 Three physicians independently verified the determination of each death and disagreements among raters were resolved by discussion. All-cause mortality was the primary outcome in all analyses; in the primary analysis, we examined the association between marijuana use and the rate of mortality over up to 18 years of follow-up, and in a sensitivity analysis, we restricted the analysis to the first 10 years of follow-up to examine the period closer to the index event.
Statistical Analysis
We constructed Cox proportional hazards models and calculated hazard ratios and 95% confidence intervals to examine the relationship between any self-reported marijuana use and all-cause mortality. We also constructed a model with a term for marijuana use less than once per week and a term for marijuana use once or more per week. We tested whether there was a dose-response relationship by creating a continuous variable and assigning ordinal values for no use, less than once per week and one or more times per week and we used the Wald χ2 to formally test for the gradient in risk.
In an initial model, we adjusted for age and sex. In a second model, we further adjusted for covariates selected a priori based on their plausible relationship with marijuana use and for consistency with our prior study19: age (continuous), sex, race (white versus other), body mass index (continuous and quadratic terms), marital status (married versus other), smoking status (never, former, current), usual frequency of physical activity (none, 1 to 4 episodes per week, 5 or more episodes per week), tea consumption (none, <2 cups per day, 2 or more cups per day), alcohol intake (tertiles), binge drinking (≥3 drinks in a 2-hour period within the last year, yes/no), any cocaine use in the previous year (yes/no), neighborhood median household income (tertiles), years of education (less than high school, high school graduate, some college), previous MI, congestive heart failure, diabetes mellitus, hypertension, noncardiac comorbidities (yes/no), current medication use (yes/no; aspirin, β-blockers, calcium-channel blockers, digoxin, diuretics, hypolipidemic agents, and angiotensin-converting enzyme inhibitors), thrombolytic therapy.
In a sensitivity analysis, we restricted the analysis to the first 10 years of follow-up; in another analysis, we examined whether the association was different for the first (August 1989–September 1994) and second (October 1994–September 1996) cohorts of enrolled patients by testing the significance of an interaction term for any marijuana use and enrollment cohort. Only the first cohort was included in our prior report.19
In an additional sensitivity analysis, we calculated propensity scores to further address confounding between those who did and did not report recent marijuana use. The propensity score is the individual’s probability of self-reported marijuana use, based upon demographic, behavioral, and clinical characteristics. Scores were generated using a logistic regression model, with marijuana use as the dependent variable, and the covariates listed for the Cox models above were included as independent variables. We used the nearest available pair matching method24 to match each marijuana user to two nonusers. Twenty-two marijuana users were excluded from the sensitivity analysis because of disjoint propensity scores. We compared Kaplan-Meier estimates of survival using the log-rank test among those with available propensity score matched pairs, and inspected the resulting curve to conduct a sensitivity analysis for relevant time windows.
We tested the proportional hazards assumption in the Cox models by testing the statistical significance of a term for the interaction between marijuana use and the natural logarithm of time, and we found no evidence that the association between marijuana use and all-cause mortality varied over time during the follow-up period (p=0.42). We also examined the log -log plots and found no departure from the proportional hazards assumption. We used SAS version 9.2 (SAS Institute, Cary, NC). All P values presented are 2-sided, and we considered values <0.05 to be statistically significant.
This work was supported by a training grant from the National Institutes of Health (T32-HL098048) and the Harvard Medical School Scholars in Medicine Office. The original data was collected with funding from the National Institutes of Health. The authors are solely responsible for the design and conduct of this study, all study analyses, the drafting and editing of the paper and its final contents.
Results
There were 3886 patients enrolled in the Onset Study. Since all marijuana users were 63 years of age or younger, we excluded MI patients older than 63 years of age (n=1767) to avoid extrapolations beyond the range of observed data. Additionally, we excluded people with no information on marijuana use (n=22), resulting in a final sample size of 2097 for this analysis. There were 109 patients (5.2%) who reported marijuana use in the year preceding their MI. Marijuana users tended to be younger, male, current smokers, heavy alcohol drinkers, unmarried, and had fewer comorbidities than nonusers (Table I).
Table I.
Characteristics of Onset Study participants according to self-reported marijuana use. Mean ± standard deviation or frequency (percent)
| Patient Characteristics | Marijuana Use | |
|---|---|---|
| Yes (n=109) | No (n=1,988) | |
| Age (y) | 43.7 ± 8.2 | 52.3 ± 7.7 |
| Female | 7 (6) | 465 (23) |
| White | 85 (78) | 1710 (86) |
| Education | ||
| Less than high school | 21 (19) | 370 (19) |
| High School Graduate | 45 (41) | 799 (40) |
| Some College | 38 (35) | 785 (39) |
| Median Household Income ($k) | 34.7 ± 17.5 | 38.9 ± 16.5 |
| Education (years of schooling) | 12.9 ± 2.8 | 13.1 ± 3.2 |
| Married | 50 (46) | 1416 (71) |
| Body Mass Index (kg/m2) | 29.9 ± 5.6 | 28.3 ± 5.2 |
| Smoking Status | ||
| Never | 11 (10) | 354 (18) |
| Former | 24 (22) | 670 (34) |
| Current | 73 (67) | 956 (48) |
| Episodes Physical Activity per Week | ||
| None | 78 (72) | 1616 (81) |
| 1 to 4 | 22 (20) | 291 (15) |
| ≥5 | 9 (8) | 81 (4) |
| Weekly Alcohol Consumption (cups) | 15.9 ± 29.6 | 6.8 ± 53.2 |
| Binge Drinking | 58 (53) | 392 (20) |
| Cocaine | 17 (16) | 29 (1) |
| History of | ||
| Hypertension | 30 (28) | 741 (37) |
| Diabetes Mellitus | 10 (9) | 341 (17) |
| Myocardial Infarction | 24 (22) | 427 (21) |
| Angina | 12 (11) | 408 (21) |
| Congestive Heart Failure | 1 (1) | 41 (2) |
| Noncardiac comorbidities | 5 (5) | 210 (11) |
| Regular use of: | ||
| Aspirin | 41 (38) | 728 (37) |
| β-Blockers | 13 (12) | 343 (17) |
| Calcium Channel Blockers | 12 (11) | 378 (19) |
| Digoxin | 2 (2) | 65 (3) |
| Diuretics | 5 (5) | 204 (10) |
| Hypolipidemics | 8 (7) | 194 (10) |
| ACE inhibitors | 8 (7) | 211 (11) |
| Thrombolytic Therapy | 49 (45) | 919 (46) |
ACE=Angiotensin-converting enzyme.
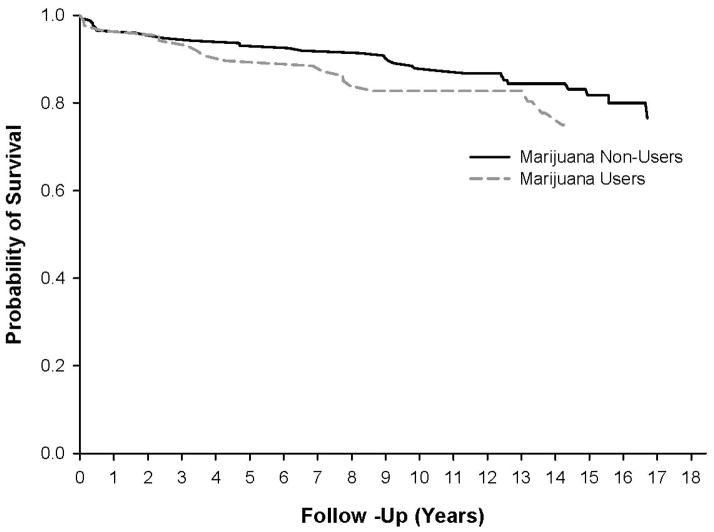
Over a median of 12.7 years of follow-up, 519 patients died, including 22 of the 109 patients reporting marijuana use at the time of their MI. In the fully adjusted models, any marijuana use in the year prior to MI was associated with a 29% higher rate of all-cause mortality (95% CI 0.81 to 2.05, p=0.28). Compared to non-users, the mortality rate was higher for people reporting marijuana use less than once per week (hazard ratio [HR]=1.31, 95% CI 0.74 to 2.35, p=0.36) and for those reporting use once or more per week (HR=1.27, 95% CI 0.63 to 2.56, p=0.51). There was no evidence of a dose-response relationship (p trend =0.32). The results were not materially different when the follow-up was restricted to 10 years (Table II). The prior report19 included participants of all ages from the first cohort, and this updated analysis includes all individuals 63 years of age and younger from both the first and second enrollment cohort. In fully adjusted models stratified by cohort, most estimates were higher in the first cohort than the second cohort (Table III), but there was no statistical evidence of differences by enrollment cohort (p interaction=0.80). In the analysis using propensity scores, we compared the survival of 87 marijuana users matched to 174 non-users, and the HR for association between any marijuana use and all-cause mortality was 1.10 (95% CI 0.62 to 1.96, p=0.74). The Figure shows the estimated survival among the marijuana users and non-users. The higher mortality rate associated with marijuana use appears to begin only after the first three years following the MI, but the assumption of proportional hazards in the matched cohort is not violated (p=0.94).
Table II.
Hazard ratios and 95% confidence intervals for the association between marijuana use and all-cause mortality among 2,097 participants in the MI Onset Study followed for up to 18 years
| Follow- Up | Marijuan a Use | # Deaths | Person -Years | Age/Sex Adjusted HR (95% CI) P-Value | Fully Adjusted* HR (95% CI) P-Value | P- trend† |
|---|---|---|---|---|---|---|
| 0–18 years | None | 497 | 24,452 | 1.00 (reference) | 1.00 (reference) | 0.32 |
| Any | 22 | 1,333 | 1.28 (0.82–1.98) 0.28 |
1.29 (0.81–2.05) 0.28 |
||
| <1 per Week | 13 | 706 | 1.36 (0.78–2.38) 0.28 |
1.31 (0.74–2.35) 0.36 |
||
| ≥1 per Week | 9 | 615 | 1.19 (0.61–2.33) 0.61 |
1.27 (0.63–2.56) 0.51 |
||
|
| ||||||
| 0–10 years | None | 355 | 18,085 | 1.00 (reference) | 1.00 (reference) | 0.17 |
| Any | 19 | 975 | 1.55 (0.96–2.49) 0.08 |
1.45 (0.88–2.40) 0.15 |
||
| <1 per Week | 11 | 511 | 1.63 (0.89–3.00) 0.12 |
1.45 (0.77–2.73) 0.26 |
||
| ≥1 per Week | 8 | 454 | 1.46 (0.72–3.00) 0.30 |
1.47 (0.69–3.12) 0.32 |
||
Adjusted for age (continuous), sex, race (white versus other), body mass index (continuous and quadratic terms), marital status (married versus other), smoking status (never, former, current), usual frequency of physical activity (none, 1 to 4 episodes per week, 5 or more episodes per week), tea consumption (none, <2 cups per day, 2 or more cups per day), alcohol intake (tertiles), binge drinking (≥3 drinks in a 2-hour period within the last year, yes/no), any cocaine use in the previous year (yes/no), neighborhood median household income (tertiles), years of education (less than high school, high school graduate, some college), previous MI, congestive heart failure, diabetes mellitus, hypertension, noncardiac comorbidities (yes/no), current medication use (yes/no; aspirin, β-blockers, calcium-channel blockers, digoxin, diuretics, hypolipidemic agents, and angiotensin-converting enzyme inhibitors), thrombolytic therapy.
P-trend for no marijuana use, <1 per week and ≥1 per week in the fully adjusted model
Table III.
Hazard ratios and 95% confidence intervals for the association between marijuana use and all-cause mortality among 2,097 participants in the MI Onset Study followed for up to 18 years, stratified by enrollment cohort*
| First Cohort August 1989–September 1994 (n=1037) | Second Cohort October 1994–September 1996 (n=1060) | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Marijuan a Use | # Deaths | Person -Years | HR (95% CI)† P-Value | # Deaths | Person- Years | HR (95% CI)† P-Value |
| None | 312 | 13,180 | 1.00 (reference) | 185 | 11,272 | 1.00 (reference) |
| Any | 14 | 693 | 1.49 (0.82–2.71) 0.19 |
8 | 640 | 1.08 (0.50–2.34) 0.84 |
| <1 per Week | 9 | 413 | 1.41 (0.69–2.89) 0.35 |
4 | 293 | 1.13 (0.40–3.21) 0.83 |
| ≥1 per Week | 5 | 279 | 1.66 (0.65–4.25) 0.29 |
4 | 335 | 1.05 (0.35–3.17) 0.93 |
The prior report19 included participants from the first enrollment cohort followed for a median of 3.8 years.
Adjusted for age (continuous), sex, race (white versus other), body mass index (continuous and quadratic terms), marital status (married versus other), smoking status (never, former, current), usual frequency of physical activity (none, 1 to 4 episodes per week, 5 or more episodes per week), tea consumption (none, <2 cups per day, 2 or more cups per day), alcohol intake (tertiles), binge drinking (≥3 drinks in a 2-hour period within the last year, yes/no), any cocaine use in the previous year (yes/no), neighborhood median household income (tertiles), years of education (less than high school, high school graduate, some college), previous MI, congestive heart failure, diabetes mellitus, hypertension, noncardiac comorbidities (yes/no), current medication use (yes/no; aspirin, β-blockers, calcium-channel blockers, digoxin, diuretics, hypolipidemic agents, and angiotensin-converting enzyme inhibitors), thrombolytic therapy.
Discussion
In this prospective multi-center cohort study of MI survivors followed prospectively for up to 18 years, there was no conclusive evidence of an association between smoking marijuana and mortality. Though we had wide confidence intervals and did not demonstrate statistical significance, our results seem consistent with prior studies, and suggest that there may be a higher mortality rate associated with marijuana use among MI survivors.
Our prior report19 of the first 1935 enrolled participants followed for a median of 3.8 years, including only 7 marijuana users that died, resulted in a statistically significant higher rate of death for users compared to non-users. However, in the present pooled analysis of 3886 participants from both enrollment cohorts followed for up to 18 years, there is no definitive evidence of an association. In an analysis stratified by enrollment cohort, there was an apparent stronger association among participants enrolled between August 1989 and September 1994 than the association among participants enrolled between October 1994 and September 1996. Over the duration of study enrollment, the case-fatality rate declined due to improvements in acute care including revascularization, and more widespread use of aggressive secondary prevention, such as beta-blockers, ace inhibitors and aspirin and improvements in risk factors including blood pressure and cholesterol control and smoking cessation. These improvements in care and prognosis over the periods between the first and second cohort enrollment may have blunted the association between smoking marijuana and mortality.
Our results are consistent with recent observations that elevated endocannabinoid plasma levels are associated with coronary circulatory dysfunction in obese subjects3 and type 1 diabetic cardiomyopathy.2 These findings are also consistent with case reports of acute myocardial infarction among three teenagers who used synthetic cannabinoids.4 Several studies examined the association between heavy cannabinoid use and addiction and the rate of survival10–13 and some14–16, but not all, studies in the general population have shown that there is a higher mortality rate associated with cannabinoid use. However, our study provides a unique opportunity to examine this relationship among people who sustained an MI.
Marijuana use has several effects on the cardiovascular system. Marijuana acutely increases blood pressure, probably mediated through sympathetic stimulation and reduced parasympathetic activity.29 This rise in norepinephrine increases myocardial oxygen demand and reduced left ventricular ejection time, thereby lowering the threshold for angina and peripheral vascular resistance in skeletal muscles.30 In addition, the increased carbon monoxide exposure from marijuana smoking results in even higher blood levels of carboxyhemoglobin than does smoking standard cigarettes.31
There are some limitations that warrant discussion. As with any observational study, we cannot rule out the possibility of unmeasured or residual confounding. We do not have information on secondary prevention measures or access to care, which could be important determinants of survival. However, in our fully adjusted model, we included information on median household income. Since most of the patients in the MI Onset Study were on some medications before sustaining an MI, it seems likely that they received secondary prevention measures as well in a manner unrelated to marijuana use. It is possible that some participants emigrated from the United States and therefore, we may have underestimated the number of deaths. However, it seems unlikely that any loss to follow-up would be different for those who smoked marijuana in the year prior to MI. We relied on self-reported marijuana use, so there may be some exposure misclassification. However, because outcomes were assessed prospectively, any misclassification of marijuana use would likely be non-differential with respect to mortality. Furthermore, the misclassification is unlikely to affect the rank ordering of marijuana use among the study participants and thus should not affect the internal validity of our results. Finally, because marijuana use was not common, we did not have sufficient power to attain statistical significance for the estimates in our survival models. However, the findings from the propensity-matched cohort and the statistical adjustment for several potential confounders suggest that there may be a higher mortality rate associated with marijuana use among MI survivors. Despite these limitations, the study has several strengths. This study is based on a multicenter, prospectively assembled cohort with extensive clinical and demographic information. It provides a unique opportunity to study the impact of marijuana use in a population of MI survivors followed for up to 18 years.
In summary, in this multi-center cohort study of MI survivors there was a suggestion of a higher rate of mortality after acute MI in marijuana users. With the growing prevalence of marijuana use in middle aged adults, this risk may have great importance in the future. Larger studies with repeated measures of marijuana use are needed to definitively establish whether there are adverse cardiovascular consequences of smoking marijuana among patients with coronary heart disease. Given the prior evidence of acutely increased risk following each episode of smoking marijuana, it seems prudent to caution patients with coronary heart disease and those at high risk of cardiovascular disease to abstain from smoking marijuana.
Figure.
Kaplan Meier estimates of post-MI survival among 87 marijuana users and 174 propensity-matched non-users.
Acknowledgments
Elizabeth Mostofsky received support from a grant from the National Institutes of Health (T32-HL098048) and Joshua I. Rosenbloom received support from the Harvard Medical School Scholars in Medicine Office.
Role of the Sponsors
The sponsors had no role in the design and conduct of the study, in the collection, analysis, and interpretation of the data, or in the preparation, review, or approval of the manuscript.
Footnotes
Disclosures
None.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Substance Abuse and Mental Health Services Administration. 2010 [Google Scholar]
- 2.Rajesh M, Batkai S, Kechrid M, et al. Cannabinoid 1 receptor promotes cardiac dysfunction, oxidative stress, inflammation, and fibrosis in diabetic cardiomyopathy. Diabetes. 2012;61:716–27. doi: 10.2337/db11-0477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Quercioli A, Pataky Z, Vincenti G, et al. Elevated endocannabinoid plasma levels are associated with coronary circulatory dysfunction in obesity. Eur Heart J. 2011;32:1369–78. doi: 10.1093/eurheartj/ehr029. [DOI] [PubMed] [Google Scholar]
- 4.Mir A, Obafemi A, Young A, et al. Myocardial infarction associated with use of the synthetic cannabinoid K2. Pediatrics. 2011;128:e1622–7. doi: 10.1542/peds.2010-3823. [DOI] [PubMed] [Google Scholar]
- 5.Pacher P, Mechoulam R. Is lipid signaling through cannabinoid 2 receptors part of a protective system? Prog Lipid Res. 2011;50:193–211. doi: 10.1016/j.plipres.2011.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Steffens S, Veillard NR, Arnaud C, et al. Low dose oral cannabinoid therapy reduces progression of atherosclerosis in mice. Nature. 2005;434:782–6. doi: 10.1038/nature03389. [DOI] [PubMed] [Google Scholar]
- 7.Pacher P, Batkai S, Kunos G. The endocannabinoid system as an emerging target of pharmacotherapy. Pharmacol Rev. 2006;58:389–462. doi: 10.1124/pr.58.3.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sidney S. Cardiovascular consequences of marijuana use. J Clin Pharmacol. 2002;42:64S–70S. doi: 10.1002/j.1552-4604.2002.tb06005.x. [DOI] [PubMed] [Google Scholar]
- 9.Mittleman MA, Lewis RA, Maclure M, et al. Triggering myocardial infarction by marijuana. Circulation. 2001;103:2805–9. doi: 10.1161/01.cir.103.23.2805. [DOI] [PubMed] [Google Scholar]
- 10.Arendt M, Munk-Jorgensen P, Sher L, et al. Mortality among individuals with cannabis, cocaine, amphetamine, MDMA, and opioid use disorders: a nationwide follow-up study of Danish substance users in treatment. Drug Alcohol Depend. 2011;114:134–9. doi: 10.1016/j.drugalcdep.2010.09.013. [DOI] [PubMed] [Google Scholar]
- 11.Pavarin RM, Berardi D. Mortality risk in a cohort of subjects reported by authorities for cannabis possession for personal use. Results of a longitudinal study. Epidemiol Prev. 2011;35:89–93. [PubMed] [Google Scholar]
- 12.Callaghan RC, Cunningham JK, Verdichevski M, et al. All-cause mortality among individuals with disorders related to the use of methamphetamine: A comparative cohort study. Drug Alcohol Depend. 2012 doi: 10.1016/j.drugalcdep.2012.03.004. [DOI] [PubMed] [Google Scholar]
- 13.Hser YI, Kagihara J, Huang D, et al. Mortality among substance-using mothers in California: a 10-year prospective study. Addiction. 2012;107:215–22. doi: 10.1111/j.1360-0443.2011.03613.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Calabria B, Degenhardt L, Hall W, et al. Does cannabis use increase the risk of death? Systematic review of epidemiological evidence on adverse effects of cannabis use. Drug Alcohol Rev. 2010;29:318–30. doi: 10.1111/j.1465-3362.2009.00149.x. [DOI] [PubMed] [Google Scholar]
- 15.Davstad I, Allebeck P, Leifman A, et al. Self-reported drug use and mortality among a nationwide sample of Swedish conscripts - a 35-year follow-up. Drug Alcohol Depend. 2011;118:383–90. doi: 10.1016/j.drugalcdep.2011.04.025. [DOI] [PubMed] [Google Scholar]
- 16.Muhuri PK, Gfroerer JC. Mortality associated with illegal drug use among adults in the United States. Am J Drug Alcohol Abuse. 2011;37:155–64. doi: 10.3109/00952990.2011.553977. [DOI] [PubMed] [Google Scholar]
- 17.Andreasson S, Allebeck P. Cannabis and mortality among young men: a longitudinal study of Swedish conscripts. Scand J Soc Med. 1990;18:9–15. doi: 10.1177/140349489001800102. [DOI] [PubMed] [Google Scholar]
- 18.Sidney S, Beck JE, Tekawa IS, et al. Marijuana use and mortality. Am J Public Health. 1997;87:585–90. doi: 10.2105/ajph.87.4.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mukamal KJ, Maclure M, Muller JE, et al. An exploratory prospective study of marijuana use and mortality following acute myocardial infarction. Am Heart J. 2008;155:465–70. doi: 10.1016/j.ahj.2007.10.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mittleman MA, Maclure M, Tofler GH, et al. Triggering of acute myocardial infarction by heavy physical exertion. Protection against triggering by regular exertion. Determinants of Myocardial Infarction Onset Study Investigators. N Engl J Med. 1993;329:1677–83. doi: 10.1056/NEJM199312023292301. [DOI] [PubMed] [Google Scholar]
- 21.Krieger N, Chen JT, Waterman PD, et al. Geocoding and monitoring of US socioeconomic inequalities in mortality and cancer incidence: does the choice of area-based measure and geographic level matter? : the Public Health Disparities Geocoding Project. Am J Epidemiol. 2002;156:471–82. doi: 10.1093/aje/kwf068. [DOI] [PubMed] [Google Scholar]
- 22.Krieger N, Chen JT, Waterman PD, et al. Choosing area based socioeconomic measures to monitor social inequalities in low birth weight and childhood lead poisoning: The Public Health Disparities Geocoding Project (US) J Epidemiol Community Health. 2003;57:186–99. doi: 10.1136/jech.57.3.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stampfer MJ, Willett WC, Speizer FE, et al. Test of the National Death Index. Am J Epidemiol. 1984;119:837–9. doi: 10.1093/oxfordjournals.aje.a113804. [DOI] [PubMed] [Google Scholar]
- 24.Parsons LS. Reducing Bias in a Propensity Score Matched-Pair Sample Using Greedy Matching Techniques. Proceedings of the Twenty-Sixth Annual SAS Users Group International Conference; 2001; Cary (NC): SAS Institute; 2001. [Google Scholar]
- 25.Wellenius GA, Mittleman MA. Disparities in myocardial infarction case fatality rates among the elderly: the 20-year Medicare experience. Am Heart J. 2008;156:483–90. doi: 10.1016/j.ahj.2008.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ford ES, Ajani UA, Croft JB, et al. Explaining the decrease in U.S. deaths from coronary disease, 1980–2000. N Engl J Med. 2007;356:2388–98. doi: 10.1056/NEJMsa053935. [DOI] [PubMed] [Google Scholar]
- 27.Jones RT. Cardiovascular system effects of marijuana. J Clin Pharmacol. 2002;42:58S–63S. doi: 10.1002/j.1552-4604.2002.tb06004.x. [DOI] [PubMed] [Google Scholar]
- 28.Aryana A, Williams MA. Marijuana as a trigger of cardiovascular events: speculation or scientific certainty? Int J Cardiol. 2007;118:141–4. doi: 10.1016/j.ijcard.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 29.Gash A, Karliner JS, Janowsky D, et al. Effects of smoking marihuana on left ventricular performance and plasma norepinephrine: studies in normal men. Ann Intern Med. 1978;89:448–52. doi: 10.7326/0003-4819-89-4-448. [DOI] [PubMed] [Google Scholar]
- 30.Pratap B, Korniyenko A. Toxic Effects of Marijuana on the Cardiovascular System. Cardiovasc Toxicol. 2011 doi: 10.1007/s12012-011-9150-y. [DOI] [PubMed] [Google Scholar]
- 31.Wu TC, Tashkin DP, Djahed B, et al. Pulmonary hazards of smoking marijuana as compared with tobacco. N Engl J Med. 1988;318:347–51. doi: 10.1056/NEJM198802113180603. [DOI] [PubMed] [Google Scholar]