Abstract
Background and Purpose
History of stroke and Transient Ischemic Attack (TIA) are documented risk factors for subsequent stroke and all-cause mortality. Recent reports suggest increased risk among those reporting stroke symptoms absent stroke or TIA. However, the relative magnitude of increased stroke risk has not been described across the symptomatic spectrum: 1) asymptomatic (Asx), 2) stroke symptoms only (SS), 3) TIA, 4) stroke in the distant past (DS), and 5) recent stroke (RS).
Methods
Between 2003–2007 the REasons for Geographic And Racial Differences in Stroke (REGARDS) study enrolled 30,239 black and white Americans aged 45+. DS and RS were defined as self-report of physician diagnosis of stroke >5 or <5 years before baseline, respectively. SS was defined as a history of any of six sudden onset stroke symptoms absent TIA/stroke diagnosis. Kaplan-Meier and proportional hazards analysis were used to contrast stroke risk differences.
Results
Over 5.0 ± 1.72 years of follow up, 737 strokes were validated. Compared to Asx persons, those with SS, TIA, DS and RS all had increased risk of future stroke. After adjustment for age, race, sex, income, education, alcohol intake, current smoking, and a history of diabetes, hypertension, myocardial infarction, atrial fibrillation, and dyslipidemia, there was 1.20-fold (not statistically significant) increased stroke risk for SS (95% CI 0.96, 1.51), 1.73-fold for TIA (95% CI 1.27, 2.36), 2.23-fold for DS (95% CI 1.61, 3.09) and 2.85-fold for RS (95% CI 2.16, 3.76).
Discussion
Results suggest a spectrum of risk from stroke symptoms to TIA, distant stroke, and recent stroke, and imply a need for establishing these categories in health screenings to manage risk for future stroke, reinforcing the clinical importance of stroke history including the presence of stroke symptoms.
Keywords: stroke, TIA, stroke symptoms, mortality
Introduction
Previous studies demonstrated that having a prior history of stroke or transient ischemic attack (TIA) confers a substantial risk for subsequent stroke. Pooled analyses from the Framingham Heart Study, the Atherosclerosis Risk in Communities Study, and the Cardiovascular Health Study demonstrated that between 13 and 32% of individuals experiencing a stroke will have a recurrent stroke within 5 years1. Additional population based studies demonstrated that the risk of stroke immediately following a Transient Ischemic Attack (TIA) is between 3 and 17.3%2–4. However, many people who experience TIA or stroke either were either never diagnosed with it or were not aware of a diagnosis they received5. Consequently, in studies utilizing self-report of stroke/TIA diagnoses, misclassification in the outcome occurs (fewer outcomes will be observed than are actually occurring) and might lead to underestimation of associations. Queries to research subjects on self-report of stroke-like symptoms might help to improve classification of prior stroke and identify persons at increased risk of subsequent stroke5–7.
The clinical importance of evaluating stroke symptoms in the absence of a stroke or TIA diagnosis is underscored by several recent observations in the REGARDS cohort. First, the prevalence of stroke like symptoms is over 18% in the general population aged 45+,5 substantially higher than the 2.9% prevalence of stroke in the population aged 20+.1 Second, presence of these stroke symptoms are associated with higher Framingham Stroke Risk Score5, increased odds of cognitive impairment8, and lower quality of life9. Finally, in the REGARDS cohort there was a 36% increased risk of future stroke following report of any stroke symptom (sudden onset of weakness, numbness, blindness, difficulty in communicating or difficulty in understanding); a 46% increased risk for people reporting two symptoms, and a 77% increased risk for those reporting three7. Although the risk of stroke following self-reported symptoms is now well characterized6, 7, no study has been large enough to contrast the magnitude of increased risk of subsequent stroke or death in those with stroke symptoms, history of diagnosed stroke, or history of diagnosed TIA6, 10.
We sought to characterize the history of cerebrovascular events (CVA) across a spectrum utilizing self-report of diagnosed stroke/TIA and stroke symptoms as exposure variables. Understanding the association of self-report of cerebrovascular events/symptoms and risk of future stroke is clinically important to expand upon the validity of self-reported history of CVA. The Reasons for Geographic and Racial Differences in Stroke (REGARDS) cohort, a large, biracial and nationally representative cohort of 30,239 subjects, provides a unique opportunity to study risk of stroke following a number of types of cerebrovascular events (including stroke and TIA) and/or cerebrovascular event symptoms.
Methods
The REGARDS cohort was assembled between 2003 and 2007 and includes 30,239 black and white adults age 45 and over residing in the 48 continental United States. The study was designed to oversample in the Stroke Belt, a section of the Southeastern United States characterized by high stroke mortality (North Carolina, South Carolina, Georgia, Alabama, Mississippi, Tennessee, Arkansas and Louisiana). Target recruitment was to have half of the cohort residing in the Southeast, half male, and half African American.
The study methods have been described elsewhere11. Briefly, participants were recruited from commercially available lists (Genesys, Inc) similar to the methods used by the National Center for Health Statistics Behavioral Risk Factor Surveillance Study (BRFSS). After a letter was sent to the participant’s home describing the study and informing the individual that he/she would be receiving a phone call, the call center contacted the participant and invited him/her to be a part of the study. Participants provided verbal consent and completed a 45 minute phone interview to collect demographic, socio-economic, risk factors, and history of disease information. The telephone response rate was 33% and cooperation rate was 49%, similar to other cohort studies12. Following the phone call, a trained health professional went to the participant’s home to collect blood and urine samples, samples, blood pressure measurements, an electrocardiogram (ECG), and other key study variables. Blood was stored and analyzed at the central lab at the University of Vermont and ECGs were centrally read at a Wake Forest University. The study was approved by Institutional Review Boards at all participating institutions.
Self-reported history of stroke, TIA, and stroke symptoms were classified across a four-level spectrum: recent stroke (RS), distant stroke (DS), TIA and stroke symptoms (SS). If the participant answered yes to “Were you ever told by a physician that you had a stroke?” we then asked “How old were you when you had your first stroke?” If the participant could not remember the exact age at which he/she had the stroke we asked them to estimate the decade in which the stroke occurred. We used this information to characterize DS as a stroke that occurred more than five years from baseline and a RS as one that occurred within five years of baseline. Time to previous stroke was calculated as the time from reported stroke date to baseline interview. In cases where participants gave a range of years when the stroke may have happened, we used the midpoint of the interval as the date at which first stroke occurred. In the case when a participant reported more than one stroke before baseline, we calculated time from most recent stroke. For those not reporting a history of stroke, self-report of TIA was characterized using the question “Were you ever told by a physician that you had a mini-stroke or TIA, also known as a transient ischemic attack?” The time since diagnosis of TIA was not asked. For those not reporting a history of stroke or TIA, we then used the six questions from the Questionnaire for Verifying Stroke-Free Status (QVSFS)13. They include “Have you ever had sudden painless weakness on one side of your body?”, “Have you ever had sudden numbness or a dead feeling on one side of your body?”, “Have you ever had sudden painless loss of vision in one or both eyes?”, ” Have you ever suddenly lost one half of your vision?”, “Have you ever suddenly lost the ability to understand what people were saying?”, and “Have you ever suddenly lost the ability to express yourself verbally or in writing?”. We considered a yes to any of the six questions as a positive response to history of stroke symptoms.
Age, race, sex, region of residence, education, income, alcohol intake, and current smoking were all collected during the baseline telephone interview via self-report. History of diabetes, hypertension, coronary artery disease, atrial fibrillation, and dyslipidemia were collected from self-report and use of medical information from the in home visit. Hypertension was defined as self-reported use of medications to lower blood pressure, or blood pressure at or above 140/90 mmHg. Diabetes was defined as a fasting glucose level ≥126 mg/dL (or non-fasting glucose ≥ 200 mg/dL if the participant was not fasting) or self-reported medication use for glucose control. Dyslipidemia was defined as a triglycerides >=240 mg/dL or LDL>=160 mg/dL or HDL<=40 mg/dL. Atrial fibrillation were defined as either self-report or ECG evidence14. History of heart disease was defined as self-reported prebaseline myocardial infarction/heart attack, coronary artery bypass surgery, coronary angioplasty/stenting, or evidence of myocardial infarction from ECG.
Stroke Event Ascertainment
Questions related to all hospitalizations were asked of participants or their proxies by interview at 6-month intervals, and medical records were pursued for all hospitalizations suspected to be related to stroke, TIA, or stroke symptoms. Medical records for strokes that occurred before baseline were not pursued. Upon receipt of medical records, they were first reviewed by a trained neurological nurse to verify the record is complete and to remove clear non-stroke cases; then suspected strokes are forwarded on to review by a team of stroke experts. A stroke is defined as focal neurologic symptoms lasting greater than twenty-four hours or non-focal symptoms with imaging positive for stroke. For deaths in which medical records are not available (participant died at home or did not make it to the hospital), a proxy was interviewed to probe for information relating to the stroke. Stroke adjudicators then utilized the death certificate, National Death Index and proxy interview to determine if a stroke occurred. For this analysis, stroke events were available through February 1, 2011.
Death Ascertainment
In addition to stroke outcomes, the risk of all-cause mortality was assessed across the symptomatic spectrum. Notification of death was provided by proxies either through the mail, during the routine six month telephone calls, or by telephone calls to a toll free number for REGARDS participants. Searches using the Social Security Death Index (SSDI) death master file and the National Death Index (NDI) were used to look for participants who may have died for whom there was no proxy report of death and was also used to confirm the date of death given by proxies. For this analysis death events were available through April 1, 2011.
Statistical Methods
Cox Proportional Hazards modeling was used to examine the association between the main exposure (the spectrum of cerebrovascular event history modeled as a 5-level categorical dummy variable) and both the stroke and death outcomes. We also used non-parametric Kaplan-Meier plots to visually display the data. Incremental models were fit to assess the influence of groups of covariates: 1) demographics, 2) then adding socioeconomic status (defined by highest education obtained and household income), and 3) adding stroke risk factors. As there was some racial difference in terms of medical records obtained, we applied a mathematical correction for the final model to ensure that this bias did not alter our results15. We included the following covariates in all final models: age, race, sex, region of residence, education, income, alcohol intake, current smoking, and a history of diabetes, hypertension, myocardial infarction, atrial fibrillation, and dyslipidemia.
Results
Participants were included if they had at least one follow-up phone call after the baseline interview (n=29846) and participants were excluded if they did not answer the stroke, TIA, or stroke symptom questions (n=431), resulting in a final sample of 29415 (95% of the study sample).
Compared to the Asx group, participants with a self-report of prior stroke diagnosis were more likely to be male, black, and not have graduated college (Table 1). These trends were similar across exposure groups such that those with self-report of prior stroke were more likely to be male, black and not have graduated college than those who reported a TIA or stroke symptom. In addition those with recent strokes were more likely to have other concomitant disease like heart disease, diabetes and atrial fibrillation. They were also less likely to consume alcohol and to be a current smoker. Across the categories of self-reported stroke, TIA or SS, the prevalence of hypertension declined but in all cases was higher than those without any of the components of the symptomatic spectrum. 82% of those with a recent stroke had hypertension, compared to 77% of those with a distant stroke, 75% of those reporting a TIA, 65% of those reporting SS and 56% of those without any history of stroke, TIA or SS.
Table 1.
Demographic, socio-economic and health characteristics in those people self-reporting a history of stroke, TIA or stroke symptom in the REasons for Geographic and Racial Differences in Stroke (REGARDS) study.
| No reported history of stroke, TIA, or stroke symptoms N=22795 |
Stroke symptom N=3871 |
TIA N=1096 |
Distant stroke N=807 |
Recent stroke N=846 |
pa | |
|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | ||
| Males | 10194 (44.8) | 1697 (44.0) | 454 (41.5) | 373 (46.5) | 437 (52.0) | <0.001 |
| Blacks | 8786 (38.6) | 1957 (50.8) | 429 (39.3) | 439 (54.7) | 414 (49.4) | <0.001 |
| Residence outside of stroke belt | 10098 (44.4) | 1663 (43.2) | 511 (46.8) | 377 (47.0) | 370 (44.0) | 0.17 |
| College graduate | 8539 (37.5) | 1013 (26.3) | 341 (31.2) | 179 (22.5) | 198 (23. 7) | <0.001 |
| Income less than $20k | 3506 (15.4) | 1001 (26.0) | 235 (21.5) | 257 (32.0) | 247 (29.4) | <0.001 |
| Current Smoker | 3045(13.4) | 675 (17.6) | 173 (15.9) | 153 (19.1) | 161 (19.2) | <0.001 |
| Alcohol intake | <0.001 | |||||
| Heavy | 956(4.3) | 133 (3.6) | 34 (3.2) | 26 (3.3) | 20 (2.4) | |
| Moderate | 7900 (35.3) | 1024 (27.4) | 300 (28.0) | 203 (26.0 | 194 (23.4) | |
| None | 13506 (59.3) | 2578 (69.0) | 738 (68.8) | 553 (70.7) | 617 (74.3) | |
| Concomitant disease history | ||||||
| Heart disease | 2366 (10.6) | 602 (15.9) | 242 (22.9) | 191 (24.5) | 229 (27.8) | <0.001 |
| Diabetes | 4214 (19.2) | 1063 (28.7) | 316 (29.9) | 263 (34.7) | 330 (40.7) | <0.001 |
| Hypertension | 12667 (55.8) | 2487 (64.8) | 819 (75.1) | 624 (77.7) | 687 (82.0) | <0.001 |
| Atrial Fibrillation | 1593 (7.1) | 481 (12.9) | 184 (17.4) | 115 (14.9) | 126 (15.6) | <0.001 |
| Dyslipidemia | 12618 (57.5) | 2306 (62.5) | 720 (67.2) | 525 (68.7) | 578 (71.9) | <0.001 |
A recent stroke is defined as a stroke within 5 years of the baseline interview. A distant stroke is defined as a stroke that occurred 5 years or further from baseline interview. Recent stroke, distant stroke, TIA and stroke symptoms were all ascertained by self-report.
p values are for chi-squared test
Compared with those not reporting stroke or SS, self-report of a recent stroke (within the past five years) was most strongly associated with future stroke, HR = 3.72; 95% CI=2.89-4.78 (Table 2) after adjusting for age, race and sex. Adding region of residence, education, income, alcohol intake, current smoking, and a history of diabetes, hypertension, heart disease, atrial fibrillation, and dyslipidemia to the model attenuated the association only modestly (HR=2.85; 95% CI=2.16-3.76). Figure 1 demonstrates a progressive relationship between no stroke, SS, TIA, distant stroke and recent stroke in a Kaplan Meier plot. Even after adjusting for the risk factors mentioned above, the strong graded association between no stroke and SS, TIA, DS and recent stroke persisted. The fully adjusted hazard ratios increased from 1.20 (p>0.05) in those reporting SS, to 1.73 (p<0.01) in those reporting TIA, to 2.23 (p<0.01) in those reporting a DS, and finally to 2.85 (p<0.01) in those reporting an RS. All hazard ratios are relative to those not reporting SS, TIA or stroke.
Table 2.
Risk of future stroke following self-reported stroke, TIA or stroke symptoms in the REasons for Geographic and Racial Differences in Stroke (REGARDS) study.
| N | No report of stroke symptom, TIA or stroke 22795 |
Stroke symptom 3871 |
TIA 1096 |
Distant stroke1 807 |
Recent stroke1 846 |
p (trend) |
|---|---|---|---|---|---|---|
| Number of adjudicated strokes |
456 | 104 | 56 | 50 | 71 | |
| Adjusts for age, race, and sex |
ref | 1.32 (1.07, 1.64) |
2.15 (1.62, 2.84) |
2.74 (2.05, 3.68) |
3.72 (2.89, 4.78) |
<0.001 |
| Adjusts for above plus region, income and education |
ref | 1.26 (1.02, 1.57) |
2.11 (1.59, 2.79) |
2.61 (1.95, 3.51) |
3.49 (2.71, 4.50) |
<0.001 |
| Adjusts for above plus comorbidites‡ |
ref | 1.20 (0.96, 1.51) |
1.73 (1.27, 2.36) |
2.23 (1.61, 3.09) |
2.85 (2.16, 3.76) |
<0.001 |
A recent stroke is defined as a stroke within 5 years of the baseline interview. A distant stroke is defined as a stroke that occurred 5 years or further from baseline interview. Recent stroke, distant stroke, TIA and stroke symptoms were all ascertained by self-report.
Comorbidities include alcohol intake, current smoking, and a history of diabetes, hypertension, history of coronary artery disease, atrial fibrillation, dyslipidemia, and the racial difference in retrieving medical records
Figure 1.
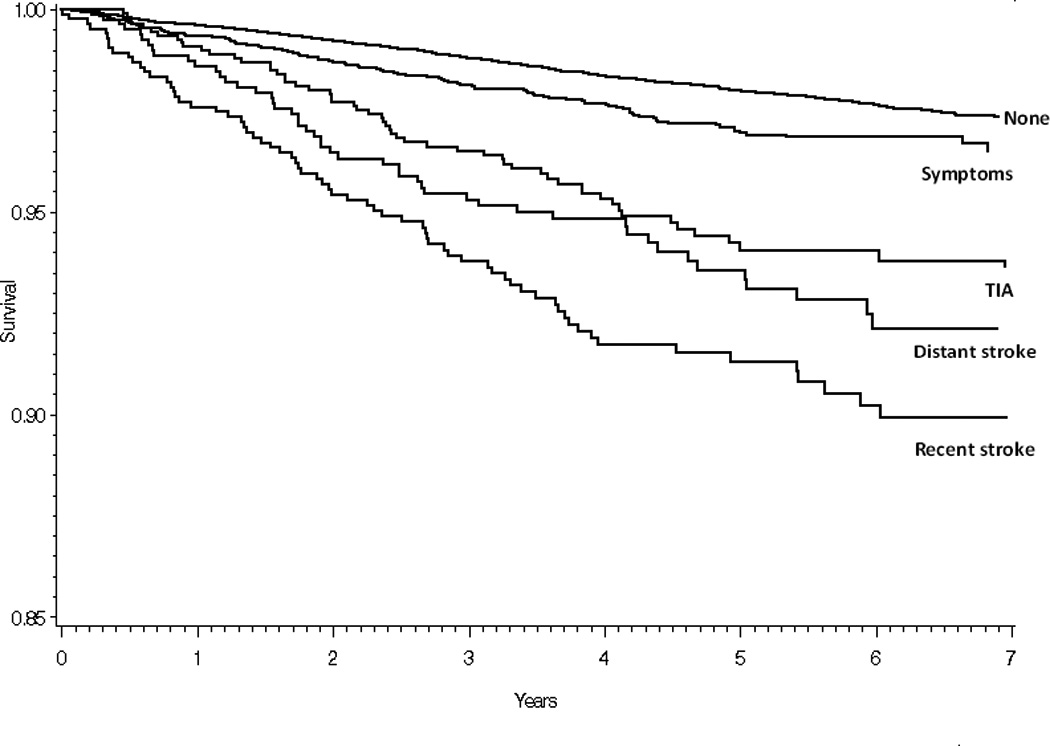
Risk of future stroke (Kaplan-Meier) following self-report stroke, TIA or stroke symptoms in the REasons for Geographic and Racial Differences in Stroke (REGARDS) study. Self-report was obtained at baseline between 2003 and 2007. Participants have been followed for stroke events which are confirmed by a physician (baseline strokes were not physician verified) for a mean of 5.0 ± 1.72 years. A older stroke is defined as a stroke that occurred 5 years or further from baseline interview. Recent stroke, distant stroke, TIA and stroke symptoms were all ascertained by self-report.
Over a median of 4.5 years, we observed a similar strong association across the stroke spectrum with risk of all-cause mortality (Table 3). In participants reporting a stroke within five years of baseline the risk of death was over two-fold greater than in those without a stroke, TIA or SS at baseline (HR=2.47; 95% CI=2.14-2.85). This was only modestly attenuated in the fully adjusted model (HR=1.79; 95% CI=1.53, 2.09). A dose response association was present across the symptomatic spectrum (p<0.001). Hazard ratios of death for the other three stroke spectrum categories were: DS (HR=1.86; 95% CI=1.58, 2.20), TIA (HR=1.58; 95% CI=1.35, 1.85), and for SS (HR=1.33; 95% CI=1.19, 1.48). Contrary to the stroke findings the differences between the RS group and the DS group were more modest. Although a linear trend was still present, the HRs for RS and DS were similar across all models.
Table 3.
Risk of death following self-reported stroke, TIA or stroke symptoms in the REasons for Geographic and Racial Differences in Stroke (REGARDS) study.
| N | No report of stroke symptom, TIA or stroke 22795 |
Stroke symptom 3871 |
TIA 1096 |
Distant stroke1 807 |
Recent stroke1 846 |
p (trend) |
|---|---|---|---|---|---|---|
| Number of deaths | 1844 | 529 | 213 | 196 | 211 | |
| Adjusts for age, race, and sex |
ref | 1.63 (1.47, 1.79) |
2.01 (1.74, 02.32) |
2.51 (2.16, 2.91) |
2.47 (2.14, 2.85) |
<0.001 |
| Adjusts for above plus income and education |
ref | 1.45 (1.33, 1.60) |
1.88 (1.63, 2.18) |
2.07 (1.78, 2.42) |
2.07 (1.78, 2.39) |
<0.001 |
| Adjusts for above plus comorbidites‡ |
ref | 1.33 (1.19, 1.48) |
1.58 (1.35, 1.85) |
1.86 (1.58, 2.20) |
1.79 (1.53, 2.09) |
<0.001 |
A recent stroke is defined as a stroke within 5 years of the baseline interview. A distant stroke is defined as a stroke that occurred 5 years or further from baseline interview. Recent stroke, distant stroke, TIA and stroke symptoms were all ascertained by self-report.
Comorbidities include alcohol intake, current smoking, and a history of diabetes, hypertension, myocardial infarction, atrial fibrillation, and dyslipidemia
Discussion
In the REGARDS cohort, a large population based sample of US adults, relative to other types of cerebrovascular events, people who self-reported a recent stroke have the largest risk for having a stroke in the future. In fact, this risk was nearly twice as high as the hazard ratios of stroke for atrial fibrillation and hypertension in REGARDS16. A strong dose response, as indicated by a p for trend less than 0.001, was observed across our four categories of SS, TIA, DS and RS for both the stroke and mortality outcome. This suggests that the eight questions asked of REGARDS participants (history of stroke, history of TIA, and six questions from the validated questionnaire for verifying stroke-free status QVSFS) could help primary care doctors identify people at a high risk of stroke and death for targeted risk factor management13, 17, 18.
Previous studies have not found self-report of stroke to be highly correlated with actual stroke when stroke neurologists have examined medical records and imaging results of those self-reporting stroke. In one study, the sensitivity for a self-report of stroke predicting actual stroke was 32.4% and specificity was 78.9%19. Interestingly, this study also found evidence for racial differences in the predictive value of self-report of stroke (in whites: sensitivity = 26.5% and specificity 83.5% and in blacks: sensitivity = 37.3% and specificity 77.4%). This confirmed previous studies also showing high false negative rates (low sensitivity) for diagnosis of stroke when relying solely on self-report of stroke20. Although our study does not refute the findings of the previous work, it does provide some perspective about the potential health risks associated with perceived stroke. Even though it is possible that as few as 26% of the strokes we identified through self-report were real strokes, these reported strokes were associated with a high rate of future stroke. From a public health perspective, while these events were not adjudicated as stroke, they may still provide a population that is at high risk for future stroke and may thereby benefit from interventional studies21, 22. It is also possible that REGARDS participants had better knowledge of prior stroke given their willingness to participate in the study.
The strong associations of history of TIA and SS with future stroke risk and death are also worth noting. It is possible these TIAs and SS were undiagnosed stroke events, consistent with other findings that “silent infarcts” are associated with increased risk of stroke23, 24. It is not currently known whether these SS and TIAs represent actual strokes but future studies including brain imaging to document this would be helpful. In the meantime, that these symptoms are associated with up to a 20% greater risk of stroke and a 34% increased risk of death in people who have not reported having had a stroke or TIA intriguing.
There are some limitations of the current study. As discussed above, misclassification of prebaseline stroke and/or TIA are likely, however, associations of these self-reports with future stroke were strong nonetheless. Although the exposure may be misclassified, the incident stroke outcome was adjudicated by stroke experts providing a robust outcome measure. Second, ascertainment of stroke events in blacks was not as complete as in the whites due to the racial difference in medical record retrieval. We were however able to account for this using imputation25.
In conclusion, we report a graded association of the spectrum of baseline stroke, from SS to TIA, to distant stroke and recent stroke, with the risk of future stroke. Further, these same conditions were associated with substantial mortality risk. Findings have potentially important public health importance if other studies can demonstrate that special interventions in these patient groups are beneficial at reducing stroke.
Acknowledgements
We would like to first acknowledge the participants in the REGARDS study for their time in helping study racial and regional differences in stroke. We would like to acknowledge the coordinating center and survey research unit at the University of Alabama Birmingham for all of their excellent work in putting together this rich dataset. Dr Judd acknowledges funding from the NIH loan repayment program.
Sources of Funding: This research project is supported by a cooperative agreement U01 NS041588 from the National Institute of Neurological Disorders and Stroke, National Institutes of Health, Department of Health and Human Services and also an ARRA supplement. The content is solely the responsibility of the authors and does not necessarily represent the official views and positions of the National Institute of Neurological Disorders and Stroke or the National Institutes of Health. Representatives of the funding agency were involved in the review of the manuscript prior to submission for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures: None of the co-authors on the manuscript have anything to disclose that would provide a conflict of interest when interpreting the results of this study.
References
- 1.Lloyd-Jones D, Adams R, Carnethon M, De Simone G, Ferguson TB, Flegal K, et al. Heart disease and stroke statistics--2009 update: A report from the american heart association statistics committee and stroke statistics subcommittee. Circulation. 2009;119:480–486. doi: 10.1161/CIRCULATIONAHA.108.191259. [DOI] [PubMed] [Google Scholar]
- 2.Johnston SC, Fayad PB, Gorelick PB, Hanley DF, Shwayder P, van Husen D, et al. Prevalence and knowledge of transient ischemic attack among us adults. Neurology. 2003;60:1429–1434. doi: 10.1212/01.wnl.0000063309.41867.0f. [DOI] [PubMed] [Google Scholar]
- 3.Kleindorfer D, Panagos P, Pancioli A, Khoury J, Kissela B, Woo D, et al. Incidence and short-term prognosis of transient ischemic attack in a population-based study. Stroke. 2005;36:720–723. doi: 10.1161/01.STR.0000158917.59233.b7. [DOI] [PubMed] [Google Scholar]
- 4.Lisabeth LD, Ireland JK, Risser JM, Brown DL, Smith MA, Garcia NM, et al. Stroke risk after transient ischemic attack in a population-based setting. Stroke. 2004;35:1842–1846. doi: 10.1161/01.STR.0000134416.89389.9d. [DOI] [PubMed] [Google Scholar]
- 5.Howard VJ, McClure LA, Meschia JF, Pulley L, Orr SC, Friday GH. High prevalence of stroke symptoms among persons without a diagnosis of stroke or transient ischemic attack in a general population: The reasons for geographic and racial differences in stroke (regards) study. Arch Intern Med. 2006;166:1952–1958. doi: 10.1001/archinte.166.18.1952. [DOI] [PubMed] [Google Scholar]
- 6.Chambless LE, Toole JF, Nieto FJ, Rosamond W, Paton C. Association between symptoms reported in a population questionnaire and future ischemic stroke: The aric study. Neuroepidemiology. 2004;23:33–37. doi: 10.1159/000073972. [DOI] [PubMed] [Google Scholar]
- 7.Kleindorfer D, Judd S, Howard VJ, McClure L, Safford MM, Cushman M, et al. Self-reported stroke symptoms without a prior diagnosis of stroke or transient ischemic attack: A powerful new risk factor for stroke. Stroke. 2011;42:3122–3126. doi: 10.1161/STROKEAHA.110.612937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wadley VG, McClure LA, Howard VJ, Unverzagt FW, Go RC, Moy CS, et al. Cognitive status, stroke symptom reports, and modifiable risk factors among individuals with no diagnosis of stroke or transient ischemic attack in the reasons for geographic and racial differences in stroke (regards) study. Stroke. 2007;38:1143–1147. doi: 10.1161/01.STR.0000259676.75552.38. [DOI] [PubMed] [Google Scholar]
- 9.Haley WE, Roth DL, Kissela B, Perkins M, Howard G. Quality of life after stroke: A prospective longitudinal study. Qual Life Res. 2011;20:799–806. doi: 10.1007/s11136-010-9810-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hart CL, Hole DJ, Smith GD. The relation between questions indicating transient ischaemic attack and stroke in 20 years of follow up in men and women in the renfrew/paisley study. J Epidemiol Community Health. 2001;55:653–656. doi: 10.1136/jech.55.9.653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Howard VJ, Cushman M, Pulley L, Gomez CR, Go RC, Prineas RJ, et al. The reasons for geographic and racial differences in stroke study: Objectives and design. Neuroepidemiology. 2005;25:135–143. doi: 10.1159/000086678. [DOI] [PubMed] [Google Scholar]
- 12.Morton LM, Cahill J, Hartge P. Reporting participation in epidemiologic studies: A survey of practice. American Journal of Epidemiology. 2006;163:197–203. doi: 10.1093/aje/kwj036. [DOI] [PubMed] [Google Scholar]
- 13.Jones WJ, Williams LS, Meschia JF. Validating the questionnaire for verifying stroke-free status (qvsfs) by neurological history and examination. Stroke. 2001;32:2232–2236. doi: 10.1161/hs1001.096191. [DOI] [PubMed] [Google Scholar]
- 14.Soliman EZ, Howard G, Meschia JF, Cushman M, Muntner P, Pullicino PM, et al. Self-reported atrial fibrillation and risk of stroke in the reasons for geographic and racial differences in stroke (regards) study. Stroke. 2011;42:2950–2953. doi: 10.1161/STROKEAHA.111.621367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Howard GT, Norton WN, Stroot PG, Bailey KL, Watson EJ. Association of the genus acinetobacter with the decomposition of a swine carcass and the isolation and characterization of a novel strain of acinetobacter sp. P4. Curr Microbiol. 2011 doi: 10.1007/s00284-011-0030-2. [DOI] [PubMed] [Google Scholar]
- 16.Howard G, Cushman M, Kissela BM, Kleindorfer DO, McClure LA, Safford MM, et al. Traditional risk factors as the underlying cause of racial disparities in stroke: Lessons from the half-full (empty?) glass. Stroke. 2011 doi: 10.1161/STROKEAHA.111.625277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Meschia JF, Brott TG, Chukwudelunzu FE, Hardy J, Brown RD, Jr., et al. Verifying the stroke-free phenotype by structured telephone interview. Stroke. 2000;31:1076–1080. doi: 10.1161/01.str.31.5.1076. [DOI] [PubMed] [Google Scholar]
- 18.Meschia JF, Lojacono MA, Miller MJ, Brott TG, Atkinson EJ, O'Brien PC. Reliability of the questionnaire for verifying stroke-free status. Cerebrovascular diseases. 2004;17:218–223. doi: 10.1159/000075794. [DOI] [PubMed] [Google Scholar]
- 19.Reitz C, Schupf N, Luchsinger JA, Brickman AM, Manly JJ, Andrews H, et al. Validity of selfreported stroke in elderly african americans, caribbean hispanics, and whites. Arch Neurol. 2009;66:834–840. doi: 10.1001/archneurol.2009.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sorensen SP, Boysen G, Jensen G, Schnohr P. Prevalence of stroke in a district of copenhagen the copenhagen city heart study. Acta Neurol Scand. 1982;66:68–81. doi: 10.1111/j.1600-0404.1982.tb03130.x. [DOI] [PubMed] [Google Scholar]
- 21.Rothwell PM, Johnston SC. Transient ischemic attacks: Stratifying risk. Stroke. 2006;37:320–322. doi: 10.1161/01.STR.0000200555.89117.d2. [DOI] [PubMed] [Google Scholar]
- 22.Rothwell PM, Giles MF, Chandratheva A, Marquardt L, Geraghty O, Redgrave JN, et al. Effect of urgent treatment of transient ischaemic attack and minor stroke on early recurrent stroke (express study): A prospective population-based sequential comparison. Lancet. 2007;370:1432–1442. doi: 10.1016/S0140-6736(07)61448-2. [DOI] [PubMed] [Google Scholar]
- 23.Bernick C, Kuller L, Dulberg C, Longstreth WT, Jr, Manolio T, Beauchamp N, Price T. Silent mri infarcts and the risk of future stroke: The cardiovascular health study. Neurology. 2001;57:1222–1229. doi: 10.1212/wnl.57.7.1222. [DOI] [PubMed] [Google Scholar]
- 24.Sylaja PN, Coutts SB, Subramaniam S, Hill MD, Eliasziw M, Demchuk AM. Acute ischemic lesions of varying ages predict risk of ischemic events in stroke/tia patients. Neurology. 2007;68:415–419. doi: 10.1212/01.wnl.0000252938.76188.52. [DOI] [PubMed] [Google Scholar]
- 25.Howard G, McClure LA, Moy CS, Safford MM, Cushman M, Judd SE, et al. Imputation of incident events in longitudinal cohort studies. Am J Epidemiol. 2011;174:718–726. doi: 10.1093/aje/kwr155. [DOI] [PMC free article] [PubMed] [Google Scholar]


