Summary
Background
The aim of this study was to investigate whether the 3 different substances that can decrease the development of atherosclerosis – nebivolol, AVE 0991 and doxycycline – could at the same time diminish the level of inflammatory indicators interleukin-6 (IL-6), interleukin-12 (IL-12), serum amyloid A (SAA), and monocyte chemotactic protein-1 (MCP-1).
Material/Methods
Forty 8-week-old female apoE–knockout mice on the C57BL/6J background were divided into 4 groups and put on chow diet for 4 months. Three experimental groups received the same diet as a control group, mixed with AVE 0991 at a dose 0.58 μmol per kg of body weight per day, nebivolol at a dose 2.0 μmol per kg of body weight per day, and doxycycline at a dose 1.5 mg per kg of body weight per day. At the age of 6 months, the mice were sacrificed.
Results
All inflammatory indicators (MCP-1, IL-6, IL-12 and SAA) were diminished by AVE 0991. There was also a tendency to lower MCP-1, IL-6, IL-12 and SAA levels by nebivolol and doxycycline; however, it did not reach statistical significance.
Conclusions
Of the 3 presented substances, only AVE 0991 was able to diminish the rise of inflammatory markers. Therefore, drug manipulations in the renin-angiotensin-aldosterone axis seem to be the most promising in the future treatment of atherogenesis.
Keywords: atherosclerosis model, inflammatory markers, nebivolol, AVE 0991, doxycycline
Background
Although atherosclerosis was long thought to be mainly a degenerative disease, it is now well ascertained that its pathogenesis is inflammatory. The pivotal stage of atherogenesis is the antigen presentation by macrophages to T lymphocytes. This antigen could be a fragment of oxidized low-density lipoproteins “digested” by macrophages, heat shock protein 60, β2-glycoprotein I, or fragments of bacterial antigens. For interaction between the immunological cells, the presence of CD40 receptor on macrophages and its ligand CD40L on the surface of T lymphocytes are necessary. During the interaction between these cells an immunological type T helper 1 or Treg response arises. Th1 response and its mediators – interferon γ, tumor necrosis factor α, interleukin-1, interleukin-12 and interleukin-18 – enhance atherogenesis, whereas Treg response and its mediators – interleukin-10 and transforming growth factor β (TGF-β) – inhibit the development of atherosclerosis [1].
apoE-knockout mice played an important role in the history of a new theory of atherogenesis since there has been lack of unequivocal evidence of an important inflammatory component in atherogenesis. This evidence was delivered by a new technique – gene targeting – for the invention of which Mario R. Capecchi, Martin J. Evans and Oliver Smithies received the Nobel Prize in Physiology or Medicine in 2007.
This technique enabled the investigators to create apoE-knockout mice [2,3], an ideal animal model to test the influence of singular proteins participating in the inflammatory response on the development of atherosclerosis. These studies showed, for example, that the absence of only 1 cytokine, interferon γ (IFN-γ), reduced atherosclerosis by 60% [4]. The overexpression of adhesive molecules (vascular adhesion molecule 1 and intercellular adhesion molecule 1) at sites with atheromatous changes was also observed in apoE-knockout mice [5]. Monocyte chemotactic protein (MCP-1) was shown to play an important part in the progression of atheromatous lesions [6,7]. Moreover, it was observed that interleukin-18 knockout decreased atherosclerosis by 35% [8,9].
Finally, in apoE-knockout mice with severe combined immunodeficiency (SCID), atherosclerosis was reduced by 70% in comparison to the control group, due to a significantly lower number of lymphocytes in mice with SCID. It was demonstrated that transfer of T cells to these mice aggravated atherosclerosis by 164% [10].
Atherosclerosis is therefore a chronic inflammatory disease, in most cases initiated by hypercholesterolemia. Nowadays, hypercholesterolemia and inflammation are considered as “partners in crime”. The concept of atherosclerosis as inflammatory disease is fairly new, but it is already considered as an undisputable achievement of science and has particular therapeutic consequences [11–13].
Our goal was to investigate whether 3 different substances that can decrease the development of atherosclerosis – nebivolol, AVE 0991 and doxycycline [14–16] – could at the same time diminish the level of inflammatory indicators interleukin-6 (IL-6), interleukin-12 (IL-12), serum amyloid A (SAA), and monocyte chemotactic protein-1 (MCP-1).
Material and Methods
Animals
Forty female apoE-knockout mice on the C57BL/6J background were obtained from Taconic (Ejby, Denmark) [8]. Mice were maintained on 12-h dark/12-h light cycles in air-conditioned rooms (22.5±0.5°C, 50±5% humidity) and access to food and water ad libitum. All animal procedures were approved by the Jagiellonian University Ethics Committee on Animal Experiments (approval nr Zi/496/2009).
Protocol of studies
At the age of 8 weeks, mice were put on chow diet made by Ssniff (Soest, Germany) for 4 months. Three experimental groups (in each n=10) received the same diet as a control group, mixed with: AVE 0991 (a kind gift from Sanofi-Aventis Deutschland GmbH, Frankfurt am Main, Germany) at a dose 0.58 μmol per kg of body weight per day, or nebivolol (a kind gift from Janssen Pharmaceutica, Geel, Belgium) at a dose 2.0 μmol per kg of body weight per day, as well as doxycycline (Sigma Aldrich, St. Louis, MO, USA) at a dose 1.5 mg per kg of body weight per day [17–19].
At the age of 6 months, 1000 UI of Fraxiparine (Sanofi-Synthelabo, France) was injected i.p. and after 10 min mice were sacrificed in a chamber filled with carbon dioxide. The blood was collected from the right ventricle. Plasma was separated by centrifugation at 1000 × g at 4°C for 10 min and stored in −80°C [20].
Measurement of inflammatory mediators
Plasma levels of interleukin-6 (IL-6), interleukin-12 (IL-12) and serum amyloid A (SAA) (all from R&D Systems, Minneapolis, MN, USA) and macrophage chemotactic protein-1 (MCP-1) (BioSource, Camarillo, CA, USA) were measured using ELISA test [21].
Statistical analysis
Results are expressed as mean ±SEM. The nonparametric Mann-Whitney U test was used for statistical analysis of the data. P<0.05 was considered as statistically significant.
Results
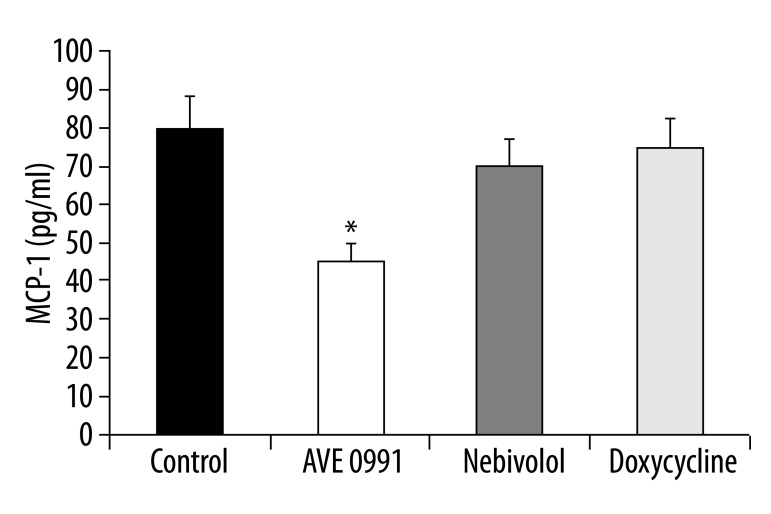
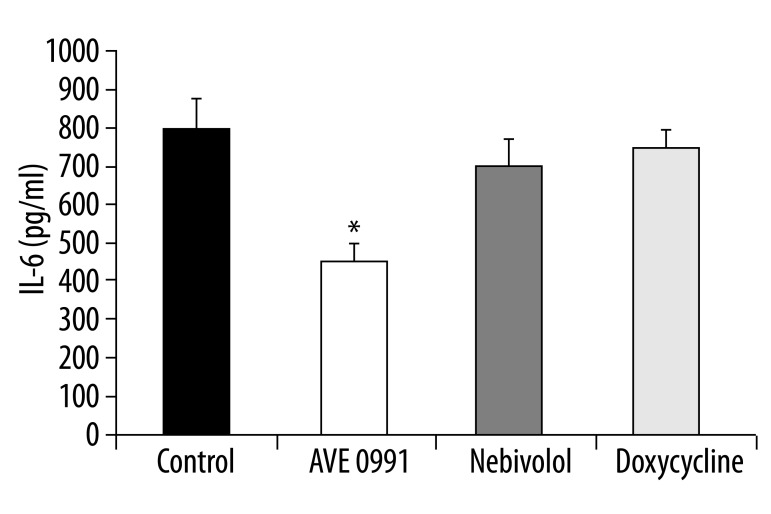
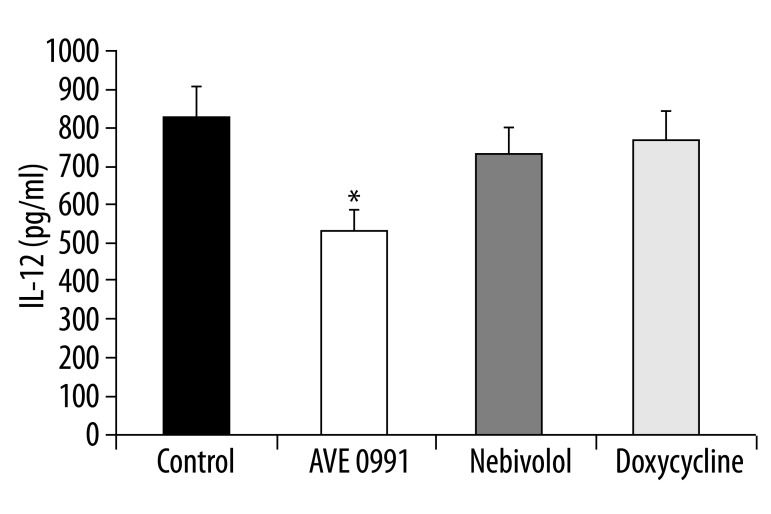
All inflammatory indicators: MCP-1, IL-6, IL-12 and SAA were diminished by AVE 0991. There was also a tendency to lower MCP-1, IL-6, IL-12 and SAA levels by nebivolol as well as by doxycycline; however, it did not reach statistical significance.
As regards MCP-1, the level was 78±9 pg/ml in the control group, 44±5 pg/ml (p<0.05) in the AVE 0991-treated group, 69±7 pg/ml (p>0.05) in the nebivolol-treated group, and 74±6 pg/ml (p>0.05) in the doxycycline-treated group.
As for IL-6, in control group the level was 792±76 pg/ml, in the AVE 0991-treated group it was 447±24 pg/ml (p<0.05), in the nebivolol-treated group it was 685±67 pg/ml (p>0.05), and in the doxycycline-treated group it was 714±69 pg/ml (p>0.05).
IL-12: in the control group the level was 845±95 pg/ml, in the AVE 0991-treated group it was 524±65 pg/ml (p<0.05), in the nebivolol-treated group it was 736±67 pg/ml (p>0.05), and in the doxycycline-treated group it was 774±86 pg/ml (p>0.05).
As for SAA, in control group the level was 17±3 μg/ml, in the AVE 0991-treated group it was 8±1 μg/ml (p<0.05), in the nebivolol-treated group it was 14±2 μg/ml (p>0.05), and in the doxycycline-treated group it was 16±2 μg/ml (p>0.05) (Figures 1–4).
Figure 1.
Plasma level of MCP-1 in all groups (n=10). * p<0.05, comparing to control group.
Figure 4.
Plasma level of SAA in all groups (n=10). * p<0.05, comparing to control group.
Discussion
Angiotensin II (Ang II) is involved in physiology and pathology of the cardiovascular system [22]. Recent evidence shows that the renin-angiotensin system is a crucial player in the atherosclerotic processes [23]. It was also proved that Ang II promotes atherogenesis. On the other hand, angiotensin-(1–7) [Ang-(1–7)] opposes Ang II action [24]. Therefore, we would like to find out whether angiotensin-(1–7) receptor agonist: AVE 0991, could ameliorate atherosclerosis progression in an experimental model of atherosclerosis: apolipoprotein E (apoE) – knockout mice [25].
The renin-angiotensin system (RAS) is a highly complicated hormonal system controlling the cardiovascular system, kidney and adrenal glands, and is thus crucial for hydro-electrolyte balance and blood pressure regulation [22]. Ang II is the best described peptide of RAS. Ang II increases activity of sympathetic nervous system, acts as a vasoconstrictor, and increases aldosterone release and sodium retention [26]. Additionally, Ang II stimulates free radical production, plasminogen activator inhibitor-1 (PAI-1) release, and expression of tissue factor (TF) and adhesion molecules (VCAM-1). Moreover, in blood vessels it stimulates smooth muscle cell proliferation and leukocyte adhesion. Importantly, Ang II inhibits nitric oxide synthase (NOS), thus diminishing all beneficial effects of nitric oxide (NO).
Ang-(1–7) is an active peptide of RAS. It counteracts vasoconstriction by releasing nitric oxide and prostacyclin. Moreover, it opposes Ang II mitogenic, arrhythmogenic and procoagulant activities [27]. Enhancing natriuresis and diuresis, it inhibits water and sodium retention caused by Ang II. Recently it has been shown that vasodilatative and diuretic activities of Ang-(1–7) are mediated via Mas, G-coupled protein receptor [28]. Furthermore, some activities of Ang-(1–7) are blocked by AT1 and AT2 receptors antagonists [29]. On the other hand, Ang-(1–7), independent of Mas-receptor, increases bradykinin activity and antagonizes hypertrophic action of Ang II [30]. In 2002 non-peptide antagonist of Ang-(1–7) receptor: AVE 0991 has been described [31–33].
Ang II has several potential mechanisms that may increase the atherogenic process [34]. First, Ang II may indirectly influence the atherogenic process via hemodynamic effects resulting from increased arterial blood pressure. Marked increases in arterial blood pressure have been demonstrated to increase the severity of experimental atherosclerosis. Second, Ang II has been demonstrated to exert several direct effects relevant to the development of atherosclerosis, including stimulation of monocyte recruitment, activation of macrophages, and enhanced oxidative stress, all of which have been linked to an increase in the atherogenesis process. These effects of Ang II occur independent of elevations in arterial blood pressure. In our experiment we have shown that AVE 0991 inhibits atherogenesis in a mouse model of atherosclerosis. This phenomenon is in agreement with general “anti-Ang II” action of Ang-(1–7). Since Ang II is a potent proatherogenic agent, its functional antagonist was able to diminish all markers of inflammation to a statistically significant degree.
The endothelium plays a crucial role in vessel wall homeostasis and its inflammatory and proliferative phenotype influences the progression of atherosclerosis [34]. Nebivolol, a novel third generation β1-selective antagonist has been shown to increase bioavailability of endothelium-derived nitric oxide (NO) and to attenuate inflammatory activation of endothelial cells [35]. Here, using an atherosclerosis model of apoE-knockout mice, we confirmed the anti-atherogenic action of nebivolol. Although the details of endothelial action remain unclear, it seems that nebivolol augments vascular nitric oxide release via endothelial β2- or β3-adrenergic receptors [36,37]. Furthermore, it was shown that nebivolol prevents vascular nitric oxide synthase (NOS) III uncoupling in experimental hyperlipidemia and inhibits NADPH oxidase activity in endothelial and inflammatory cells [37,38]. Recently, nebivolol appeared to be a potent antioxidant and has been shown to reduce expression of inflammatory adhesion molecules (ICAM-1, E-selectin) and cytokines (TNF-α, IL-6), as well as prothrombotic factors (PAI-1) on endothelial and smooth muscle cells [39]. Our preliminary data show that inhibition of atherogenesis by nebivolol in apoE knockout mice is associated with its tendency to decrease of plasma sICAM-1 and VCAM-1 levels (unpublished data). Furthermore, Baumhakel et al. reported that nebivolol, but not metoprolol, improved endothelial function of the corpus cavernosum in apoE-knockout mice [40]. Interestingly, the third generation of β-adrenoreceptor antagonists with ancillary vasodilator properties (nebivolol and carvedilol) possesses superior clinical efficacy as compared to the classical β-blockers [41,42]. This seems to be related not to their β-blocking properties, but to their ability to reverse endothelial dysfunction. Indeed, nebivolol, but not atenolol, reversed endothelial dysfunction in patients with heart failure and hypertension [43,44]. Our data showed an anti-atherogenic action of nebivolol. However, even though there was a tendency to diminish the level of inflammatory markers, it did not reach statistical significance.
Extracellular matrix (ECM) degradation is tightly regulated within the normal vessel wall through a balance between proteinases and their endogenous inhibitors. However, within the atherosclerotic plaque the balance may become shifted towards matrix degradation, since accumulating macrophages and phenotypically altered smooth muscle cells secrete a plethora of proteinases, including matrix metalloproteinases (MMPs) [45].
Although undetectable in normal arteries, MMP-1 expression has been localized to the fibrous cap and the shoulder regions of carotid atherosclerotic lesions [46]. In the latter tissue, the cellular sources of MMP-1 are mainly represented by macrophages, smooth muscle cell SMCs, and endothelial cells. Morphological analysis of the plaques have, in addition, revealed higher MMP-1 transcript levels in carotid lesions with a large lipid core and thin fibrous cap as compared with fibrous lesions with thick fibrous caps [47]. The latter findings suggest an increased MMP-1 expression associated with plaque vulnerability, which has also been supported by the MMP-1 messenger RNA (mRNA) levels detected in carotid lesions derived from patients with recent ischemic manifestations. Finally, a study of carotid lesions derived from patients undergoing repeated vascular intervention has shown that an increased MMP-1 expression correlated with the more foam cell-dominated late lesions compared with early restenotic lesions, which were characterized by increased SMC content [48]. Taken together, these studies support a role of MMP-1 derived from inflammatory cells in ECM degradation associated with plaque rupture [49].
Exogenous synthetic inhibitors generally contain a chelating group that binds the catalytic zinc atom in the enzyme active site. Doxycycline, already at sub-antimicrobial doses, inhibits MMPs activity, and has been used in various experimental setups for this purpose [50]. It is used clinically for the treatment of periodontal disease and is the only MMP inhibitor that is widely available clinically [51,52]. MMPs have been also considered as putative therapeutic targets in the prevention of atherogenesis.
In experiments made by Madan et al., there was a positive effect of doxycycline on atherogenesis in a special apoE heterozygote murine model infected with Porphyromonas gingivalis[53]. Therefore, our data, provided on apoE-knockout mice, broaden the current knowledge about the positive effect of doxycycline in sub-antimicrobial doses on atherogenesis. Here, as in the case of nebivolol, there was a tendency to diminish the level of inflammatory markers, which, however, did not reach statistical significance.
Conclusions
From the 3 checked substances – AVE 0991, nebivolol and doxycycline – that were able to inhibit atherosclerosis (an inflammatory disease), only AVE 0991 was at the same time able to diminish the rise of inflammatory markers. Therefore, drug manipulations in the renin-angiotensin-aldosterone axis seem to be the most potent and promising in the future treatment of atherogenesis.
Figure 2.
Plasma level of IL-6 in all groups (n=10). * p<0.05, comparing to control group.
Figure 3.
Plasma level of IL-12 in all groups (n=10). * p<0.05, comparing to control group.
Footnotes
Source of support: This study was supported by National Center of Science (NCN) grant nr: N N401 548340 for the years 2011–2012
References
- 1.Libby P, Ridker PM, Hansson GK. Progress and challenges in translating the biology of atherosclerosis. Nature. 2011;473(7347):317–25. doi: 10.1038/nature10146. [DOI] [PubMed] [Google Scholar]
- 2.Piedrahita JA, Zhang SH, Hagaman JR, et al. Generation of mice carrying a mutant apolipoprotein E gene inactivated by gene targeting in embryonic stem cells. Proc Natl Acad Sci. 1992;89(10):4471–75. doi: 10.1073/pnas.89.10.4471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Plump AS, Smith JD, Hayek T, et al. Severe hypercholesterolemia and atherosclerosis in apolipoprotein E – deficient mice created by homologous recombination in ES cells. Cell. 1992;71(2):343–53. doi: 10.1016/0092-8674(92)90362-g. [DOI] [PubMed] [Google Scholar]
- 4.Gupta S, Pablo AM, Jiang X, et al. IFN-gamma potentiates atherosclerosis in ApoE knock-out mice. J Clin Invest. 1997;99(11):2752–61. doi: 10.1172/JCI119465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nakashima Y, Raines EW, Plump AS, et al. Upregulation of VCAM-1 and ICAM-1 at atherosclerosis-prone sites on the endothelium in the ApoE-deficient mouse. Arterioscler Thromb Vasc Biol. 1998;18(5):842–51. doi: 10.1161/01.atv.18.5.842. [DOI] [PubMed] [Google Scholar]
- 6.Aiello RJ, Bourassa PA, Lindsey S, et al. Monocyte chemoattractant protein-1 accelerates atherosclerosis in apolipoprotein E-deficient mice. Arterioscler Thromb Vasc Biol. 1999;19(6):1518–25. doi: 10.1161/01.atv.19.6.1518. [DOI] [PubMed] [Google Scholar]
- 7.Ni W, Egashira K, Kitamoto S, et al. New anti-monocyte chemoattractant protein-1 gene therapy attenuates atherosclerosis in apolipoprotein E-knockout mice. Circulation. 2001;103(16):2096–101. doi: 10.1161/01.cir.103.16.2096. [DOI] [PubMed] [Google Scholar]
- 8.Elhage R, Jawien J, Rudling M, et al. Reduced atherosclerosis in interleukin-18 deficient apolipoprotein E-knockout mice. Cardiovasc Res. 2003;59(1):234–40. doi: 10.1016/s0008-6363(03)00343-2. [DOI] [PubMed] [Google Scholar]
- 9.Tenger C, Sundborger A, Jawien J, Zhou X. IL-18 accelerates atherosclerosis accompanied by elevation of IFN-gamma and CXCL16 expression independently of T cells. Arterioscler Thromb Vasc Biol. 2005;25(4):791–96. doi: 10.1161/01.ATV.0000153516.02782.65. [DOI] [PubMed] [Google Scholar]
- 10.Zhou X, Nicoletti A, Elhage R, Hansson GK. Transfer of CD4(+) T cells aggravates atherosclerosis in immunodeficient apolipoprotein E knockout mice. Circulation. 2000;102(24):2919–22. doi: 10.1161/01.cir.102.24.2919. [DOI] [PubMed] [Google Scholar]
- 11.Cymerys M, Bogdański P, Pupek-Musialik D, et al. Influence of hypertension, obesity and nicotine abuse on quantitative and qualitative changes in acute-phase proteins in patients with essential hypertension. Med Sci Monit. 2012;18(5):CR330–36. doi: 10.12659/MSM.882740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chhabra A, Aronow W, Ahn C, et al. Incidence of new cardiovascular events in patients with and without peripheral arterial disease seen in a vascular surgery clinic. Med Sci Monit. 2012;18(3):CR131–34. doi: 10.12659/MSM.882517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Karwowski W, Naumnik B, Szczepański M, Myśliwiec M. The mechanism of vascular calcification – a systematic review. Med Sci Monit. 2012;18(1):RA1–11. doi: 10.12659/MSM.882181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kus K, Gajda M, Pyka-Fosciak G, et al. The effect of nebivolol on atherogenesis in apoE – knockout mice. J Physiol Pharmacol. 2009;60(4):163–65. [PubMed] [Google Scholar]
- 15.Toton-Zuranska J, Gajda M, Pyka-Fosciak G, et al. AVE 0991 – angiotensin-(1–7) receptor agonist, inhibits atherogenesis in apoE-knockout mice. J Physiol Pharmacol. 2010;61(2):181–83. [PubMed] [Google Scholar]
- 16.Pawłowska M, Gajda M, Pyka-Fościak G, et al. The effect of doxycycline on atherogenesis in apoE-knockout mice. J Physiol Pharmacol. 2011;62(2):247–50. [PubMed] [Google Scholar]
- 17.Elhage R, Gourdy P, Jawien J, et al. The atheroprotective effect of 17b-estradiol depends on complex interactions in adaptive immunity. Am J Pathol. 2005;167(1):267–74. doi: 10.1016/s0002-9440(10)62971-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jawien J, Gajda M, Mateuszuk L, et al. Inhibition of nuclear factor-kappaB attenuates artherosclerosis in apoE/LDLR – double knockout mice. J Physiol Pharmacol. 2005;56(3):483–89. [PubMed] [Google Scholar]
- 19.Szczeklik A, Jawien J. Immunoglobulin E in acute phase response to surgical stress. Clin Exp Allergy. 1996;26(3):303–7. [PubMed] [Google Scholar]
- 20.Olszanecki R, Jawien J, Gajda M, et al. Effect of curcumin on atherosclerosis in apoE/LDLR – double knockout mice. J Physiol Pharmacol. 2005;56(4):627–35. [PubMed] [Google Scholar]
- 21.Jawien J, Gajda M, Rudling M, et al. Inhibition of five lipoxygenase activating protein (FLAP) by MK-886 decreases atherosclerosis in apoE/LDLR – double knockout mice. Eur J Clin Invest. 2006;36(3):141–46. doi: 10.1111/j.1365-2362.2006.01606.x. [DOI] [PubMed] [Google Scholar]
- 22.Kramkowski K, Mogielnicki A, Buczko W. The physiological significance of the alternative pathways of angiotensin II production. J Physiol Pharmacol. 2006;57(4):529–39. [PubMed] [Google Scholar]
- 23.Montecucco F, Pende A, Mach F. The renin-angiotensin system modulates inflammatory processes in atherosclerosis: evidence from basic research and clinical studies. Mediators Inflamm. 2009;2009:752406. doi: 10.1155/2009/752406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Daugherty A, Manning MW, Cassis LA. Angiotensin II promotes atherosclerotic lesions and aneurysms in apolipoprotein E-deficient mice. J Clin Invest. 2000;105(11):1605–12. doi: 10.1172/JCI7818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jawien J, Nastalek P, Korbut R. Mouse models of experimental atherosclerosis. J Physiol Pharmacol. 2004;55(3):503–17. [PubMed] [Google Scholar]
- 26.Lu P, Liu H, Yin H, Yang L. Expression of angiotensinogen during hepatic fibrogenesis and its effect on hepatic stellate cells. Med Sci Monit. 2011;17(9):BR248–56. doi: 10.12659/MSM.881928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Benter IF, Yousif MH, Cojocel C, et al. Angiotensin-(1–7) prevents diabetes-induced cardiovascular dysfunction. Am J Physiol Heart Circ Physiol. 2007;292(1):666–72. doi: 10.1152/ajpheart.00372.2006. [DOI] [PubMed] [Google Scholar]
- 28.Kucharewicz I, Pawlak R, Matys T, et al. Antithrombotic effect of captopril and losartan is mediated by angiotensin-(1–7) Hypertension. 2002;40(5):774–79. doi: 10.1161/01.hyp.0000035396.27909.40. [DOI] [PubMed] [Google Scholar]
- 29.Santos RA, Simoes e Silva AC, Maric C, et al. Angiotensin-(1–7) is an endogenous ligand for the G protein-coupled receptor Mas. Proc Natl Acad Sci USA. 2003;100(14):8258–63. doi: 10.1073/pnas.1432869100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Clark MA, Diz DI, Tallant EA. Angiotensin-(1–7) downregulates the angiotensin II type 1 receptor in vascular smooth muscle cells. Hypertension. 2001;37(4):1141–46. doi: 10.1161/01.hyp.37.4.1141. [DOI] [PubMed] [Google Scholar]
- 31.Wiemer G, Dobrucki LW, Louka FR, et al. AVE 0991, a nonpeptide mimic of the effects of angiotensin-(1–7) on the endothelium. Hypertension. 2002;40(6):847–52. doi: 10.1161/01.hyp.0000037979.53963.8f. [DOI] [PubMed] [Google Scholar]
- 32.Pinheiro SV, Simoes E, Silva AC, Sampaio WO, et al. Nonpeptide AVE 0991 is an angiotensin-(1–7) receptor Mas agonist in the mouse kidney. Hypertension. 2004;44(4):490–96. doi: 10.1161/01.HYP.0000141438.64887.42. [DOI] [PubMed] [Google Scholar]
- 33.Lemos VS, Silva DM, Walther T, et al. The endothelium dependent vasodilator effect of the nonpeptide Ang(1–7) mimic AVE 0991 is abolished in the aorta of mas-knockout mice. J Cardiovasc Pharmacol. 2005;46(3):274–79. doi: 10.1097/01.fjc.0000175237.41573.63. [DOI] [PubMed] [Google Scholar]
- 34.Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med. 2005;352(16):1685–95. doi: 10.1056/NEJMra043430. [DOI] [PubMed] [Google Scholar]
- 35.Weiss R. Nebivolol: a novel beta-blocker with nitric oxide induced vasodilatation. Vasc Health Risk Manag. 2006;2(3):303–8. doi: 10.2147/vhrm.2006.2.3.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Broeders MA, Doevendans PA, Bekkers BC, et al. Nebivolol: a third-generation beta-blocker that augments vascular nitric oxide release: endothelial beta(2)-adrenergic receptor-mediated nitric oxide production. Circulation. 2000;102(6):677–84. doi: 10.1161/01.cir.102.6.677. [DOI] [PubMed] [Google Scholar]
- 37.Dessy C, Saliez J, Ghisdal P, et al. Endothelial beta3-adrenoreceptors mediate nitric oxide-dependent vasorelaxation of coronary microvessels in response to the third-generation beta-blocker nebivolol. Circulation. 2005;112(8):1198–205. doi: 10.1161/CIRCULATIONAHA.104.532960. [DOI] [PubMed] [Google Scholar]
- 38.Mollnau H, Schulz E, Daiber A, et al. Nebivolol prevents vascular NOS III uncoupling in experimental hyperlipidemia and inhibits NADPH oxidase activity in inflammatory cells. Arterioscler Thromb Vasc Biol. 2003;23(4):615–21. doi: 10.1161/01.ATV.0000065234.70518.26. [DOI] [PubMed] [Google Scholar]
- 39.Wolf SC, Sauter G, Preyer M, et al. Influence of nebivolol and metoprolol on inflammatory mediators in human coronary endothelial or smooth muscle cells. Effects on neointima formation after baloon denudation in carotid arteries of rats treated with nebivolol. Cell Physiol Biochem. 2007;19(1–4):129–36. doi: 10.1159/000099201. [DOI] [PubMed] [Google Scholar]
- 40.Baumhakel M, Schlimmer N, Buyukafsar K, et al. Nebivolol, but not metoprolol, improves endothelial function of the corpus cavernosum in apolipoprotein e-knockout mice. J Pharmacol Exp Ther. 2008;325(3):818–23. doi: 10.1124/jpet.107.135681. [DOI] [PubMed] [Google Scholar]
- 41.Flather MD, Shibata MC, Coats AJ, et al. Randomized trial to determine the effect of nebivolol on mortality and cardiovascular hospital admission in elderly patients with heart failure (SENIORS) Eur Heart J. 2005;26(3):215–25. doi: 10.1093/eurheartj/ehi115. [DOI] [PubMed] [Google Scholar]
- 42.Tzemos N, Lim PO, MacDonald TM. Nebivolol reverses endothelial dysfunction in essential hypertension: a randomized, double-blind, crossover study. Circulation. 2001;104(5):511–14. doi: 10.1161/hc3001.094207. [DOI] [PubMed] [Google Scholar]
- 43.Wei-Kang G, Dong-Liang Z, Xin-Xin W, et al. Actin cytoskeleton modulates ADMA-induced NF-kappaB nuclear translocation and ICAM-1 expression in endothelial cells. Med Sci Monit. 2011;17(9):BR242–47. doi: 10.12659/MSM.881927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Weakley S, Jiang J, Lu J, et al. Natural antioxidant dihydroxybenzyl alcohol blocks ritonavir-induced endothelial dysfunction in porcine pulmonary arteries and human endothelial cells. Med Sci Monit. 2011;17(9):BR235–41. doi: 10.12659/MSM.881926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Johnson JL, Fritsche-Danielson R, Behrendt M, et al. Effect of broad-spectrum matrix metalloproteinase inhibition on atherosclerotic plaque stability. Cardiovasc Res. 2006;71(3):586–95. doi: 10.1016/j.cardiores.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 46.Galis ZS, Sukhova GK, Lark MW, Libby P. Increased expression of matrix metalloproteinases and matrix degrading activity in vulnerable regions of human atherosclerotic plaques. J Clin Invest. 1994;94(6):2493–503. doi: 10.1172/JCI117619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Piotrowski W, Gorski P, Pietras T, et al. The selected genetic polymorphisms of metalloproteinases MMP2, 7, 9 and MMP inhibitor TIMP2 in sarcoidosis. Med Sci Monit. 2011;17(10):CR598–607. doi: 10.12659/MSM.881987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Higashikata T, Yamagishi M, Higashi T, et al. Altered expression balance of matrix metalloproteinases and their inhibitors in human carotid plaque disruption: results of quantitative tissue analysis using real-time RT-PCR method. Atherosclerosis. 2006;185(1):165–72. doi: 10.1016/j.atherosclerosis.2005.05.039. [DOI] [PubMed] [Google Scholar]
- 49.Michalska M, Gluba A, Mikhailidis D, et al. The role of polyphenols in cardiovascular disease. Med Sci Monit. 2010;16(5):RA110–19. [PubMed] [Google Scholar]
- 50.Kuzuya M, Nakamura K, Sasaki T, et al. Effect of MMP-2 deficiency on atherosclerotic lesion formation in apoE-deficient mice. Arterioscler Thromb Vasc Biol. 2006;26(5):1120–25. doi: 10.1161/01.ATV.0000218496.60097.e0. [DOI] [PubMed] [Google Scholar]
- 51.Hanemaaijer R, Visser H, Koolwijk P, et al. Inhibition of MMP synthesis by doxycycline and chemically modified tetracyclines (CMTs) in human endothelial cells. Adv Dent Res. 1998;12(2):114–18. doi: 10.1177/08959374980120010301. [DOI] [PubMed] [Google Scholar]
- 52.Gapski R, Hasturk H, Van Dyke TE, et al. Systemic MMP inhibition for periodontal wound repair: results of a multicentre randomized-controlled clinical trial. J Clin Periodontol. 2009;36(2):149–56. doi: 10.1111/j.1600-051X.2008.01351.x. [DOI] [PubMed] [Google Scholar]
- 53.Madan M, Bishayi B, Hoge M, Messas E, Amar S. Doxycycline affects diet- and bacteria-associated atherosclerosis in an ApoE heterozygote murine model: cytokine profiling implications. Atherosclerosis. 2007;190(1):62–72. doi: 10.1016/j.atherosclerosis.2006.02.026. [DOI] [PubMed] [Google Scholar]