Summary
Background
Devic’s disease, also known as neuromyelinitis optica (NMO), is a severe, rare demyelinating disorder, previously considered to be a form of multiple sclerosis (MS). The aim of this study was to present the case report of 21-year-old woman with a very early diagnosis of Devic’s disease, established following electrophysiological testing.
Case Report
A 21-year-old woman was referred to Warsaw Medical University, Department of Ophthalmology, with subjective visual impairment. The patient underwent a full clinical examination, colour vision and Goldmann visual field testing, fluorescein angiography, OCT, multifocal ERG, and visual evoked potentials (VEPs).
Conclusions
Visual evoked potentials are a very useful diagnostic tool in optic nerve neuropathies. In our patient, the electrophysiological testing allowed us to establish a proper diagnosis very early, before typical clinical signs of Devic’s disease.
Keywords: visual evoked potentials, demyelination, Devic’s disease, neuromyelitis optica
Background
Devic’s disease, or neuromyelitis optica (NMO), is an uncommon demyelinating syndrome of the central nervous system, characterized by bilateral optic neuritis and transverse acute myelitis, with no other neurological involvement. The first description of the disease was provided by Eugene Devic at the end of the 19th century in Lyon, France. NMO was previously considered to be a subtype of multiple sclerosis [1,2]. Devic’s disease is now considered as an auto-immune channelopathy [3]. Most NMO patients produce auto-antibodies against aquaporin-4 (AQP-4), also known as NMO-IgG. AQP-4 is a water channel expressed on astrocytes and in brain blood vessels [4–6]. In 2006, Wingerchuk proposed revised diagnostic criteria for NMO: 2 major criteria – optic neuritis and transverse myelitis, and at least 2 of 3 supportive criteria – MRI lesions extending over 3 vertebral segments, onset brain MRI not meeting diagnostic criteria for multiple sclerosis, and NMO-IgG seropositive status [7].
Devic’s disease most frequently affects non-Caucasian women who are older than those with multiple sclerosis. In comparison to MS, Devic’s disease also leads to more severe neurological impairment [1,8–10].
Case Report
A 21-year-old woman presented with non-specific ocular phenomena, referred as a subjective visual impairment and “blurry” vision for 3 weeks. No other complaints were reported, and the family history concerning general and ocular diseases was negative. The patient had previously been examined in 2 other ophthalmic departments and no abnormalities were found, so the patient was classified as having psychosomatic disturbances and a psychological consultation was recommended.
The patient’s best corrected visual acuity was 6/6 in both eyes on Snellen charts.
Colour vision testing using the Ishihara tables was normal.
Examinations of pupillary reflexes, anterior segment, the eye fundus and the visual field (full field 120, Humphrey) were normal. A fluorescein angiography and macular OCT (Cirrus, Zeiss) were also non-contributory.
These symptoms were still unclear, so the patient underwent electrophysiological testing by using the RetiScan RetiPort system (Roland Consult).
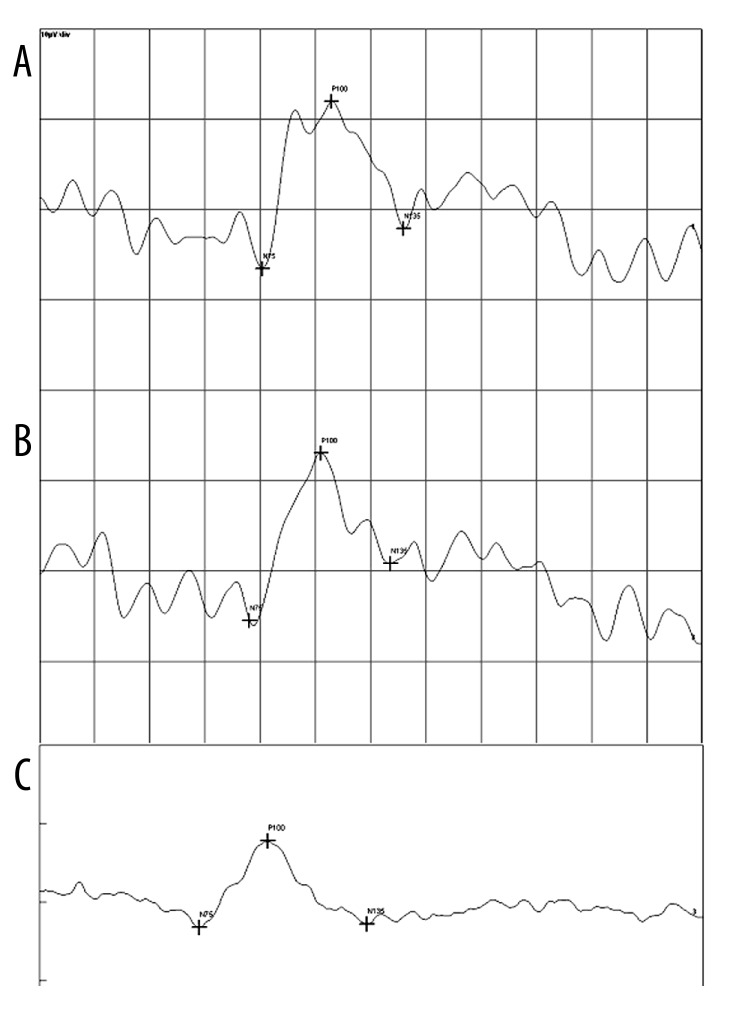
A multifocal ERG was performed to assess retinal function. The mfERG results were normal. Pattern visual evoked responses (PVER) were performed according to ISCEV standards and compared with normal values. The latencies of P100 wave was 132 ms and 127 ms in right and left eye, respectively, so they were prolonged over 20% in both eyes in comparison to normal values. The morphology of the waves was also abnormal (Figure 1). On the basis of PVER, the suspicion of a demyelinating process was established.
Figure 1.
Pattern visual evoked potentials of the right (A) and left (B) eye in comparison to normal responses (C).
The brain MRI with contrast revealed 3 lesions not meeting diagnostic criteria for multiple sclerosis. The orbital MRI with contrast revealed no lesions. A spinal cord MRI showed 1 lesion on the C3/C4 level.
The patient was referred to the neurology ward and a suspicion of Devic’s disease was established. Within 6 weeks after first symptoms (three weeks after ophthalmic examination) the patient presented a weakening of the lower limbs and developed clinical transverse myelitis. The patient was treated by IV steroids. The spinal cord MRI revealed lesions extending over 3 vertebral segments. The diagnosis of Devic’s syndrome was established, which was later confirmed by NMO-IgG seropositive status.
In 4 years’ observation, the visual function remains quite good (6/9 in both eyes), but urinary incontinence and walking disorders significantly worsen the 25-year-old patient’s quality of life.
Discussion
Devic’s disease is considered to be an acute and devastating disease. It was reported that 55.8% of NMO patients need support to walk within 5 years from diagnosis, mortality rate ranges from 2.9% to 25%, and about 50% of patients have severe visual deficits within 5 years from diagnosis [1,8–11]. Although it is very rare disease, its early diagnosis may allow administering proper treatment (IV steroids, plasmapheresis, Imuran, rituximab), thus preventing mortality.
Most papers describe full clinical manifestation of Devic’s disease. Our paper presents a case report of very early NMO diagnosis. In our patient, non-specific ocular phenomena preceded the neurological manifestations. Although the ophthalmologic examination and tests were normal, visual evoked potentials pointed to a demyelinating process. Further diagnostic procedures (brain and spinal cord MRI, neurological consultation) allowed establishing a proper diagnosis.
Conclusions
We would like to emphasize that non-specific ocular symptoms or subjective visual impairment in young patients in their 20s or 30s, with full visual acuity, normal ophthalmic and accessory investigation results, should be examined by visual evoked potentials testing to exclude demyelination. In these cases, it is essential to exclude a neuromyelitis optica, a disease with a worse prognosis than multiple sclerosis.
Footnotes
Statement
The authors had no financial or proprietary interest in any product, material or method mentioned.
Source of support: Departmental sources
References
- 1.Wingerchuk DM, Hogancamp WF, O’Brien PC, Weinshenker BG. The clinical course of neuromyelitis optica (Devic’s syndrome) Neurology. 1999;53:1107–14. doi: 10.1212/wnl.53.5.1107. [DOI] [PubMed] [Google Scholar]
- 2.Rivera JF, Kurtzke JF, Booth VJA, Corona T. Characteristics of Devic’s disease (neuromyelitis optica) in Mexico. J Neurol. 2008;255:710–15. doi: 10.1007/s00415-008-0781-2. [DOI] [PubMed] [Google Scholar]
- 3.Fazio R, Radaelli M, Furla R. Neuromyelitis optica: Concepts in evolution. J Neuroimmunol. 2011;231:100–4. doi: 10.1016/j.jneuroim.2010.10.012. [DOI] [PubMed] [Google Scholar]
- 4.Lennon VA, Kryzer TJ, Pittock SJ, et al. IgG marker of optic-spinal multiple sclerosis binds to the aquaporin-4 water channel. J Exp Med. 2005;202:473–77. doi: 10.1084/jem.20050304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lennon VA, Wingerchuk DM, Kryzer TJ, et al. A serum autoantibody marker of neuromyelitis optica: distinction from multiple sclerosis. Lancet. 2004;364:2106–12. doi: 10.1016/S0140-6736(04)17551-X. [DOI] [PubMed] [Google Scholar]
- 6.Waters P, Vincent A. Detection of anti-aquaporin-4 antibodies in neuromyelitis optica: current status of the assays. The International MS Journal. 2008;15:99–105. [PubMed] [Google Scholar]
- 7.Wingerchuk DM, Lennon VA, Pittock SS, et al. Revised diagnostic criteria for neuromyelitis optica. Neurology. 2006;66:1485–89. doi: 10.1212/01.wnl.0000216139.44259.74. [DOI] [PubMed] [Google Scholar]
- 8.Bergamaschi R, Ghezzi A. Devic’s neuromyelitis optica: clinical features and prognostic factors. Neurological Sciences. 2004;25:364–67. doi: 10.1007/s10072-004-0342-0. [DOI] [PubMed] [Google Scholar]
- 9.Ghezzi A, Bergamaschi R, Martinelli V, et al. Clinical characteristics, course and prognosis of relapsing Devic’s neuromyelitis optica. J Neurol. 2004;251:47–52. doi: 10.1007/s00415-004-0271-0. [DOI] [PubMed] [Google Scholar]
- 10.Sellner J, Boggild M, Clanet M, et al. EFNS guidelines on diagnosis and management of neuromyelitis optica. Eur J Neurol. 2010;17:1019–32. doi: 10.1111/j.1468-1331.2010.03066.x. [DOI] [PubMed] [Google Scholar]
- 11.Mandler RN, Davis LE, Jeffrey DR, Kornfeld M. Devic’s neuromyelitis optica: a clinopathological study of 8 patients. Ann Neurol. 1993;34:162–68. doi: 10.1002/ana.410340211. [DOI] [PubMed] [Google Scholar]