Summary
Background
Many anesthetics reduce lower esophageal sphincter pressure (LESP) and consequently the gastro-esophageal pressure gradient (GEPG); thus they may promote gastro-esophageal reflux and contribute to aspiration pneumonia. Our goals were to evaluate the association between LESP and 2 measures of sedation: bispectral index (BIS) and the responsiveness component of the Observer’s Assessment of Alertness score (OAA/S).
Material/Methods
Eleven healthy volunteers were each sedated on 2 separate days. Subjects were given sedative infusions of increasing target plasma concentrations of dexmedetomidine or propofol. LESP and GEPG were recorded after starting each infusion phase. Generalized estimating equation modeling was used to assess the relationship between LESP and, respectively, BIS and OAA/S. The existence of a drug-dependent association was evaluated within these models by testing an interaction term. Wald tests were used to evaluate the relationships within the models.
Results
We found a significant relationship between LESP and BIS (P=0.0043) after adjusting for the main effect of sedative type – a deepening of sedation as measured by a decrease in BIS of 10% was associated with a decrease [Bonferroni-adjusted 95% CI] in LESP of −1.34 [−2.39, −0.29] mmHg. After adjusting for the main effect of sedative drug, LESP significantly declined with declining OAA/S (P=0.001); a unit decrease of OAA/S was associated with a decrease [Bonferroni-adjusted 95% CI] in LESP of −2.01 [−3.20, −0.81] mmHg.
Conclusions
Deeper sedation, as measured by either BIS or OAA/S, significantly reduces LESP.
Keywords: BIS, lower esophageal sphincter, dexmedetomidine, propofol
Background
The lower esophageal sphincter is a circular smooth muscle barrier between the stomach and the esophagus. The main function of this sphincter is to prevent gastric contents from regurgitating into the esophagus and pharynx [1]. Reduced pressure and consequent reduction in the gastro-esophageal pressure gradient (GEPG) may promote gastro-esophageal reflux, which increases the chances of aspiration, and thus contribute to aspiration pneumonia, pneumonitis, and associated morbidity. Many sedatives and anesthetics reduce lower esophageal sphincter pressure (LESP), but LESP per se is difficult to measure [2–4]. The relationship between sedation level and lower esophageal sphincter functionality is of considerable clinical interest.
The most widely used and best validated monitor of hypnotic state during sedation and anaesthesia is the bispectral index (BIS), a measure derived from processed electroencephalographic signals. An alternative in sedated subjects is the Observer’s Assessment of Alertness and Sedation (OAA/S) score, a well-established and commonly used tool for evaluating sedative drugs [5].
Previous studies have shown a good correlation between anesthetic dose and reduced LESP [2–4], suggesting that there may also be an association between sedation level and LESP. We thus evaluated the association between lower esophageal sphincter pressure and 2 measures of sedation: BIS and the responsiveness component of the Observer’s Assessment of Alertness score.
Material and Methods
We report a new analysis of results obtained during a previously published study in which we evaluated the effects of 2 different drugs and different doses on lower esophageal sphincter pressures [6].
Protocol
After obtaining approval from the University of Louisville Institutional Review Board, and informed consent of volunteers, we studied 11 healthy volunteers aged 18 to 40 years. Exclusion criteria were obesity with body mass index more than 30 kg/m2, pregnancy, drug or alcohol abuse, heartburn reported to occur more than once per week, history of gastro-esophageal reflux disease, or a history of any esophagus or stomach surgery. Volunteers were instructed not to take any medications likely to alter gastroesophageal sphincter pressure.
Volunteers were randomly allocated to propofol or dexmedetomidine sedation on 2 separate study days according to a computer-generated randomization. Propofol and dexmedetomidine were given via target-controlled infusion using a Harvard infusion pump (Harvard Clinical Technology, Inc., South Natick, MA) driven by STANPUMP software (available at http://www.opentci.org) using the Schnider model [7].
Propofol was given in increasing steps to target effect-site concentration of 1, 2, and 4 μg/mL; dexmedetomidine was given to target plasma concentration of 0.6, 1.2, and 2.4 ng/mL. Volunteers were monitored through the study period for electrocardiogram, non-invasive blood pressure, heart rate, pulse oximeter saturation (SpO2) and end-tidal PCO2. BIS (Bispectral Index, BIS XP 3.4 monitor, Aspect Medical Systems, Newton, MA, USA) was recorded continuously and sedation level was evaluated every 5 minutes with the OAA/S score [5].
Measurements
An esophageal manometry probe was passed transnasally, and lower-esophageal sphincter (LES) was identified using the station pull-through technique at 1-cm intervals as described by Mittal et al. [8] The pressure tracings were recorded continuously using a multi-channel recording system. Baseline gastric, LES, and distal esophageal peristaltic pressures were recorded. Pressures were again recorded after 20 and 40 minutes of sedative infusion at each concentration. Esophageal and gastric pressures were evaluated by an investigator blinded to drug and dose allocations.
Statistical analysis
First, exploratory graphical analyses were performed to informally assess bivariate relationships between LESP and BIS and between LESP and OAA/S. These graphical analyses are useful for visually evaluating overall trends, but do not yield a formal measure of association and do not account for potential intra-subject correlation exhibited by repeated measurements within a volunteer. Thus, in order to formally estimate the degree of the relationship between LESP and a given predictor of interest (for instance, BIS), a generalized estimating equation (GEE) model was developed. This model appropriately accounts for the intra-subject correlation while estimating the slope (our model incorporated an exchangeable correlation structure).
In the GEE model, we considered the potential for the relationship between BIS and LESP to depend on the type of sedative drug administered by testing the interaction between type of sedative and BIS (generalized score test [9]); if this interaction term was statistically significant at the 0.10 level, separate slopes were estimated for each drug; otherwise, a common slope was estimated after adjusting for type of sedative. The same GEE modeling approach was used to characterize the relationship between OAA/S and LESP.
For each predictor of interest, a (Wald) chi-squared test for GEE model terms was used to test the significance of the relationship with LESP. Since there were 2 predictors of interest (BIS and OAA/S), we used an outcome-specific significance level of 0.025, which reflects the Bonferroni correction for 2 comparisons. If a significant interaction term was found, we similarly employed the Bonferroni correction to test the drug-specific slope measuring the dependence of LESP on the relevant predictor at the 0.0125 significance level.
In addition to estimating the relationships between the respective exposures and LESP, we considered the ability of each exposure to explain observed variance among LESP measurements – that is, over and above that explained by type of sedative drug administered alone. The likelihood ratio R2 statistic for GEE models [10] is a quantity ranging from 0 to 1, where a value of 0 represents independence between drug-adjusted LESP and the relevant predictor (for instance, BIS) and a value of 1 represents perfect explanatory capability of the predictor. This likelihood ratio R2 statistic is thus analogous to a partial R2 from a standard linear regression model; the only difference is that it adjusts for the intra-subject correlation exhibited by repeated measures on a volunteer.
R software version 2.12.1 (The R Foundation for Statistical Computing, Vienna, Austria) and SAS software version 9.2 (SAS Institute, Cary, NC, USA) were used for the statistical analysis.
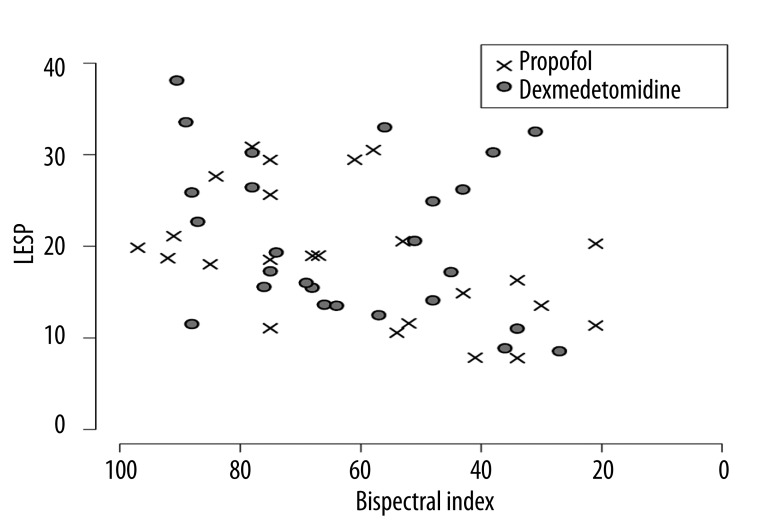
The GEE modeling will appropriately account for the intra-subject correlation. Of course it is always ideal in any study if the relationship of interest can be visualized graphically – we considered using different symbols for each of the volunteers but this would make the scatterplot more confusing. Connecting them with lines would be more confusing, since patients may not have smoothly transitioned down the BIS and OAA/S scales with decreasing LESP (for example, there might be a line going from (LESP=30, BIS=80) to (20,60) to (10,80)). It is hoped that readers will recognize the summary nature of the figures and regard to the GEE analysis as the formal evaluation of the hypotheses.
Results
Eleven volunteers participated; they were aged 24±4 years, had a body weight of 70±12 kg, and were 175±5 cm tall. Fifty observations on these volunteers were available for analysis.
Without considering the intra-subject correlation, an overall slightly-declining relationship between LESP and deepening sedation as measured by BIS was noted, and this relationship appeared not to differ between propofol and dexmedetomidine (Figure 1).
Figure 1.
Lower esophageal sphincter pressure (LESP) and bispectral index (BIS) measurements among 11 volunteers given propofol and dexmedetomidine sedation on two separate trial days.
Indeed, the interaction term in the GEE model that adjusted for the intra-subject correlation was not statistically significant (P=0.14, generalized score test). But after adjusting for the main effect of type of sedative drug administered, we found a significant relationship between LESP and BIS (P=0.0043, chi-squared test): a deepening of sedation as measured by a decrease in BIS of 10% was associated with a decrease [Bonferroni-adjusted 95% confidence interval] in LESP of −1.34 [−2.39, −0.29] mmHg. BIS explained an additional 10.4% of variability in LESP over and above that explained by type of sedative drug administered, as given by the likelihood ratio R2.
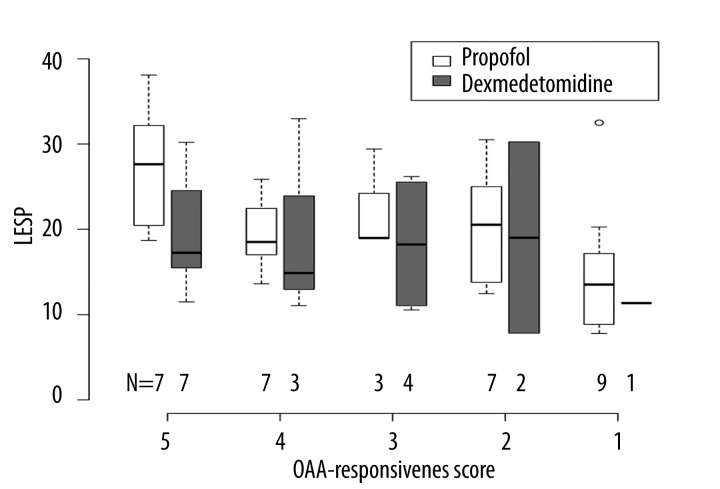
Box plots characterizing the distribution of LESP for each drug-OAA/S combination are given in Figure 2. Due to the fact that sedation is generally deeper with propofol than with dexmedetomidine, we only had 3 measurements where the OAA/S score was less than 3. Based on a visual inspection of the box plots, a moderately declining relationship was observed among measurements obtained under propofol sedation, while a flat-to-increasing relationship was observed among the dexmedetomidine measurements.
Figure 2.
Box plots of lower esophageal sphincter pressure (LESP), by type of sedative drug administered and by the responsiveness component of the Observer’s Assessment of Alertness (OAA) score.
In the GEE analysis for OAA/R, however, there was no such evidence of differing slopes for the 2 sedative drugs (generalized score test P=0.22 for the interaction). After adjusting for the type of sedative drug administered, LESP significantly declined with declining OAA/R (P=0.001, chi-squared test): a unit decrease of OAA/S was associated with a decrease [Bonferroni-adjusted 95% confidence interval] in LESP of −2.01 [−3.20, −0.81] mmHg. OAA/S scores explained 20.9% of the observed variability in LESP, over and above that explained by type of sedative drug administered.
Discussion
Most anesthetic and sedation techniques reduce LES tone, thus presumably increasing the chance of patients regurgitating gastric content into the esophagus – and consequent risk of aspiration. Regurgitation risk is especially important when sedation is given to patients with unsecured airways. Aspiration is relatively rare, but the associated morbidity and mortality is devastating, and includes detrimental aspiration pneumonitis and pneumonia [11]. Microaspirations from the stomach and oropharynx are believed to play a major role in etiology of nosocomial and ventilator-associated pneumonia [12]. Preventing aspiration thus likely reduces the risk of ventilator-associated pneumonia – which justifies careful consideration of preventive strategies and bundled-care approach. One strategy is control of sedation and hypnotic levels.
Propofol and dexmedetomidine are frequently used sedative agents in the perioperative setting and also in the ICU. In our previous study [6], both agents caused dose-dependent reductions in lower esophageal sphincter pressures. There is no simple way to determine or estimate LESP; measurement of the sphincter pressure is a complicated process requiring expertise and special equipment. The bispectral index (BIS) is an empirically calibrated value derived from processed adult EEG data, which correlates with depth of the hypnotic component of general anesthesia in adults. BIS is frequently used in the perioperative setting and also has been validated in some groups of ICU patients to determine the depth of sedation [13–15]. Our results demonstrate that BIS measurements correlate significantly with LESP.
That there is a correlation between BIS and LESP is unsurprising, considering that previous studies have also demonstrated a dose-dependent action of different anesthetics on LESP. For example Thörn et al. showed that inhalation induction with sevoflurane titrated to a BIS of 40 resulted in significant decreases in LESP and barrier pressure, although the barrier pressure was kept positive in all patients [16]. There is also a slight relationship between the frequency of spontaneous esophageal contractions and end-tidal halothane concentration [17], suggesting that anesthetic depth and esophageal muscle tone are related.
Although we found a statistically significant relation between the BIS and LESP measurements, the strength of the correlation was marginal. Furthermore, the strength of correlation may vary in different patient populations under different sedation regimens. For example, it may be much greater in critical care patients compared to the healthy volunteers studied in this trial. Similarly, the relationship between BIS and LESP may be altered by concomitant medications. It is thus reasonable to conclude that deeper hypnotic planes (lower BIS) are very likely to be associated with further reduced LESP.
While there was a weak relationship between OAA/S sedation scores and LESP for propofol, there was no relationship with dexmedetomidine sedation. The difference may be a consequence of distinct clinical profiles of the 2 drugs. Both provide good clinical sedation; but unlike patients given propofol, those given dexmedetomidine remain arousable. A corollary is that OAA/S may not be the appropriate clinical scale for use in evaluating dexmedetomidine sedation. But even with propofol, the strength of the correlation between OAA/S and LESP was too weak to reliably predict LESP as a function of BIS, or to reliably use OAA/S to titrate to safe esophageal sphincter pressures. Another explanation would simply be the major difference between BIS and OAA/S as the sedation assessment tools. One of them is a passive measure, which records EEG waveforms from a probe placed on forehead (BIS). The other is an active assessment tool, which requires an observer to physically stimulate the subject to monitor the response (OAA/S). In spite of many obvious and subtle differences in these sedation assessment systems, we concluded that OAA/S – like BIS – is related to LESP (at least with propofol), but that the strength of the correlation only permits the general conclusion that deeper sedative and hypnotic planes reduce LESP, and presumably augment aspiration risk.
Conclusions
We found that there is significant correlation between BIS, OAA/S scale and LESP. Deepening of sedation significantly reduces LESP. Sedation should be carefully titrated and maintained at the lightest effective level in patients at risk of aspiration.
Footnotes
Statement
None of the authors has a personal financial interest in this research.
Source of support: Institutional and departmental sources
References
- 1.Hornby PJ, Abrahams TP. Central control of lower esophageal sphincter relaxation. Am J Med. 2000;108(Suppl 4a):90–98S. doi: 10.1016/s0002-9343(99)00345-9. [DOI] [PubMed] [Google Scholar]
- 2.Cox MR, Martin CJ, Dent J, Westmore M. Effect of general anaesthesia on transient lower oesophageal sphincter relaxations in the dog. Aust NZJ Surg. 1988;58:825–30. doi: 10.1111/j.1445-2197.1988.tb00987.x. [DOI] [PubMed] [Google Scholar]
- 3.Thorn K, Thorn SE, Wattwil M. The effects on the lower esophageal sphincter of sevoflurane induction and increased intra-abdominal pressure during laparoscopy. Acta Anaesthesiol Scand. 2006;50:978–81. doi: 10.1111/j.1399-6576.2006.01069.x. [DOI] [PubMed] [Google Scholar]
- 4.van der Hoeven CW, Attia A, Deen L, Klopper PJ. The influence of anaesthetic drugs on the lower oesophageal sphincter in propofol/nitrous oxide anaesthetized dogs. Pressure profilometry in an animal model. Acta Anaesthesiol Scand. 1995;39:822–26. doi: 10.1111/j.1399-6576.1995.tb04178.x. [DOI] [PubMed] [Google Scholar]
- 5.Chernik DA, et al. Validity and reliability of the Observer’s Assessment of Alertness/Sedation Scale: study with intravenous midazolam. J Clin Psychopharmacol. 1990;10:244–51. [PubMed] [Google Scholar]
- 6.Turan A, et al. Effects of dexmedetomidine and propofol on lower esophageal sphincter and gastroesophageal pressure gradient in healthy volunteers. Anesthesiology. 2010;112:19–24. doi: 10.1097/01.anes.0000365963.97138.54. [DOI] [PubMed] [Google Scholar]
- 7.Schnider TW, et al. The influence of method of administration and covariates on the pharmacokinetics of propofol in adult volunteers. Anesthesiology. 1998;88:1170–82. doi: 10.1097/00000542-199805000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Mittal RK, McCallum RW. Characteristics and frequency of transient relaxations of the lower esophageal sphincter in patients with reflux esophagitis. Gastroenterology. 1988;95:593–99. doi: 10.1016/s0016-5085(88)80003-9. [DOI] [PubMed] [Google Scholar]
- 9.Boos DD. On Generalized Score Tests. The American Statistician. 1992;46 [Google Scholar]
- 10.Magee L. R2 Measures Based on Wald and Likelihood Ratio Joint Significance Tests. The American Statistician. 1990;44:250–53. [Google Scholar]
- 11.Raghavendran K, Nemzek J, Napolitano LM, Knight PR. Aspiration-induced lung injury. Crit Care Med. 2011;39:818–26. doi: 10.1097/CCM.0b013e31820a856b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Metheny NA, et al. Tracheobronchial aspiration of gastric contents in critically ill tube-fed patients: frequency, outcomes, and risk factors. Crit Care Med. 2006;34:1007–15. doi: 10.1097/01.CCM.0000206106.65220.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Iselin-Chaves IA, et al. The effect of the interaction of propofol and alfentanil on recall, loss of consciousness, and the Bispectral Index. Anesth Analg. 1998;87:949–55. doi: 10.1097/00000539-199810000-00038. [DOI] [PubMed] [Google Scholar]
- 14.Liu J, Singh H, White PF. Electroencephalographic bispectral index correlates with intraoperative recall and depth of propofol-induced sedation. Anesth Analg. 1997;84:185–89. doi: 10.1097/00000539-199701000-00033. [DOI] [PubMed] [Google Scholar]
- 15.Triltsch AE, et al. Bispectral index-guided sedation with dexmedetomidine in intensive care: a prospective, randomized, double blind, placebo-controlled phase II study. Crit Care Med. 2002;30:1007–14. doi: 10.1097/00003246-200205000-00009. [DOI] [PubMed] [Google Scholar]
- 16.Thorn K, Thorn SE, Wattwil M. The effects on the lower esophageal sphincter of sevoflurane induction and increased intra-abdominal pressure during laparoscopy. Acta Anaesthesiologica Scandinavica. 2006;50:978–81. doi: 10.1111/j.1399-6576.2006.01069.x. [DOI] [PubMed] [Google Scholar]
- 17.Sessler DI, Stoen R, Olofsson CI, Chow F. Lower esophageal contractility predicts movement during skin incision in patients anesthetized with halothane, but not with nitrous oxide and alfentanil. Anesthesiology. 1989;70:42–46. doi: 10.1097/00000542-198901000-00010. [DOI] [PubMed] [Google Scholar]