Summary
Background
There is a growing interest in examining death rates associated with different pregnancy outcomes for time periods beyond one year. Previous population studies, however, have failed to control for complete reproductive histories. In this study we seek to eliminate the potential confounding effect of unknown prior pregnancy history by examining mortality rates associated specifically with first pregnancy outcome alone. We also examine differences in mortality rates associated with early abortion and late abortions (after 12 weeks).
Material/Method
Medical records for the entire population of women born in Denmark between 1962 and 1991 and were alive in 1980, were linked to death certificates. Mortality rates associated with first pregnancy outcomes (delivery, miscarriage, abortion, and late abortion) were calculated. Odds ratios examining death rates based on reproductive outcomes, adjusted for age at first pregnancy and year of women’s births, were also calculated.
Results
A total of 463,473 women had their first pregnancy between 1980 and 2004, of whom 2,238 died. In nearly all time periods examined, mortality rates associated with miscarriage or abortion of a first pregnancy were higher than those associated with birth. Compared to women who delivered, the age and birth year adjusted cumulative risk of death for women who had a first trimester abortion was significantly higher in all periods examined, from 180 days (OR=1.84; 1.11 <95% CI <3.71) through 10 years (1.39; 1.22 <95% CI <1.61), as was the risk for women who had abortions after 12 weeks from one year (OR=4.31; 2.18 <95% CI <8.54) through 10 years (OR=2.41; 1.56 <95% CI <2.41). For women who miscarried, the risk was significantly higher for cumulative deaths through 4 years (OR=1.75; 1.34 <95% CI <2.27) and at 10 years (OR=1.48; 1.18 <95% CI <1.85).
Conclusions
Compared to women who delivered, women who had an early or late abortion had significantly higher mortality rates within 1 through 10 years. A lesser effect may also be present relative to miscarriage. Recommendations for additional research are offered.
Keywords: abortion, maternal mortality, childbirth, late-term abortion, miscarriage, mortality rates
Background
Previous record based studies in Finland have shown that death rates within 1 year of a pregnancy event are significantly higher for women who had a pregnancy loss compared to women who were not pregnant and to women who carried to full term [1–4]. The results of a U.S. study revealed that elevated rates of death following a pregnancy loss persisted for 4 years or more; but the researchers also found that the effects may be mitigated by successful delivery of subsequent pregnancies [5].
All existing studies of mortality rates associated with prior pregnancy outcomes have been limited to pregnancies within an arbitrary range of women’s reproductive lives and have lacked information on the subjects’ complete reproductive history. Therefore, one of the main purposes of this study is to eliminate the potential confounding effect of unknown prior pregnancy history by examining mortality rates associated specifically with first pregnancy outcome alone.
An additional purpose of this study is to distinguish between mortality rates associated with early induced abortions versus later abortions, a subject that has not been previously addressed in any population register based studies. While there is well established consensus that late-term abortions are associated with more physiological risks and higher rates of maternal mortality in the short term compared to early abortions [6], very little is known regarding mortality rates beyond one year.
Material and Methods
The present investigation is a register based study using existing data from Statistic Denmark: the National Hospital Register (1977–2004) for information on miscarriages, ectopic pregnancies and other losses; the Fertility database (FTDB) for births and stillbirths; the National Board of Health Abortion Registry (1973–2004) for abortions; the Cause of Death Register; and the day of death from the CPR register (1980–2004). Data from all registers was linked using unique identification numbers assigned to all residents of Denmark. The study was approved by the National Board of Health and the Data Protection Agency.
The population includes all women in Denmark born over a 30 year period, from 1962 through 1991, who were alive as of January 1, 1980 and did not die prior to age 16. The oldest women in this study population were 11 years-old in 1973 (when the abortion registry began), and 15 years-old in 1977 (when information on miscarriages treated in hospitals became available).
Pregnancy histories were constructed from the fertility register, abortion register, and hospital discharge registers. First pregnancy outcomes were segregated by live birth, miscarriage, early abortion, and late abortion. Only singleton births were included in the birth group, to eliminate the confounding effects of cases of multiple births and situations including both a live birth and pregnancy loss. Miscarriage data is only available for cases which included a record of hospital treatment. Other losses, including ectopic pregnancy, still birth, and other products of conception were excluded from this analysis due to comparatively low numbers. Induced abortions were classified as late abortions if they occurred after the first twelve weeks of gestation.
Unadjusted death rates per 100,000 cases were calculated for (1) each of the first 10 years following the date of the pregnancy outcome, and (2) for cumulative periods from 180 days, 1 to 5 years, 10 years, and for the full length of the data window. Chi-square tests for significance were conducted for each time period using women who gave birth as the control group.
To control for the effects of time associated with changing medical technology and population health over the three decades examined, adjusted odds ratios were then calculated to control for the year of each woman’s birth and the woman’s age at the time of her first pregnancy outcome. These logistic regression analyses were conducted to yield odds ratios and 95% confidence intervals (95% CI) for the cumulative mortality rates associated with each of the three pregnancy loss groups compared to the single live birth group for periods of 180 days, 1 to 5 years, up to 10 years, and over the full length of the data window.
Results
A total of 463,473 women who had at least one pregnancy between 1980 and 2004 were included in the study, 2,238 of whom had died. The average year of birth for those who died (n=2,238) was 1966.45 (SD=4.33). First pregnancies in the population occurred at an average age of 24.69 years (SD=4.63). The average age at death was 27.4 (SD=7.3), with a range of 16 to 43 years of age.
Table 1 shows unadjusted death rates per 100,000 cases occurring within each year of the first ten years following each first pregnancy outcome. Death rates associated with birth were lower than those associated with all three types of pregnancy loss in every year. Chi-squared tests were run to compare death rates for miscarriage and early abortion to death rates for birth in each year. The difference between birth and early abortion groups was significant in 6 of the 10 years; whereas the difference between birth and miscarriage was significant in 2 of the 10 years. Significance tests were not conducted for late abortion since there were fewer than 5 deaths per year for that group, rendering any tests for significance unreliable.
Table 1.
Annual Mortality Rates per 100,000 (number of deaths). During each of first ten years following first pregnancy outcome.
| First pregnancy outcome | 1st yr | 2nd yr | 3rd yr | 4th yr | 5th yr | 6th yr | 7th yr | 8th yr | 9th yr | 10th yr |
|---|---|---|---|---|---|---|---|---|---|---|
| Birth | 17.9 (57) | 20.7 (66) | 22.0 (70) | 22.0 (70) | 21.3 (68) | 22.9 (73) | 22.9 (73) | 28.2 (90) | 21.7 (69) | 19.8 (63) |
| Miscarriage | 31.2 (8) | 15.6 (4)# | 31.2 (8) | 27.3 (7) | 39.0 (10) | 54.6 (14)* | 31.2 (8) | 62.4 (16)* | 27.3 (7) | 15.6 (4)# |
| Early Abortion | 33.8 (39)† | 38.9 (45)‡ | 28.6 (33) | 32.0 (37) | 44.1 (51)‡ | 44.1 (51)‡ | 37.2 (43)* | 28.6 (33) | 38.9 (27)* | 23.4 (27) |
| Late Abortion** | 110.0 (4)# | 55.0 (2)# | 82.5 (3)# | 27.5 (1)# | 110.0 (4)# | 55.0 (2)# | 55.0 (2)# | 55.0 (2)# | 27.5 (1)# | 27.5 (1)# |
Cell counts <5; chi-square test for significance not reliable.
p<.05;
p<.01;
p<.001; using birth as the control group.
Table 2 shows the unadjusted cumulative death rates during periods of time from 180 days up to the full study period segregated by first pregnancy outcome. The table also shows the average age at first pregnancy and at death stratified for each pregnancy outcome. Compared to mortality rates of women who gave birth, the mortality rates associated with early abortion were significantly higher for every time period examined. The cumulative mortality rate associated with late abortion was significantly higher than for birth for every time period greater than one year. The cumulative mortality rate associated with miscarriage was not significantly different from the birth group except for the longest periods of time examined, for 10 years and for the full study period.
Table 2.
Cumulative deaths per 100,000 women from within specified time period from date of pregnancy outcome to end of time period.
| N (deaths) | Avg age preg (SD) | Avg age death (SD) | Time period | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 180 days | 1 yr | 2 yrs | 3 yrs | 4 yrs | 5 yrs | 10 yrs | Full study period | ||||
| Birth | 318,646 (1,240) | 25.89 (4.07) | 32.58 (5.61) | 7.8 | 17.9 | 38.6 | 60.6 | 82.5 | 103.9 | 219.4 | 389.1 |
| Miscarriage | 25,648 (147) | 24.80 (4.60) | 31.61 (5.61) | 19.5 | 31.2 | 46.8 | 78.0 | 105.3 | 144.3 | 335.3‡ | 573.1‡ |
| Early abortion | 115,543 (809) | 20.99 (3.94) | 29.81 (6.5) | 19.0* | 33.8† | 72.7‡ | 101.3‡ | 133.3‡ | 177.4‡ | 349.7‡ | 700.2‡ |
| Late abortion | 3,636 (42) | 20.46 (4.73) | 28.98 (6.73) | 55.0# | 110.0# | 165.0‡ | 247.5‡ | 275.0‡ | 385.0‡ | 605.1‡ | 1155.1‡ |
Cell counts < 5; chi-square test for significance not reliable.
p<.05;
p<.01;
p<.001; using birth as the control group.
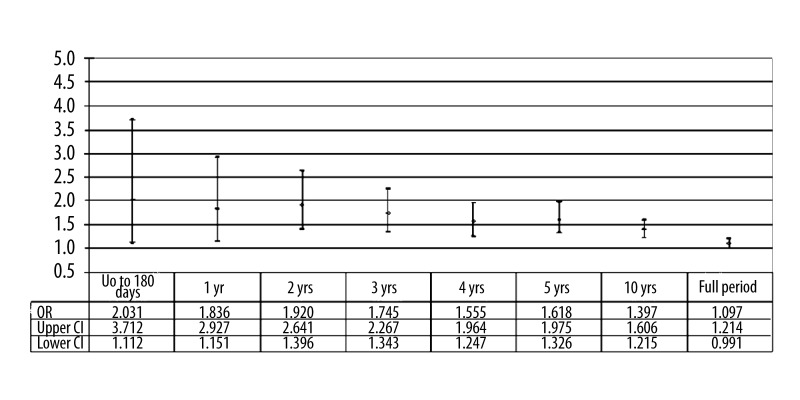
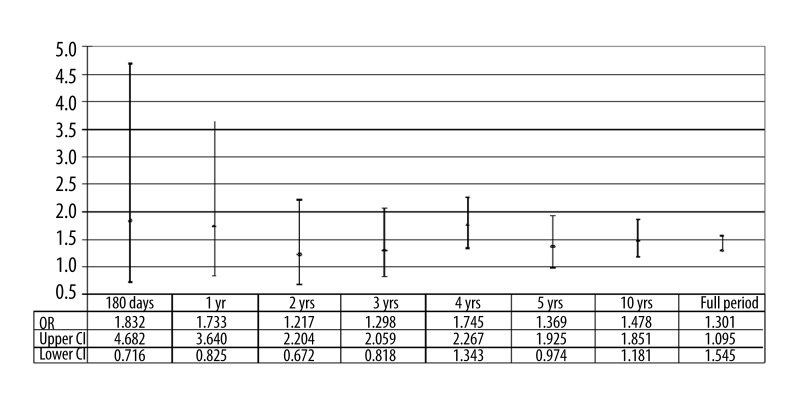
Results from the logistic regression analyses, controlling for age at first pregnancy and the year of the woman’s birth, are shown in Figures 1–3. These figures show the observed odds ratios for cumulative deaths occurring up to each identified period along with upper and lower 95% confidence intervals for each time period analyzed.
Figure 1.
Odds ratio for cumulative mortality rates associated with early abortion compared to birth – adjusted for woman’s year of birth and age at first pregnancy.
Figure 3.
Odds ratio for cumulative mortality rates associated with miscarriage compared to birth – adjusted for woman’s year of birth and age at first pregnancy.
Figure 1 shows the adjusted odds ratios associated with first pregnancies ending in early abortion compared to those ending in a live birth after adjusting for age at first pregnancy and year of the woman’s birth. The risk of death associated with an early abortion was significantly higher during nearly all time periods examined.
Figure 2 shows the adjusted odds ratios associated with late abortions compared to birth. The results should be interpreted cautiously, however, due to the low frequencies (only 4 deaths occurred in the first year, and only 22 deaths in the 10 year window). But even with low numbers, the results were statistically significant for all time periods examined (lower 95% CI >1.0).
Figure 2.
Odds ratio for cumulative mortality rates associated with abortion after 12 weeks compared to birth – adjusted for woman’s year of birth and age at first pregnancy.
Figure 3 shows the adjusted odds ratios for deaths among women who had a miscarriage treated in a hospital compared to women who successfully gave birth. The observed odds ratio was greater than 1 in all periods examined, but the results were only statistically significant (lower 95% CI >1.0) for cumulative periods beyond 4 years.
Discussion
The results of our analyses support the hypothesis that first pregnancy prenatal loss is associated with higher mortality rates compared to carrying to term, both within the first year and over a number of years to follow. The greatest differences were observed within the first 180 days of the pregnancy outcome, but the higher rates of death persisted well beyond the first year. These findings are consistent with prior studies which were blind to the history of any prior pregnancies [1,3,5] but are an important addition to the literature because they eliminate the possibility that unknown prior pregnancy outcomes may account for the observed differences.
Statistically significant results were strongest in regard to both early and late abortions (after 12 weeks) compared to birth. Although the numbers of cases for late abortions is relatively low, resulting in very wide confidence intervals, it appears likely that both the short and long term death rates associated with late abortion are greater than those associated with early abortion.
The most reliable results are found relative to early abortions and births, for which we have both a high number of cases and very complete records. The adjusted odds ratios indicate that compared to a first pregnancy ending in a live birth, an abortion prior to 12 weeks is associated with 80% higher risk of death within the first year and a 40% higher risk of death over 10 years.
Examination of death rates associated with abortion over longer periods of time is especially warranted by the need to more accurately identify abortion related deaths, which are defined by the Centers for Disease Control (CDC) in the United states as including deaths which may be due to aggravation of preexisting psychological or physiological conditions “regardless of the amount of time between the abortion and death” [6]. Previous research has revealed that without data linkage to complete pregnancy and abortion records, 73% of all pregnancy associated deaths could not be identified from death certificates alone [7]. This is why the CDC recommends identification of “pregnancy associated deaths” (without regard to cause) as a precursor to efforts to identify “pregnancy related deaths” (which are contributed to by the pregnancy) [8]. Given the difficulties inherent in determining cause of death and identifying full pregnancy history, securing measures of deaths associated with pregnancy outcome is an essential step in the process of defining future research priorities.
Extra caution should be applied to interpreting our findings regarding miscarriage. Our data on miscarriages was limited to only miscarriages treated in hospital settings. The observed effects may not represent those associated with very early and uncomplicated miscarriages. Secondly, while the observed odds ratios were consistently higher, and of a magnitude similar to that observed for early abortions, the results were not statistically significant until after five years.
Readers may notice that the adjusted odds ratio for the full study period, especially in Figure 1, are trending downward. This is likely due to the fact that over longer periods of observation the odds ratio will necessarily trend toward 1.0 precisely because everyone dies. By the end of the study period women born in 1962, for example, are beginning to die at higher rates regardless of their reproductive history, a fact that begins to erase differences that would otherwise be observed when the 1962 cohort were all 30 years of age.
Limitations
Our analysis did not consider the possible impact of subsequent pregnancy outcomes. Prior research has shown that different pregnancy outcomes for multiple pregnancies are associated with different mortality rates. For example, during an 8 year period examined among low income women in California, the mortality rate for women who had a delivery following abortion was 462 per 100,000, significantly lower than for women who had only abortions during the same time frame, 854 per 100,000 [5]. Subsequent pregnancy outcomes may therefore be an important mediating factor in mortality rates
Another limitation is that our analysis does not control for socioeconomic factors, marital status, psychological history, or other factors prior to first pregnancy which may affect the subsequent risk of death.
Still another limitation of our study is that all causes of death were analyzed together. Previous studies have shown that elevated risks of death associated with perinatal loss were most pronounced relative to external causes of death (suicide, homicide, accidents) [2,4,5]. But higher rates of deaths from natural causes [3,5], including significantly higher mortality rates from circulatory and cerebrovascular disease [5], have also been observed. Additional research is necessary to determine how first pregnancy outcome may be associated with specific causes of death.
Interpretation of results
There are at least three theories which may explain the differences in mortality rates observed. The first theory may be called the ”healthy pregnant woman effect” [3,9]. This theory suggests that healthier women are more likely to be able to concieve and carry a pregnancy to term. Conversely, women who are unhealthy may be unable to concieve or may be more likely to have a spontaneous or therapuetic abortion.
The second theory is that pregnancy, especially one carried to term, produces health benefits which reduce the risk of death. For example, carrying a pregancy to term is associated with physiological changes associated with a reduced risk of breast [10], ovarian [11], and endrometrial cancers [12]. Live births may also contribute to psychological benefits, or at least behavioral changes and lifestyle choices associated with being a parent which improve health and/or reduce unhealthy or risk-taking behaviors.
The third theory is that pregnancy loss may contribute to physiological or psychological effects which increase risk of death. For example, abortion is associated with an increased risk of suicide [4], substance abuse [13], post-traumatic stress disorder [14], and a lower assessment of general health [15]. In addition, it is notable that the elevated rates of mortality associated with pregnancy loss observed in this study are on the same order of magnitude as the elevated rates of mortality among women who experience the death of a child under 18 years of age [16]. Factors common to both experiences may explain the effect observed in both groups.
All three theories, and other factors not yet identified, may contribute to the effects revealed by our analyses. Further research is necessary to tease out both any positive health effects of childbirth and any negative health effects of pregnancy loss.
Recommendations regarding future research
As discussed in the limitations section above, a very large number of additional factors should be explored to better understand the effects observed. Subsequent pregnancies, prior physical and mental health, relationship status, and socioeconomic factors are all likely to have effects on mortality rates. Many of these factors likely have interdependencies and serial correlations which seriously complicate regression analyses. In particular, both the occurrence and outcome of subsequent pregnancies may be correlated with earlier pregnancy outcomes. For example, pregnant teenagers are 4 to 6 times more likely to abort if they have already had a prior abortion than teens without a prior history of abortion [17]. To most carefully explore interactions relative to multiple pregnancies, we recommend that future research examine results stratified by all combinations of earlier pregnancy outcomes. For example, mortality rates for each second pregnancy outcome should be stratified relative to whether the first pregnancy ended in birth, miscarriage or abortion.
A good deal of insight might also be gained by case-control studies which are carefully designed [18]. In addition to selecting control groups relative to year of the woman’s birth, age at first pregnancy, marital status, and socioeconomic status, cases should be matched to controls with similar psychiatric histories prior to the year of the first pregnancy.
An important objective of future research should be to identify which subgroups of women experiencing a pregnancy loss may benefit the most from additional health care or counseling services. For example, it is hypothetically possible that most of the observed effects occur among low income women with a history of depression. But until additional research narrows the subgroups of the population most at risk, this and previous studies [2,4,5] clearly demonstrate that both voluntary and involuntary pregnancy loss are at least markers for increased risk of death, both in the short term and the longer term. We therefore repeat our previous recommendation that clinicians should routinely inquire about a history of pregnancy loss as a step toward inviting discussion of any unresolved issues relative to a prior abortion or miscarriage which patients might hesitate to reveal without a specific invitation to discuss it [19]. This information may help to alert general practitioners, gynecologists, mental health workers, and others, to offer information, treatments, and referrals which may avoid or mitigate any increased risks for negative outcomes associated with pregnancy loss.
Conclusions
Compared to women who delivered, women who had an early or late abortion had significantly higher mortality rates within 1 through 10 years. A lesser effect may also be present relative to miscarriage. Recommendations for additional research are offered.
Footnotes
Statement
The authors have no financial disclosures to declare and no conflicts of interests to report.
Source of support: Departmental sources
References
- 1.Gissler M, Kauppila R, Merilainen J, et al. Pregnancy – associated deaths in Finland 1987–1994 – definition problems and benefits of record linkage. Acta Obset Gynecol Scand. 1997;76:651–57. doi: 10.3109/00016349709024605. [DOI] [PubMed] [Google Scholar]
- 2.Gissler M, Berg C, Bouvier-Colle MH, Buekens P. Injury deaths, suicides and homicides associated with pregnancy, Finland 1987–2000. Eur J Public Health. 2005;15(5):459–63. doi: 10.1093/eurpub/cki042. [DOI] [PubMed] [Google Scholar]
- 3.Gissler M, Berg C, Bouvier-Colle MH, Buekens P. Pregnancy-associated mortality after birth, spontaneous abortion or induced abortion in Finland, 1987–2000. Am J Ob Gyn. 2004;190:422–27. doi: 10.1016/j.ajog.2003.08.044. [DOI] [PubMed] [Google Scholar]
- 4.Gissler M, Hemminki E, Lonnqvist J. Suicides after pregnancy in Finland: 1987–94: register linkage study. BMJ. 1996;313:1431–34. doi: 10.1136/bmj.313.7070.1431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reardon DC, Ney PG, Scheuren FJ, et al. Deaths associated with pregnancy outcome: a record linkage study of low income women. South Med J. 2002;95(8):834–41. [PubMed] [Google Scholar]
- 6.Bartlett LA, et al. Risk Factors for Legal Induced Abortion-Related Mortality in the United States. Obstet Gynecol. 2004;103(4):729–37. doi: 10.1097/01.AOG.0000116260.81570.60. [DOI] [PubMed] [Google Scholar]
- 7.Gissler M, Berg C, Bouvier-Colle MH, Buekens P. Methods for identifying pregnancy-associated deaths: population-based data from Finland 1987–2000. Paediatr Perinat Epidemiol. 2004;18(6):448–55. doi: 10.1111/j.1365-3016.2004.00591.x. [DOI] [PubMed] [Google Scholar]
- 8.Atrash HK, Lawson HW, Ellerbrock TV, et al. Pregnancy-related mortality From data to action CDC’s public health surveillance for women, infants, and children. 1994:141–54. [Google Scholar]
- 9.Ronsmans C, Khlat M, Kodio B, et al. Evidence for a “healthy pregnant woman effect” in Naikhar, Senegal? Int J Epidemiol. 2001;20:467–73. doi: 10.1093/ije/30.3.467. [DOI] [PubMed] [Google Scholar]
- 10.Ursin G, Bernstein L, Lord SJ, et al. Reproductive factors and subtypes of breast cancer defined by hormone receptor and histology. Br J Cancer. 2005;93:364–71. doi: 10.1038/sj.bjc.6602712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Risch HA, Marrett LD, Howe GR. Parity, contraception, infertility, and the risk of epithelial ovarian cancer. Am J Epidemiol. 1994;140(7):585–97. doi: 10.1093/oxfordjournals.aje.a117296. [DOI] [PubMed] [Google Scholar]
- 12.Brinton LA, et al. Reproductive, menstrual, and medical risk factors for endometrial cancer: Results from a case-control study. Am J Obstet Gynecol. 1992;167:1317–25. doi: 10.1016/s0002-9378(11)91709-8. [DOI] [PubMed] [Google Scholar]
- 13.Coleman PK. Abortion and mental health: quantitative synthesis and analysis of research published 1995–2009. British J Psychiatry. 2011;199:180–86. doi: 10.1192/bjp.bp.110.077230. [DOI] [PubMed] [Google Scholar]
- 14.Rue VM, Coleman PK, Rue JJ, Reardon DC. Induced abortion and traumatic stress: a preliminary comparison of American and Russian women. Med Sci Monit. 2004;10(10):SR5–16. [PubMed] [Google Scholar]
- 15.Ney PG, Fung T, Wickett AR, Beaman-Dodd C. The effects of pregnancy loss on women’s health. Soc Sci Med. 1994;48(9):1193–200. doi: 10.1016/0277-9536(94)90184-8. [DOI] [PubMed] [Google Scholar]
- 16.Li J, Precht DH, Mortensen PB, Olsen J. Mortality in parents after death of a child in Denmark: a nationwide follow-up study. Lancet. 2003;361:363–67. doi: 10.1016/S0140-6736(03)12387-2. [DOI] [PubMed] [Google Scholar]
- 17.Joyce T. The social and economic correlates of pregnancy resolution among adolescents in New York city, by race and ethnicity: a multivariate analysis. Am j Public Health. 1988;78(6):626. doi: 10.2105/ajph.78.6.626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bloom MS, Schisterman EF, Hediger ML. The use and misuse of matching in case-control studies: the example of polycystic ovary syndrome. Fertil Steril. 2007;88(3):707–10. doi: 10.1016/j.fertnstert.2006.11.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Reardon DC, Cougle JR, Rue VM, et al. Psychiatric admissions of low income women following abortion and childbirth. Can Med Assoc J. 2003;168(10):1253–57. [PMC free article] [PubMed] [Google Scholar]