Abstract
Social and marital factors may influence women's health outcomes. This is of particular relevance in sub-Saharan Africa, where women's health indicators lag behind the rest of the world. Our study examines the impact of social mediators of women's health during key events (pregnancy and illness) in urban Mali. In this cross-sectional study, we interviewed 324 women aged 15-80, living in Bamako, the capital city, in 1999. We used mixed quantitative and qualitative methods to obtain detailed histories of pregnancy and illness during specific time periods preceding the survey. We examined the role of marital factors (polygyny, widowhood), social factors (sources of support and scales derived for social network and social power), and household wealth on women's therapeutic itineraries. We compared the sociodemographic characteristics of our sample with those of the 2001 Mali Demographic and Health Survey and used their data on contraception to enrich analyses.
We found that most pregnant women delivered in a health center and most women sought medical care during an illness event. Household wealth influenced illness reporting, and financial concerns were obstacles to medical care. Polygyny was associated with lower prevalence of contraceptive use, lower social power, as well as with less support received during pregnancy from women's husbands and in-laws. Widowhood appeared to increase susceptibility to illness, while decreasing resort to biomedical care. Our social composite scores highlighted differences in healthcare utilization in an urban setting with near-uniform access to biomedical care. We validate the utility of locally-derived composite scores, which may provide a deeper understanding into the social mediation of health outcomes for women.
Keywords: Women's health, marriage, Africa, Mali, pregnancy, social network, social power
Introduction
In sub-Saharan Africa, women's development lags behind that of the rest of the world, in terms of maternal and child mortality, education, and economic parity. Within this context, women's ability to access key resources and to effect decisions by using wealth and social mediators -- such as marital factors, social networks and social power --, may positively impact their health and that of their children (Adams et al., 2002; Haddad et al., 1997; Madhavan, 2002; Madhavan & Adams, 2003; Pick & Obermeyer, 1996; Simon et al., 2002).
Among marital factors, marital type (monogamy, polygyny) and status (married, single, widowed) have been identified as important social mediators of women's health. For example, polygyny is a normative marital system in sub-Saharan Africa that structures women's access to critical resources, requires both intense cooperation and competition among co-wives, and persists in light of urbanization, female education and other broad social changes (Lesthaeghe et al., 1989; van de Walle, 2005). In sub-Saharan Africa, studies suggest that polygyny may modulate reproductive health, including sexually transmitted infections (STIs) (Adeokun & Nalwadda, 1997), fertility (Gibson & Mace, 2007) and infant survivorship (Gyimah, 2009). It may also be a risk factor for intimate partner violence (Uthman et al., 2010) and mental health problems (Donkor & Sandall, 2007; Mbassa Menick & Sylla, 1996). Postulated mechanisms include weaker conjugal bonds and increased infidelity by husbands in polygynous marriages, husbands' preferential investment in wives and children, and co-wife conflict. Individual fertility, household income, support from sons, relationship with one's mother-in-law, and marital rank modulate the relationship between marital type and health outcomes (Bove & Valeggia, 2009; Jankowiak et al., 2005; Madhavan, 2002; Wittrup, 1990). It should be noted that quantitative research on polygyny in sub-Saharan Africa is hampered by a number of confounders (e.g. women's age and position within the life cycle), by the fact that most monogamous marriages have the potential to become polygynous with increasing husband age and status, and by high rates of divorce and remarriage.
Widows also face additional risks, due to financial and economic hardship, land and housing insecurity, loss of social standing and support from agnatic kin, social isolation, depression and grief—all factors with implications for fertility and physical and mental health (Millman & Potter, 1984; Ogungbamila & Adeyanju, 2010; Onadeko et al., 2002) (Chapoto et al., 2011; Davhana-Maselesele, 2005). Additionally, the practice of the levirate, by which a widow is obligated to marry her late husband's brother, is a specific risk factor for the transmission of STI's (Agot et al., 2010; Lopman et al., 2009).
In addition to marital factors, social power and connectedness have been acknowledged as mediators of women's health in recent years. A quantification of women's social support networks in Mali revealed that both the size and composition (e.g. parity; presence of subject's mother vs. conjugal kin; cooperative vs. conflictual relationships among co-wives; membership in a women's association) of these networks vary across the life cycle, and that they influence contraceptive use, number of children born, and child survival (Adams et al., 2002; Madhavan & Adams, 2003; Simon et al., 2002).
Still, the impact of women's social power and connectedness on health beyond the arenas of reproductive health and STI transmission remains understudied. Women's social connectedness may be linked to obesity in more resource-rich areas (Shayo & Mugusi, 2011) and may improve palliation at the end of life (in cancer and HIV settings (Selman et al., 2011)); conversely, lack of connectedness may be associated with cognitive decline (Gureje et al., 2011). Additionally, women who are in a position to care for their grandchildren may enjoy better nutritional status (Ice et al., 2011).
In the current study, we asked how marital and social factors in an urban African setting might influence the therapeutic itinerary of women. This itinerary denotes the path that an individual follows from symptom onset, to selection of healer(s) (e.g. traditional vs. biomedical) and therapies (traditional vs. pharmacological), and eventual outcomes. Therapeutic itineraries in sub-Saharan Africa are not only affected by geographic accessibility and affordability of care but also by sociocultural representations of illness, cultural and gender-based norms governing behavior, individual autonomy, and expectations surrounding the expertise of and possibility for communication with the given provider (Bila & Egrot, 2009; Commeyras et al., 2006; Ly et al., 2002; Ouendo et al., 2005).
In our analysis of the therapeutic itinerary of women during pregnancy and illness, we used quantitative data obtained from semi-structured interviews of 324 women, as well as more detailed qualitative interviews from a subset of 25 women, from the Health Itinerary and Social Support Survey (HISSS) conducted in 1999 in Bamako, Mali. We ask the following research questions:
What is the role of social factors, including marital, household and social characteristics, in determining women's access to care or support received?
What are important deviations of social support received during illness from cultural norms, and how might these highlight key social mediators?
Data and Methods
Study Site and Population
Setting
This study is composed of two cross sectional surveys of women living in Bamako, the capital of the Republic of Mali. Mali, a landlocked country in West Africa, is one of the poorest countries in the world, ranking 178 out of 182 countries in the 2007 Human Development Index of the United Nations Development Program (UNDP). Mali had a population of 9.8 million people in 1998 (DNSI/Institut du Sahel, 2004) and 15.4 million in 2010 (World Bank, http://data.worldbank.org/country/mali). In Bamako, a city of approximately 1 million inhabitants, many ethnicities are represented, including the dominant Malinke and Bamanan, as well as other groups including the Fulani (Peul), Dogon, Bozo, Songhai and Tuareg. The primary income in Mali is from agriculture, animal husbandry and fishing, but the country relies heavily on foreign aid. For 1998-2000, the World Bank indicators for Mali include a GNI per capita of 240 USD, and per capita health expenditure of 17 USD per year. The total fertility rate was 6.8 children per woman; 17 % of women aged 15-24 were literate; the maternal mortality rate was 980 per 100,000 live births, and under-5 mortality was 217 per 1,000 live births (World Bank, http://data.worldbank.org/country/mali). In Bamako, 74% of people lived within 15 kilometers of a hospital and 86% lived within 5 kilometers of a health center in 2001 (94% within 14 km) (CPS/MS et al., 2002). Among women aged 15-49, 86% were married (29% of these were married polygynously), and 59% were employed. Following a decade of continued human development, the maternal mortality rate of 830 per 100,000 live births in 2008 and under-5 mortality rate of 178 per 1,000 live births in 2010 remain high (World Bank, http://data.worldbank.org/country/mali), with Mali ranked 175 out of 187 countries in the 2011 the UNDP Human Development Index (http://hdr.undp.org/en/statistics).
Study Design
Sample 1:1999 Health Itinerary and Social Support Survey (HISSS)
The primary sample from which our observations were drawn consists of a cross-sectional questionnaire administered to 324 women, aged 15-80, living in Bamako. Our study was conducted November and December, 1999. Three neighborhoods were selected for study inclusion, based on recency of settlement of inhabitants, material development (running water, electrification) and demographic growth (Marcoux et al., 1995): Medina Coura (N=108), Lafiabougou (N=120), and Sabalibougou (N=96). Of these three neighborhoods, Medina Coura was the first settled and most developed, and Sabalibougou was composed mostly of recent migrants and the least developed. A random generator was then used to assign an interviewing order to women aged 15-25, 25-45 and over 45 in a 1:2:1 ratio. This was performed in order to increase our sample of older, hence polygynously married or widowed, women. In compensation for their time, women were given a bag of seasoning, which is typically a women's expense in Malian households. No women refused to participate.
Data were collected using a combination of exploratory and triangulation mixed methods strategies, as described by Creswell, in several steps (2008). In an initial exploratory sequential phase, the lead author conducted three months of qualitative research in Bamako, including focus groups and interviews with women of various ages, traditional healers, public health administrators and medical professionals. This work led to the design of a research qualitative instrument. In a second phase, we used a concurrent triangulation strategy, in order to draw upon the strengths both of simultaneously collected quantitative and qualitative research. A semi-structured quantitative questionnaire, informed by our exploratory phase, was administered by four experienced female Malian research assistants. The questionnaire was initially written in French, translated into Bambara by the team of researchers, and reverse-translated into French to ensure accuracy. The following information was requested: demographic, marital, and household characteristics; sources of social support; pregnancy history in the prior two years; knowledge of contraception; and illness history in the prior three months. Additionally, interviewers were trained in qualitative interviewing techniques, and using open-ended questioning, asked women probing questions about the impact on illness experiences of their relationships with husbands and other household members. These additional questions were performed following individual responses, as well as at the conclusion of the interview. A more detailed qualitative ethnographic interview was held immediately following the quantitative questionnaire by the lead author, for a subset of 25 women, with a translator's assistance. Approval for this study was granted by Mali's Centre National de la Recherche Scientifique et Technologique.
Independent variables
Individual characteristics such as age, marital status, ethnicity, religion, education, employment and place of birth were included in the analyses. Additionally, the following household characteristics were considered: household size (# individuals), ownership status, and neighborhood of residence.
We constructed three composite variables from the HISSS dataset based on reported sources of household wealth, social power or social network:
The household wealth index is a composite variable modeled on the DHS wealth index and based on principal components analysis of four variables: the construction material of the house (mud or concrete), lighting source (lamp or electricity), sanitation type (rudimentary or ameliorated latrine) and water source (exterior or interior tap) (Filmer & Pritchett 2001; http://www.measuredhs.com/topics/Wealth-and-Socioeconomics.cfm). All available variables on asset ownership and housing characteristics were considered, and principal components factor analysis indicated that variation in wealth was primarily determined by construction material, lighting source and water source. These three indicators were maintained and used to produce the wealth index score. For ease of interpretation, we then split this index into quartiles.
The social power score is a composite variable that is designed to leverage women's major sources of power within their households. Selection was based on an extensive literature search on women's sources of power in sub-Saharan Africa, as well as on the initial exploratory phase of this study. Variables included literacy (representing a measure of societal autonomy), independent source of income (affording some economic independence), freedom of choosing a husband and whether or not related to a husband (personal autonomy), living son (a major source of status for women in a patriarchal society), and presence of natal family in the household (a source of emotional and kin-based support) (Adams et al., 2002; Ahmed et al., 2010; Beyeza-Kashesy et al., 2010; Campbell & Campbell, 1997; McTavish et al., 2010). Using the selected six items, we conducted a principal-components factor analysis to classify the items into a meaningful composite variable representing social power (eigenvalue of 1.86, and percentage of the covariance explained of 31%). We then split the resulting composite variable score into quartiles. This section of the analysis was not conducted for the 55 widows, because they were not asked about their choice in husband.
The social network score is a composite variable based on the total number of individuals a respondent identified in answering questions about number of domestic helpers, friends, and own children present in the household available to assist them and provide support. Like the previous two composite variables, principal components factor analysis was conducted to create a composite variable representing social network (eigenvalue of 1.12, and percentage of the covariance explained of 37%), and the resulting score was split into quartiles.
Outcome variables
There were three sets of outcome variables. First, pregnancy histories in the two years prior to the survey were obtained. This included use of prenatal care, delivery characteristics, and use of postnatal care. Second, women's knowledge of contraception was recorded. Third, women were asked about illness symptoms in the prior three months, and if present, treatments sought, financing of treatments, and sources of social support received during illness.
Sample 2: Enquête Démographique et de Santé Mali (EDSM) 2001 (Mali DHS 2001)
We compared our sample to—and supplemented our analysis with—data from Bamako collected in the 2001 Mali Demographic and Health Survey. The sampling methodology for the DHS has been extensively described elsewhere (Vaessen et al., 2005). Data from all women aged 15-49 surveyed in the EDSM 2001 who lived in Bamako were included for supplementary analysis (N = 2,067). Individual and household characteristics were included, as well as responses to a questionnaire on contraception. This allowed us to (1) assess the representativeness of our sample by comparing HISSS sociodemographic data against those obtained with EDSM sampling methodology, and (2) to supplement our analysis of contraception, for which limited data were collected in HISSS.
Statistical analysis
Data were analyzed using STATA version 11. Using the HISSS sample, we summarized sociodemographic characteristics for all women. Of the total sample of 324 women, we selected only those who were married or widowed at the time of the survey for statistical analysis, leaving an analytical sample of 308 individuals. Then, in order to examine the relationship between individual and household sociodemographic factors and health outcomes for HISSS, logistic and linear regression techniques were employed with age, marital type, neighborhood and composite scores as the independent variables, and contraception, reported illness, pregnancy, health system utilization, and social support as the outcome variables. All regressions included clustering for household.
We incorporated 2001 EDSM data on all women living in Bamako in two ways. First, we compared sociodemographic characteristics of women in HISSS and EDSM samples. Because the HISSS sampled for predetermined age categories with the intention of increasing the number of polygynous and widowed women, the age distribution was purposefully different from a sample representative of a growing population. Second, for outcomes pertaining to contraception, regression analyses were conducted both for HISSS and EDSM.
Results
I. Subject characteristics
Sociodemographics: comparison of HISSS and EDSM
Women in both samples had similar ethnicity, religion, and migration status profiles (Table 1). Women in HISSS were more often widowed, less literate, and polygynous women were more often senior wives than in EDSM, which likely reflects the age-based sampling in HISSS designed to include women beyond their reproductive years. As with HISSS, polygynous and widowed women in the EDSM tended to be older than monogamous women.
Table 1. Descriptive Characteristics of Women in the HISSS and EDSM samples (Percentage).
| Variable | All | Monogamous | Polygynous | Widowed | ||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| HISSS | EDSM | HISSS | EDSM | HISSS | EDSM | HISSS only | ||
| Marital Status | 100 | 100 | 56 | 70 | 22 | 27 | 17 | |
| Age Group | ||||||||
| 15 to 24 | 27 | 31 | 39 | 37 | 14 | 19 | 0 | |
| 25 to 34 | 25 | 40 | 30 | 42 | 27 | 37 | 7 | |
| 35 to 44 | 21 | 22 | 21 | 17 | 30 | 32 | 6 | |
| 45+ | 27 | 7 | 10 | 4 | 29 | 12 | 87 | |
| Schooling Level | ||||||||
| None | 53 | 51 | 43 | 49 | 56 | 55 | 89 | |
| Primary | 20 | 20 | 23 | 20 | 26 | 21 | 5 | |
| Secondary | 14 | 26 | 15 | 28 | 10 | 22 | 2 | |
| Tertiary | 14 | 3 | 19 | 4 | 9 | 1 | 4 | |
| Literate | 34 | 42 | 41 | 44 | 30 | 38 | 4 | |
| Ethnicity | ||||||||
| Bambara | 32 | 33 | 32 | 34 | 36 | 32 | 28 | |
| Malinke | 18 | 14 | 16 | 16 | 19 | 11 | 23 | |
| Peul | 21 | 16 | 24 | 16 | 11 | 17 | 23 | |
| Other | 30 | 37 | 28 | 35 | 34 | 41 | 26 | |
| Muslim | 98 | 98 | 97 | 97 | 100 | 100 | 98 | |
| Born in Bamako | 41 | 41 | 46 | 43 | 39 | 36 | 18 | |
| Neighborhood | ||||||||
| Sabalibougou | 30 | n/a | 28 | n/a | 31 | n/a | 33 | |
| Lafiabougou | 37 | n/a | 39 | n/a | 34 | n/a | 33 | |
| Medina Coura | 33 | n/a | 32 | n/a | 34 | n/a | 34 | |
| Household Head Owns House | 69 | n/a | 62 | n/a | 83 | n/a | 78 | |
|
| ||||||||
| Mean # Children Ever Born (std deviation) | 4.3(3.3) | 2.2(2.7) | 3.5(3.0) | 3.0(2.6) | 5.1(3.3) | 4.1(3.0) | 6.2(3.3) | |
|
| ||||||||
| N | 324 | 1,242 | 183 | 855 | 70 | 320 | 55 | |
Marital Factors
Approximately one quarter of HISSS women were married polygynously, with 76% of polygynous marriages consisting of only 2 wives, and 46% of polygynous women reporting being senior wives. Fewer than 6% of polygynous marriages had more than 3 wives. Sixty-seven percent of polygynous women lived in the same house as their co-wives.
Polygynous women were older than monogamous women, less often born in Bamako, less literate, had fewer years of schooling, and had more children. They more often lived in a house that was owned by the household head and that had more inhabitants overall, (Table 1). However, when controlling for age, only the differences in household size and household ownership between polygynous and monogamous women were statistically significant.
On average, polygynous women reported larger social networks than monogamous women, and larger percentages were in the lower wealth quartiles (Table 2); however, these did not differ after adjusting for age. Polygyny was significantly associated with a lower social power quartile even after adjusting for age.
Table 2. Descriptive Characteristics for Composite Variables from Mali 1999 HISSS Survey (Percentage).
| Composite Variable | All | Monogamous | Polygynous | Widows |
|---|---|---|---|---|
| Household Wealth | ||||
| Index Quartile | ||||
| First | 26 | 21 | 27 | 38 |
| Second | 30 | 32 | 33 | 21 |
| Third | 21 | 23 | 20 | 15 |
| Fourth | 23 | 23 | 20 | 25 |
| N | 274 | 163 | 64 | 47 |
| Social Power Quartile | ||||
| First | 29 | 25 | 38 | - |
| Second | 39 | 39 | 41 | - |
| Third | 8 | 9 | 6 | - |
| Fourth | 24 | 27 | 16 | - |
| N | 233 | 167 | 64 | - |
| Social Network | ||||
| Quartile | ||||
| First | 27 | 33 | 18 | 19 |
| Second | 23 | 19 | 18 | 43 |
| Third | 27 | 29 | 32 | 13 |
| Fourth | 23 | 19 | 31 | 26 |
| N | 292 | 173 | 65 | 54 |
Widows were older than married women. They had less schooling, were less literate, and had more children (Table 1), but these relationships were not significant when controlling for age. Their household wealth index scores were lower, with more clustering at both tails of the distribution; when controlling for age, there were no statistically significant differences between widows and married women in either of the composite variables for which widows were included (Table 2).
II Reproductive Health Data
A. Pregnancy care and outcome (HISSS)
Descriptive characteristics
Approximately 60% of women aged 18-49 reported a pregnancy in the prior two years. Of women reporting a pregnancy, 72% reported a live birth; 23% were pregnant at the time of interview, and 5% reported a miscarriage/abortion. Of the 103 live births, two infants subsequently died.
Women reported a fairly homogeneous perinatal health care utilization, with 81% going to at least the 4 World Health Organization recommended prenatal visits (WHO, 2006). The majority (77%) of these visits cost 1,000CFA or less (approximately 1.5 USD in 1999), and 85% were paid for by the subjects' husbands. Nearly all women delivered at a health center or hospital (98%). Women were accompanied to their delivery by agnatic kin (mother-in-law, usually) in 52% of cases, friends/neighbors in 15%, husbands in 13%, natal kin in 11%, co-wife in 4%, no-one in 3%, and midwife in 3% of cases. Just over half of women had at least one postnatal visit at the time of the study.
Marital Factors
There was no association between marital type and 2-year pregnancy history. Polygynous women were 83% less likely than monogamous women to be escorted to delivery by their husband or agnatic kin than were monogamous women, controlling for age, parity, neighborhood, household wealth index, social power and social network (OR=.17 and p < .01). There were no statistically significant differences between polygynous and monogamous women, and between senior and junior polygynous wives, in terms of pregnancy rates, prenatal visits, delivery location or postnatal visits.
Social Composite Scores
Larger social networks were significantly associated with increased odds of reporting a pregnancy in the prior two years, controlling for age (OR=1.36, p < .01). Additionally, controlling for age, an increase in household wealth index quartile was associated with a 73% increase in the odds of a husband or agnate kin escorting the woman to delivery (p < .05).
B. Contraception (HISSS and EDSM)
Descriptive Characteristics
Most respondents were aware of contraception (95% for EDSM and 83% for HISSS), although only 49% and 35% of EDSM and HISSS respondents, respectively, reported ever using a contraceptive method.
In HISSS qualitative interviews, confusion surrounding side effects of various contraceptives affected their utilization: “I stopped using the Pill because it made my periods late. Now I use injections” (24, monogamous, 2 children); or, “I had been using injections. Then I started the Pill but I had bleeding so I got scared. Now I don't use anything” (21, monogamous, 3 children).
Additionally, several women presented a cultural belief that with age, and as they become grandmothers, women should begin to limit their fertility. “My pregnancies have already become more spaced, so there is no need to use contraception to space them further” (30, monogamous, 3 children). Similarly, “I have been told that young girls should use the pill or condoms, and older women who already have had children should use injections” (41, polygynous, 5 children).
Marital Factors
Women in EDSM reported low partner approval for and communication about contraception: respondents reported husband approval in 47% of cases, disapproval in 32% cases, and 21% did not know how their husbands felt. Additionally, 49% did not discuss family planning with their husbands.
In EDSM, controlling for age, polygynous women were half as likely to report knowledge of contraception (OR= 0.45, p < .01), had 29% lower odds of discussing family planning with their partner (OR=.71, p < .05), and had 29% lower odds of using contraception (OR=.71, p < .05) compared to monogamous women.
In HISSS qualitative interviews married women often reported that their husbands forbade them from using contraception, usually because of expectations of fertility, or because contraception is perceived to reflect infidelity: Once married, “My husband said that I cannot use contraception, so I use the rhythm method” (26, monogamous, 1 child). One woman reported undergoing a clandestine medical abortion because “my husband refused to do family planning” (57 monogamous, 9 children). However, outside the institution of marriage, contraception became more important: “While I am divorced, I use contraception” (36, divorced, 2 children). Some women referred to the difficulties faced by unwed mothers in a society where marriage is normative: “I had my first daughter, unmarried, when I was 12. Now I am widowed and I don't want to ruin my life again, as that first birth took away the happiness of my youth. So, I use contraception” (32, widowed, 4 children).
Social Composite Scores
Controlling for age, higher household wealth (OR=1.53, p < .05), and social power (OR=2.64, p < .05) quartiles were associated with increased odds of reporting knowledge of contraception. Social network was not significantly associated with knowledge of contraception.
III. Health itineraries during Illness (HISSS)
Thirty-eight percent (n=123) of women reported illness symptoms in the prior 3 months. Among these, 61% sought treatment outside their homes. Table 3 summarizes the primary treatment characteristics. A majority consulted either a health clinic (56%) or a hospital (26%). Half of all women went to their healer alone, while 24% were accompanied by their husbands. Twenty-four percent of women reported that their illness was a reproductive health related (e.g. abnormal vaginal bleeding, pregnancy complications, STI).
Table 3. Health Seeking Characteristics of Mali 1999 HISSS Women Reporting Illness in Prior 3 Months.
| Variable | |
|---|---|
| Type of Healer (percent) | |
| Natal family | 1 |
| Traditional healer | 7 |
| Pharmacy | 3 |
| Health center | 1 |
| Health agent | 6 |
| Bamako hospital | 26 |
| Health clinic | 49 |
| Other | 7 |
| N | 72 |
| Escort to Healer (percent) | |
| No one | 50 |
| Husband | 24 |
| Healer went to her | 6 |
| Natal family | 11 |
| Agnate family | 8 |
| Other | 1 |
| N | 72 |
| Median cost of treatment in CFA (min, max) | 1000 (500, 50,000) |
| N | 50 |
Women named the following as the primary decision-maker for their therapeutic itinerary: their husband (61%), themselves (30%), another family member (6%), and another party (4%). One respondent clarified: “In a household the husband is the master. We owe him respect, and he must ensure the smooth running of the household. We are obliged to ask his permission” (35, monogamous, 2 children).
Financial concerns were a major obstacle to healthcare access. As one woman indicated, “I only used traditional medicines, because there was not enough money to follow modern treatments” (48, monogamous, 6 children). For married women, husbands had the primary role of financing women's health treatments, either directly or by enlisting the assistance of the household and extended kinship networks: “If my husband is in town he pays for my medication, otherwise I pay” (31, monogamous, 3 children). Sometimes, husbands were unable to pay: “My husband couldn't pay for all my rheumatism medication so he bought it in the pharmacy on credit (55, polygynous, 3 children). In the absence of a husband, “Women will give sarongs or kola nuts or other small gestures towards healers when they cannot pay them directly” (68, widowed, 2 children). Financial problems were routinely cited as significant stressors in the illness experience: “It is so difficult to become ill because there is no money to repay loans from people. Often my worries keep me up all night, since my children are not old enough yet to work. It's really painful” (38, monogamous, 5 children).
Individual characteristics
Older women were significantly more likely to report an illness than younger women. For example, women aged 45 and older had 3.7 times greater odds of reporting an illness compared to women aged 15-25 (p < 0.01). Controlling for age, birthplace outside Bamako was associated with a 45% reduced odds of reporting illness in the past 3 months (p < 0.05). After adjusting for age, there was no statistical association between education, household size, or neighborhood and illness symptoms or patterns of health utilization.
Marital variables
Polygynous women reported more illness symptoms than monogamous women (40% vs. 33%). Polygynous women more frequently stated that their husbands had made the decision to seek treatment (94% vs. 67%) and reported symptoms more commonly related to reproductive health (38% vs. 30%) than monogamous women. Because of the small amount of women who reported illness, there was not enough power to establish statistical significance in these differences. There was no effect of marital rank (senior versus junior co-wives).
Widows were more likely than married women to report illness symptoms, yet fewer of them sought outside treatment (45%). More widows than married women made therapeutic decisions themselves (85%); more attributed their illness to old age (28%), and fewer reported illnesses related to reproductive health (4%). The differences between widows and married women were almost certainly confounded by age; however, low numbers precluded tests of significance.
Social composite scores
Controlling for age, a one-quartile increase in household wealth index was associated with an 18% decrease in the odds of reporting an illness in the past 3 months (OR=.82, p < .10). Household wealth was not associated with the likelihood of seeking outside treatment. Neither social power nor social network was significantly associated with any illness-related outcomes (odds of illness, outside treatment sought).
IV. Social support during illness
A normative pattern of social connectedness during a woman's illness emerged from our interviews. According to social norms, a sick woman's husband should mobilize his resources and those of his extended kin to help cover expenses; her co-wives, sisters- and daughters- in law should step in to assist with domestic work and childcare, with older daughters helping as well; her husband and grown sons and a trusted friend should provide advice; and her friends, neighbors and extended family should visit her.
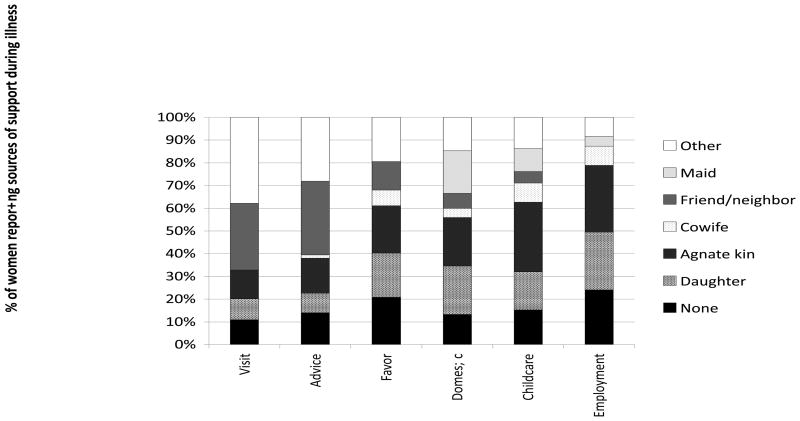
However, in the quantitative questionnaires probing recent illness experiences, husbands were rarely named as a source of support, even though women cited their husbands as the major decision-makers in their care (Figure 1). Between 10% and 20% of women received no support. While sons provided some advice, daughters provided help with forms of work, highlighting a gendered division of labor even in childhood. Sisters provided minimal support.
Figure 1.
Sources of support reported by HISSS women during illness for different social and economic needs.
Only 21% of polygynous women cited their co-wives as sources of support during illness in the quantitative data. Common were such responses in the qualitative data as, “Each co-wife does her house chores separately, we do not overlap. In the absence of a girl aged 10 or 12, or another family member or a servant, each must do all her work herself” (45, polygynous, 3 children). Latent conflict emerged around fertility issues: “If my co-wife helped me with domestic work while I was sick in the beginning stages of my pregnancy, it is because I was sick and for no other reason” (41, polygynous, 3 children). Similarly, “My illness is difficult for me because my co-wife has 6 children while I have only 3. It is because I have been infertile, I think because of family planning injections” (32, polygynous, 3 children).
In contrast to their relationships with their co-wives, many women developed friendships with their sisters-in-law: “My friend is married to my husband's brother. We don't want each other to make any other friends, that would destabilize our current harmonious relationship” (19, monogamous, 1 child).
In general, women cited female in-laws as major sources of assistance during illness, and as major determinants of their experiences in their husbands' extended households: “I get along well with my mother-in-law because she considers that everything that her son earns goes to me” (34, monogamous, 4 children).
As expected, widows reported increased strains, including financial concerns and diminished social standing and social support. “When I was married, my husband was a truck driver, and I sold eggs and other products between Abidjan and Bamako. He died three years ago, and I do not go out at all, I live with my parents and my two children” (48, widowed, 2 children). A 41-year-old widow, who had one child, stated: “I lost my husband in an accident. We have two daughters but I lost one. Now I only have one daughter, but her eyes have been ruined, so I must do all my work myself. There is no one to help me.”
In turn, some women attributed their health problems to their widowhood: “I have had diabetes for months. This arose because of my worries and fatigue from feeding my children, because their father died very young […] So I must do all kinds of things to support [them]” (61, widowed, 6 children).
Interestingly, many women expressed weariness at extending their social networks to unrelated women. “I don't need a friend. I have my daughters. Having a friend doesn't do you any good and doesn't get your anywhere. You are just going to fight” (55, polygynous, 6 children). Similarly, “I am afraid of having a friend. They will steal your husband. In Bamako friends are very dangerous” (24, monogamous, 2 children).
Women stated that the rules governing social behavior in Bamako were different from rural areas: “I came from my village to Bamako; I am afraid of having a friend here” (32, monogamous, 5 children). Some sought friends from women in positions of social power. “When I came from my village to this neighborhood, the only woman who reached out to me is the wife of the chef de quartier, she is older than me but I esteem her and she is now my friend” (56, widowed, 8 children).
In addition to their social relationships, women described their ability to maintain independent incomes as critical during illness and health. Approximately 60% of married women reported remunerative activities on the quantitative questionnaires. “I am a trader and I go to the Ivory Coast to purchase merchandise; while I am away my maid does everything for me” (40, polygynous, 4 children). Women often relied on their husbands for seed money: “To start a small business, one requires an initial investment; without this, one cannot start one's own business” (31, monogamous, 5 children). Thus, “Since I got married, my husband has not allowed me to do commerce” (27, monogamous, 2 children). Therefore, a high onus was placed on in-laws who bolstered women to continue income-generating activities during their illnesses, and who defended their autonomy to do so vis-à-vis their husbands.
Discussion
In this study, our primary goal was to examine the role of marital and social factors on the pregnancy and therapeutic trajectories of women living in urban Mali. In order to paint a nuanced picture of the social and household context that may influence women's health-related itineraries and outcomes, we devised three composite indices, based on reported sources of social power and support in our community. In contrast to prior studies (Adams et al., 2002; Madhavan, 2002; Madhavan & Adams, 2003; Simon et al., 2002), we did not use a continuous score but instead incorporated both inductive variables (e.g. the social status derived from having produced a son) as well as deductive variables borne out during our preliminary interviews (e.g. having a daughter in the household able to help). Additionally, we examined their effect during discrete, key events (pregnancy and illness). We demonstrate that these variables do significantly capture variability in contraceptive knowledge and odds of reporting an illness. When applied to a local setting, such composite scores may help guide culturally informed quantitative research in social networks.
Pregnant women reported minimal variability in healthcare seeking behaviors: most women aged 40 or under reported a pregnancy in the prior 2 years, and most used prenatal services. Women were most often escorted to their deliveries by their mothers-in-law, with whom harmonious relationships are essential in a patrilocal society. Although escort to delivery may represent only one form of support by husbands during pregnancy (Maman et al., 2011), our finding that polygynous women were less likely to be escorted to their delivery by their husbands or their agnates, is consistent with reports of emotional aloofness between spouses in polygynous families (Draper, 1989; Orubuloye et al., 1997), which may have important implications for communication about family planning and reproductive symptoms. Interestingly, an increase in the household wealth index also increased likelihood of husband and agnates escorting women to delivery, perhaps reflecting either aspects of the conjugal bond or time allocation in wealthier households. While prior studies have suggested that some older polygynous women may experience sexual abandonment by their husbands in favor of younger co-wives (reviewed in (Bove & Valeggia, 2009), we found no association between marital type and percentage of women 40 years and older reporting a pregnancy in the prior two years.
Our findings about contraception echo focused studies of contraceptive use in West African societies, that have highlighted (1) reluctance on the part of husbands to endorse contraception, both because of high fertility goals and because it is seen as an indicator of female infidelity; (2) significant misconceptions around contraceptive use, and in particular fears of the social consequences of side effects such as menstrual disruption (Castle, 2003); and (3) women's willingness to adopt contraception when it supports cultural notions that women should begin to “rest” with age, eventually retiring from childbearing in favor of caring for grandchildren (Bledsoe et al., 1998).
During illness, social composite variables did appear to play a role. The odds of reporting an illness did not only increase with age (and consequent age-associated decline in immune, musculoskeletal and cardiovascular function), but declined with household wealth index. This may be due to improved sanitation measures or nutrition. With respect to marital status, polygynous and monogamous women reported similar frequency of symptoms, health care access, and social support. Widows reported more symptoms, and were less likely to seek treatment. This is consistent with studies of Nigerian widows reporting many symptoms as well as financial hardship and poor support (Ogungbamila & Adeyanju, 2010; Onadeko et al., 2002). Overall, in an urban setting with proximity to health care, our findings suggest that despite strong cultural norms of interpersonal assistance and support, finances may play a stronger role than social factors in determining therapeutic trajectories (Abor et al., 2011; Ahmed et al., 2010; Okolo et al., 2011; Peters et al., 2008).
Despite ideals of broader intra-household support, women reported that the bulk of help received came from their daughters and other female relatives by marriage. This confirms the important managerial role of older women in regulating social and labor dynamics within households, and the power of mothers-in-law in affecting women's daily lives. Only one quarter of polygynous women reported that their co-wife was a significant source of support; this is in contrast to a commonly cited advantage of polygyny for women, that co-wives help one another during illness and pregnancy (Tabi et al., 2010). Additionally, husbands and sons played a limited role, pointing to a gendered division of labor and social support (Shelton & John, 1996; Taylor et al., 1996).
The primary limitation of this study is that the data were obtained one decade ago, a decade of social progress with respect to female education and employment opportunities. However, some major mediators of social structure, such as polygyny, persist despite broad social changes. Poverty persists; marriage remains normative; female education remains low, and polygyny remains a facet of life in urban Mali.
Therefore, we argue the data provided here remain pertinent and informative for broad swaths of women. Second, this study was cross-sectional and retrospective in design, and relied on recall. Although we attempted to limit this to a 3-month period for illness histories, prospectively gathered data on a cohort of women would be of great benefit. Longitudinal studies that follow women across illness events, prospectively documenting symptoms, sources of social support and stressors, would provide more modulated data and would help to further disentangle the impact of social mediators of women's health.
This study adds to the understanding of the powerful ways in which women's households, marriages, social networks, and their ability to exert social power within these structures, influence their general and reproductive health. A comparison of our data to EDSM showed that our subjects were representative of women in urban Bamako. Our composite scores were predictive of health events, and our mixed methods approach enhanced our ability to interpret quantitative findings. While resort to biomedical care was fairly uniform in our sample, our mixed methods nonetheless allowed us to identify socially vulnerable groups that might be specifically targeted with health interventions, and to provide a nuanced understanding of the factors, beyond income and access to care, which may influence women's health outcomes in sub-Saharan Africa.
Research Highlights.
In urban Mali, important social mediators of women's health include marital status and type, social network and power.
Women with lower household wealth index are more likely to report an illness in the preceding three months.
Polygyny is negatively associated with support by husbands during pregnancy and with use of contraception.
Partially due to their age, widows report higher frequency of illness and resort less often to biomedical care.
These findings highlight the need to target widows and pregnant polygynous women as potentially vulnerable subgroups.
Acknowledgments
The authors are indebted to the respondents who provided their time and insights for this study. They wish to thank researchers and staff at the CERPOD (Centre d'Etudes et de Recherches sur la Population pour le Développement) including Drs. Rene Dala, Mouhamadou Gueye, Issa Guindo, Mamadou Kani Konate, and Alpha Toure; the following interviewers: Hawa Bouare, Aminata Fongoro, Aissata Timbely and Yaye Toure; Drs Sarah Castle, Eduardo Fernandez-Duque and Sangeetha Madhavan for their advice; and anonymous reviewers for their constructive comments. This research was supported by the Fulbright Organization.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Riley M Bove, Email: rbove@partners.org.
Emily Vala-Haynes, Email: evala@sas.upenn.edu.
Claudia Valeggia, Email: valeggia@sas.upenn.edu.
References
- Abor PA, Abekah-Nkrumah G, Sakyi K, Adjasi CKD, Abor J. The socio-economic determinants of maternal health care utilization in Ghana. International Journal of Social Economics. 2011;38:628–648. [Google Scholar]
- Adams AM, Madhavan S, Simon D. Women's social networks and child survival in Mali. Social Science & Medicine. 2002;54:165–178. doi: 10.1016/s0277-9536(01)00017-x. [DOI] [PubMed] [Google Scholar]
- Adeokun LA, Nalwadda RM. Serial marriages and AIDS in Masaka District. Health transition review: the cultural, social, and behavioural determinants of health. 1997;7(Suppl):49–66. [PubMed] [Google Scholar]
- Agot KE, Vander Stoep A, Tracy M, Obare BA, Bukusi EA, Ndinya-Achola JO, et al. Widow inheritance and HIV prevalence in Bondo District, Kenya: baseline results from a prospective cohort study. PloS one. 2010;5:e14028. doi: 10.1371/journal.pone.0014028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmed S, Creanga AA, Gillespie DG, Tsui AO. Economic status, education and empowerment: implications for maternal health service utilization in developing countries. PloS one. 2010;5:e11190. doi: 10.1371/journal.pone.0011190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beyeza-Kashesy J, Neema S, Ekstrom AM, Kaharuza F, Mirembe F, Kulane A. “Not a boy, not a child”: A qualitative study on young people's views on childbearing in Uganda. African journal of reproductive health. 2010;14:71–81. [PubMed] [Google Scholar]
- Bila B, Egrot M. Gender asymmetry in healthcare-facility attendance of people living with HIV/AIDS in Burkina Faso. Social science & medicine. 2009;69:854–861. doi: 10.1016/j.socscimed.2009.05.035. [DOI] [PubMed] [Google Scholar]
- Bledsoe C, Banja F, Hill AG. Reproductive mishaps and western contraception: an African challenge to fertility theory. Population and Development Review. 1998;241:15–57. [Google Scholar]
- Bove R, Valeggia C. Polygyny and women's health in sub-Saharan Africa. Social science & medicine. 2009;68:21–29. doi: 10.1016/j.socscimed.2008.09.045. [DOI] [PubMed] [Google Scholar]
- Campbell EK, Campbell PG. Family size and sex preferences and eventual fertility in Botswana. Journal of biosocial science. 1997;29:191–204. doi: 10.1017/s0021932097001910. [DOI] [PubMed] [Google Scholar]
- Castle S. Factors influencing young Malians' reluctance to use hormonal contraceptives. Studies in Family Planning. 2003;34:186–199. doi: 10.1111/j.1728-4465.2003.00186.x. [DOI] [PubMed] [Google Scholar]
- Chapoto A, Jayne TS, Mason NM. Widows' land security in the era of HIV/AIDS: panel survey evidence from Zambia. Economic development and cultural change. 2011;59:511–547. doi: 10.1086/658346. [DOI] [PubMed] [Google Scholar]
- Commeyras C, Ndo JR, Merabet O, Kone H, Rakotondrabe FP. Household behaviour regarding health and drug consumption in Cameroon. Sante. 2006;16:5–12. [PubMed] [Google Scholar]
- Creswell JW. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches. Third. Los Angeles: Sage; 2008. [Google Scholar]
- Davhana-Maselesele M. “Why did this happen to me?” Experiences of widowhood among the Vhavenda in Limpopo Province. Curationis. 2005;28:15–24. [PubMed] [Google Scholar]
- Donkor ES, Sandall J. The impact of perceived stigma and mediating social factors on infertility-related stress among women seeking infertility treatment in Southern Ghana. Social science & medicine. 2007;65:1683–1694. doi: 10.1016/j.socscimed.2007.06.003. [DOI] [PubMed] [Google Scholar]
- Draper P. African marriage systems: perspectives from evolutionary ecology. Ethology and Sociobiology. 1989;10:145–169. [Google Scholar]
- Gibson MA, Mace R. Polygyny, reproductive success and child health in rural Ethiopia: why marry a married man? Journal of biosocial science. 2007;39:287–300. doi: 10.1017/S0021932006001441. [DOI] [PubMed] [Google Scholar]
- Gureje O, Ogunniyi A, Kola L, Abiona T. Incidence of and risk factors for dementia in the Ibadan study of aging. Journal of the American Geriatrics Society. 2011;59:869–874. doi: 10.1111/j.1532-5415.2011.03374.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gyimah SO. Polygynous marital structure and child survivorship in sub-Saharan Africa: some empirical evidence from Ghana. Social science & medicine. 2009;68:334–342. doi: 10.1016/j.socscimed.2008.09.067. [DOI] [PubMed] [Google Scholar]
- Haddad H, Hoddinott J, Alderman H. Intrahousehold allocation in developing countries: Models, methods and policy. Baltimore: Johns Hopkins University Press; 1997. [Google Scholar]
- Ice GH, Heh V, Yogo J, Juma E. Caregiving, gender, and nutritional status in Nyanza Province, Kenya: grandmothers gain, grandfathers lose. American journal of human biology: the official journal of the Human Biology Council. 2011;23:498–508. doi: 10.1002/ajhb.21172. [DOI] [PubMed] [Google Scholar]
- Jankowiak W, Sudakov M, Wilreker BC. Co-wife conflict and co-operation. Ethnology. 2005;44:81–98. [Google Scholar]
- Lesthaeghe R, Kaufmann G, Meekers D. The nuptiality regimes in sub-Saharan Africa. In: Lesthaeghe R, editor. Reproduction and social organization in sub-Saharan Africa. Berkeley: University of California Press; 1989. pp. 238–337. [Google Scholar]
- Lopman BA, Nyamukapa C, Hallett TB, Mushati P, Spark-du Preez N, Kurwa F, et al. Role of widows in the heterosexual transmission of HIV in Manicaland, Zimbabwe, 1998-2003. Sexually transmitted infections. 2009;85(1):i41–48. doi: 10.1136/sti.2008.033043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ly M, Diop S, Sacko M, Baby M, Diop CT, Diallo DA. Breast cancer: factors influencing the therapeutic itinerary of patients in a medical oncology unit in Bamako (Mali) Bulletin du cancer. 2002;89:323–326. [PubMed] [Google Scholar]
- Madhavan S. Best of friends and worst of enemies: competition and collaboration in polygyny. Ethnology. 2002;41:69–84. [Google Scholar]
- Madhavan S, Adams A. Women's networks and the social world of fertility behavior. International family planning perspectives. 2003;29:58–68. doi: 10.1363/ifpp.29.058.03. [DOI] [PubMed] [Google Scholar]
- Maman S, Moodley D, Groves AK. Defining male support during and after pregnancy from the perspective of HIV-positive and HIV-negative women in Durban, South Africa. Journal of midwifery & women's health. 2011;56:325–331. doi: 10.1111/j.1542-2011.2011.00029.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcoux R, Marin R, Ouédraogo D, Gingras L. L'Insertion residentielle à Bamako. In: Piche V, Ouedraogo OD, editors. L'Insertion urbaine à Bamako. Paris: Karthala; 1995. pp. 75–106. [Google Scholar]
- Mbassa Menick D, Sylla O. Marital conflict in Senegal: an anguished plea from the women. Medecine tropicale: revue du Corps de sante colonial. 1996;56:423–429. [PubMed] [Google Scholar]
- McTavish S, Moore S, Harper S, Lynch J. National female literacy, individual socio-economic status, and maternal health care use in sub-Saharan Africa. Social science & medicine. 2010;71:1958–1963. doi: 10.1016/j.socscimed.2010.09.007. [DOI] [PubMed] [Google Scholar]
- Millman SR, Potter RG. The fertility impact of spousal separation. Studies in Family Planning. 1984;15:121–126. [PubMed] [Google Scholar]
- Ogungbamila B, Adeyanju AB. Health and psychosocial complaints of elderly Ijaw widows in Yenagoa, Nigeria. Gerontology. 2010;56:200–207. doi: 10.1159/000251713. [DOI] [PubMed] [Google Scholar]
- Okolo CO, Reidpath DD, Allotey P. Socioeconomic inequalities in access to health care: examining the case of Burkina Faso. Journal of health care for the poor and underserved. 2011;22:663–682. doi: 10.1353/hpu.2011.0039. [DOI] [PubMed] [Google Scholar]
- Onadeko MO, Lawoyin T, Amodu MO, Ejikeme C, Dairo MD. Problems of widowhood: a study of widows in a tertiary institution in Ibadan, south west Nigeria. African journal of medicine and medical sciences. 2002;31:201–206. [PubMed] [Google Scholar]
- Orubuloye IO, Caldwell JC, Caldwell P. Perceived male sexual needs and male sexual behavior in Southwest Nigeria. Social Science & Medicine. 1997;44:1195–1207. doi: 10.1016/s0277-9536(96)00254-7. [DOI] [PubMed] [Google Scholar]
- Ouendo EM, Makoutode M, Paraiso MN, Wilmet-Dramaix M, Dujardin B. Therapeutic itinerary of poor patients in Benin (poverty and health care) Tropical medicine & international health: TM & IH. 2005;10:179–186. doi: 10.1111/j.1365-3156.2004.01371.x. [DOI] [PubMed] [Google Scholar]
- Peters DH, Garg A, Bloom G, Walker DG, Brieger WR, Rahman MH. Poverty and access to health care in developing countries. Annals of the New York Academy of Sciences. 2008;1136:161–171. doi: 10.1196/annals.1425.011. [DOI] [PubMed] [Google Scholar]
- Pick WM, Obermeyer CM. Urbanisation, household composition and the reproductive health of women in a South African city. Social science & medicine. 1996;43:1431–1441. doi: 10.1016/0277-9536(96)00035-4. [DOI] [PubMed] [Google Scholar]
- Sahel DId. Profil socio-demographique au Mali 2004 [Google Scholar]
- Selman LE, Higginson IJ, Agupio G, Dinat N, Downing J, Gwyther L, et al. Quality of life among patients receiving palliative care in South Africa and Uganda: a multi-centred study. Health and quality of life outcomes. 2011;9:21. doi: 10.1186/1477-7525-9-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shayo GA, Mugusi FM. Prevalence of obesity and associated risk factors among adults in Kinondoni municipal district, Dar es Salaam Tanzania. BMC public health. 2011;11:365. doi: 10.1186/1471-2458-11-365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shelton BA, John W. The division of household labor. Annual Review of Sociology. 1996;22:299–322. [Google Scholar]
- Simon D, Adams AM, Madhavan S. Women's social power, child nutrition and poverty in Mali. Journal of biosocial science. 2002;34:193–213. doi: 10.1017/s0021932002001931. [DOI] [PubMed] [Google Scholar]
- Tabi MM, Doster C, Cheney T. A qualitative study of women in polygynous marriages. International nursing review. 2010;57:121–127. doi: 10.1111/j.1466-7657.2009.00762.x. [DOI] [PubMed] [Google Scholar]
- Taylor L, Seeley J, Kajura E. Informal care for illness in rural southwest Uganda: the central role that women play. Health Transition Review. 1996;6:49–56. [PubMed] [Google Scholar]
- Uthman OA, Lawoko S, Moradi T. The role of individual, community and societal gender inequality in forming women's attitudes toward intimate-partner violence against women: a multilevel analysis. World health & population. 2010;12:5–17. doi: 10.12927/whp.2010.22007. [DOI] [PubMed] [Google Scholar]
- Vaessen M, Thiam M, Le T. Household Sample Surveys in Developing and Transition Countries. New York: United Nations, Department of Economic and Social Affairs, Statistics Division; 2005. The Demographic and Health Surveys; pp. 495–518. [Google Scholar]
- van de Walle E. African households: Censuses and surveys. General Demography of Africa Series 2005 [Google Scholar]
- WHO. Pregnancy, childbirth, postpartum and newborn care - A guide for essential practice: World Health Organization. Department of Making Pregnancy Safer; 2006. [PubMed] [Google Scholar]
- Wittrup I. Me and my husband's wife: an analysis of polygyny among Mandinka in the Gambia. Folk. 1990;32:117–141. [Google Scholar]