Abstract
In the pediatric hematology-oncology population, lumbar punctures (LP’s) are commonly performed to administer intrathecal chemotherapy and obtain CSF samples. Difficult LP’s can arise due to obesity, fibrous tissue formation due to repeated LP procedures, or spinal abnormalities. For difficult LP’s that require imaging-guidance, fluoroscopy is generally?? Fluoroscopy, however, subjects the patient and healthcare providers to radiation while also potentially increasing procedure cost and time. We retrospectively studied the utility of ultrasound-guidance to facilitate LP in 4 pediatric hematology-oncology patients. All 4 patients had a history of difficult LP and 3 of 4 had previously required use of fluoroscopy. With the use of ultrasound, the LP was successfully performed in all 4 patients with one attempt (number of attempts not recorded in one patient). Procedure time was less than 20 minutes in all 4 patients. Our preliminary data suggests that ultrasound may be an efficacious alternative to fluoroscopy. By using ultrasound to identify the landmarks in the lumbar region, the appropriate puncture point can be determined allowing access to the intrathecal space with relative ease. This would decrease the need for fluoroscopy-guidance, the incidence of multiple punctures as well as reducing the procedure time and costs.
Keywords: Ultrasound, diagnosis, difficult lumbar puncture, pediatric, oncology
Introduction
In the pediatric oncologic population, lumbar puncture (LP) is commonly used for both diagnostic and therapeutic purposes. Although LP can generally be performed quickly with procedural sedation, anatomical issues or variations in the patient’s body habitus including obesity may preclude successful performance or require multiple attempts and prolonged sedation. In such cases, radiological imaging such as fluoroscopy has been shown to be a useful adjunct [1]. However, fluoroscopy exposes the patient and healthcare providers to radiation, results in higher patient costs, and increases procedure time. A potential alternative to fluoroscopy is ultrasound.
Ultrasound is currently used in the adult population as a routine clinical tool for peripheral nerve block and to facilitate neuraxial (epidural and spinal) approaches in patients with difficult surface landmarks or abnormal anatomy [2,3]. In the pediatric population, the utility of ultrasound-guided techniques is also increasing with demonstration of its use as an adjunct for neuraxial blockade and in facilitating LP [4-6]. We present additional retrospective experience with the use of ultrasound to facilitate LP in pediatric hematology-oncology patients who have previously required multiple attempts or the use of fluoroscopy. The potential application of this technology in facilitating the performance of LP in the pediatric population is reviewed.
Case report
The patient was a 14-year-old, 86 kg (body mass index 31 kg/M2) adolescent who was diagnosed with acute lymphoblastic leukemia (ALL) and undergoing maintenance therapy. Intrathecal chemotherapy began within the first month of diagnosis and was administered at regular intervals. During the initial months following the initiation of therapy, the performance of the LP was uneventful. In a time span of approximately 3 months, the patient’s weight increased by 9 kilograms and there was increasing difficulty with performance of the LP. The subsequent procedures required multiple attempts to enter the intrathecal space and in two instances the procedure required more than 20 minutes. Eventually, after continuing to gain another 17 kilograms, there was a failed LP attempt and fluoroscopy-guidance was used to successfully obtain the CSF sample and administer intrathecal chemotherapy. As per the routine practice at our institution, all of these LP attempts were performed using deep sedation or general anesthesia provided by the pediatric anesthesiology service. Given the logistics of scheduling, added procedure time, and radiation exposure, the potential use of ultrasound-assisted LP was offered by the Department of Anesthesiology & Pain Medicine. The patient was held nil per os for 6 hours per the procedural sedation policy and was brought into the operating room. Routine American Society of Anesthesiologists’ monitors were placed and anesthesia induced with intravenous propofol followed by maintenance anesthesia with inhaled sevoflurane administered via a laryngeal mask airway. The patient was positioned in the right lateral decubitus position. The GE LOGIQ E ultrasound model with a high frequency (12 mHz) linear 12L-RS transducer was used. The ultrasound probe was used to distinguish the appropriate landmarks including the spinous and transverse processes of the vertebral bodies (Figure 1). The midline was identified and the spinous processes of L2, L3, and L4 were marked. The L3-4 interspace was identified and marked (Figure 2). The lumbar area was cleaned with chlorhexidine and a 22 gauge, 3.5 inch spinal needle with stylet was inserted and advanced in the midline at the L3-4 interspace. One attempt was required to enter the intrathecal space and free-flowing, clear, and bloodless CSF was obtained. Procedure time including ultrasound scanning was 10 minutes.
Figure 1.
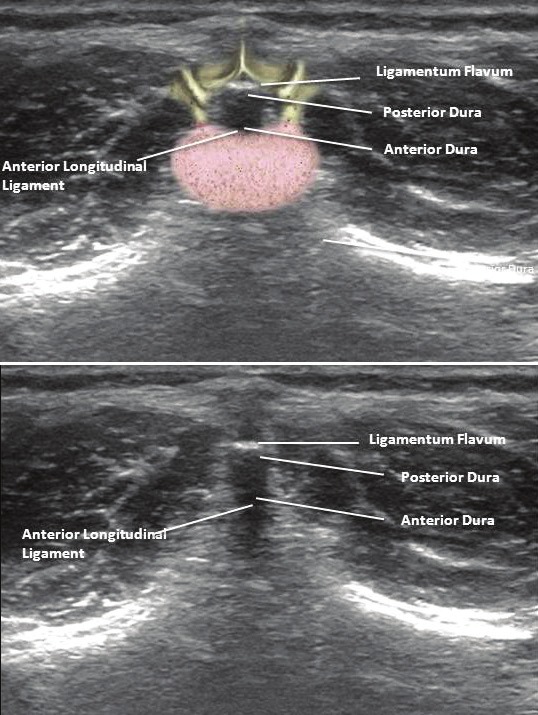
Transverse scan through the lumbar area showing ligamentum flavum, anterior border of the dura, posterior border of the dura, and the anterior longitudinal ligament.
Figure 2.
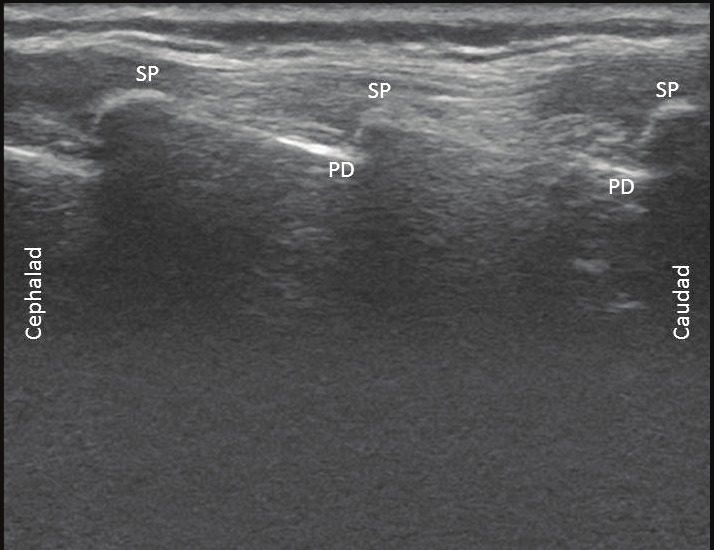
Longitudinal scan through lumbar area with probe placed in the midline. Multiple spinous processes (SP) as well as the posterior dural (PD) border can be identified. The intrathecal space is just distal to the PD.
Methods & results
Following approval by the Institutional Review Board of Nationwide Children’s Hospital, we retrospectively identified patients in whom ultrasound guidance was used to facilitate LP over a 3 month period. The following demographic data were obtained: age, weight, and gender. Additional data included previous history of difficult LP (multiple attempts, failed access or prolonged procedure time), and previous use of fluoroscopy to achieve successful LP. Procedure time was calculated as the start of positioning to completion of the injection of chemotherapy including the use of ultrasound. The data are listed in Table 1.
Table 1.
Demographic data and information of retrospective study cohort
| Patient | Demographic data (age, weight, and gender) | Previous difficult LP (yes or no) | Previous use of fluoroscopy (yes or no) | Results with ultrasound (number of attempts, procedure time*) |
|---|---|---|---|---|
| 1 | 19 year old, 50.4 kilograms, female | Yes | Yes | No record of number of attempts - 17 minutes |
| 2 | 15 year old, 56.2 kilogram, male | Yes | No | One attempt - 8 minutes |
| 3 | 16 year old, 145.7 kilogram, male | Yes | Yes | One attempt – 14 minutes |
LP = lumbar puncture.
Discussion
Procedures that involve vascular access, peripheral nerve blockade, lumbar puncture, and neuraxial anesthesia have classically been performed using surface landmarks and assumptions regarding the underlying anatomy. As such, the site for skin puncture is generally landmark based. Variations in anatomy, both surface and internal, can create difficulties in such procedures leading to multiple puncture attempts or failures. This may result in increased post-procedure pain for the patient, increased procedure time, and increased exposure to anesthetic or sedative agents. All of these can not only result in patient morbidity, but also increased healthcare costs.
When multiple attempts are required to gain access to the intrathecal space, radiologic imaging techniques may be used. Fluoroscopy is the traditional imaging modality that is used. Ultrasound has long been utilized in clinical medicine for diagnostic imaging. Recently, it has seen expanded use by non-radiologists in anesthesiology, emergency medicine, urology, and orthopedics [7-12]. This has included its use to facilitate epidural anesthesia to obstetrics patients and peripheral nerve blockade. In particular, ultrasound-guidance may be especially helpful in procedures that require visual appraisal of surface landmarks.
Ultrasound has also been used to successfully access the intrathecal space in the pediatric population, particularly infants, in whom intrathecal approaches can be challenging due to their smaller size [5]. Coley et al demonstrated that in addition to facilitating performance of the LP, ultrasound can help identifying anatomical issues which may preclude LP [13]. In their study, the LP was deferred or cancelled in 14 in 47 cases based on the initial findings on the ultrasound including obliteration of the CSF space from a hematoma due to previous attempts or minimal fluid. Others have demonstrated the utility of ultrasound in determining optimal patient positioning for LP, needle entry angle for LP, and epidural catheter placement in neonates [14-16].
To date, the majority of experience with using ultrasound to facilitate LP has been in the neonatal and infant populations. Our retrospective experience demonstrates the potential utility of ultrasound in pediatric hematology-oncology patients with a previous history of or anticipated difficult LP. Difficulties in the successful performance of LP may be the result of obesity, subcutaneous fibrosis, or spinal deformities such as scoliosis or lordosis. Such difficulties may result in increased procedure time, missed chemotherapy administrations, and increased post-procedure pain.
The usual solution for such patients is a referral to interventional radiology for fluoroscopy-guidance LP. Fluoroscopy-guidance, though helpful, subjects both the patient and the healthcare provider to radiation, may result in logistical scheduling issues, and results in increased procedure costs. We, therefore, believe that ultrasound was a safer and more convenient alternative to fluoroscopy. This is especially true in our hospital setting where many of these procedures are already performed in the operating room using deep sedation or general anesthesia. As the anesthesia providers are facile in the use of ultrasound, a third party (radiologist) is not necessary thereby limiting the manpower needs to the hematologist-oncologist and the anesthesiologist.
Our preliminary experience suggests that ultrasound is an alternative imaging-guide to fluoroscopy when conducting difficult LP’s in pediatric hematology-oncology patients. Ultrasound can be quickly used to delineate neuraxial landmarks quickly and ensure successful entry into the intrathecal space. Moreover, ultrasound-guidance eliminates patient and healthcare worker exposure to fluoroscopy-related radiation, decreases procedure time, and overall costs. The use of ultrasound-guidance for lumbar punctures may also be advantageous for the pediatric anesthesiologist or hematologist-oncologist, providing increased flexibility and independence when faced with performance of a difficult LP. The limitations of our current report include its retrospective nature and the potential difficulty in obtaining accurate data regarding procedure time and number of attempts. As this was an observational study, no definitive conclusions can be drawn. Future projects may prospectively compare the efficacy of ultrasound-guidance versus fluoroscopy-guidance.
References
- 1.Eskey CJ, Ogilvy CS. Fluoroscopy-guided Lumbar Puncture: Decreased frequency of traumatic tap and implications for the assessment of CT-negative acute subarachnoid hemorrhage. AJNR Am J Neuroradiol. 2001;22:571–576. [PMC free article] [PubMed] [Google Scholar]
- 2.Chin KJ, Perlas A, Singh M, Arzola C, Prasad A, Chan V, Brull R. An ultrasound-assisted approach facilitates spinal anesthesia for total joint arthroplasty. Can J Anaesth. 2009;56:643–650. doi: 10.1007/s12630-009-9132-8. [DOI] [PubMed] [Google Scholar]
- 3.Chin KJ, Perlas A, Chan V, Brown-Shreves D, Koshkin A, Vaishnav V. Ultrasound imaging facilitates spinal anesthesia in adults with difficult surface anatomy landmarks. Anesthesiology. 2011;115:94–101. doi: 10.1097/ALN.0b013e31821a8ad4. [DOI] [PubMed] [Google Scholar]
- 4.Tsui BC, Suresh S. Ultrasound imaging for regional anesthesia in infants, children, and adolescents: a review of current literature and its application in the practice of neuroaxial blocks. Anesthesiology. 2010;112:719–728. doi: 10.1097/ALN.0b013e3181c5e03a. [DOI] [PubMed] [Google Scholar]
- 5.Ayalin T, Lam SH. Ultrasound-assisted lumbar puncture in infants. Acad Emerg Med. 2011;18:e36–e39. doi: 10.1111/j.1553-2712.2011.01044.x. [DOI] [PubMed] [Google Scholar]
- 6.Bruccoleri RE, Chen L. Needle entry angle for lumbar puncture in children as determined by using ultrasonography. Pediatrics. 2011;127:e921–e926. doi: 10.1542/peds.2010-2511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grau T, Leipold RW, Conradi R, Martin E, Motsch J. Efficacy of ultrasound imaging in obstetric epidural anesthesia. J Clin Anesth. 2002;14:169–175. doi: 10.1016/s0952-8180(01)00378-6. [DOI] [PubMed] [Google Scholar]
- 8.Maecken T, Grau T. Ultrasound imaging in vascular access. Crit Care Med. 2007;35:S178–S185. doi: 10.1097/01.CCM.0000260629.86351.A5. [DOI] [PubMed] [Google Scholar]
- 9.Pirotte T. Ultrasound-guided vascular access in adults and children: beyond the internal jugular vein puncture. Acta Anaesthesiol Belg. 2008;59:157–166. [PubMed] [Google Scholar]
- 10.Halpern EJ. Contrast-enhanced ultrasound imaging of prostate cancer. Rev Urol. 2006;8:S29–37. [PMC free article] [PubMed] [Google Scholar]
- 11.Cortellaro F, Colombo S, Coen D, Duca PG. Lung ultrasound is an accurate diagnostic tool for the diagnosis of pneumonia in the emergency department. Emerg Med J. 2012;29:19–23. doi: 10.1136/emj.2010.101584. [DOI] [PubMed] [Google Scholar]
- 12.Watanabe Y, Matsushita T, Bhandari M, Zdero R, Schemitsch EH. Ultrasound for fracture healing: current evidence. J Orthop Trauma. 2010;24:S56–61. doi: 10.1097/BOT.0b013e3181d2efaf. [DOI] [PubMed] [Google Scholar]
- 13.Coley BD, Shiels WE, Hogan MJ. Diagnostic and interventional ultrasonography in neonatal and infant lumbar puncture. Pediatr Radiol. 2001;31:399–402. doi: 10.1007/s002470100453. [DOI] [PubMed] [Google Scholar]
- 14.Oncel S, Gunlemez A, Anik Y, Alvur M. Positioning of infants in the neonatal intensive care unit for lumbar puncture as determined by bedside ultrasonography. Arch Dis Child Fetal Neonatal Ed. 2012 doi: 10.1136/archdischild-2011-301475. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 15.Bruccoleri RE, Chen L. Needle-entry angle for lumbar puncture in children as determined by using ultrasonography. Pediatrics. 2001;127:e921–e926. doi: 10.1542/peds.2010-2511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Willschke H, Bosenberg A, Marhofer P, Willschke J, Schwindt J, Weintraud M, Kapral S, Kettner S. Epidural catheter placement in neonates: sonoanatomy and feasibility of ultrasonographic guidance in term and preterm neonates. Reg Anesth Pain Med. 2007;32:34–40. doi: 10.1016/j.rapm.2006.10.008. [DOI] [PubMed] [Google Scholar]


