Summary
Background
Circulation plays an essential role in tissue healing. Moist heat and warm water immersion have been shown to increase skin circulation; however, these heating modalities can cause burns. Recent research has shown that passive vibration can also increase circulation but without the risk of burns.
Material/Methods
The aim of this study is to compare the effects of short-duration vibration, moist heat, and a combination of the two on skin blood flow (SBF) and skin temperature (ST). Ten (10) subjects, 5 female and 5 male, aged 20–30 years of age, received two interventions a day for 3 consecutive days: Intervention 1 – Active vibration only (vibration exercise), Intervention 2 – passive vibration only, Intervention 3 – moist heat only, Intervention 4 – passive vibration combined with moist heat, Intervention 5 – a commercial massaging heating pad, and Intervention 6 – no intervention, resting in supine only (control). SBF and ST were measured using a laser Doppler imager during the 10 minute intervention and then throughout the nine minute recovery period.
Results
The mean skin blood flow following a ten-minute intervention of the combination of passive vibration and moist heat was significantly different from the control, active vibration, and the commercial massaging heating pad. Skin temperature following the ten-minute interventions of moist heat alone and passive vibration alone were both significantly different from the commercial massaging heating pad and active vibration interventions.
Conclusions
The combination of passive vibration and moist heat produced the greatest increase in skin blood flow and the second highest increase in skin blood flow nine minutes post application.
Keywords: whole body vibration, skin blood flow, skin temperature, vibration, moist heat
Background
Whole body vibration (WBV) has received a great deal of attention with reported increases in muscular strength [1–5], improvements in body composition [3,4,6], changes in muscle performance and balance [7–10], increases in lower back and hamstring flexibility [11], improvements in human athletic performance such as improvement in jumping and running parameters [1,9,12,13], and changes in peripheral circulation [14]. These reported changes in peripheral circulation occurred without significantly stressing the cardiovascular system [15]. Standing on a platform, vibrating at 26 Hz for 9 minutes, increased relative moving blood volume of the quadriceps and gastrocnemius muscles and popliteal artery mean blood flow with a decrease of flow resistance [14]. Oxygen utilization rates during exercise have been shown to be increased with WBV[16].
A study conducted by Lohman et al. (2007) documented significant transient increases in skin blood flow due to a short duration (3 minutes) of high-amplitude (5–6 mm), high-frequency vibration (30 Hz) mechanically delivered to the posterior calf muscles with the subjects in a relaxed supine position. A follow up study focusing on passive vibration applied to the forearm muscles demonstrated that both 30 Hz and 50 Hz vibration significantly increased skin blood flow; however, 50 Hz was more efficient and gains lasted during the entire 15 minute recovery period [17]. The authors found that blood flow peaked at 5 minutes; with no added benefits from an additional 5 minutes of vibration application [15]. Hazell et al. (2008) reported that increases in skin temperature occur after 8 minutes of lower extremity vibration exercise. Significant increases in skin blood flow were also reported after 12 minutes of vibration exercise [15]. Both skin temperature and skin blood flow remained elevated during the 10 minute recovery period [15]. Noticeable extremity erythema has been reported in numerous studies following vibration exercise [13,14].
The vast majority of WBV studies have involved vertically directed mechanical stimuli (25 to 50Hz) in standing or combined with vibration exercise. For this study, we have coined the term “active vibration” for this form of vibration intervention. One vascular study applied vertical vibration in the supine position (head-to-toe whole body acceleration) using a lower frequency (2 Hz) [18]. To date, there have been a small number of studies that have examined the effects of WBV on circulation with the subject resting and the target area receiving horizontal vibration. The mechanical sinusoidal vibration was delivered at a right angle to the long bones of the extremity, blood vessels, and muscle fibers [17,19]. For this study, we have coined the term “passive vibration” for horizontally delivered vibration to specific body regions in the relaxed subject because the subject is not receiving vibration to the whole body nor are they active in the process. The active process is when the subject stands on the platform, holding the safety handles, and is not relaxed. The active process involves whole body weight bearing while the passive process is not whole body weight bearing.
Impaired autonomic and endothelial function is attributed to the aging and disease processes such as Diabetes Mellitus [20]. Circulation plays an essential role in maintaining healthy integumentary system function and promotion of tissue healing [19]. Local heating, such as moist heat hydrocollator packs (hot packs) and warm water immersions increase circulation in healthy individuals. Increased blood flow has been shown to increase tissue nutrients, decrease susceptibility to infection, improve wound healing, and facilitate soft tissue repair [21–23]. It is well established that when heat is applied to the skin there is an increase in skin blood flow [24–26]. Initially, after the application of local heat, tactile neurons in the skin release Substance P and Calcitonin Gene Related Peptide which causes an increase in potassium permeability in vascular smooth muscle surrounding the endothelial cell [24,27–29]. This then, in turn, causes an increase in blood flow. But this response only lasts a few minutes. The sustained response to increasing temperature in the skin is mediated by Transient Receptor Potential Vanilloid-4 (TRPV-4) voltage gated calcium channels in the vascular endothelial cells [30,31]. Above a temperature of 35°C, these cells cause an exponential increase in calcium influx into the endothelial cell from the interstitial space. Calcium activates the enzyme nitric oxide synthetase producing endothelial nitric oxide [26]. Nitric oxide, a potent vasodilator, diffuses into the surrounding smooth muscle activating cyclic GMP which in turn increases potassium permeability and relaxes vascular smooth muscle [28,29,32–34].
Moist heat is more effective than dry heat at raising tissue temperature, but moist heat does have a greater risk of causing a skin burn [35,36]. However, all heating modalities do have a risk of possible burns [37]. This is especially true in individuals with compromised circulation who would benefit most from modalities that increase skin circulation. To achieve these therapeutic benefits, moist heat must be applied for a minimum of 10 minutes. According to Prentice (2002), it takes approximately 10 minutes of superficial therapeutic moist heat to reach a maximum heating depth of up to 1 cm below the skin [37].
The purpose of our study is to determine the effects of short-term exposure to vibration versus moist heat (alone and combined) on lower extremity skin blood flow and skin temperature. Our hypothesis is that skin blood flow will increase following short-term, low frequency vibration under the treatment site for all interventions except for active vibration (vibration exercise) as compared to the control intervention. We hypothesize skin blood flow and skin temperature at the calf will rank as following (most to least): 1) Passive vibration combined with moist heat, 2) moist heat only, 3) passive vibration only, 4) commercial massaging (“vibrating”) heating pad, 5) active vibration, and 6) control. Furthermore, it is hypothesized that with the combination of moist heat and vibration, local skin temperature will increase at a slower rate than with moist heat alone due to increased circulation and decreased skin impedance provided by passive vibration.
Material and Methods
Subjects
The subjects included 10 healthy adult volunteers aged 20–30 years (mean = 25.7 years) from the Loma Linda University community. Five females (age = 25.8±4.1 years; weight = 53.8 ±6.1 kg.; height = 160.6±3.2 cm) and five males (age = 25.6±1.5 years; weight = 67.8±11.3 kg; height = 168.9±8.7 cm) participated in the study.
The subjects received the following interventions on three separate days to the posterior calf region: Intervention 1 – active vibration (vibration exercise) only, Intervention 2 – passive vibration only, Intervention 3 – moist heat only, Intervention 4 – passive vibration combined with moist heat, Intervention 5 – a commercially marketed, over the counter massaging heating pad, and Intervention 6 – the control intervention (no intervention). The six interventions were randomly assigned for each subject. Two interventions were applied each day, one intervention to each leg. The Institutional Review Board at Loma Linda University approved all of the procedures and all subjects signed a statement of informed consent. All subjects were free of neurological, orthopedic, and circulatory disorders (e.g., deep vein thrombophlebitis, bleeding disorders) that which would have limited their participation in the study. Pregnant subjects and subjects with pacemakers or skin ulcers were also excluded from this study. These exclusion parameters were determined through a subjective interview and a brief physical examination.
Laser Doppler
Skin blood flow was measured by a laser Doppler flow meter (Figures 1 and 2) produced by BioPac, Inc. (Goleta, California). The device was secured with hypo-allergic tape to the middle of the gastrocnemius muscle belly. This device is a completely non-invasive device. The error on repeat measurements is less than 5% from day to day [38]. Subjects were placed in the supine position with the lower limbs elevated 10 cm. The units of blood flow stated in the results are in “flux” units, the measure of flow generated by laser Doppler systems.
Figure 1.

Laser Doppler Flow Meter and Skin Thermoster.
Figure 2.
Biopac System.
Skin temperature
A thermoster (BioPac, Inc. Goleta, California) was used to record skin temperature. The thermoster was placed within 2 cm of the Doppler probe (Figures 1 and 2).
Whole body vibration
The mechanical stimulation of WBV was provided by a Power Plate® for five of the subjects. The Power Plate® is a vibration platform (Power Plate® North America, LLC, Culver City, California, USA), as shown in Figure 3, with frequency settings ranging from 30–50 Hz. The Power Plate® has an option for either low amplitude (2–3 mm) or high amplitude (5–6 mm) plate oscillations [39]. A frequency of 40–50 Hz with low or high amplitude is recommended for massage and non-weight bearing activities [40,41]. For this study, the vibration parameters were set at a frequency of 50 Hz, an amplitude of a0=5–6 mm (high amplitude), and therefore a peak acceleration of approximately 62.40 m/s2 (6.24 g). The other five subjects received vibration interventions from a similar vibration platform, the Globus Physioplate®, using the same settings. A 2 cm rubber pad was used to reduce friction to the skin during massage related vibration techniques. This also reduces the amplitude by approximately 1–2 mm; however, frequency is unchanged. This slightly reduced the overall gravitational force applied to the lower extremity.
Figure 3.

Power Plate Vibration Platform.
Moist heat
Moist heat was supplied by a commercial hydrocollator heat pack from an approximately 160°F water tank with a heating unit. The hydrocollator pack is a canvas-covered pouch, filled with hydrophilic substances such as petroleum distillate or bentonite that provides superficial therapeutic moist heat up to 1 cm below the skin [37]. It takes approximately 10 minutes for the maximum depth of 1 cm tissue heating to occur [37]. According to Prentice (2002), the therapeutic temperature range is approximately 86 to 104°F. The canvas cover is used with 6–8 layers of dry towels between the subject’s skin and the hydrocollator pack to avoid skin burns [37]. Commercial terry cloth covers provides approximately 4 thicknesses of toweling [37]. Chattanooga™ Hydrocollator® hot packs and covers were used in this study.
Typically, subjects do not lay on the hydrocollator pack. In this case, the weight of the leg is relatively low so the patient’s calf was placed on top of the hydrocollator pack. As an example, a 90 kg-male-subject’s lower leg will produce approximately 5.44 kg of force over a surface area of approximately 24 cm2 or 0.23 kg/cm2.
Sunbeam® Health at Home® Massaging Heating Pad
This commercial heating pad product, powered by 120-Volt AC, provides a “massaging (vibration) heat” with either a dry or moist heat option. To create the moist heat option for this study, the product sponge was saturated in warm water and then gently wrung out before attaching the sponge under the cloth heating pad cover. Both the heat and massage (vibration) settings were set to “high” for this study. The vibration characteristics are that the unit runs at 35 watts and at 0.3 Amps at 120 volts. The temperature at the surface of this product ranged from 90.7 to 93.6°F after 10 minutes of use at the high settings of both massage and heat. This temperature range is at the lower half of the therapeutic temperature range of 86 to 104°F [37].
Procedures
Subjects who meet the inclusion/exclusion criteria were given an invitation to participate in this study and signed an informed consent document prior to participation. The subjects were led into an environmental room where room temperature was regulated between 72 to 75°F. Humidity was controlled between 35 and 40%. The subjects were placed in a prone position on a horizontally positioned plinth. The room was pre-warmed to 72–75°F for at least 30 minutes so that all tables and walls temperatures were constant. The skin was marked with skin-safe ink on the muscle belly of the gastrocnemius muscles to insure that the Doppler flow readings were measured at the same location on all three test days. The subjects rested comfortably for a ten-minute rest period prior to Doppler testing.
Following the initial rest period and without repositioning the subject, a Homan’s sign test was performed to help rule out the possibility of a deep vein thrombosis. The subject’s ankle was passively dorsiflexed while assessing for pain in the posterior aspect of the calf. Pallor, swelling, tenderness, and warmth to palpation of the posterior lower limb were also assessed bilaterally. These signs and symptoms are indicative of a possible deep vein thrombosis, thromboembolism, or superficial thrombophlebitis; which are contraindications for WBV. A positive finding of any of the above procedures served as exclusion from this study.
The subjects were then repositioned to the supine position with their calf muscles elevated approximately 10 cm. A baseline Doppler skin blood flow and skin temperature readings were taken in this position. The subjects received two of the following interventions for 10 minutes each, per day, over a three day period: 1) Standing on Power Plate® (active vibration), 2) a passive calf massage with the calf resting on the Power Plate® or Globus Physioplate® (passive vibration), 3) moist heat, 4) a combination of passive vibration and moist heat, 5) Sunbeam® massaging heating pad, and 6) no intervention, resting in supine (control). An intervention was applied to the right and left posterior calf each day (at approximately the same time of day) to allow for all six interventions to be tested in a three day period without retesting the same extremity on any one day. Refer to Table 1 for a description of the six interventions. During the heat interventions, if the subject became too warm anytime during the 10-minute intervention or if the skin became excessively blotchy at the 5-minute inspection, an additional layer of toweling was added. Additional toweling was added in order to prevent a skin burn.
Table 1.
Therapeutic procedure parameters description by intervention.
| Number | Intervention | Position & Parameters | Hydrocollator Hot Pack | WBV |
|---|---|---|---|---|
| Intervention 1 | Vibration – Active | Subjects stand with one foot on a firm vibration platform and the other on a firm wooden box for 10 minutes. Next the subject will rest supine with their calf elevated 2 cm above the platform with a support under the heel for an additional 10 minutes. | No | WBV: 50 HZ, 5–6 mm amplitude oscillations, 10 exposures of 60 seconds. |
| Intervention 2 | Vibration – Passive | Subject resting in supine with lower leg elevated 10cm with calf resting on a firm vibration platform for 10 minutes. Then the calf will be elevated 2 cm above the platform with a support under the heel for an additional 10 minutes. | No | WBV: 50 HZ, 5–6 mm amplitude oscillations, 10 exposures of 60 seconds. |
| Intervention 3 | Moist heat | Subject resting in supine with lower leg elevated 10cm with calf resting on a firm platform for 10 minutes. Then the calf will be elevated 2 cm above the platform with a support under the heel for an additional 10 minutes. | The subject’s posterior calf will rest on the hydro-collator with the equivalent to 6 layers of toweling. The subject will be instructed to move lower leg off of hydrocollator pack if too warm. The subject’s skin will be inspected at 5 and 10 minutes. | No |
| Intervention 4 | Vibration – Passive & Moist Heat | Subject resting in supine with lower leg elevated 10cm with calf resting on a firm vibration platform for 10 minutes. Then the calf will be elevated 2 cm above the platform with a support under the heel for an additional 10 minutes. | The subject’s posterior calf will rest on the hydro-collator with the equivalent to 6 layers of toweling. The subject will be instructed to move lower leg off of hydrocollator pack if too warm. The subject’s skin will be inspected at 5 and 10 minutes. | WBV: 50 HZ, 5–6 mm amplitude oscillations, 10 exposures of 60 seconds. |
| Intervention 5 | Commercial massaging heating pad | Subject resting in supine with lower leg elevated 10cm with calf resting on a firm platform for 10 minutes. Then the calf will be elevated 2 cm above the platform with a support under the heel for an additional 10 minutes. | The subject’s posterior calf will rest on the Sunbeam® massaging heating pad with the manufacture’s recommended toweling. The subject will be instructed to move lower leg off of heating pad if too warm. The subject’s skin will be inspected at 5 and 10 minutes. | Vibration setting: High Temperature setting: High Duration: 10 minutes |
| Intervention 6 | Control | Subject resting in supine with lower leg elevated 12 cm with posterior calf elevated 2 cm above a firm, stationary platform for 20 minutes. | No | No |
Once the therapeutic intervention was completed, the subject’s skin blood flow and temperatures were recorded for an additional nine minutes. During this time period the posterior calf was elevated approximately 2 cm above the platform (a small bolster under the subject’s heel) to prevent skin contact with the residual warmth from the heating modality on the surface of the platform. This procedure assured avoidance of continued heating of the skin during the nine post-intervention assessments.
Data analysis
Demographics and baseline characteristics were summarized using descriptive statistics. Friedman’s ANOVA was used to test for changes in temperature and blood flow between the different modalities. The level of significance was set at p<0.05. Wilcoxon tests were used to follow-up any findings that were significant.
Results
Skin blood flow
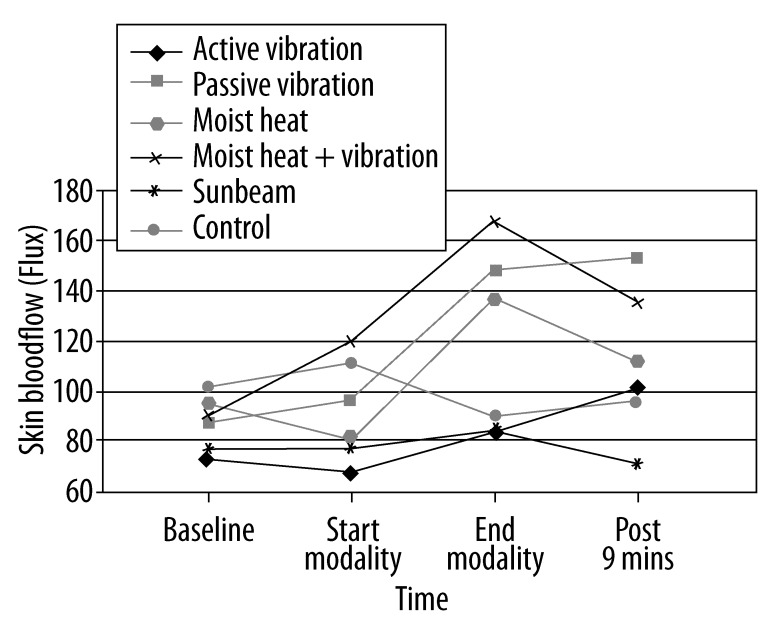
Changes in mean skin blood flow across time during the different modalities are represented in Figure 4 and Tables 2–4. For the passive vibration modality, there was a significant increase in mean skin blood flow from baseline to 9 minutes post-intervention (88.3±16.9 Flux vs. 150.5±40.4 Flux) (p=0.01). This increase in skin blood flow was also significant from the start of the intervention to 9 minutes post-intervention (96.6±52.5 Flux vs. 150.5±40.4 Flux) (p=0.03). At the end of the intervention, mean skin blood flow was significantly higher in the moist heat and passive vibration combination intervention than compared to the Sunbeam (commercial massaging heating pad) intervention (163.9 Flux ± 71.8 vs. 85.0±28.6 Flux);(p=.01), control (163.9 Flux ±71.8 vs. 90.0±56.8 Flux); (p=.04), and active vibration (163.9 Flux ±71.8 vs. 84.3±40.8 Flux); (p=.04). These differences remained significant at 9 minutes post-intervention. The moist heat and passive vibration combination intervention had significantly higher skin blood flows than both the Sunbeam intervention (133.7±46.1 Flux vs. 73.0±18.7 Flux); (p=.01) and the control intervention (133.7±46.1 Flux vs. 96.7±39.1 Flux); (p=.04). In addition, at 9 minutes post-intervention, mean skin blood flow was significantly higher in the passive vibration intervention than the moist heat intervention (150.5±40.4 Flux vs. 135.2±95.1 Flux);(p=.04) and Sunbeam intervention (150.5±40.4 Flux vs. 73.0±18.7 Flux); (p=.01).
Figure 4.
Mean skin blood flow across time with the different interventions.
Table 2.
Mean skin blood flow (Flux) ±(SD) across time for each intervention.
| Modality (M) | Baseline (B) | Start (S) | End (E) | 9 minutes post M (9) | p value | p value (B-E)* | p value (S-E)* | p value (B-9)* | p value (S-9)* |
|---|---|---|---|---|---|---|---|---|---|
| Active Vibration | 73.8 (16.7) | 69.7 (13.4) | 84.3 (40.8) | 101.0 (52.6) | .59 | ||||
| Passive Vibration | 88.3 (16.9) | 96.6 (52.5) | 145.2 (102.1) | 150.5 (40.4) | .02 | .11 | .11 | .01 | .03 |
| Moist Heat | 95.7 (35.0) | 82.0 (22.5) | 135.2 (95.1) | 111.3 (46.9) | .90 | ||||
| Moist Heat & Passive Vibration | 90.7 (27.8) | 118.4 (41.5) | 163.9 (71.8) | 133.7 (46.1) | .15 | ||||
| Sunbeam | 77.9 (40.7) | 78.8 (26.4) | 85.0 (28.6) | 73.0 (18.7) | .27 | ||||
| Control | 101.7 (40.8) | 110.5 (50.8) | 90.0 (56.8) | 96.7 (39.1) | .22 |
p value was calculated using Friedman’s ANOVA, when significant (p<0.05), p value is further expressed using Wilcoxon Signed Ranked test.
Table 4.
Mean blood flow (Flux) ±(SD) comparisons between interventions at 9 minutes post modality.
| Modality | Active vib 101.0 (52.6) | Passive vib 150.5 (40.4) | Moist heat 111.3 (46.9) | Passive plus moist heat 133.7 (46.1) | Sunbeam 73.0 (18.7) | Control 96.7 (39.1) |
|---|---|---|---|---|---|---|
| Active vib 101.0 (52.6) | ||||||
| Passive vib 150.5 (40.4) | 0.09 | |||||
| Moist heat 111.3 (46.9) | 0.52 | 0.04 | ||||
| Passive plus moist heat 133.7 (46.1) | 0.44 | 0.51 | 0.39 | |||
| Sunbeam 73.0 (18.7) | 0.11 | 0.01 | 0.06 | 0.01 | ||
| Control 96.7 (39.1) | 0.59 | 0.03 | 0.51 | 0.04 | 0.07 |
Wilcoxon Signed Ranks Test p<0.05
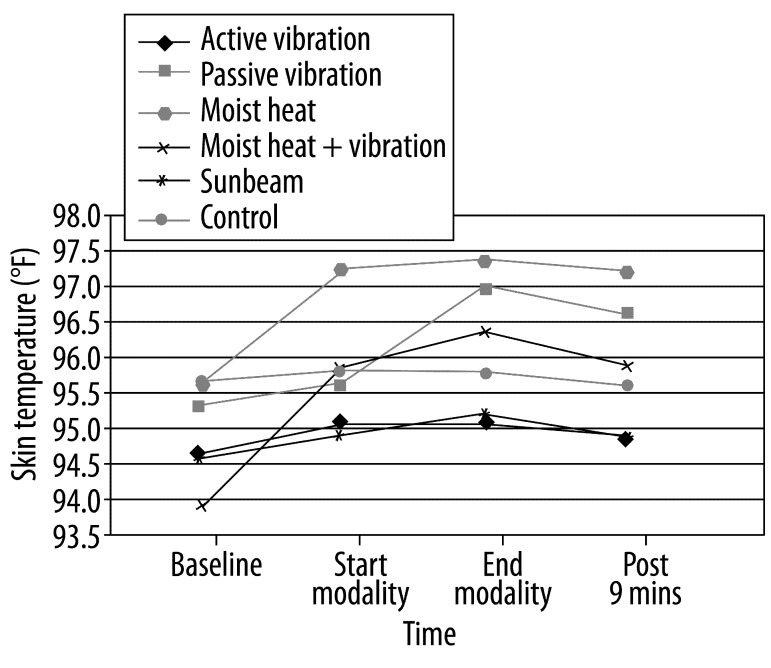
Skin temperature
Changes in mean skin temperature across time during the different interventions are represented in Figure 5 and Tables 5–7. In the passive vibration intervention, there was a significant increase in mean skin temperature from baseline to the end of the intervention (95.4±2.7 deg F vs. 97.0±2.8 deg F); (p=.02) and from baseline to 9 minutes post –intervention (95.4±2.7 deg F vs. 96.6±3.3 deg F); (p=.05). This increase in skin temperature was also significant from start of the intervention to the end of the intervention (95.7±3.1 deg F vs. 97.0±2.8 deg F); (p=.01). In the moist heat & passive vibration combination intervention, mean skin temperature at the end of the intervention (96.4±4.7 deg F) and 9 minutes post-intervention (95.9±4.6 deg F) were significantly higher than mean baseline skin temperature (94.0±4.6 deg F); (p=.01; p=.01 respectively).
Figure 5.
Mean skin temperature across time with the different modalities.
Table 5.
Mean skin temperature (°F) ±(SD) across time for each modality.
| Modality (M) | Baseline (B) | Start (S) | End (E) | 9 minutes post M (9) | p value | p value (B-E)* | p value (S-E)* | p value (B-9)* | p value (S-9)* |
|---|---|---|---|---|---|---|---|---|---|
| Active Vibration | 94.7 (3.8) | 95.1 (3.9) | 95.1 (3.8) | 95.0 (4.2) | .30 | ||||
| Passive Vibration | 95.4 (2.7) | 95.7 (3.1) | 97.0 (2.8) | 96.6 (3.3) | .01 | .01 | .01 | .05 | .07 |
| Moist Heat | 95.7 (2.9) | 97.3 (97.3) | 97.4 (5.3) | 97.2 (5.5) | .15 | ||||
| Moist Heat & Passive Vibration | 94.0 (4.6) | 95.9 (4.8) | 96.4 (4.7) | 95.9 (4.6) | .001 | .01 | .16 | .01 | .95 |
| Sunbeam | 94.6 (4.8) | 95.0 (4.7) | 95.2 (4.6) | 95.0 (5.2) | .18 | ||||
| Control | 95.7 (3.8) | 95.9 (3.8) | 95.8 (4.1) | 95.7 (4.4) | .85 |
p value was calculated using Friedman’s ANOVA, when significant (p<0.05), p value is further expressed using Wilcoxon Signed Ranked test
Table 7.
Mean skin temperature(°F) ± (SD) comparisons between interventions at 9 minutes post modality.
| Modality | Active vib 95.0 (4.2) | Passive vib 96.6 (3.3) | Moist heat 97.2 (5.5) | Passive plus moist heat 95.9 (4.6) | Sunbeam 95.0 (5.2) | Control 95.7 (4.4) |
|---|---|---|---|---|---|---|
| Active vib 95.0 (4.2) | ||||||
| Passive vib 96.6 (3.3) | .01 | |||||
| Moist heat 97.2 (5.5) | .02 | .44 | ||||
| Passive plus moist heat 95.9 (4.6) | .07 | 1.00 | .29 | |||
| Sunbeam 95.0 (5.2) | .95 | .07 | .02 | .20 | ||
| Control 95.7 (4.4) | .24 | .20 | .10 | .44 | .26 |
Wilcoxon Signed Ranks Test p<0.05
Mean skin temperature was significantly higher in the moist heat intervention at the end of the intervention compared to Sunbeam intervention (97.4±5.3 deg F vs. 95.2±4.6 deg F); (p=0.05) and active vibration interventions (97.4±5.3 deg F vs. 95.1±3.8 deg F); (p=.03). These differences remained significant at 9 minutes post-intervention with the moist heat intervention’s mean skin temperature being significantly higher than Sunbeam intervention (97.2±5.5 deg F vs. 95.0±5.2 deg F); (p=.02) and active vibration intervention (97.2±5.5 deg F vs. 95.0±4.2 deg F); (p=.02).
Disscussion
We hypothesized that local skin blood flow would increase while skin temperature would increase less with the combination of moist heat and passive vibration as compared to moist heat alone. We theorized this would be due to increased circulation and decreased skin impedance. The findings of this study supported this hypothesis.
After the ten-minute interventions, skin blood flow was significantly greater with the combination of passive vibration and moist heat as compared to active vibration, Sunbeam® massaging heating pad, and the control intervention. Although the combination of passive vibration and moist heat had a greater mean skin blood flow after a 10-minute intervention, it was not significantly different from either moist heat or passive vibration alone. Nine minutes after the 10-minute intervention, passive vibration alone had the highest mean skin blood (150.5 flux), followed by passive vibration plus moist heat (133.7 flux), and moist heat alone (111.3 flux).
The Sunbeam® massaging heating pad was turned on at the start of the intervention and began immediately to massage and also began warming. Since the skin blood flow measurements were recorded within the first minute (start) and immediately after the tenth minute of the intervention, this device may not have reached either its maximum heating potential at these data collection points. In fairness to the product, if this product is used in a follow up study, the product should be allowed to reach the maximum warmth prior to application to the subject or collecting data.
After the ten-minute interventions, mean skin temperature was highest with moist heat alone (97.4°F), followed closely by passive vibration alone (97.0°F). Mean skin temperature following ten-minute interventions of both passive vibration alone and moist heat alone was significantly different than active vibration. The control (95.8°F), Sunbeam® massaging heating pad (95.2°F), and active vibration (95.1°F) intervention had similar low skin temperatures at the end of the ten-minute intervention. The combination of moist heat and passive vibration (96.4°F) skin temperature was between these other interventions.
Nine minutes after the cessation of the interventions, mean skin temperature remained relatively unchanged for all interventions with the combination of passive vibration and moist heat having the greatest drop in skin temperature of only.5°F. The authors conclude that this lowered skin temperature is due to the high skin blood from the combination of moist heat and passive vibration.
The most plausible explanation for why skin blood flow was reduced during active vibration is that during high intensity exercise activities, the body directs blood away from the organs such as the skin and is redirected to the skeletal muscles [42]. Adrenal medulla regulated epinephrine release and sympathetic regulation results in vasodilation of skeletal muscle vessels [43] and vasoconstriction of the vessels of the epidermis and dermis. The muscle contractions necessary for skeletal movement and support during exercise are executed by muscle fibers that contain cells that must be supplied with nutrients (e.g., glucose) and oxygen by the capillaries. As nutrients and oxygen are supplied to the muscle cells during exercise, waste products (e.g., carbon dioxide) are also removed by the capillary system. At rest, approximately 20% of cardiac output is directed to skeletal muscle at a rate of 3 ml/minute per 100 mg of muscle mass [42,44]. At rest, only approximately 20% of capillaries in skeletal muscles are open. At the start of exercise, this rate of skeletal blood flow approaches 20 times the resting rate. During high intensity, endurance exercises (e.g., cross country skiing), skeletal muscle blood flow approaches 80% of cardiac output [45] and 100% of capillaries in skeletal muscles are open. This initial sympathetic regulated reduction of skin blood flow at the start of exercise is replaced by hypothalamus regulated skin vasodilation as body temperature increases. The exercise regimen performed in this study during active vibration was that of short duration activities.
In addition, active exercises were performed in standing with the vibratory forces being applied vertically through the soles of the shoes. During passive vibration, the vibratory forces were applied directly to the skin of the calf in a perpendicular direction. The muscles are relaxed and the skin is mechanically stressed resulting in shear stress-induced nitric oxide production.
One of the concerns with heat modality applications is the risk of increasing skin temperature to the point that a skin burn occurs. Skin temperature, with the combination of passive vibration and moist heat to the calf, was similar to and not significantly different from the control intervention at both the end of the intervention and nine minutes post intervention. Although not a thermal modality, passive vibration to the posterior calf increased skin temperature almost as much as moist heat which had the highest skin temperature at both the end of the application and nine minutes post application.
The three interventions in this study that produced significant increases in skin blood flow (SBF), ranked highest to lowest, include: 1) Passive vibration combined with moist heat, 2) passive vibration alone, and 3) moist heat alone. Of these top three SBF interventions, the rank order for skin temperature (ST), ranked highest to lowest, include: 1) Moist heat alone, 2) Passive vibration alone, and 3) Passive vibration combined with moist heat. These relatively low skin temperature increases with the combined intervention occurred at both the end of the intervention as well as nine minutes post-intervention. When considering an intervention that has the ability to increase skin blood flow to dissipate heat from the skin to the blood stream while having a relatively low increase in skin temperature, the combination of passive vibration and moist heat appears to be the superior intervention. There are no reports in literature to suggest any risk of a skin burn from the non-thermal modality of passive vibration. Anecdotally, prolonged passive vibration could potentially cause a friction rub that could cause skin irritation; however, this theoretical risk can be further reduced through the use of the 2cm rubber pad (skin-platform interface) provided by the manufacture. Since passive vibration alone does not possess the risk of a burn, this modality provides a safe alternative to moist heat to increase skin blood flow in individuals at risk for burns such as individuals with compromised skin blood flow.
Increased blood flow has been shown to increase tissue nutrients, decrease susceptibility to infection, improve wound healing, and facilitate soft tissue repair [21–23]. In our study, moist heat, passive vibration, and a combination of the two all provided increased skin blood flow. Of these three, moist heat alone increases skin temperature more than the other two modalities, suggesting that this modality may place individuals at a greater risk of a burn.
This study was performed on healthy, young individuals, free of Diabetes Mellitus. Consequently, this study does not provide direct applicability to the elderly and diabetic populations who have a greater prevalence of skin wounds due to decreased extremity circulation. A follow up study applying these modalities and methods to these vulnerable populations would be beneficial. Follow-up studies to compare passive vibration to warm water immersion on skin blood flow and temperature are also suggested. A study to determine the benefit of the combination of both of these modalities may also prove beneficial. A limitation to our study was our sample size. Future studies will have a power analysis conducted and will be taken into account.
Conclusions
The combination of passive vibration and moist heat produced the greatest increase in skin blood flow and the second highest skin blood flow at nine minutes post-intervention. These therapeutic benefits combined with relatively low increases in skin temperature, may make the combination of these two modalities an intervention of choice.
Table 3.
Mean blood flow (Flux) ±(SD) comparisons between interventions at end modality.
| Modality | Active vib 84.3 (40.8) | Passive vib 145.2 (102.1) | Moist heat 135.2 (95.1) | Passive plus moist heat 163.9 (71.8) | Sunbeam 85.0 (28.6) | Control 90.0 (56.8) |
|---|---|---|---|---|---|---|
| Active vib 84.3 (40.8) | 0.093 | 0.0386 | 0.037 | 0.959 | ||
| Passive vib 145.2 (102.1) | 0.09 | 0.959 | 0.646 | 0.203 | ||
| Moist heat 135.2 (95.1) | 0.39 | 0.96 | 0.333 | 0.203 | ||
| Passive plus moist heat 163.9 (71.8) | 0.04 | 0.65 | 0.33 | 0.005 | ||
| Sunbeam 85.0 (28.6) | 0.96 | 0.20 | 0.20 | 0.01 | ||
| Control 90.0 (56.8) | 0.72 | 0.11 | 0.14 | 0.04 | 0.65 |
Wilcoxon Signed Ranks Test p<0.05.
Table 6.
Mean skin temperature (°F) ± (SD) comparisons between interventions at end modality.
| Modality | Active vib 95.1 (3.8) | Passive vib 97.0 (2.8) | Moist heat 97.4 (5.3) | Passive plus moist heat 96.4 (4.7) | Sunbeam 95.2 (4.6) | Control 95.8 (4.1) |
|---|---|---|---|---|---|---|
| Active vib 95.1 (3.8) | 0.093 | 0.0386 | 0.037 | 0.959 | ||
| Passive vib 97.0 (2.8) | .01 | |||||
| Moist heat 97.4 (5.3) | .03 | .29 | ||||
| Passive plus moist heat 96.4 (4.7) | .07 | .72 | .51 | |||
| Sunbeam 95.2 (4.6) | .59 | .05 | .05 | .14 | ||
| Control 95.8 (4.1) | .14 | .20 | .11 | .26 | .20 |
Wilcoxon Signed Ranks Test p<0.05.
Footnotes
Source of support: Departmental sources
References
- 1.Delecluse C, et al. Effects of whole body vibration training on muscle strength and sprint performance in sprint-trained athletes. Int J Sports Med. 2005;26(8):662–68. doi: 10.1055/s-2004-830381. [DOI] [PubMed] [Google Scholar]
- 2.Delecluse C, Roelants M, Verschueren S. Strength increase after whole-body vibration compared with resistance training. Med Sci Sports Exerc. 2003;35(6):1033–41. doi: 10.1249/01.MSS.0000069752.96438.B0. [DOI] [PubMed] [Google Scholar]
- 3.Roelants M, Delecluse C, Verschueren SM. Whole-body-vibration training increases knee-extension strength and speed of movement in older women. J Am Geriatr Soc. 2004;52(6):901–8. doi: 10.1111/j.1532-5415.2004.52256.x. [DOI] [PubMed] [Google Scholar]
- 4.Roelants M, et al. Whole-body-vibration-induced increase in leg muscle activity during different squat exercises. J Strength Cond Res. 2006;20(1):124–29. doi: 10.1519/R-16674.1. [DOI] [PubMed] [Google Scholar]
- 5.Roelants M, et al. Effects of 24 weeks of whole body vibration training on body composition and muscle strength in untrained females. Int J Sports Med. 2004;25(1):1–5. doi: 10.1055/s-2003-45238. [DOI] [PubMed] [Google Scholar]
- 6.Vissers D, et al. Effect of long-term whole body vibration training on visceral adipose tissue: a preliminary report. Obes Facts. 2010;3(2):93–100. doi: 10.1159/000301785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Runge M, Rehfeld G, Resnicek E. Balance training and exercise in geriatric patients. J Musculoskelet Neuronal Interact. 2000;1(1):61–65. [PubMed] [Google Scholar]
- 8.Torvinen S. Effect of whole body vibration on muscluar performance, balance, and bone. University of Tampere; Finland: 2003. pp. 20–22. [Google Scholar]
- 9.Torvinen S, et al. Effect of a vibration exposure on muscular performance and body balance. Randomized cross-over study. Clin Physiol Funct Imaging. 2002;22(2):145–52. doi: 10.1046/j.1365-2281.2002.00410.x. [DOI] [PubMed] [Google Scholar]
- 10.Torvinen S, et al. Effect of four-month vertical whole body vibration on performance and balance. Med Sci Sports Exerc. 2002;34(9):1523–28. doi: 10.1097/00005768-200209000-00020. [DOI] [PubMed] [Google Scholar]
- 11.Di Giminiani R, et al. Effects of individualized whole-body vibration on muscle flexibility and mechanical power. J Sports Med Phys Fitness. 2010;50(2):139–51. [PubMed] [Google Scholar]
- 12.Paradisis G, Zacharogiannis E. Effects of whole-body vibration on sprint running kinetics and explosive strength performance. Journal of Sports Science and Medicine. 2007;6:44–49. [PMC free article] [PubMed] [Google Scholar]
- 13.Rittweger J, Beller G, Felsenberg D. Acute physiological effects of exhaustive whole-body vibration exercise in man. Clin Physiol. 2000;20(2):134–42. doi: 10.1046/j.1365-2281.2000.00238.x. [DOI] [PubMed] [Google Scholar]
- 14.Kerschan-Schindl K, et al. Whole-body vibration exercise leads to alterations in muscle blood volume. Clin Physiol. 2001;21(3):377–82. doi: 10.1046/j.1365-2281.2001.00335.x. [DOI] [PubMed] [Google Scholar]
- 15.Hazell TJ, et al. Inlfluence of acut vertical whole body vibrtaion on selected cardiac and vascular responses. Applied Physiology, Nutrition, and Metabolism. 2008:7–234. [Google Scholar]
- 16.Coza A, Nigg BM, Dunn FJ. Effects of Vibrations on Gastrocnemius Medialis Tissue Oxygenation. Med Sci Sports Exerc. 2011;43(3):509–15. doi: 10.1249/MSS.0b013e3181f2589f. [DOI] [PubMed] [Google Scholar]
- 17.Maloney-Hinds C, Petrofsky JS, Zimmerman G. The effect of 30 Hz vs. 50 Hz passive vibration and duration of vibration on skin blood flow in the arm. Med Sci Monit. 2008;14(3):CR112–16. [PubMed] [Google Scholar]
- 18.Sackner M, Gummels E, Adams JA. Nitric oxide is released into circulation with whole-body, periodic acceleration. Chest. 2005;127(1):30–39. doi: 10.1378/chest.127.1.30. [DOI] [PubMed] [Google Scholar]
- 19.Lohman EB, III, et al. The effect of whole body vibration on lower extremity skin blood flow in normal subjects. Med Sci Monit. 2007;13(2):CR71–76. [PubMed] [Google Scholar]
- 20.Petrofsky J, Lee S. The effects of type 2 diabetes and aging on vascular endothelial and autonomic function. Med Sci Monit. 2005;11(6):CR247–54. [PubMed] [Google Scholar]
- 21.Baker RJ, Bell GW. The effect of therapeutic modalities on blood flow in the human calf. J Orthop Sports Phys Ther. 1991;13(1):23–27. doi: 10.2519/jospt.1991.13.1.23. [DOI] [PubMed] [Google Scholar]
- 22.Bracciano AG. Physical agent modalities: theory and application for the occupational therapist. 2nd ed. Thorofare, NJ: SLACK; 2008. p. xvi.p. 300. [Google Scholar]
- 23.Halverson GA. Therapeutic heat and cold for athletic inuries. Physician and Sports Med. 1990;18:87–94. doi: 10.1080/00913847.1990.11710045. [DOI] [PubMed] [Google Scholar]
- 24.Petrofsky J, et al. Effects of contrast baths on skin blood flow on the dorsal and plantar foot in people with type 2 diabetes and age-matched controls. Physiother Theory Pract. 2007;23(4):189–97. doi: 10.1080/09593980701209295. [DOI] [PubMed] [Google Scholar]
- 25.Petrofsky JS, Laymon M. Heat transfer to deep tissue: the effect of body fat and heating modality. J Med Eng Technol. 2009;33(5):337–48. doi: 10.1080/03091900802069547. [DOI] [PubMed] [Google Scholar]
- 26.Wong BJ, Fieger SM. Transient receptor potential vanilloid type-1 (TRPV-1) channels contribute to cutaneous thermal hyperaemia in humans. J Physiol. 2010;588(Pt 21):4317–26. doi: 10.1113/jphysiol.2010.195511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Charkoudian N, et al. Effects of chronic sympathectomy on locally mediated cutaneous vasodilation in humans. J Appl Physiol. 2002;92(2):685–90. doi: 10.1152/japplphysiol.00758.2001. [DOI] [PubMed] [Google Scholar]
- 28.Charkoudian N, Fromy B, Saumet JL. Reflex control of the cutaneous circulation after acute and chronic local capsaicin. J Appl Physiol. 2001;90(5):–1860–64. doi: 10.1152/jappl.2001.90.5.1860. [DOI] [PubMed] [Google Scholar]
- 29.Minson CT, Berry LT, Joyner MJ. Nitric oxide and neurally mediated regulation of skin blood flow during local heating. J Appl Physiol. 2001;91(4):1619–26. doi: 10.1152/jappl.2001.91.4.1619. [DOI] [PubMed] [Google Scholar]
- 30.Watanabe H, et al. Heat-evoked activation of TRPV4 channels in a HEK293 cell expression system and in native mouse aorta endothelial cells. J Biol Chem. 2002;277(49):47044–51. doi: 10.1074/jbc.M208277200. [DOI] [PubMed] [Google Scholar]
- 31.Watanabe M, et al. Assessment of mechanical and thermal thresholds of human C nociceptors during increases in skin sympathetic nerve activity. Clin Neurophysiol. 2002;113(9):1485–90. doi: 10.1016/s1388-2457(02)00159-1. [DOI] [PubMed] [Google Scholar]
- 32.Charkoudian N, Rabbitts JA. Sympathetic neural mechanisms in human cardiovascular health and disease. Mayo Clin Proc. 2009;84(9):822–30. doi: 10.4065/84.9.822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Petrofsky J, et al. Dry heat, moist heat and body fat: are heating modalities really effective in people who are overweight? J Med Eng Technol. 2009;33(5):361–69. doi: 10.1080/03091900802355508. [DOI] [PubMed] [Google Scholar]
- 34.Petrofsky J, et al. Does skin moisture influence the blood flow response to local heat? A re-evaluation of the Pennes model. J Med Eng Technol. 2009;33(7):532–37. doi: 10.1080/03091900902952683. [DOI] [PubMed] [Google Scholar]
- 35.Abramson DI, et al. Comparison of wet and dry heat in raising temperature of tissues. Arch Phys Med Rehabil. 1967;48(12):654–61. [PubMed] [Google Scholar]
- 36.Erdman WJ, II, Stoner EK. Comparative heating effects of moistaire and hydrocollator hot packs. Arch Phys Med Rehabil. 1956;37(2):71–74. [PubMed] [Google Scholar]
- 37.Prentice WE. Therapeutic modalities for physical therapists. 2nd ed. New York: McGraw-Hill; 2002. p. xxii.p. 548. [Google Scholar]
- 38.Petrofsky JS, et al. Impairment in orthostatic tolerance during heat exposure in individuals with Type I and Type II diabetes. Med Sci Monit. 2005;11(4):CR153–59. [PubMed] [Google Scholar]
- 39.Ma C, et al. Empowering patients with essential information and communication support in the context of diabetes. Int J Med Inform. 2006;75(8):577–96. doi: 10.1016/j.ijmedinf.2005.09.001. [DOI] [PubMed] [Google Scholar]
- 40.Xie L, et al. [The in-vitro interferon-gamma release assay for the diagnosis of tuberculosis and Mycobacterium tuberculosis infections]. Zhonghua Jie He He Hu Xi Za Zhi. 2005;28(8):545–49. [PubMed] [Google Scholar]
- 41.Fivey D. Vibrate yourself to fitness. Successful Coaching. 2006;32:6–7. [Google Scholar]
- 42.Wilmore JH, Costill DL. Physiology of Sport and Exercise. 3rd ed. Champaign, IL: 2005. [Google Scholar]
- 43.Halliwill JR. Hypoxic regulation of blood flow in humans. Skeletal muscle circulation and the role of epinephrine. Adv Exp Med Biol. 2003;543:223–36. [PubMed] [Google Scholar]
- 44.Klabunde RE. Cardiovascular Physiology Concepts. Mar 29, 2007. [cited 2011 02/15]; Available from: http://www.cvphysiology.com/Blood%20Flow/BF015.htm.
- 45.Rhoades RA. Medical Physiology: Principles for Clinical Medicine. 3rd ed. Baltimore: Lippincott Williams&Wilkins; 2009. [Google Scholar]