Abstract
Alveolar bone loss can be caused by periodontitis or periodontal trauma. We have evaluated the effects of transplanted undifferentiated human mesenchymal stem cells (hMSCs) on alveolar bone reaction and periodontal ligament healing in an experimental periodontal wound model. The hMSCs seeded onto a self-assembling peptide hydrogel in combination with collagen sponge were implanted into the right mandible of 12 rats and followed for 1 (n=6) or 4 weeks (n=6) postoperatively. The other 12 sham-treated rats were used as controls. Histological and histomorphometrical methods were used to assess the periodontal tissue reaction. The alveolar bone volume density was significantly higher at 1 week after surgery, and the osteoclast number was significantly lower at both 1 week and 4 weeks postoperatively in the mandibles treated with hMSCs. The implanted cells were detected only at 1 week after surgery. In conclusion, transplanted hMSCs can contribute to alveolar bone preservation after a periodontal surgical trauma at least by decreasing local osteoclast number.
Key words: bone repair, inflammation, osteoclast, PuraMatrix
Introduction
It is well known that alveolar bone has a very rapid turnover and is lost in the absence of a tooth.1 Moreover, the alveolar bone resorption is one of the risks of periodontal surgery and is frequent in periodontitis.2
The common therapies for reconstruction of the alveolar bone such as guided tissue repair by using cell-occlusive barrier membranes, root surface conditioning, bone substitutes, and autologous bone grafts have had a limited effect. These techniques are clinically unpredictable, and do not provide the cells and microenvironment that are capable of initiating and promoting new periodontal tissue formation, resulting in only partial repair at best.3,4
Interestingly, it has been shown that maximum bone repair and almost complete anatomical restoration with no permanent loss of the operated alveolar bone is achieved if the preoperative bone is the thick cancellous type with many marrow spaces which contain mesenchymal stem cells (MSCs).5 Bone marrow-derived MSCs, also named bone marrow stromal cells, are multipotent and have the ability to differentiate into osteoblasts, chondrocytes, adipocytes, and smooth muscle cells.6 Moreover, the therapeutic potential of the MSCs is often related to their ability to modulate the immune response, as indicated by numerous in vitro studies.7,8
A delivery vehicle may be an important regulator of the MSC performance in vivo where hypoxia and host immune response threaten the viability of the implanted cells, and might dictate the success of the cell therapy.9 A self-assembling peptide hydrogel (PuraMatrix) in combination with a collagen sponge was used in our study to deliver bone marrow-derived human MSCs (hMSCs) to the site of periodontal wound in rats. It has been reported that self-assembling peptide hydrogels could provide a three-dimensional (3D) microenvironment with specific properties that could promote in vitro proliferation of chondrocytes, hepatocytes, endothelial cells, osteoblasts, neuronal cells, and stem cells.10 We have hypothesized that undifferentiated MSCs delivered onto peptide hydrogel may preserve host alveolar bone and enhance periodontal healing after surgical trauma by modulating the local inflammatory reaction. To our knowledge, there have been no published studies reporting the alveolar bone reaction toward constructs composed of MSCs, peptide hydrogel, and collagen sponge.
Materials and Methods
The absorbable collagen sponge HELISTAT (Integra Life Sciences Corp.) was derived from bovine deep flexor tendon. The peptide hydrogel PuraMatrix (PM) (3DM, Inc.) consists of 1% aqueous solution of purified synthetic resorbable peptide (pH=3). Under physiological conditions, the peptide component self-assembles into a 3D hydrogel that exhibits a nanometer scale fibrous structure with an average pore size of 50–200 nm.
Cryopreserved hMSCs derived from bone marrow of an 18 year-old male donor were provided by Cambrex Bio Science (Osiris Therapeutics, Inc.). The hMSCs were proved to be able to differentiate into adipocytes (oil red O assay), chondrocytes (proteoglycans-safranin stain, collagen type II assay), and osteoblasts (calcium deposition assay) by the supplier.
Implant preparation
The hMSCs at passage 4 or 5 were used in our experiments. The cells were cultured in Dulbecco's modified Eagle medium containing 1000 mg/L D-glucose, sodium pyruvate, supplemented with 10% heat-inactivated fetal bovine serum, and penicillin (50 units/mL)–streptomycin (50 μg/mL) (all from Gibco Invitrogen) at 37°C in a humidified atmosphere of 5% CO2. After detachment, the viable cells were counted and re-suspended in 20% sucrose solution. The hMSC-loaded construct was prepared by mixing a 100 μL sucrose solution containing 1.5 million hMSCs with 100 μL peptide hydrogel. The number of cells per implant was selected according to the data published by Mankani et al.11 The resultant mixture was applied with a pipette onto a 2 mm×2 mm×3.5 mm piece of collagen sponge placed into an Eppendorf plastic tube; 400 μL cell media were subsequently added to the tube. The cell media were changed thrice in the next 25 min in order to quickly adjust the low pH of the peptide hydrogel. Afterward, the constructs were incubated at 37°C for 2 h on a slowly shaking platform and then left overnight in the incubator at 37°C in an atmosphere of 5% CO2.
Before implantation, the constructs were washed twice with phosphate buffer solution to remove the culture media. The tubes with the constructs were kept on ice before the surgery. After the construct implantation, the residual hMSCs left in the tubes were counted. The procedure was similar for the preparation of the control constructs (without hMSCs), except that only the culture media without cells were added to the peptide hydrogel.
Two separate constructs seeded with the hMSCs were used to assess morphology and cell viability before implantation. One of the constructs was fixed in 4% solution paraformaldehyde overnight at 4°C and then dehydrated and embedded in paraffin; 5-μm serial sections were prepared and placed on glass slides (SuperFrost Plus; Menzel-Gläser). The sections were stained with hematoxylin-eosin (HE) for assessment of general morphology or used for fluorescent in situ hybridization (FISH) analysis. The other construct was used for MTT assay (MTT cell proliferation kit; Roche) in order to check the cell viability.
Periodontal defect model
The experiment was approved by the Research Ethics Committee of Karolinska University—Huddinge Hospital in accordance with the policy on humane care and use of laboratory animals. The rats were maintained under uniform conditions for a period of least 1 week before commencement of the experiment. Free access to water and standard pelleted food was provided. The rats received soft food during the first 2 days after surgery, and the weight of the rats was followed during the postoperative interval. A rat periodontal wound model reported by King and Hughes12 was used. Briefly, the rats were anaesthetized by isoflurane inhalation (4% induction, 2%–3% maintenance); then, an extraoral incision was made at the lower border of the mandible and the underlying fascia, and a masseter was retracted to permit direct access to the mandibular bone. Bone, periodontal ligament, cementum, and superficial dentine overlying the distal roots of the first molars were removed using a bur in a slow-speed handpiece with saline irrigation. The superior border of the fenestration was ∼1 mm below the alveolar crest. The defect height and depth were ∼2 mm and were extended horizontally by 3–4 mm. The first molar vitality was completely preserved after surgery. Both mandible sides, left and right, were operated in all rats. The periodontal wound was covered with a construct containing hMSCs or a construct alone, or left untreated. The incisions were closed with single sutures in two layers. All rats daily received cyclosporin-A (Sandimmun, Novartis Sverige AB; 5 mg/kg subcutaneously). The used dosage of cyclosporin-A is considered low, and the drug did not interfere with the bone tissue turnover.13
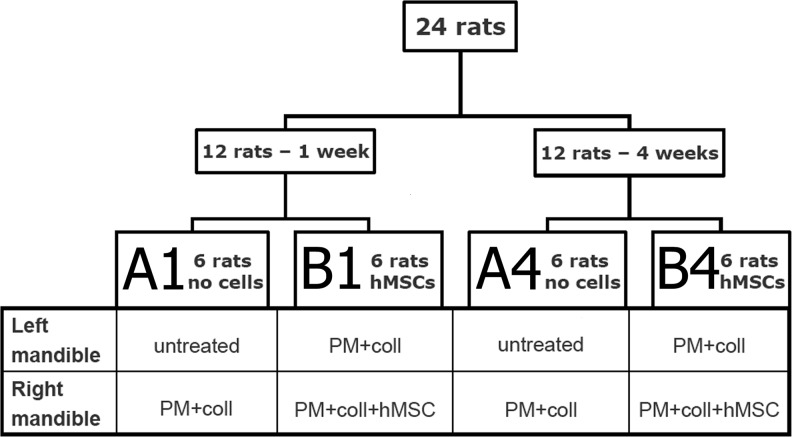
Twenty-four Sprague–Dawley rats (male, ∼350 g) were operated. The rats were randomly and equally divided into four groups: A1, B1, A4, and B4 (Fig. 1). Twelve rats (groups A1 and B1) were followed for 1 week, and the other 12 rats (groups A4 and B4) were followed for 4 weeks after surgery. The hMSCs seeded onto the scaffold were implanted into the right mandible side in six rats for each time interval (groups B1-right and B4-right). The other operated half-mandibles were either untreated (groups A1-left and A4-left) or received the construct alone (groups A1-right, B1-left, A4-right, and B4-left).
FIG. 1.
Diagram representing the experimental set-up, including animal number, type of treatment, and healing time. A1, B1, A4, B4, group labels; PM, PuraMatrix peptide hydrogel; coll, collagen sponge HELISTAT; hMSCs, human mesenchymal stem cells.
Three nonoperated rats also daily received cyclosporin-A (5 mg/kg subcutaneously) for 1 week before euthanasia. Their mandibles were collected, and used as healthy controls.
Tissue preparation
The rats were euthanized by CO2 inhalation and mandibles, bone marrow, and calvaria bone were collected.
The left and right mandibles from four rats that received the hMSCs (two rats per each time point) were frozen at −70°C, and subsequently used for DNA extraction. The rest of the mandibles were fixed in 4% solution paraformaldehyde overnight, decalcified for 4 weeks in 12.5% EDTA at 4°C, and embedded in paraffin; 5-μm serial horizontal sections were prepared and placed on glass slides. Tissue sections were stained with HE for the assessment of general morphology, bone formation, and local inflammatory response, or stained for tartrate-resistant acid phosphatase (TRAP) for osteoclast detection. TRAP staining was performed according to the manufacturer's guidelines (Leukocyte Acid Phosphatase [TRAP] kit; Sigma-Aldrich). Osteoclasts were defined as TRAP-positive cells with two or more nuclei attached to the bone surface.
Bone marrow was collected from each rat by flushing the right femur diaphysis with 1 mL of phosphate buffer solution. The calvaria bones were collected from the rats with no hMSCs implanted. The samples were frozen and stored at −70°C.
hMSCs tracking in vivo
The FISH method described by Hertegård et al.14 was used for the hMSCs tracking in vivo by detecting a human-specific DNA sequence in the rat mandible tissue sections. Moreover, total DNA was extracted from the frozen rat mandibles, rat calvarias, rat bone marrow, and cultured human osteogenic sarcoma cells (SAOS-2; American Type Culture Collection) with the DNeasy Blood and Tissue kit (Qiagen). The samples were treated according to the standard protocol with the exception of the rat mandibles and calvaria. The mandibles and calvaria were incubated with ATL buffer and proteinase K, both from the DNeasy Blood and Tissue kit, at 56°C for 24 h instead of 2 h. Absolute quantification of the human DNA present in the rat tissues was performed in accordance with previously published data.15
The primers designed for the human-specific repetitive ALU DNA sequence were synthesized by Cybergene with the following sequences: ALU Fw: 5′-GAC ATC GAG ACC ATC CCG GCT AAA-3′; ALU Rev: 5′-CTC AGC CTC CCA AGT AGC TG-3′. Real-time PCRs were run in a 7500 PCR system (Applied Biosystems) for 40 cycles.
Alveolar bone histomorphometry
The bone volume density (%) of the alveolar bone that surrounded the roots of the first molar was calculated using the grid-system approach and image-analysis software (ImageJ; National Institutes of Health). Three HE-stained tissue sections per each sample were analyzed.
The osteoclast number (cells/mm2) was calculated based on the measurement of the bone tissue area of the alveolar bone that surrounded the roots of the first molar and the counting of TRAP-positive cells in contact with the bone. Two TRAP-stained tissue sections (two levels) per sample were analyzed. Detailed descriptions of the histomorphometric methods can be found elsewhere.16,17
The data were statistically analyzed by one-way ANOVA followed by the paired Student's t-test with Bonferroni adjustment of p-values. The significance was defined as p<0.05.
Results
hMSCs survival
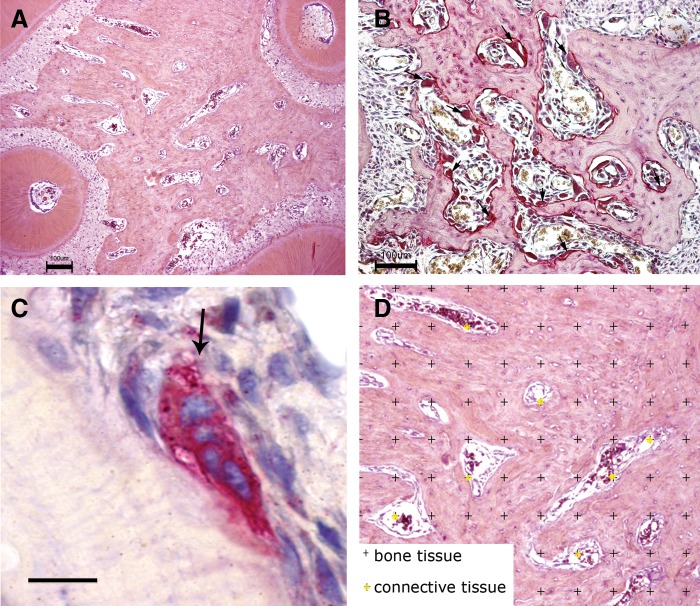
MTT assay showed that seeded hMSCs were viable before implantation (Fig. 2A). Morphological analysis of the in vitro seeded scaffold revealed that the hMSCs were completely surrounded and embedded in the PM peptide hydrogel (Fig. 2B). The collagen sponge formed the nucleus of the construct. No hMSCs migrated into the collagen sponge. The PM peptide hydrogel formed loose bonds with the collagen sponge. The presence of collagen sponge facilitated the handling and the implantation of the construct.
FIG. 2.
Photomicrographs showing the construct seeded with the hMSCs. (A) MTT staining of viable cells. (B) Hematoxylin-eosin (HE) staining showing rounded hMSCs inside the PM. MSCs, mesenchymal stem cells. Bar=100 μm.
The human DNA was detected only in the right rat mandibles at 1 week after surgery where the hMSCs were implanted. No human DNA was found in all other samples, including the rat bone marrow samples.
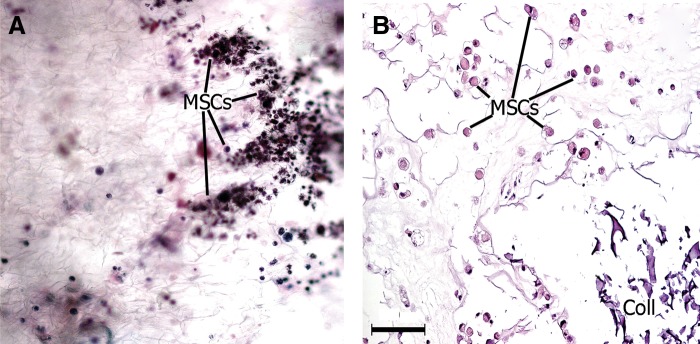
The FISH analysis revealed human cells only in the right rat mandibles at 1 week after surgery where the hMSCs were implanted (Fig. 3A). The hMSCs were mainly located in the periodontal defect area. However, a few human cells were scattered between the bone periosteum and overlying muscles. No human cells were detected in all other rat mandibles. The sections from the scaffold seeded with hMSCs were used as positive controls for the FISH (Fig. 3B).
FIG. 3.
Fluorescent in situ hybridization analysis. (A) Representative picture of a right mandible defect area with the implanted hMSCs at 1 week after surgery. (B) Scaffold seeded with hMSCs used as a positive control. Bar=100 μm.
Periodontal wound healing
All rats survived the postoperative period, and there was no decrease in body mass.
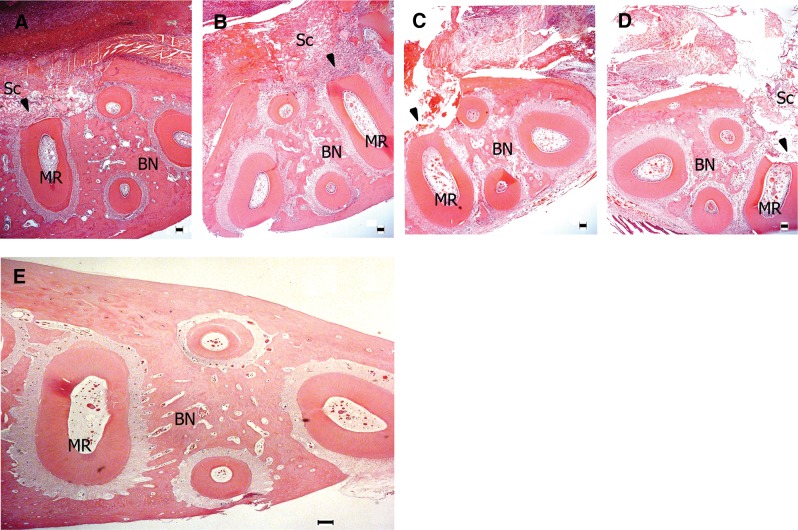
Periodontal wounds without any implants were filled with loose connective tissue at 1 week after surgery (Fig. 4C). Many remnants of the scaffold were founded at the site of implantation at 1 week after surgery (Fig. 4A, B, D). Bone defects remained unhealed, and no new bone formation was found in any of the samples at 1 week after surgery. The damaged periodontal ligament and cementum also remained unhealed in all operated rats at 1 week after surgery.
FIG. 4.
Histological images illustrating the general morphological aspect of the alveolar bone surrounding the roots of the first molar at 1 week after surgery. Arrow heads point to the defect areas and the damaged roots. (A) Left mandible, defect covered with an empty scaffold (group B1-left); (B) right mandible, defect covered with a scaffold containing hMSCs (group B1-right); (C) left mandible, untreated defect (group A1-left); (D) right mandible, defect covered with an empty scaffold (group A1-right); (E) normal rat mandible. Sc, residual scaffold; BN, alveolar bone; MR, molar root. Bars=100 μm. HE staining.
The bone defects were healed by newly formed bone tissue in all operated rats at 4 weeks after surgery (Fig. 5A–D). The damaged periodontal ligament and cementum were restored to some extent but not completely at 4 weeks after surgery. Some traces of the implanted scaffolds were still present in the rat tissue at 4 weeks after surgery. There were no obvious differences in the amount of the newly formed bone or the healing rate of the cementum, or the periodontal ligament between the treated groups. Furthermore, there was no increase in the local inflammatory reaction, and no tumor-like formations were found in any of the mandibles treated with the hMSCs at 1 week or 4 weeks after surgery. Damaged dentin did not heal in any of the rats.
FIG. 5.
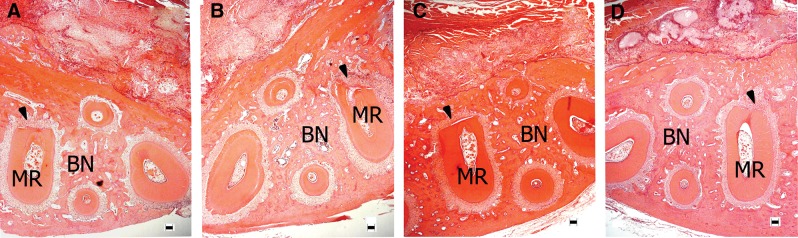
Histological images illustrating the general morphological aspect of the alveolar bone surrounding the roots of the first molar at 4 weeks after surgery. Arrow heads point to the defect areas and the damaged roots. (A) Left mandible, defect covered with an empty scaffold (group B4-left); (B) right mandible, defect covered with a scaffold containing hMSCs (group B4-right); (C) left mandible, untreated defect (group A4-left); (D) right mandible, defect covered with an empty scaffold (group A4-right). Bars=100 μm. HE staining.
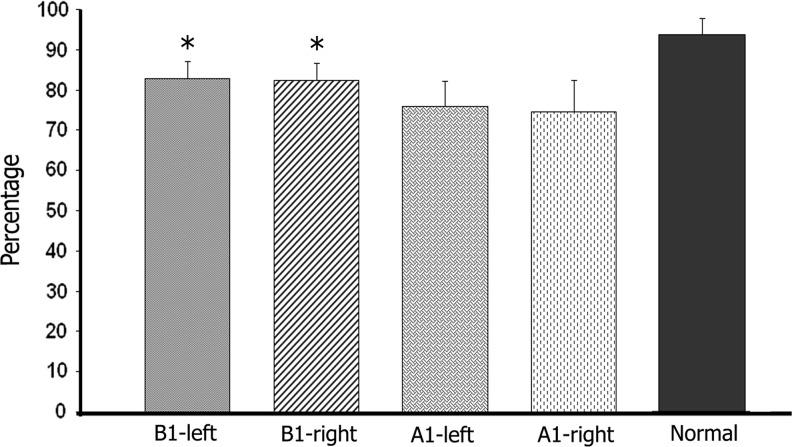
The quantitative assessment of the bone tissue surrounding the roots of the first molar showed a significant decrease in the bone volume density in all operated mandibles at 1 week and 4 weeks after surgery compared with a similar area of the healthy nonoperated mandibles. However, at 1 week after surgery, the bone volume density of the alveolar bone was significantly better in the operated mandibles of the rats that received hMSCs (groups B1-left and B1-right) compared with the operated mandibles from the rats without hMSCs implantation (groups A1-left and A1-right) (Fig. 6).
FIG. 6.
Graph showing the volume density of the alveolar bone surrounding the roots of the first molar at 1 week after surgery (groups A1, B1). Three tissue sections (three levels) per sample were analyzed. *Significance is marked in comparison to the alveolar bone from the operated rats with no hMSCs implanted.
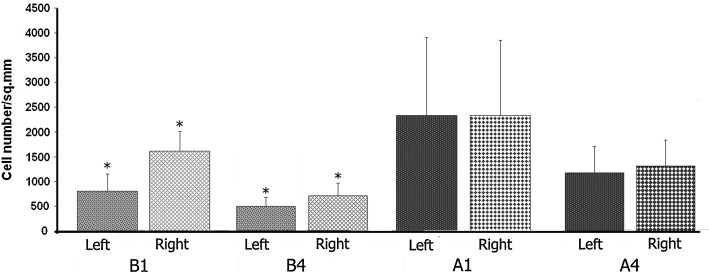
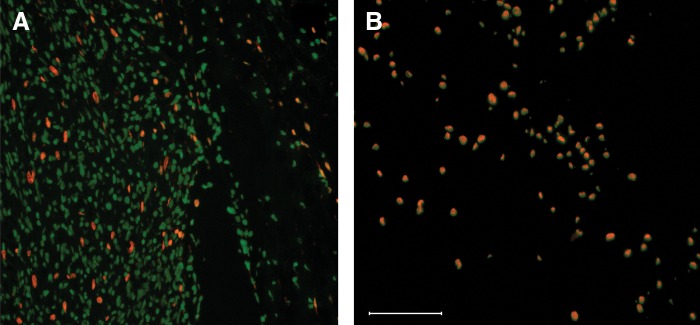
The osteoclast number (TRAP-positive cells) in the bone tissue surrounding the roots of the first molar was significantly reduced in the operated rats treated with hMSCs (groups B1 and B4) compared with the control rats at 1 week and 4 weeks after surgery (groups A1 and A4) (Fig. 7). There was no statistically significant difference in the osteoclast number inside the groups (when compared from left to right). No osteoclasts were found in the healthy nonoperated mandibles (Fig. 8A), which was contrary to the vast number of osteoclasts in the operated mandibles (Fig. 8B).
FIG. 7.
Number of osteoclasts found in the alveolar bone surrounding the roots of the first molar at 1 week (groups A1 and B1) or 4 weeks after surgery (groups A4 and B4). Two tissue sections (two levels) per sample were analyzed. *Significance is marked in comparison to the alveolar bone from the operated rats with no hMSCs implanted.
FIG. 8.
Representative photomicrographs showing tartrate-resistant acid phosphatase (TRAP) stained tissue sections. Arrows point to TRAP-positive multinucleated cells (osteoclasts). (A) Normal bone from nonoperated mandible. (B) bone surrounding the roots of the first molar of the right operated mandible from the rat with no hMSCs implanted. (C) higher magnification of a TRAP-positive multinucleated cell similar to those presented in (B). (D) Examples of identification of histomorphometric parameters (registration of intersection hits) using the grid system on the digital images of HE-stained mandible tissue sections. Bars=100 μm (A, B), and 10 μm (C).
Discussion
A better understanding of the periodontal wound healing would allow us to develop new therapies that might lead to complete periodontal regeneration.18 In the current study, a rat periodontal wound model was used to elucidate the effects of local treatment with undifferentiated hMSCs on periodontal healing and alveolar bone reaction. We have mixed hMSCs with PM in combination with collagen sponge as a delivery vehicle for the cells by taking into consideration existing published data. According to Bokhari et al.,19 the PM might enhance osteoblast growth and differentiation in vitro, and Misawa et al.20 reported that PM facilitated the healing of calvarial bone defects in mice. Moreover, collagen sponges have been proved to enhance the survival of different cell types, including cardiomyoblasts, for the treatment of ischemic rat hearts21 and hMSCs for the treatment of traumatic brain injury.22 In our case, the PM-collagen constructs were easier to handle and possessed better mechanical and hemostatic properties compared with PM alone.
We have hypothesized that undifferentiated MSCs delivered on the PM-collagen constructs may enhance periodontal wound healing and could prevent alveolar bone loss by modulating the local inflammatory reaction. Indeed, the rats treated with hMSCs had a significantly better alveolar bone density at 1 week after surgery at both the site of cell implantation and the opposite site, suggesting a paracrine osteo-protective mechanism by means of soluble factors that are able to modulate the host immune response without generating the new tissue. Tour et al.23 reported a similar modulatory effect on the local inflammatory reaction in rat calvarial defects treated with MSC-loaded constructs. However, the exact mechanisms behind the immunomodulatory effects are not fully defined but appear to be mostly mediated by the secreted transforming growth factor-beta 1, hepatocyte growth factor, prostaglandin E2, indoleamine 2,3-dioxygenase, soluble HLA-G5, IL-10, and IL-6.24 We found no difference in bone volume density at 4 weeks after surgery that may be linked to the fact that hMSCs were not present anymore.
The local treatment with hMSCs has also significantly decreased osteoclast number at the site of injury at both 1 week and 4 weeks after surgery. Osteoclasts are tissue-specific multinucleated cells derived from the monocyte/macrophage hematopoietic lineage that are capable of breaking down mineralized bone, dentine, and calcified cartilage.25,26 We may speculate that macrophages could be the major type of effector cells through which MSCs exert their osteo-protective effects. We believe that MSCs may interact with the host monocyte/macrophage populations already at early time points, therefore mediating the local inflammatory response and osteoclast formation. This is supported by the published data reporting the therapeutic effect of MSCs through the stimulation of host macrophages to produce IL-10,27 which has a potent inhibitory effect on osteoclastogenesis.28
hMSCs survival
The FISH analysis and PCR data revealed that hMSC number decreased significantly over time, and no hMSCs were detectable at 4 weeks after implantation. The significant reduction of hMSCs may indicate an early cell death that can be attributable to ischemia and inflammation-related factors. Anyhow, several strategies have been suggested for improving the survival of the implanted hMSCs and subsequently increase the rate of cell engraftment. These strategies might include pretreatment with pro-survival cocktail targeting key factors of potential death pathways as suggested by Laflamme et al.29 or a chemokine preconditioning as suggested by Pasha et al.30 Furthermore, various experimental settings demonstrated the important role of MSC osteogenic induction in vitro. For example, Castano-Izquierdo et al. showed that rat bone marrow-derived MSCs stimulated in vitro with osteogenic media for 4 days induced the largest new bone formation in vivo.31 However, they used a different substrate (titanium fiber mesh) and a different cell-culture setup before implantation in vivo.
In conclusion, the transplanted hMSCs seeded onto peptide hydrogel have had an osteo-protective effect. The hMSCs can contribute to the alveolar bone preservation after surgical trauma, at least by decreasing the osteoclast number.
Acknowledgments
This work was supported by funds from the Swedish Research Council, the Stockholm City Council, and Karolinska Institutet.
Author Disclosure Statement
The authors have nothing to disclose.
References
- 1.Nanci A. Bosshardt DD. Structure of periodontal tissues in health and disease. Periodontol 2000. 2006;40:11–28. doi: 10.1111/j.1600-0757.2005.00141.x. [DOI] [PubMed] [Google Scholar]
- 2.Papapanou PN. Tonetti MS. Diagnosis and epidemiology of periodontal osseous lesions. Periodontol 2000. 2000;22:8–21. doi: 10.1034/j.1600-0757.2000.2220102.x. [DOI] [PubMed] [Google Scholar]
- 3.Wang HL. Greenwell H. Fiorellini J, et al. Periodontal regeneration. J Periodontol. 2005;76:1601–1622. doi: 10.1902/jop.2005.76.9.1601. [DOI] [PubMed] [Google Scholar]
- 4.Zohar R. Tenenbaum HC. How predictable are periodontal regenerative procedures? J Can Dent Assoc. 2005;71:675–680. [PubMed] [Google Scholar]
- 5.Carnevale G. Kaldahl WB. Osseous resective surgery. Periodontol 2000. 2000;22:59–87. doi: 10.1034/j.1600-0757.2000.2220106.x. [DOI] [PubMed] [Google Scholar]
- 6.Chamberlain G. Fox J. Ashton B. Middleton J. Concise review: mesenchymal stem cells: their phenotype, differentiation capacity, immunological features, and potential for homing. Stem Cells. 2007;25:2739–2749. doi: 10.1634/stemcells.2007-0197. [DOI] [PubMed] [Google Scholar]
- 7.Maggini J. Mirkin G. Bognanni I, et al. Mouse bone marrow-derived mesenchymal stromal cells turn activated macrophages into a regulatory-like profile. PLoS One. 2010;5:e9252. doi: 10.1371/journal.pone.0009252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nauta AJ. Kruisselbrink AB. Lurvink E, et al. Mesenchymal stem cells inhibit generation and function of both CD34+-derived and monocyte-derived dendritic cells. J Immunol. 2006;177:2080–2087. doi: 10.4049/jimmunol.177.4.2080. [DOI] [PubMed] [Google Scholar]
- 9.Srouji S. Kizhner T. Livne E. 3D scaffolds for bone marrow stem cell support in bone repair. Regen Med. 2006;1:519–528. doi: 10.2217/17460751.1.4.519. [DOI] [PubMed] [Google Scholar]
- 10.Semino CE. Self-assembling peptides: From bio-inspired materials to bone regeneration. J Dent Res. 2008;87:606–616. doi: 10.1177/154405910808700710. [DOI] [PubMed] [Google Scholar]
- 11.Mankani MH. Kuznetsov SA. Marshall GW, et al. Creation of new bone by the percutaneous injection of human bone marrow stromal cell and HA/TCP suspensions. Tissue Eng Part A. 2008;14:1949–1958. doi: 10.1089/ten.tea.2007.0348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.King GN. Hughes FJ. Bone morphogenetic protein-2 stimulates cell recruitment and cementogenesis during early wound healing. J Clin Periodontol. 2001;28:465–475. doi: 10.1034/j.1600-051x.2001.028005465.x. [DOI] [PubMed] [Google Scholar]
- 13.Movsowitz C. Epstein S. Fallon M, et al. Cyclosporin-A in vivo produces severe osteopenia in the rat: effect of dose and duration of administration. Endocrinology. 1988;123:2571–2577. doi: 10.1210/endo-123-5-2571. [DOI] [PubMed] [Google Scholar]
- 14.Hertegård S. Cedervall J. Svensson B, et al. Viscoelastic and histologic properties in scarred rabbit vocal folds after mesenchymal stem cell injection. Laryngoscope. 2006;116:1248–1254. doi: 10.1097/01.mlg.0000224548.68499.35. [DOI] [PubMed] [Google Scholar]
- 15.Nicklas JA. Buel E. Development of an Alu-based, real-time PCR method for quantitation of human DNA in forensic samples. J Forensic Sci. 2003;48:936–944. [PubMed] [Google Scholar]
- 16.Dalle Carbonare L. Valenti MT. Bertoldo F, et al. Bone microarchitecture evaluated by histomorphometry. Micron. 2005;36:609–616. doi: 10.1016/j.micron.2005.07.007. [DOI] [PubMed] [Google Scholar]
- 17.Vedi S. Compston J. Bone histomorphometry. Methods Mol Med. 2003;80:283–298. doi: 10.1385/1-59259-366-6:283. [DOI] [PubMed] [Google Scholar]
- 18.Aukhil I. Biology of wound healing. Periodontol 2000. 2000;22:44–50. doi: 10.1034/j.1600-0757.2000.2220104.x. [DOI] [PubMed] [Google Scholar]
- 19.Bokhari MA. Akay G. Zhang S, et al. The enhancement of osteoblast growth and differentiation in vitro on a peptide hydrogel-polyHIPE polymer hybrid material. Biomaterials. 2005;26:5198–5208. doi: 10.1016/j.biomaterials.2005.01.040. [DOI] [PubMed] [Google Scholar]
- 20.Misawa H. Kobayashi N. Soto-Gutierrez A, et al. PuraMatrix facilitates bone regeneration in bone defects of calvaria in mice. Cell Transplant. 2006;15:903–910. doi: 10.3727/000000006783981369. [DOI] [PubMed] [Google Scholar]
- 21.Kutschka I. Chen IY. Kofidis T, et al. Collagen matrices enhance survival of transplanted cardiomyoblasts and contribute to functional improvement of ischemic rat hearts. Circulation. 2006;114:167–173. doi: 10.1161/CIRCULATIONAHA.105.001297. [DOI] [PubMed] [Google Scholar]
- 22.Lu D. Mahmood A. Qu C, et al. Collagen scaffolds populated with human marrow stromal cells reduce lesion volume and improve functional outcome after traumatic brain injury. Neurosurgery. 2007;61:596–602. doi: 10.1227/01.NEU.0000290908.38438.B2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tour G. Wendel M. Tcacencu I. Bone marrow stromal cells enhance the osteogenic properties of hydroxyapatite scaffolds by modulating the foreign body reaction. J Tissue Eng Regen Med. 2012 Jul 10; doi: 10.1002/term.1574. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 24.Keating A. How do mesenchymal stromal cells suppress T cells? Cell Stem Cell. 2008;2:106–108. doi: 10.1016/j.stem.2008.01.007. [DOI] [PubMed] [Google Scholar]
- 25.Martin TJ. Sims NA. Osteoclast-derived activity in the coupling of bone formation to resorption. Trends Mol Med. 2005;11:76–81. doi: 10.1016/j.molmed.2004.12.004. [DOI] [PubMed] [Google Scholar]
- 26.Chambers TJ. Regulation of the differentiation and function of osteoclasts. J Pathol. 2000;192:4–13. doi: 10.1002/1096-9896(2000)9999:9999<::AID-PATH645>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- 27.Nemeth K. Leelahavanichkul A. Yuen PS, et al. Bone marrow stromal cells attenuate sepsis via prostaglandin E(2)-dependent reprogramming of host macrophages to increase their interleukin-10 production. Nat Med. 2009;15:42–49. doi: 10.1038/nm.1905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Evans KE. Fox SW. Interleukin-10 inhibits osteoclastogenesis by reducing NFATc1 expression and preventing its translocation to the nucleus. BMC Cell Biol. 2007;8:4. doi: 10.1186/1471-2121-8-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Laflamme MA. Chen KY. Naumova AV, et al. Cardiomyocytes derived from human embryonic stem cells in pro-survival factors enhance function of infarcted rat hearts. Nat Biotechnol. 2007;25:1015–1024. doi: 10.1038/nbt1327. [DOI] [PubMed] [Google Scholar]
- 30.Pasha Z. Wang Y. Sheikh R, et al. Preconditioning enhances cell survival and differentiation of stem cells during transplantation in infarcted myocardium. Cardiovasc Res. 2008;77:134–142. doi: 10.1093/cvr/cvm025. [DOI] [PubMed] [Google Scholar]
- 31.Castano-Izquierdo H. Alvarez-Barreto J. van den Dolder J, et al. Pre-culture period of mesenchymal stem cells in osteogenic media influences their in vivo bone forming potential. J Biomed Mater Res A. 2007;82:129–138. doi: 10.1002/jbm.a.31082. [DOI] [PubMed] [Google Scholar]