Abstract
The efficacy and safety of plague vaccines based on the modified vaccinia Ankara (MVA) viral vector was evaluated. MVA recombinants were constructed expressing Yersinia pestis antigens under the translational control of the encephalomyocarditis virus (EMCV) internal ribosomal entry site (IRES) and/or fused to the tissue plasminogen activator (tPA) secretory signal. A MVA/Y. pestis recombinant that expressed a truncated version of the low-calcium response V antigen (MVA/IRES/tPA/V307), conferred significant protection (87.5%–100%) against intranasal or intraperitoneal challenge with CO92 (encapsulated) or Java 9 (non-encapsulated) strains of Y pestis, respectively. In contrast, a MVA/Y. pestis recombinant that expressed the full-length V antigen provided only 37.5% protection against challenge with CO92 or Java 9 strains, respectively. Interestingly, a MVA/Y. pestis recombinant that expressed the capsular protein (F1) did not elicit significant antibody titers but still conferred 50% and 25% protection against CO92 or Java 9 challenge, respectively. The MVA/Y. pestis recombinant viruses did not demonstrate any mortality or morbidity in SCID mice. Based on their safety and efficacy in mice, these MVA/Y. pestis recombinants are candidates for further development as biodefense and public health vaccines.
Introduction
Plague is primarily a disease of wild rodents transmitted by fleas, but it can also afflict humans, domestic pets, and wild animals [1, 2]. The disease has devastated human and animal populations throughout history. In recent years, Y. pestis, the causative agent of plague, has caused severe epidemics in many parts of the world, resulting in human deaths and severe economic losses [3-5]. Yersinia pestis is widespread throughout wild rodent populations in the southwestern United States, Southeast Asia, Eastern Europe, central and southern Africa, as well as in South America, and human populations in these areas are highly susceptible [6-9]. In the United States, plague has spread throughout the Western states, causing significant mortality in wild rodents [10]. Domestic cats are also susceptible to Y. pestis infections, and were identified as the main source of infection in many recent cases of human plague in the western states of the United States [11]. The emergence of multi-antibiotic resistant Y. pestis strains [12, 13] and the ability of Y. pestis to spread from person to person via inhalation of aerosolized infectious droplets [1, 2] heighten the public health concern. Because of the pathogenicity of the pneumonic form of the disease and its potential for human-to-human transmission, Y. pestis also is considered a potential bioweapon [14, 15]. Therefore, there is an immediate need for novel vaccines that can protect troops, medical and first-responder personnel from the threat of a Y. pestis bioweapon, that can limit the spread of disease by vaccination of individuals at risk after a bioterrorist attack, and that can limit disease outbreaks in endemic countries and in future epidemics [14, 15].
In recent years the development of novel plague vaccines has been the focus of extensive research, because the commercially licensed vaccines based on heat or formaldehyde killed suspension of Y. pestis, were found unsafe, require multiple immunizing doses [16, 17] and their production requires microbial culture within containment which is costly and hazardous. Current efforts have centered on the development of subunit vaccines using Y. pestis fraction 1 (F1) and the low calcium response virulence (V) antigens [16]. The capsular F1 (17.5 kDa) and V (35 kDa) antigens are natural virulence factors produced by Y. pestis [18, 19]. Both antigens target innate immune responses required to control bacterial spread at the early stages of infection. The F1 antigen renders wild-type organisms resistant to uptake by phagocytes [20]. While F1-based vaccines are immunogenic, they do not protect against naturally occurring non-encapsulated strains of Y. pestis [21]. The secreted V antigen plays an important role in the delivery of other Yersinia outer proteins (Yops) and stimulates the secretion of IL-10 (an anti-inflammatory cytokine) associated with the suppression of endogenous IL-12, TNF-α and IFN-γ, a hallmark of plague [22]. A short deletion within the V antigen (variant lacking amino acid residues 271-300) abrogated its immunosuppressive effect and this truncated V antigen elicited immune responses that protected mice and non-human primates against a lethal challenge with Y. pestis [23]. Administration of the F1 and V antigens alone, mixed, or delivered as a recombinant fusion protein elicits a strong immune response and protects against challenge with Y. pestis [24-26]. The F1-V fusion protein formulated with aluminum hydroxide provides protection against aerosolized or injected plague challenge in mice [25, 27, 28] and is being tested in human clinical trials [29]. However, antigens mixed with alum are not suitable for freezing, lyophilization or mucosal administration. The Yersinia outer proteins (Yops) are necessary for virulence [30], and have been tested as candidate vaccines [31, 32]. Vaccination with YopD provided significant protection against challenge with non-encapsulated Y. pestis strains [32].
An alternative approach in the development of plague vaccines is the use of live attenuated bacterial and viral vectors [26, 33-36]. Oral administration of attenuated Salmonella expressing F1 and/or V antigens protected mice against subcutaneous and intranasal challenge [26, 36]. A single intramuscular vaccination with adenovirus expressing V antigen also protected mice against intranasal challenge for at least 6 months [35]. A combination of raccoon pox (RCN) virus constructs expressing F1 and V (V307) antigens protect mice and prairie dogs against lethal plague [37-40]. In these studies, we also demonstrated that a vaccine containing the internal ribosomal entry site (IRES) from encephalomyocarditis virus (EMCV) and secretory signal of tissue plasminogen activator (tPA), significantly enhanced the expression levels of F1 in a recombinant RCN-based vaccine [37-40]. This vaccine was shown to fully protect mice against intradermal challenge with Y. pestis [37-40]. However, the RCN-plague vaccines have not been extensively characterized and are not suitable for use in humans. Another poxvirus, the modified vaccinia Ankara (MVA), was originally tested in over 120,000 individuals and proved to be a safe and effective vaccine against smallpox [41]. Recombinant MVA vaccine candidates have been shown to induce protective humoral and cellular immunity against diseases caused by viruses, bacteria, parasites, or tumors from which the antigens were derived [42-47]. Additional features that make MVA a desirable vector for a plague vaccine include its ability to induce protective immune responses when administered by different routes and its genetic and physical stability properties [48, 49].
In these studies, we evaluated the suitability of MVA as a vector to express Y. pestis F1 and V antigens. The effect of ECMV IRES in combination with the secretory signal of tPA on the immunogenicity and efficacy of MVA-based plague vaccines was examined. In addition, the safety of MVA-plague recombinants in severe combined immune deficient (SCID) BALB/c mice was tested. Our findings demonstrated that a recombinant MVA virus expressing a truncated form of Y. pestis V antigen in the presence of the IRES and tPA (MVA/IRES/tPA/V307) provided increased immunogenicity, safety, and protection against challenge with different strains of Y. pestis in mice.
Materials and Methods
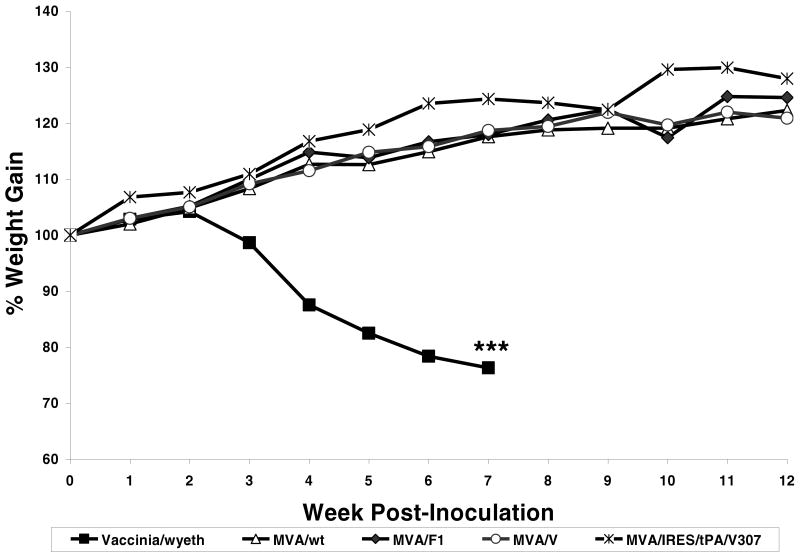
Construction of MVA recombinant vaccines
The transfer plasmid pdIIIGFP (kindly provided by Dr Joanna Shisler, University of Illinois) was used to generate recombinant MVA expressing Y. pestis antigens. This plasmid contained: 1) DNA segments (flank 1 and flank 2) adjacent to deletion III within the HindIII A fragment of MVA, 2) a strong synthetic early/late (SEL) vaccinia virus promoter upstream to a multiple cloning site (MCS), and 3) the green fluorescent protein (GFP) gene under the control of a divergent SEL promoter (Figure 1). A second transfer plasmid, pdIIIGFP/IRES/tPA, containing the ECMV IRES sequence followed by the tPA secretory signal was generated by insertion of an IRES/tPA cassette into pdIIIGFP. Expression cassettes for each of the Y. pestis antigens, F1, full lengthV and V truncated at aa 307 (V307), were inserted into pdIIIGFP or pdIIIGFP/IRES/tPA. Expression cassettes were generated by PCR (Table 1) to contain appropriate restriction sites for insertion into pdIIIGFP or pdIIIGFP/IRES/tPA. The PCR products were cloned into the MCS of pdIIIGFP or pdIIIGFP/IRES/tPA and the resulting plasmids were designated as pdIIIGFP/F1, pdIIIGFP/IRES/tPA/F1, pdIIIGFP/V, pdIIIGFP/IRES/tPA/V, pdIIIGFP/V307 and pdIIIGFP/IRES/tPA/V307.
Figure 1. Construction of recombinant MVA-plague viruses.
Expression cassettes were generated by PCR for each of the Y. pestis antigens, F1, V and V307 as described in the materials and methods. The cassettes were cloned into either the pdIIIGFP or pdIIIGFP/IRES/tPA vectors and the resulting plasmids were designated as pdIIIGFP/F1, pdIIIGFP/IRES/tPA/F1, pdIIIGFP/V, pdIIIGFP/IRES/tPA/V, pdIIIGFP/V307 and pdIIIGFP/IRES/tPA/V307. Homologous recombination into MVA was successfullycompleted and recombinant MVA/Y. pestis viruses were identified by GFP expression.
Table 1. Yersinia pestis antigen PCR primer sequences.
| Primer | PCR Primer Sequencea | RE Site |
|---|---|---|
| 5′ F1/IRES/tPA | 5′-cgcgcGTCGACgaggtaatatatgaaaaaaatcag-3′ | Sal I |
| 5′ F1 | 5′-gtgaGTCGACatgaaaaaaatcagttccgttatc-3′ | Sal I |
| 3′ F1 | 5′-gcGAATTCttattggttagatacggttacggt-3′ | EcoR I |
| 5′ V | 5′-gtgaGTCGACatgattagagcctacgaacaaaacc-3′ | Sal I |
| 5′ V/IRES/tPA | 5′-tgacGCCGGCattagagcctac-3′ | NgoM IV |
| 3′ V | 5′-cgcGAATTCtcatttaccagacgtgtcatc-3′ | EcoR I |
| 3′ V307 | 5′-gcGAATTCtcaacggttcagtgcttcaatag-3′ | EcoR I |
Restriction enzyme sites are capitalized.
Recombinant MVA-plague viruses were generated as described elsewhere [50, 51]. Briefly, chicken embryo fibroblasts (CEF) produced in house [52, 53], were infected with wild type MVA at a multiplicity of 0.05 and one hour (h) later the cells were transfected with each of the transfer vectors using Lipofectamine™ (Invitrogen, Carlsbad, CA). At 48 – 72 h post-transfection, monolayers were harvested, centrifuged at 500 RCF for 5 minutes at 4°C and cells disrupted by freeze-thaw and sonication (2 times for 15 seconds using a Virtis600 at setting 3). The disrupted cell extracts containing possible recombinant viruses expressing GFP were plated onto fresh CEF cells and overlaid with 0.8% agarose. After 48 – 72 h, recombinant virus-generated plaques were detected by fluorescence and picked into media with a glass pipette. The cell/virus samples were sonicated and plated as described above. After three consecutive rounds of plaque isolation, high titer virus stocks were prepared in CEF cells for subsequent in vitro and in vivo characterization.
In vitro expression of Y. pestis antigens
The in vitro expression of recombinant MVA viruses containing the F1, V, V307 or IRES/tPA/F1, IRES/tPA/V, IRES/tPA/V307 antigens was determined by immuno-blot analyses. CEF or Vero cells were plated into 6-well plates and infected with the recombinant MVA/F1, MVA/IRES/tPA/F1, MVA/V, MVA/IRES/tPA/V, MVA/V307 or MVA/IRES/tPA/V307 viruses at an MOI of 0.5 or 5, respectively in serum free conditions. At 48 h post-infection, the infected cells were harvested in the presence of a protease inhibitor cocktail (Mini Protease tabs, Roche Diagnostics, Indianapolis, IN), washed, resuspended in 1X loading buffer and heated to 95°C for 5 min. The supernatants from the infected cells were centrifuged and concentrated by ultrafiltration with a 3 kDa cutoff membrane (Nanosep 3K Omega, Pall, Inc., East Hills, NY). The supernatants were then combined with an equal volume of 2X loading buffer and heated to 95°C for 5 min. Supernatant and cell samples were resolved by SDS Polyacrylamide gel electrophoresis (SDS-PAGE) and transferred to a nitrocellulose membrane for immuno-blot analysis using polyclonal rabbit anti-F1 or anti-V serum produced in-house. The polyclonal antibodies were generated by inoculating specific pathogen free (SPF) rabbits with purified F1 (from caf1 operon expression system) or V (ATCC, BEI Resources, Manassas, VA, cat# NR-3832) proteins. These antibodies showed minor background to MVA wild type expressed from CEF or Vero when used in immunoblot analyses.
The F1 glycosylation state was analyzed using a protein deglycosylation enzyme mix (New England Biolabs (NEB), Ipswich, MA, cat# P6039S). Briefly, Vero and CEF cells were infected with MVA/F1 or MVA/IRES/tPA/F1 and harvested as previously described in the materials and methods. The cell pellets were suspended in 30 μL H2O, and the concentrated supernatants were processed following the manufacturer’s instruction. The re-suspended cell pellet and concentrated supernatant were denatured for 10 minutes at 100°C. After denaturation, the samples were treated with NEB deglycosylation enzyme cocktail and incubated at 37°C for 4 h. This was followed by western blot analysis using the polyclonal rabbit anti-F1 serum.
Yersinia pestis cultures
Preparation of Y. pestis cultures and subsequent animal challenge experiments were conducted in a BSL3 laboratory and animal facility in Madison, WI as previously described [37]. Briefly, to prepare a working stock, 75 μL of the frozen Y. pestis isolate was thawed, vortexed, spread onto blood agar plates (Remel, Lenexa, KS), and incubated at 28°C for 48 h. The bacterial lawn was scraped from the agar plates into 200 ml Heart Infusion Broth (Difco Laboratories, Detroit, MI) with 0.2% xylose and incubated at 28°C for 48 h. Final stocks were prepared by adding 20% glycerol to the broth culture (v/v) and were stored in aliquots at −80°C. The bacterial strains CO92 and Java 9 of Y. pestis were kindly provided by Dr. Arthur Friedlander and Dr. Mark Wolcott, respectively (US Army Medical Research Institute of Infectious Diseases, Fort Detrick, Frederick, MD). The F- strain of choice for these studies would have been the C12 strain; however, we had difficulty in obtaining this particular strain. Since our main objective was to evaluate the efficacy of the vaccine construct against encapsulated and non-encapsulated strains of Y. pestis, we used the F1- Java 9 that was readily available.
Immunization and Challenge
Groups of eight 4- 6 week-old female BALB/c mice (Harlan Sprague Dawley, Indianapolis, IN) received primary and booster immunizations (28 days apart) with each vaccine candidate via intramuscular injections into the hind legs. A dose of 5 X 107 plaque forming units (pfu) in 50μl was used for both injections. Control groups were immunized with either recombinant F1 protein (rF1 – 40 μg), empty MVA vector (MVA/GFP – 5 X 107 pfu) or with phosphate buffered saline (PBS – 50 μL). At two weeks post-boost, all animals were challenged with the wild-type Y. pestis CO92 strain by intranasal instillation of 10 μL (5 μL into each nostril) of inoculum containing 1 X 105 colony forming units (cfu) (35LD50) of the bacteria. Animals challenged with the Java 9 strain of Y. pestis received 100 μl inoculum containing 100 cfu (100LD50) intraperitoneally. The isolate of Java 9 used in this study was less virulent via the intranasal route but highly virulent when used intraperitoneally. Challenged animals were monitored for two weeks.
A group of eight 4 - 6 week-old naïve mice was passively immunized intraperitoneally with 100 μL of post-boost pooled serum with a titer of 100,000 from mice immunized with two doses of MVA/IRES/tPA/V307. The passively immunized mice were challenged intraperitoneally with a 100 μL inoculum containing 100 cfu (100LD50) of the Java 9 strain of Y. pestis. Challenged animals were monitored for two weeks. The stability and virulent phenotype of the Y. pestis CO92 or Java 9 frozen stock cultures were validated by testing aliquots for bacterial counts and lethal doses. The number of colony-forming units was determined by plating 100 μL of each dilution onto blood agar and incubating at 28°C for 48 h. Lethal dose (LD50) values were determined by inoculating groups of 11- 12 week-old BALB/c mice intranasally (10 μL) or intraperitoneally (100 μL) with 10-fold dilutions of the Y. pestis CO92 or Java 9 bacterial cultures, respectively. Following inoculation, animals were monitored for 14 days, mortalities were recorded and LD50 was calculated by Reed and Muench method [54].
Serology
Serum samples were collected on day 28 post-primary vaccination and day 14 post-boost (pre-challenge) to assess antibody titers against Y. pestis F1 or V antigens. Serum total IgG as well as IgG1 and IgG2a subclass titers were measured by enzyme-linked immunosorbent assay (ELISA) as described elsewhere [37]. Briefly, 96-well ELISA plates were coated with purified recombinant F1 or V antigen (0.1μg in 100 μL carbonate buffer, pH 9.6 per well) at 4°C overnight. Coated plates were washed twice with 0.05% Tween 20 in PBS (washing buffer) and rinsed with blocking buffer (1% BSA in PBS) for 1 h at room temperature (RT). Serum samples then were serially diluted from 1:100 – 1:100,000 in ELISA diluent (0.1% BSA in washing buffer) and added in triplicate to the prepared ELISA plates. Known negative and positive serum samples from mice inoculated with recombinant F1 or V antigen from previous studies were used as controls and plates were incubated for 1 h at RT. After washing, 100μL per well of a 1:10,000 dilution of horseradish peroxidase (HRP)-conjugated rabbit anti-mouse IgG (Abcam Inc, Cambridge, MA) was added to each well and incubated for 1 h at RT. Plates were washed, and 100 μL per well of tetra-methyl-benzidine (TMB) chromogen (Invitrogen, Calsbad, CA) was added to each well and incubated in the dark for 5minutes. The reaction was then stopped by adding 100 μL per well of 2mM H2S04 (Sigma, St Louis, MO). Colorimetry was assessed using a microplate reader (ELx800-BioTek, Winooski, VT) at test wavelength of 450 nm and a reference wavelength of 630nm. The highest dilution that was positive (exceeded the mean of known negative serum samples plus three standard deviations) was considered the endpoint, and its reciprocal value was recorded as the titer.
Safety of MVA-based vaccine constructs
Groups of six, five-week old BALB/c SCID mice (Harlan Sprague Dawley, Indianapolis, IN) were inoculated intraperitoneally with 1 X 108 pfu of MVA/F1 MVA/V, MVA/V307, MVA/IRES/tPA/V307 or wild type MVA (MVAwt). An additional group received 1 X 106 pfu of the vaccinia Wyeth strain via the same route. Mice were monitored daily for 3 months and their weight was recorded weekly. Mice died naturally or were euthanized when showing body-conditioning score less than two (BCS < 2) as previously described [55].
Statistical analysis
One way ANOVA was used to evaluate the vaccine group effects on pre-boost and pre-challenge antibody titers. If the vaccine group effect was statistically significant (P<0.05 by Kruskal-Wallis test), an all pair-wise comparison among groups was performed using an unadjusted P-value of 0.05. Survival analysis was performed to assess vaccine effectiveness against challenge with either CO92 or Java 9; reported P-values are from Fisher's exact test. Probability values < 0.05 were considered significant using the GraphPad Prism 5 software (La Jolla, CA) for all statistical analyses.
Results
Protein Expression
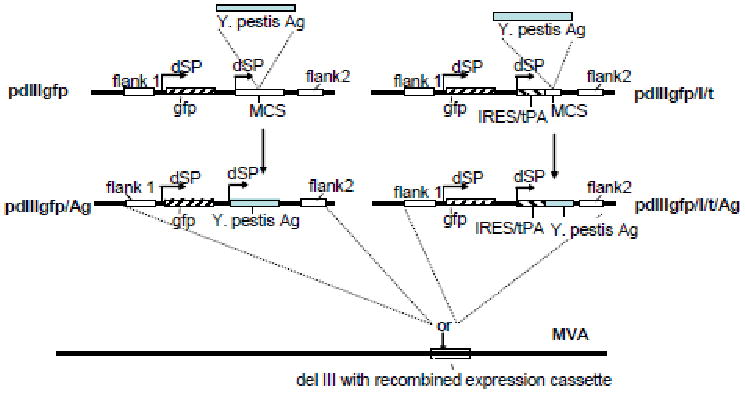
The expression of the F1, V and V307 antigens of Y. pestis was assessed by immuno-blot analyses of proteins from cells infected with the MVA/Y. pestis recombinant viruses. Expression levels were evaluated in whole cell extracts and in cell culture supernatants after infection of MVA permissive CEF cells and non-permissive mammalian Vero cells (Figure 2). Expression of the F1 protein by the MVA/F1 recombinant was detected in both the cellular pellet and cell culture supernatants. In MVA/F1 infected CEF cells, the F1 capsular antigen was observed as two lower molecular weight forms consistent with the predicted protein (approximately 18 kilodaltons, kd; predicted protein) and a higher molecular weight form at approximately 23 kd (Figure 2A). The 23 kd form was more prevalent in the cell supernatant, suggesting that it is preferentially secreted. The capsular F1 protein has one predicted N-glycosylation site and six predicted o-glycosylation sites for vertebrate cells. Thus, we postulated that the 23 kd form could represent a glycosylated protein. Indeed, deglycosylation of CEF-expressed F1 eliminated the 23 kd form and only the 18 kd form remained (Figure 2E). Higher molecular weight forms of approximately 34 kd and above also were observed in the cell pellets. These forms are consistent with dimers and other multimers; the F1 capsular protein avidly forms multimeric structures upon secretion [56, 57]. These forms were not observed upon extensive denaturation (see Figure 2E for an example). In CEF cells infected with the MVA/IRES/tPA/F1 virus, only low levels of expression of the lower molecular weight forms could be observed in the cell pellets.
Figure 2.
Western blot analysis of expression patterns from recombinant MVA-plague viruses.
Monolayers of CEF or Vero cells were transfected with recombinant MVA-plague viruses at MOI of 0.5pfu/cell. After 48 h post transfection cells were harvested and subjected to SDS-PAGE followed by western blot analysis as described in the methods. (A) F1 expression in CEF cell (c) and supernatant (s) fractions. (B) F1 expression in Vero cell (c) and supernatant (s) fractions. (C) V and V307 expression in CEF cell (c) and supernatant (s) fractions. (D) V and V307 expression in Vero cell (c) and supernatant (s) fractions.
In mammalian Vero cells infected with the MVA/F1 recombinant virus, the lower molecular weight form of 18 kd was more predominant than the 23 kd glycosylated form in both the cell pellet and the cell supernatant (Figure 2B). Again, the 23 kd form disappeared upon deglycosylation (data not shown). Higher molecular weight forms of apparent molecular weights 33, 36 and 39 kd also were detected and were relatively more prominent in the culture supernatants. In Vero cells infected with the MVA/IRES/tPA/F1 recombinant virus, only low levels of expression of the F1 antigen were detected in the cell pellets. The reduced level of expression directed by the IRES/tPA constructs is in stark contrast to similar constructs made in raccoon poxvirus [37]. In that case, IRES/tPA directed higher levels of expression and secretion in infected cells.
The expression patterns of V and V307 antigens were simpler and were similar in both infected CEF and Vero cells (Figure 2, C and D). Cells infected with either MVA/V or MVA/V307 recombinant viruses expressed a single form of approximately 36 and 35 kd, respectively, consistent with predicted sizes (37 and 35 kd). Cells infected with MVA/IRES/tPA/V expressed two molecular forms of approximately 36 and 40 kd. The higher molecular weight form was consistent with the size of tPA/V fusion and was preferentially secreted. In contrast, cells infected with the MVA/IRES/tPA/V307 recombinant virus expressed only a single form of 35 kd. The predicted V and V307 open reading frames do not encode consensus glycosylation sequences for vertebrate cells. In the case of V antigen expression, the addition of IRES/tPA only slightly reduced protein expression levels. In infected CEF cells, the ratio of secreted to cellular V antigen seemed slightly enhanced with the addition of the IRES/tPA sequence (Figure 2C). However, the ratios seemed consistent between all the constructs in infected Vero cells (Figure 2D).
Immunogenicity of MVA constructs
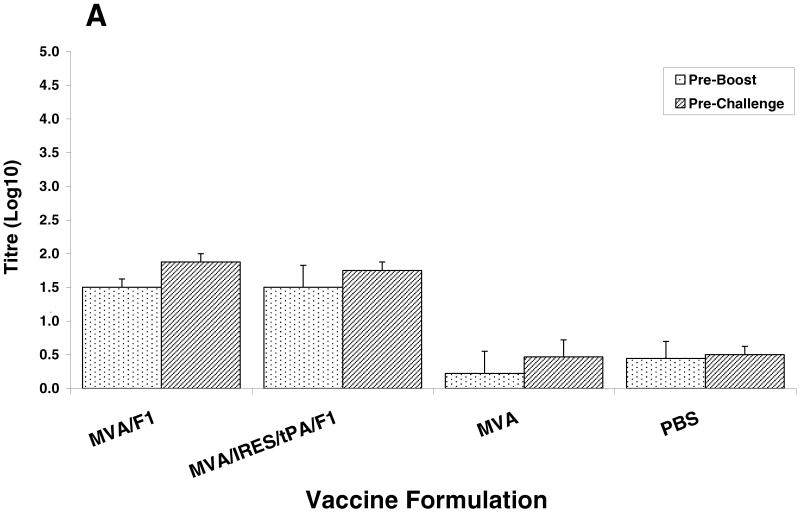
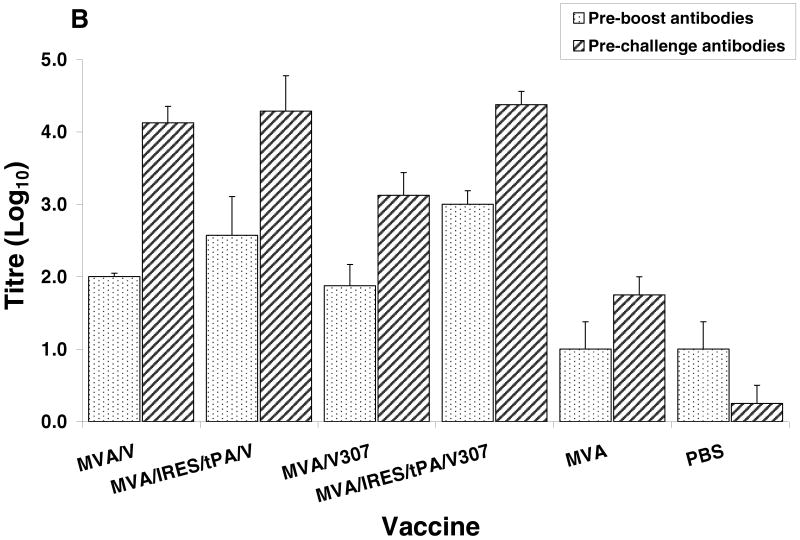
Groups of BALB/c mice were immunized intramuscularly with MVA/Y. pestis constructs encoding the F1, V or V307 antigens. Antibody titers after a single immunization (pre-boost) and after two immunizations (pre-challenge) were assessed by ELISA analysis. Pre-challenge antibody titers elicited by the MVA/V construct were significantly higher (P<0.05) than the MVA/V307 construct, however, there was no significant difference between pre-boost titers induced by these constructs (Figure 3B). The effect of the IRES and tPA sequences on immunogenicity was examined. As shown in figure 3B, expression of V307 under the control of IRES and secretory signals (MVA/IRES/tPA/V307) significantly enhanced its immunogenicity. Both pre-boost and pre-challenge antibody titers were significantly higher (P<0.05) in mice immunized with MVA/IRES/tPA/V307 than with MVA/V307. Analysis of IgG subclasses elicited by the MVA/IRES/tPA/V307 and MVA/V307 constructs showed a balanced response between IgG1 and IgG2a subclasses (data not shown). MVA constructs expressing the V antigen induced a significant booster effect (P<0.05) on antibody responses in all immunized mice as compared to primary immunization (Figure 3B). Surprisingly, no booster effect was detected in mice immunized with the MVA/F1 or MVA/IRES/tPA/F1 constructs. Moreover, pre-challenge antibody titers elicited by the MVA/F1 or MVA/IRES/tPA/F1 constructs were significantly lower (P>0.05) than titers induced by constructs expressing the V antigen (Figure 3A and 3B).
Figure 3.
Immune responses to MVA-plague vaccines in mice.
Groups of eight 4-6 week-old BALB/c mice were vaccinated intramuscularly with MVA-plague vaccines. Following two immunizations separated by 28 days, serum samples collected on days 28 and 42 post-initial vaccinations and analyzed by ELISA to determine humoral immune responses to F1 or V antigens. (A) Antibody responses to F1 antigen. (B) Antibody responses to V antigen from mice immunized with MVA/plague vaccines.
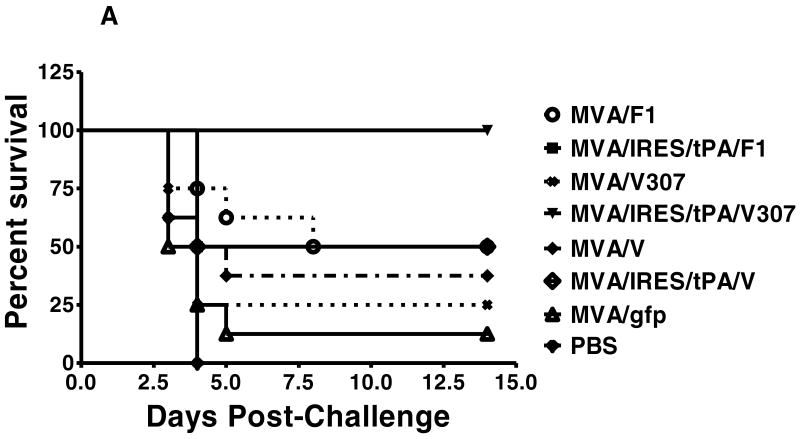
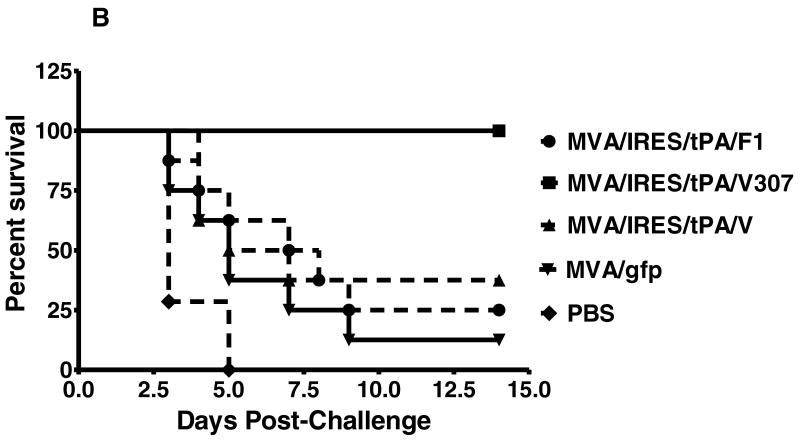
Protection against plague challenge
All mice vaccinated with the MVA/IRES/tPA/V307 survived lethal plague challenge with either the CO92 (35 LD50) or Java 9 (100 LD50) strain of Y. pestis (Figures 4A and 4B). Moreover, passive transfer of pooled immune serum from mice immunized with MVA/IRES/tPA/V307 to naïve BALB/c mice conferred significant protection (P<0.05) against the Java 9 strain of Y. pestis as compared to the control mice (data not shown). In contrast, only 25%, 37.5% to 50% of mice immunized with MVA/V307, MVA/V, or MVA/IRES/tPA/V survived challenge with the CO92 strains of Y. pestis, respectively (Figure 4A). Mice immunized with MVA/F1 or MVA/IRES/tPA/F1 had 50% or 25% survival rate against challenge with CO92 or Java 9 strain of Y. pestis, respectively (Figures 4A and 4B).
Figure 4.
Survival analysis of mice immunized with MVA-plague vaccines.
Two weeks following booster immunizations, mice were challenged (A) intranasally with 1 X 105 pfu (35LD50) of Y. pestis (CO92) or (B) intraperitoneally with 100 cfu (100 LD50) of Y. pestis (Java 9) and survival rates were recorded over a period of 2 weeks.
Minimal protective dose of MVA/IRES/tPA/V307 vaccine
To establish the minimal protective dose of the lead candidate vaccine, groups of 8 BALB/c mice were immunized (prime and boost) with increasing doses (5 X 105 pfu, 5 X 106 pfu or 5 X 107 pfu) of MVA/IRES/tPA/V307 and then challenged with either 35 or 350 LD50s of the CO92 Y. pestis strain. Mice immunized with increasing doses of MVA/IRES/tPA/V307 elicited corresponding increased immune responses with pre-challenge antibody titers of 3.38, 3.75 or 4.25 (log10), respectively. The highest immunization dose (5 X 107) elicited significantly higher antibody titer (P<0.05) compared to the lower doses and it conferred significant protection (87.5%) against challenge with either 35 or 350 LD50s of the CO92 Y. pestis strain, respectively (Table 2). There was no significant difference (P>0.05) between survival rates of mice immunized with the two lower doses of the MVA/IRES/tPA/V307 vaccine following challenge with 35LD50 of Y. pestis (Table 2). A 10-fold increase in the challenge dose (350 LD50) reduced the survival conferred by the lowest dose (5 X 105 pfu) of the MVA/IRES/tPA/V307 vaccine and was not significantly different (P>0.05) from that of the MVA/GFP control group (Table 2). However, significant protection (P=0.01) was conferred on mice immunized with 5 X 106 pfu of the vaccine against challenge with 350LD50 of Y. pestis compared to the control group.
Table 2. Survival rate of mice immunized with increasing doses of MVA/IRES/tPA/V307 and subsequently challenged via the intranasal route with CO92 strain of Y. pestis.
| Vaccination Dose (PFU) | Challenge Dose (LD50) | % Survival (14 days post-challenge) | Median Survival Time (Days)a |
|---|---|---|---|
| 5 X 105 | 35 | 62.5 | N/A |
| 5 X 106 | 35 | 37.5 | 10.5 |
| 5 X 107 | 35 | 87.5 | N/A |
| 5 X 107 (MVA/gfp) | 35 | 12.5 | 3.0 |
| 5 X 105 | 350 | 12.5 | 3.0 |
| 5 X 106 | 350 | 37.5 | 6.0 |
| 5 X 107 | 350 | 87.5 | N/A |
| 5 X 107 (MVA/gfp) | 350 | 0.0 | 3.0 |
Median survival time is the time at which 50% of animals have died. This value is not applicable (N/A) for groups with >50% survival rates.
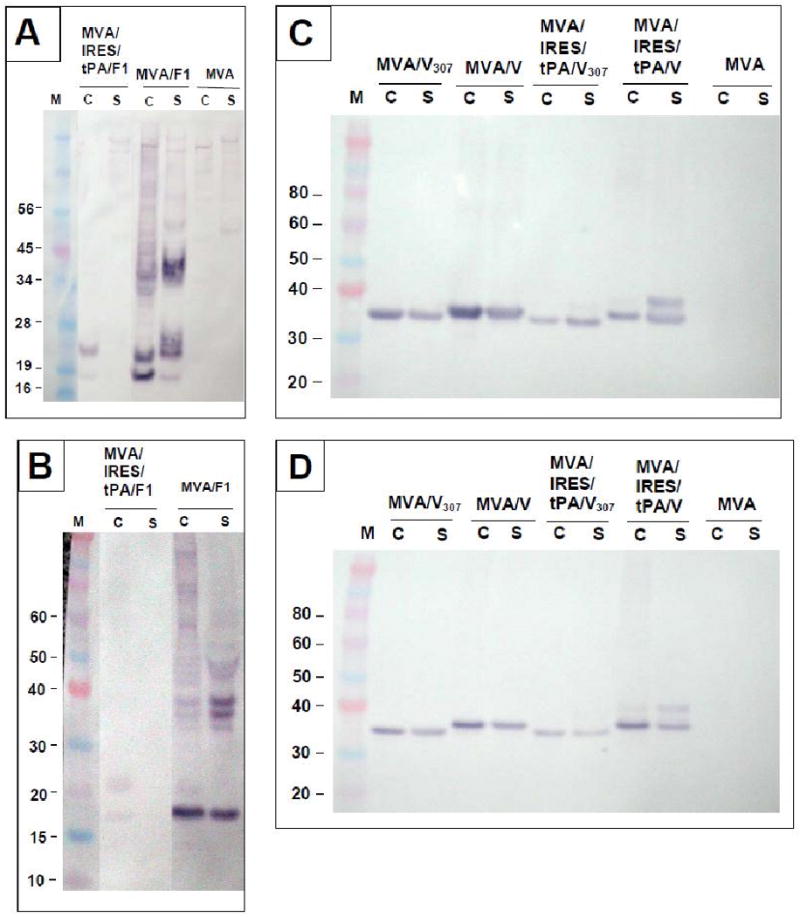
Safety of MVA/Plague vaccine candidates in immunocompromised mice
All mice in the vaccinia-Wyeth inoculated-group developed clinical disease symptoms characterized by pox lesions on their tails and feet and persistent weight loss; they died within 5 – 7 weeks post-infection. None of the animals from the MVAwt or MVA/Y. pestis vaccine constructs developed any pox lesions. Weight loss in the vaccinia-Wyeth group was significantly greater (P<0.0001) than in groups that were infected with MVAwt or MVA/plague vaccine constructs (Figure 5).
Figure 5.
Safety of MVA-plague vaccines in severe combined immune deficient (SCID) mice.
SCID mice were infected intraperitoneally with MVA/plague constructs (dose: 1 X 108 pfu), wild type MVA (MVAwt, dose: 1 X 108 pfu), or vaccinia virus Wyeth strain (dose: 1 X 106 pfu) and were weighed weekly for 12 weeks. Mice were euthanized when showing body conditioning score less than two (BCS < 2) or died naturally.
Discussion
In recent years, efforts to develop a suitable human plague vaccine have focused on subunits for the F1 and V antigens. Despite their success in inducing protective immune responses [23, 25, 26, 58, 59], subunit vaccines have several disadvantages. They generally require strong adjuvants, elicit poor CD8+ T cell responses and have short shelf lives [60]. The use of adjuvants often induces tissue reactions and multiple doses are required for a durable immunity [61]. Viral vectors, on the other hand, are capable of inducing both antibody and T-cell-mediated immunity in the absence of an adjuvant [62]. In this study, we describe the construction, expression, and preclinical efficacy and safety of novel MVA-plague vaccines containing IRES and strong secretory signals in mice. Immunogenicity studies in BALB/c mice demonstrated that MVA-vectored vaccines expressing the V antigen elicited robust antibody responses. Given the strong immunogenicity of the MVA/V construct and because V is currently one of the leading Y. pestis subunit vaccine candidates being developed for use in humans [25, 26], we focused our subsequent studies on this antigen. In particular, we examined the efficacy of MVA expressing a V gene with a deletion in the segment associated with the stimulation of the anti-inflammatory cytokine IL-10 [22]. Moreover, we examined the combined effect of the IRES and tPA on the immunogenicity and efficacy of MVA vaccines expressing the V307 gene. The insertion of molecular elements such as IRES and tPA in vaccine constructs, has been shown to facilitate the expression of target antigens and significantly enhance their immunogenicity [37-40].
All the MVA-V constructs were immunogenic, but when tested for protection against plague in mice, the MVA/IRES/tPA/V307 induced 87.5 to 100% protection against lethal challenge with the highly virulent Y. pestis CO92 strain. This finding is in agreement with earlier reports indicating improved immunogenic properties of a subunit candidate vaccine based on V307 in offering enhanced protection against plague [23]. It is interesting to note that the protection conferred by the MVA/V307 construct was significantly lower (P<0.05) than that induced by the MVA/IRES/tPA/V307 vaccine. Thus, the IRES and tPA secretory signal significantly enhanced the protective immune response, consistent with our previous studies demonstrating a similar effect in raccoon pox based vaccines against plague [63]. Interestingly, the IRES and tPA expression signals failed to significantly enhance the protective immune responses elicited by the full-length V and the F1 recombinant viruses. In our previous studies with other poxviruses, IRES/tPA both increased expression levels and improved protective efficacy [63]. In MVA vectors, IRES/tPA reduced expression levels yet still enhanced the protective efficacy of the V307 antigen. Since expression levels are not increased, we can only postulate that these post-transcriptional signals might improve antigen conformation, presentation and/or processing. In our studies, the MVA/F1 as well as the MVA/IRES/tPA/F1 vaccines did not elicit significant antibody responses against the F1 antigen. It can be speculated that the glycosylation of the expressed F1 proteins as seen in immunoblot analysis could mask epitopes, affecting the optimal induction of immune responses. However, 50% of mice immunized with the MVA/F1 or the MVA/IRES/tPA/F1 vaccine were protected against challenge with Y. pestis CO92 strain with a median survival times of 11 and 9 days, respectively. The weak anti-F1 antibody responses might have been sufficient to confer this level of protection. Alternatively, the development of cell-mediated immunity could have played a critical role in clearing the bacteria from the host.
Currently, although there are no strong correlates of protection against Y. pestis, antibodies have been shown to play an important role [64]. The production of high levels of antigen-specific antibodies elicited by the MVA/IRES/tPA/V307 construct may account for the high level of protection observed in these studies. However, the MVA/V construct generated high anti-V antibody yet demonstrated less protection from challenge. This finding is in contrast to previous studies demonstrating the protective capacity of this antigen when administered as a subunit vaccine [23, 65]. In non-human primate studies, Bashaw et al [66] showed that the presence of high antibody titers to F1 and V does not necessarily correlate with protection since some of the animals succumbed to challenge despite possessing high antibody titers. Similar reports have also asserted that humoral responses alone might not be sufficient to completely protect against plague[37, 67] Although the assessment of cellular immunity to our vaccine components were not within the scope of this paper, in future studies we plan to examine the role of humoral and cellular immune responses in protection.
Naturally occurring non-encapsulated variants of Y. pestis as well as isogenic non-encapsulated derivatives of encapsulated Y. pestis have been shown to be virulent [68-73]. An effective plague vaccine should be able to protect against infection with both encapsulated and non-encapsulated variants of Y. pestis. As reported in this study, our lead vaccine candidate MVA/IRES/tPA/V307 conferred complete protection against a non-encapsulated strain of Y. pestis (Java 9). Java 9 is a naturally occurring pathogen and despite the presence of a cryptic virulence plasmid [68-73], the lead vaccine candidate was very effective in protecting mice against challenge with this pathogen, an indication of the broad efficacy of the vaccine against diverse strains of Y. pestis. Preliminary data suggest that this protection was at least partially mediated by antibodies; passive transfer of anti-MVA/IRES/tPA/V307 antibodies protected mice from Java 9 challenge (data not shown).
These MVA vectored plague vaccines also were tested for safety. Infection of SCID BALB/c mice with replication competent poxviruses causes significant weight loss and poxvirus lesions analogous to the disseminated viremia that can occur in vaccinated individuals with underlying immune deficiencies. In our studies, the MVA-plague constructs were highly safe in SCID mice and no systemic disease was detected during the 12-week observation period.
In conclusion, these studies demonstrate the potential of MVA to effectively express Y. pestis antigens and generate protective plague immune responses. The MVA construct expressing the V307 antigen in conjunction with the IRES and tPA signal sequence was very immunogenic and safe, conferring protection against intranasal or intraperitoneal challenge with Y. pestis. These findings can lead to novel approaches to biodefense immunization since MVA has been stockpiled for use as a second-generation smallpox vaccine. A vaccine that simultaneously generates protective immune responses to two important biological threats such as smallpox and plague can be of high value in biodefense vaccination programs.
Acknowledgments
We are grateful to Dr. Arthur Friedlander and Dr. Mark Wolcott, U.S. Army Medical Research Institute for Infectious Diseases, for the Y. pestis strains used for challenge. We would also like to thank Dr. Steve Radecki for statistical analyses, Cooper Rosin, Sarah Koeppen, Devin Stinchcomb and Dr. Jeremy Jones (Inviragen, Inc.) for their technical laboratory assistance and the animal care staff of the School of Veterinary Medicine, University of Wisconsin-Madison for their expert care of the animals in these studies. We very much appreciate the critical review of this manuscript by Dr. Charalambos Partidos and Nancy Gundlach (Inviragen, Inc). These studies were partially supported by NIH grant 5R43A1061940-02
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Meyer KF. Pneumonic plague. Bacteriol Rev. 1961 Sep;25:249–61. doi: 10.1128/br.25.3.249-261.1961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Perry RD, Fetherston JD. Yersinia pestis -- etiologic agent of plague. Clin Microlbiol Rev. 1997;10(1):35–66. doi: 10.1128/cmr.10.1.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Human plague--four states, 2006. MMWR Morb Mortal Wkly Rep. 2006 Sep 1;55(34):940–3. [PubMed] [Google Scholar]
- 4.Neerinckx S, Bertherat E, Leirs H. Human plague occurrences in Africa: an overview from 1877 to 2008. Trans R Soc Trop Med Hyg. 2009 Aug 27; doi: 10.1016/j.trstmh.2009.07.028. [DOI] [PubMed] [Google Scholar]
- 5.Yin JX, Dong XQ, Liang Y, Wang P, Siriarayaporn P, Thaikruea L. Human plague outbreak in two villages, Yunnan Province, China, 2005. The Southeast Asian journal of tropical medicine and public health. 2007 Nov;38(6):1115–9. [PubMed] [Google Scholar]
- 6.Craven RB, Maupin GO, Beard ML, Quan TJ, Barnes AM. Reported cases of human plague infections in the United States, 1970-1991. J Med Entomol. 1993 Jul;30(4):758–61. doi: 10.1093/jmedent/30.4.758. [DOI] [PubMed] [Google Scholar]
- 7.Davalos VA, Torres MA, Mauricci CO, Laguna-Torres VA, Chinarro MP. Outbreak of bubonic plague in Jacocha, Huancabamba, Peru. Revista da Sociedade Brasileira de Medicina Tropical. 2001 Jan-Feb;34(1):87–90. doi: 10.1590/s0037-86822001000100013. [DOI] [PubMed] [Google Scholar]
- 8.Gabastou JM, Proano J, Vimos A, Jaramillo G, Hayes E, Gage K, et al. An outbreak of plague including cases with probable pneumonic infection, Ecuador, 1998. Trans R Soc Trop Med Hyg. 2000 Jul-Aug;94(4):387–91. doi: 10.1016/s0035-9203(00)90114-7. [DOI] [PubMed] [Google Scholar]
- 9.Migliani R, Chanteau S, Rahalison L, Ratsitorahina M, Boutin JP, Ratsifasoamanana L, et al. Epidemiological trends for human plague in Madagascar during the second half of the 20th century: a survey of 20,900 notified cases. Trop Med Int Health. 2006 Aug;11(8):1228–37. doi: 10.1111/j.1365-3156.2006.01677.x. [DOI] [PubMed] [Google Scholar]
- 10.Anderson SH, Williams ES. Plague in a complex of white-tailed prairie dogs and associated small mammals in Wyoming. J Wildl Dis. 1997;33:720–32. doi: 10.7589/0090-3558-33.4.720. [DOI] [PubMed] [Google Scholar]
- 11.Gage KL, Dennis DT, Orloski KA, Ettestad P, Brown TL, Reynolds PJ, et al. Cases of cat-associated human plague in the Western US, 1977-1998. Clin Infect Dis. 2000 Jun;30(6):893–900. doi: 10.1086/313804. [DOI] [PubMed] [Google Scholar]
- 12.Galimand M, Carniel E, Courvalin P. Resistance of Yersinia pestis to antimicrobial agents. Antimicrob Agents Chemother. 2006 Oct;50(10):3233–6. doi: 10.1128/AAC.00306-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Galimand M, Guiyoule A, Gerbaud G, Rasoamanana B, Chanteau S, Carniel E, et al. Multidrug resistance in Yersinia pestis mediated by a transferable plasmid. N Engl J Med. 1997 Sep 4;337(10):677–80. doi: 10.1056/NEJM199709043371004. [DOI] [PubMed] [Google Scholar]
- 14.Inglesby TV, Dennis DT, Henderson DA, Bartlett JG, Ascher MS, Eitzen E, et al. Plague as a biological weapon: medical and public health management. Working Group on Civilian Biodefense. Jama. 2000 May 3;283(17):2281–90. doi: 10.1001/jama.283.17.2281. [DOI] [PubMed] [Google Scholar]
- 15.Smiley ST. Current challenges in the development of vaccines for pneumonic plague. Expert Rev Vaccines. 2008 Mar;7(2):209–21. doi: 10.1586/14760584.7.2.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Titball RW, Williamson ED. Vaccination against bubonic and pneumonic plague. Vaccine. 2001 Jul 20;19(30):4175–84. doi: 10.1016/s0264-410x(01)00163-3. [DOI] [PubMed] [Google Scholar]
- 17.Williamson ED, Eley SM, Stagg AJ, Green M, Russell P, Titball RW. A single dose subunit vaccine protects against pneumonic plague. Vaccine. 2000 Oct 15;19(4-5):566–71. doi: 10.1016/s0264-410x(00)00159-6. [DOI] [PubMed] [Google Scholar]
- 18.Protsenko OA, Anisimov PI, Mozharov OT, Konnov NP, Popov Iu A. Detection and characterization of the plasmids of the plague microbe which determine the synthesis of pesticin I, fraction I antigen and “mouse” toxin exotoxin. Genetika. 1983 Jul;19(7):1081–90. [PubMed] [Google Scholar]
- 19.Philipovskiy AV, Cowan C, Wulff-Strobel CR, Burnett SH, Kerschen EJ, Cohen DA, et al. Antibody against V antigen prevents Yop-dependent growth of Yersinia pestis. Infect Immun. 2005 Mar;73(3):1532–42. doi: 10.1128/IAI.73.3.1532-1542.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Du Y, Rosqvist R, Forsberg A. Role of fraction 1 antigen of Yersinia pestis in inhibition of phagocytosis. Infect Immun. 2002 Mar;70(3):1453–60. doi: 10.1128/IAI.70.3.1453-1460.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Quenee LE, Cornelius CA, Ciletti NA, Elli D, Schneewind O. Yersinia pestis caf1 variants and the limits of plague vaccine protection. Infect Immun. 2008 May;76(5):2025–36. doi: 10.1128/IAI.00105-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nakajima R, Brubaker RR. Association between virulence of Yersinia pestis and suppression of gamma interferon and tumor necrosis factor alpha. Infect Immun. 1993 Jan;61(1):23–31. doi: 10.1128/iai.61.1.23-31.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Overheim KA, Depaolo RW, Debord KL, Morrin EM, Anderson DM, Green NM, et al. LcrV plague vaccine with altered immunomodulatory properties. Infect Immun. 2005 Aug;73(8):5152–9. doi: 10.1128/IAI.73.8.5152-5159.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Williamson ED, Flick-Smith HC, Waters E, Miller J, Hodgson I, Le Butt CS, et al. Immunogenicity of the rF1+rV vaccine for plague with identification of potential immune correlates. Microb Pathog. 2007 Jan;42(1):11–21. doi: 10.1016/j.micpath.2006.09.003. [DOI] [PubMed] [Google Scholar]
- 25.Anderson GW, Jr, Leary SE, Williamson ED, Titball RW, Welkos SL, Worsham PL, et al. Recombinant V antigen protects mice against pneumonic and bubonic plague caused by F1-capsule-positive and -negative strains of Yersinia pestis. Infect Immun. 1996 Nov;64(11):4580–5. doi: 10.1128/iai.64.11.4580-4585.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Leary SE, Griffin KF, Garmory HS, Williamson ED, Titball RW. Expression of an F1/V fusion protein in attenuated Salmonella typhimurium and protection of mice against plague. Microb Pathog. 1997 Sep;23(3):167–79. doi: 10.1006/mpat.1997.0141. [DOI] [PubMed] [Google Scholar]
- 27.Powell BS, Andrews GP, Enama JT, Jendrek S, Bolt C, Worsham P, et al. Design and testing for a nontagged F1-V fusion protein as vaccine antigen against bubonic and pneumonic plague. Biotechnol Prog. 2005 Sep-Oct;21(5):1490–510. doi: 10.1021/bp050098r. [DOI] [PubMed] [Google Scholar]
- 28.Uddowla S, Freytag LC, Clements JD. Effect of adjuvants and route of immunizations on the immune response to recombinant plague antigens. Vaccine. 2007 Nov 19;25(47):7984–93. doi: 10.1016/j.vaccine.2007.09.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Williamson ED, Flick-Smith HC, Lebutt C, Rowland CA, Jones SM, Waters EL, et al. Human immune response to a plague vaccine comprising recombinant F1 and V antigens. Infect Immun. 2005 Jun;73(6):3598–608. doi: 10.1128/IAI.73.6.3598-3608.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Leung KY, Reisner BS, Straley SC. YopM inhibits platelet aggregation and is necessary for virulence of Yersinia pestis in mice. Infect Immun. 1990 Oct;58(10):3262–71. doi: 10.1128/iai.58.10.3262-3271.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Benner GE, Andrews GP, Byrne WR, Strachan SD, Sample AK, Heath DG, et al. Immune response to Yersinia outer proteins and other Yersinia pestis antigens after experimental plague infection in mice. Infect Immun. 1999 Apr;67(4):1922–8. doi: 10.1128/iai.67.4.1922-1928.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Andrews GP, Strachan ST, Benner GE, Sample AK, Anderson GW, Jr, Adamovicz JJ, et al. Protective efficacy of recombinant Yersinia outer proteins against bubonic plague caused by encapsulated and nonencapsulated Yersinia pestis. Infect Immun. 1999 Mar;67(3):1533–7. doi: 10.1128/iai.67.3.1533-1537.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chattopadhyay A, Park S, Delmas G, Suresh R, Senina S, Perlin DS, et al. Single-dose, virus-vectored vaccine protection against Yersinia pestis challenge: CD4+ cells are required at the time of challenge for optimal protection. Vaccine. 2008 Nov 25;26(50):6329–37. doi: 10.1016/j.vaccine.2008.09.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Palin A, Chattopadhyay A, Park S, Delmas G, Suresh R, Senina S, et al. An optimized vaccine vector based on recombinant vesicular stomatitis virus gives high-level, long-term protection against Yersinia pestis challenge. Vaccine. 2007 Jan 8;25(4):741–50. doi: 10.1016/j.vaccine.2006.08.010. [DOI] [PubMed] [Google Scholar]
- 35.Chiuchiolo MJ, Boyer JL, Krause A, Senina S, Hackett NR, Crystal RG. Protective immunity against respiratory tract challenge with Yersinia pestis in mice immunized with an adenovirus-based vaccine vector expressing V antigen. J Infect Dis. 2006 Nov 1;194(9):1249–57. doi: 10.1086/507644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yang X, Hinnebusch BJ, Trunkle T, Bosio CM, Suo Z, Tighe M, et al. Oral vaccination with salmonella simultaneously expressing Yersinia pestis F1 and V antigens protects against bubonic and pneumonic plague. J Immunol. 2007 Jan 15;178(2):1059–67. doi: 10.4049/jimmunol.178.2.1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Osorio JE, Powell TD, Frank RS, Moss K, Haanes EJ, Smith SR, et al. Recombinant raccoon pox vaccine protects mice against lethal plague. Vaccine. 2003;21:1232–8. doi: 10.1016/s0264-410x(02)00557-1. [DOI] [PubMed] [Google Scholar]
- 38.Mencher JS, Smith SR, Powell TD, Stinchcomb DT, Osorio JE, Rocke TE. Protection of black-tailed prairie dogs (Cynomys ludovicianus) against plague after voluntary consumption of baits containing recombinant raccoon poxvirus vaccine. Infect Immun. 2004 Sep;72(9):5502–5. doi: 10.1128/IAI.72.9.5502-5505.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rocke TE, Iams KP, Dawe S, Smith SR, Williamson JL, Heisey DM, et al. Further development of raccoon poxvirus-vectored vaccines against plague (Yersinia pestis) Vaccine. 2009 Dec 11;28(2):338–44. doi: 10.1016/j.vaccine.2009.10.043. [DOI] [PubMed] [Google Scholar]
- 40.Rocke TE, Smith SR, Stinchcomb DT, Osorio JE. Immunization of black-tailed prairie dog against plague through consumption of vaccine-laden baits. J Wildl Dis. 2008 Oct;44(4):930–7. doi: 10.7589/0090-3558-44.4.930. [DOI] [PubMed] [Google Scholar]
- 41.Mayr A, Stickl H, Muller HK, Danner K, Singer H. The smallpox vaccination strain MVA: marker, genetic structure, experience gained with th eparenteral vaccination and behavior in organisms with a debiliteated defence mechasism (author's transl) Zentralbl Bakteriol [B] 1978;167:375–90. [PubMed] [Google Scholar]
- 42.Drexler I, Staib C, Sutter G. Modified vaccinia virus Ankara as antigen delivery system: how can we best use its potential? Curr Opin Biotechnol. 2004 Dec;15(6):506–12. doi: 10.1016/j.copbio.2004.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Garcia-Hernandez E, Gonzalez-Sanchez JL, Andrade-Manzano A, Contreras ML, Padilla S, Guzman CC, et al. Regression of papilloma high-grade lesions (CIN 2 and CIN 3) is stimulated by therapeutic vaccination with MVA E2 recombinant vaccine. Cancer Gene Ther. 2006 Jun;13(6):592–7. doi: 10.1038/sj.cgt.7700937. [DOI] [PubMed] [Google Scholar]
- 44.Harrop R, Connolly N, Redchenko I, Valle J, Saunders M, Ryan MG, et al. Vaccination of colorectal cancer patients with modified vaccinia Ankara delivering the tumor antigen 5T4 (TroVax) induces immune responses which correlate with disease control: a phase I/II trial. Clin Cancer Res. 2006 Jun 1;12(11 Pt 1):3416–24. doi: 10.1158/1078-0432.CCR-05-2732. [DOI] [PubMed] [Google Scholar]
- 45.Meyer H, Sutter G, Mayr A. Mapping of deletions in the genome of the highly attenuated vaccinia virus MVA and their influence on virulence. J Gen Virol. 1991 May;72(Pt 5):1031–8. doi: 10.1099/0022-1317-72-5-1031. [DOI] [PubMed] [Google Scholar]
- 46.Sutter G, Moss B. Novel vaccinia vector derived from the host range restricted and highly attenuated MVA strain of vaccinia virus. Dev Biol Stand. 1995;84:195–200. [PubMed] [Google Scholar]
- 47.Sutter G, Wyatt LS, Foley PL, Bennink JR, Moss B. A recombinant vector derived from the host range-restricted and highly attenuated MVA strain of vaccinia virus stimulates protective immunity in mice to influenza virus. Vaccine. 1994 Aug;12(11):1032–40. doi: 10.1016/0264-410x(94)90341-7. [DOI] [PubMed] [Google Scholar]
- 48.Hanke T, McMichael AJ, Dennis MJ, Sharpe SA, Powell LA, McLoughlin L, et al. Biodistribution and persistence of an MVA-vectored candidate HIV vaccine in SIV-infected rhesus macaques and SCID mice. Vaccine. 2005 Feb 10;23(12):1507–14. doi: 10.1016/j.vaccine.2004.08.050. [DOI] [PubMed] [Google Scholar]
- 49.Ramirez JC, Finke D, Esteban M, Kraehenbuhl JP, Acha-Orbea H. Tissue distribution of the Ankara strain of vaccinia virus (MVA) after mucosal or systemic administration. Arch Virol. 2003;148(5):827–39. doi: 10.1007/s00705-003-0006-z. [DOI] [PubMed] [Google Scholar]
- 50.Earl PL, Cooper N, Wyatt LS, Moss B, Carroll MW. Preparation of cell cultures and vaccinia virus stocks. In: Coligan John E, et al., editors. Current protocols in protein science. Unit5 12. Chapter 5. 2001. May, [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Earl PL, Moss B, Wyatt LS, Carroll MW. Generation of recombinant vaccinia viruses. In: Ausubel Frederick M, et al., editors. Current protocols in molecular biology. Unit16 7. Chapter 16. 2001. May, [DOI] [PubMed] [Google Scholar]
- 52.Gilbert PA, Comanita L, Barrett J, Peters A, Szabat M, McFadden G, et al. Current Status for High Titre Poxvirus Stock Preparation in CEF Under Serum-Free Medium Conditions: Implication for Vaccine Development. Cytotechnology. 2005 Jun;48(1-3):79–88. doi: 10.1007/s10616-005-3795-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hornemann S, Harlin O, Staib C, Kisling S, Erfle V, Kaspers B, et al. Replication of modified vaccinia virus Ankara in primary chicken embryo fibroblasts requires expression of the interferon resistance gene E3L. J Virol. 2003 Aug;77(15):8394–407. doi: 10.1128/JVI.77.15.8394-8407.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Reed LJ, Muench H. A simple method of estimating fifty percent points. Am J Hyg. 1938;27:493. [Google Scholar]
- 55.Ullman-Cullere MH, Foltz CJ. Body condition scoring: a rapid and accurate method for assessing health status in mice. Lab Anim Sci. 1999 Jun;49(3):319–23. [PubMed] [Google Scholar]
- 56.Miller J, Williamson ED, Lakey JH, Pearce MJ, Jones SM, Titball RW. Macromolecular organisation of recombinant Yersinia pestis F1 antigen and the effect of structure on immunogenicity. FEMS Immunol Med Microbiol. 1998 Jul;21(3):213–21. doi: 10.1111/j.1574-695X.1998.tb01168.x. [DOI] [PubMed] [Google Scholar]
- 57.Vorontsov ED, Dubichev AG, Serdobintsev LN, Naumov AV. Association-dissociation processes and supermolecular organisation of the capsule antigen (protein F1) of Yersinia pestis. Biomed Sci. 1990 Apr 1;4:391–6. [PubMed] [Google Scholar]
- 58.Heath DG, Anderson GW, Jr, Mauro JM, Welkos SL, Andrews GP, Adamovicz J, et al. Protection against experimental bubonic and pneumonic plague by a recombinant capsular F1-V antigen fusion protein vaccine. Vaccine. 1998 Jul;16(11-12):1131–7. doi: 10.1016/s0264-410x(98)80110-2. [DOI] [PubMed] [Google Scholar]
- 59.Titball RW, Williamson ED. Yersinia pestis (plague) vaccines. Expert Opin Biol Ther. 2004 Jun;4(6):965–73. doi: 10.1517/14712598.4.6.965. [DOI] [PubMed] [Google Scholar]
- 60.Schirmbeck R, Deml L, Melber K, Wolf H, Wagner R, Reimann J. Priming of class I- restricted cytotoxic T lymphocytes by vaccination with recombinant protein antigens. Vaccine. 1995 Jun;13(9):857–65. doi: 10.1016/0264-410x(94)00038-o. [DOI] [PubMed] [Google Scholar]
- 61.Gherardi RK, Coquet M, Cherin P, Belec L, Moretto P, Dreyfus PA, et al. Macrophagic myofasciitis lesions assess long-term persistence of vaccine-derived aluminium hydroxide in muscle. Brain. 2001;124(Pt 9):1821–31. doi: 10.1093/brain/124.9.1821. [DOI] [PubMed] [Google Scholar]
- 62.Li S, Locke E, Bruder J, Clarke D, Doolan DL, Havenga MJ, et al. Viral vectors for malaria vaccine development. Vaccine. 2007 Mar 30;25(14):2567–74. doi: 10.1016/j.vaccine.2006.07.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Osorio JE, Frank RS, Moss K, Taraska T, Powell T, Stinchcomb DT. Raccoon poxvirus as a mucosal vaccine vector for domestic cats. J Drug Target. 2003;11(8-10):463–70. doi: 10.1080/10611860410001670062. [DOI] [PubMed] [Google Scholar]
- 64.Williamson ED, Vesey PM, Gillhespy KJ, Eley SM, Green M, Titball RW. An IgG1 titre to the F1 and V antigens correlates with protection against plague in the mouse model. Clinical and experimental immunology. 1999 Apr;116(1):107–14. doi: 10.1046/j.1365-2249.1999.00859.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.DeBord KL, Anderson DM, Marketon MM, Overheim KA, DePaolo RW, Ciletti NA, et al. Immunogenicity and protective immunity against bubonic plague and pneumonic plague by immunization of mice with the recombinant V10 antigen, a variant of LcrV. Infect Immun. 2006 Aug;74(8):4910–4. doi: 10.1128/IAI.01860-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Bashaw J, Norris S, Weeks S, Trevino S, Adamovicz JJ, Welkos S. Development of in vitro correlate assays of immunity to infection with Yersinia pestis. Clin Vaccine Immunol. 2007 May;14(5):605–16. doi: 10.1128/CVI.00398-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Parent MA, Berggren KN, Kummer LW, Wilhelm LB, Szaba FM, Mullarky IK, et al. Cell-mediated protection against pulmonary Yersinia pestis infection. Infect Immun. 2005 Nov;73(11):7304–10. doi: 10.1128/IAI.73.11.7304-7310.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Burrows TW. Virulence of Pasteurella pestis. Nature. 1957 Jun 15;179(4572):1246–7. doi: 10.1038/1791246a0. [DOI] [PubMed] [Google Scholar]
- 69.Davis HL, Weeratna R, Waldschmidt TJ, Tygrett L, Schorr J, Krieg AM, et al. CpG DNA is a potent enhancer of specific immunity in mice immunized with recombinant hepatitis B surface antigen. J Immunol. 1998;160(2):870–6. [PubMed] [Google Scholar]
- 70.Davis KJ, Fritz DL, Pitt ML, Welkos SL, Worsham PL, Friedlander AM. Pathology of experimental pneumonic plague produced by fraction-1 positive and fraction-1 negative Yersinia pestis in african green monkeys. Arch Pathol Lab Med. 1996;120(156-163) [PubMed] [Google Scholar]
- 71.Drozdov IG, Anisimov AP, Samoilova SV, Yezhov IN, Yeremin SA, Karlyshev AV, et al. Virulent non-capsulate Yersinia pestis variants constructed by insertion mutagenesis. J Med Microbiol. 1995 Apr;42(4):264–8. doi: 10.1099/00222615-42-4-264. [DOI] [PubMed] [Google Scholar]
- 72.Williams JE, Harrison DN, Cavanaugh DC. Letter: Cryptic infection of rats with non-encapsulated variants of Yersinia pestis. Trans R Soc Trop Med Hyg. 1975;69(1):171–2. doi: 10.1016/0035-9203(75)90039-5. [DOI] [PubMed] [Google Scholar]
- 73.Winter CC, Cherry WB, Moody MD. An unusual strain of Pasteurella pestis isolated from a fatal human case of plague. Bull World Health Organ. 1960;23:408–9. [PMC free article] [PubMed] [Google Scholar]