Summary
Background
The expectations of post-removal cataract surgery patients are extremely high, and best vision acuity is expected. The best refractive results are influenced by two factors – cataract surgical removal and the corneal astigmatism correction. Currently, the two most often applied corneal astigmatism removal methods are laser surgery and toric intraocular lens implantation, with the latter method being both more stable and more reversible. This study aimed to estimate the surgical astigmatism correction efficiency after AcrySof Toric intraocular lens implantation in patients with corneal astigmatism.
Material/Methods
We used the AcrySof Toric IOL 1-part hydrophobic acrylic lenses. The retrospective research covered 30 eyeballs in 28 cataract and corneal astigmatism patients, with the AcrySof Toric lens implanted by one surgeon.
Results
In our test group 92.31% of post-surgical patients (phacoemulsification and toric lenses implantation) gained the best uncorrected visual acuity, range 0.6–1.0; and in 7.69% of patients the acuity was 0.4–0.6. Lens rotation was examined three weeks after the surgical procedure and a 3.24±3.41 degree axial displacement was observed; however, this lens rotation was clinically unimportant.
Based on the analysis of post-surgical results, the corneal astigmatism was 84.2% lower than before the procedure.
Conclusions
We noticed clinically and statistically important vision acuity improvement in the corneal astigmatism patients. The patients’ high satisfaction was conditioned by proper pre-surgery qualification. Astigmatism correction by cataract removal surgery is a safe and effective surgical solution. In the future, we expect the use of toric intraocular lenses will become widespread and significant.
Keywords: cataract, corneal astigmatism, toric intraocular lenses
Background
The expectations of patients undergoing cataract removal surgery are large and include complete post-surgical vision acuity. Since more than 15% of people with cataracts also have refractive corneal astigmatism, which uncorrected on the level of 2D or more allows obtaining post-surgical vision acuity of 0.1–0.7, we do not commonly achieve so-called “refractive success” [1]. To gain complete vision acuity among the patients in question, spherical intraocular lens implantation combined with laser astigmatism correction, or the toric intraocular lens implantation, is a necessity.
The first clinical trials of toric lens implantation were undertaken by Shimizu, in 1994 [2]. Toric intraocular lenses were launched in 1990 as an alternative for correction of astigmatism in cataract patients. Initially, the results were poor due to the post-surgical lens rotation. However, at the end of 2005 new and refined designs of toric intraocular lenses (AcrySof Toric) were approved by the US Food and Drug Administration (FDA). The lenses have been recognized as highly stable and bio-compatible, and therefore advisable for astigmatism correction in patients with cataracts [2]. The aim of this study was to estimate the surgical astigmatism correction efficiency after the AcrySof Toric lens implantation.
Material and Methods
In our research, the AcrySof Toric IOL one-part structured hydrophobic acrylic lens was applied. The characteristic feature of the toric lens is the toric elements’ presence on the posterior surface of the lens’ optical part [3,4]. Currently, there are 6 AcrySof Toric lens models available on the market. Among them, model T9 is used for 6D astigmatism correction [5]. In our research all available models of AcrySof Toric T3–T9 lenses were applied. Obtaining the best effect depends on proper patient qualification, as well as the correct calculation of the lens’s tensile strength and the model of the toric lens selected, which is assisted by an on-line calculating program.
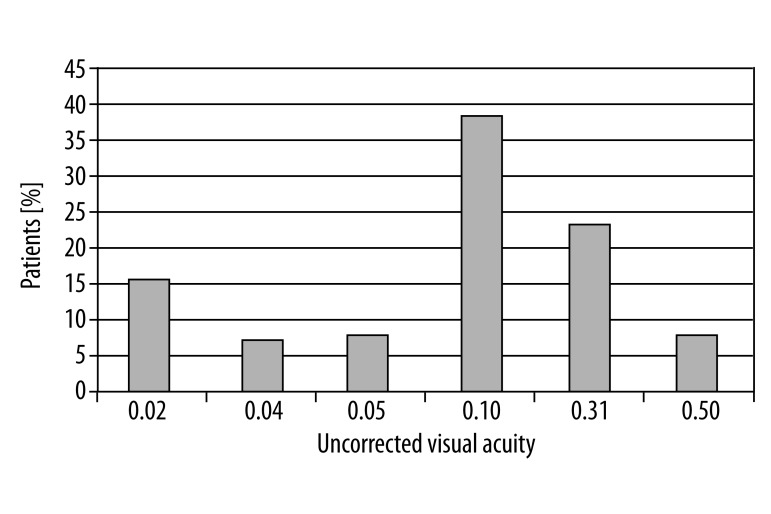
This retrospective study included 30 eyeballs in 28 patients, to whom the AcrySof Toric lens was implanted by one surgeon, during the period March – July 2010. After the study was fully explained, the patients gave their informed consent to the procedure. Patients’ regular corneal astigmatism ranged from 1.5 to 6D. The best uncorrected vision acuity was worse than 0.2 in 69.23% of patients; however, the best uncorrected vision acuity equal to 0.2–0.5 was achieved in 30.77% of patients (Figure 1).
Figure 1.
The best uncorrected visual acuity before the surgical procedure. The best uncorrected visual acuity before the surgical procedure in 69.23% patients was worse than 0.2, however, the best uncorrected visual acuity equal to 0.2–0.5 was observed in 30.77% patients.
The exclusion criteria covered the following: irregular astigmatism, unstabilized astigmatism, and diseases of the cornea and retina, amblyopia, glaucoma, post-implantation cornea condition, and refraction instability. Before the surgery, patients underwent a complete ophthalmological examination, including: uncorrected visual acuity test (UCVA), best corrected visual acuity test (BCVA), objective examination of refractive defect (performed by use of an Allergan Humphrey auto-refractometer), and slit lamp examination of the anterior segment of the eye, and examined the posterior segment using a Volk lens, manual keratometry – Javal, corneal topography (TOMEY Version 4.2C). Biometrics (IOL Master; Carl Zeiss Meditec, Jena, Germany) following the SRK-T formula and the A=118.7 constant, due to the lens’s tensile force proper calculation, was carried out in each patient. Our post-surgical aim was to obtain the emmetropia; therefore, the lens’s tensile strength and the lens’s axial placement was calculated by an on-line program which also considers the surgically induced astigmatism (SIC). The individual approach before the phacoemulsification and toric intraocular lens implantation is required in post-surgical laser refraction patients. While planning AcrySof Toric lens implantation, the reference points were marked, which was done using a Pre-Op Toric Reference Marker AE2791BL. This procedure was carried out on the dried corneal edge with the patient in the sitting position, and the reference points necessary for the toric lens axial placement in the capsule were marked on the 3, 6 and 9 o’clock positions. Next, a classical phacoemulsification procedure was performed, beginning with the main 2.6 mm incision within 120° axis, the anaesthetic and pupil diluting agents were inserted, and the capsulorhexis were performed. While its size is not large, all the optic part is well-covered, which ensures capsular stability of the toric lens. The next stage of the regular phacoemulsification was hydrodissection, hydro-delineation and the cataract mass removal (natural lens nucleus and cortex). The next step is surgical examination of the toric lens axial capsular placement, by the AcrySof Toric calculator and consideration of the previously marked reference points as well, which are marked on the dried corneal surface using the sterile Intra-Op Toric Axcis Marker – AE2792.
Then, the lens capsule is filled with the viscoelastic agent (Provisc) and, via Monarch II injector, the toric lens is placed into the capsule in the unrotatable 5–10 degree position. During the viscoelastic agent aspiration process, the lens should be finally placed in the proper axis (Figure 2).
Figure 2.
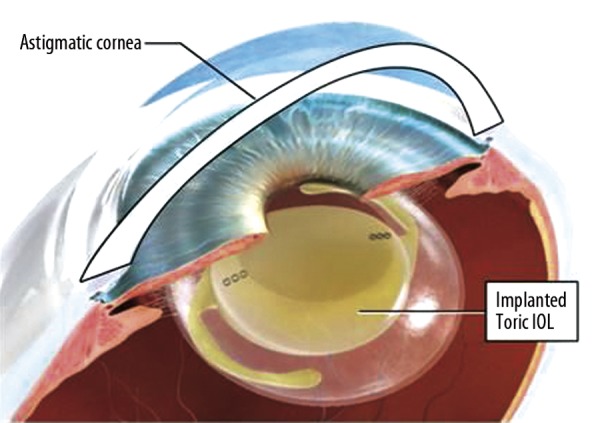
Toric intraocular lens implantation. Source: http://www.coastaljerseyeye.com/images/p-alcon-iol-implant.jpg.
During the post-surgical period, the patients were locally given Dicortineff 3 times a day and Tropidamid 3 times a day up to 1-month-period; however, after 2 weeks the dosage was lowered. The patients were observed on the first day, first month, and at three months after the surgical procedure. Every check-up covered best visual acuity with and without correction, in the presence of the slit lamp, and with the intraocular pressure measurement.
Statistical analysis methods
Statistical estimations were performed accordingly with the T-Student distribution, which is applied in interval estimation, in the parametric tests and especially for the mean values and the variances, as well as for the significance tests of statistical parameters, while dealing with the small test-group (the number N≤30). The T-Student distribution means that continuous probability distribution is frequently applied in the statistical hypothesis testing procedures, as well as for the estimation of measurement errors. Differences were statistically significant when the p value was lower than 0.05.
Results
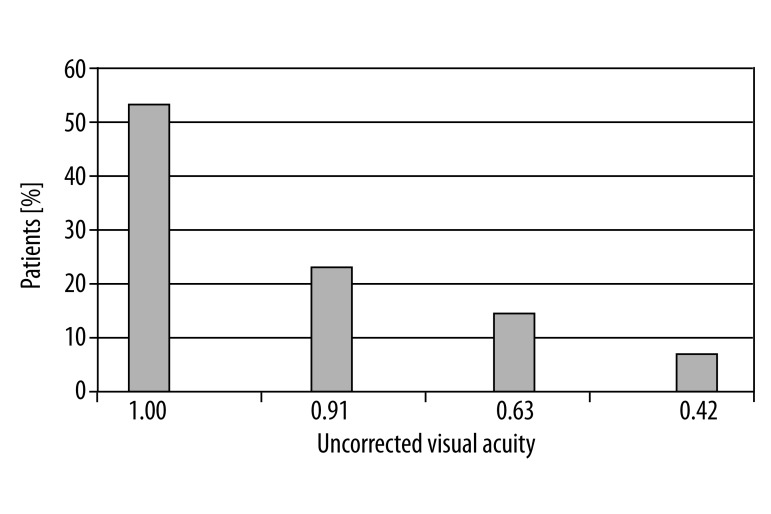
In 92.31% patients the post-surgical best uncorrected visual acuity ranged from 0.6 to 1.0; in 7.69% patients the best uncorrected visual acuity reached 0.4–0.6 (Figure 3).
The lens rotation measurement was done 3 months after the surgical procedure, and the 3.24±3.41 degree axial displacement was noticed, but was clinically unimportant.
Based on the clinical and statistical analysis of the study, the corneal astigmatism has been reduced by 84.2%.
Figure 3.
The best uncorrected visual acuity after the surgical procedure. The best uncorrected visual acuity after the surgical procedure among 92.31% patients was equal to 0.6, or even better.
Discussion
Corneal astigmatism can be corrected through the corneal, relaxation or limbal incision, or by the excimer laser. All these methods have their own limitations depending on the astigmatism degree. Moreover, the post-surgical effects are influenced by patient’s age and the size, amount, depth and length of the incisions. Toric intraocular lens implantation for corneal astigmatism correction is the best surgical option offered for patients with both cataract and corneal astigmatism.
It is important to obtain precise estimation of corneal astigmatism in order to establish proper cylindrical value as well as proper spherical lens’s tensile strength for the toric intraocular lens. In the research of Grabow [5] on the AcrySof Toric lens, manual keratometry was necessary to estimate corneal astigmatism, and 3 different methods were used – manual keratometry, optical cohesion biometry, and corneal topography – with similar results. Additionally, toric intraocular lens’ cylindrical strength and axis correction (calculated by the keratometric cylinder) gave the same value. P values were: 0.375 (manual keratometry and optical biometry), 0.236 (manual keratometry and topography) and 0.485 (optical biometry and topography). The difference between the manual keratometry and the corneal topography was 9.42±11.76 degree. The difference between optical biometry and corneal topography ranged from 10.24±13.33 degree [6]. In our research, the differences between the values estimated by IOL Master and the corneal topography were statistically unimportant. Based on the applied t-Student distribution, in the test group the p value was 0.220, which means it was statistically insignificant. The difference between the IOL Master and the cornea topography was 9.52±11.38 degree.
The main requirement for the toric intraocular lenses is their rotational stability. It is estimated that 1 degree rotation from the axis results in 3.3% cylindrical strength loss, and when lens rotation exceeds 30 degrees, there is complete loss of cylindrical strength [7]. Prior models of the toric intraocular lenses were imperfect due to their high post-surgical rotation, and the necessity of additional procedures aimed at toric intraocular lens axial correction. The procedure’s effectiveness is confirmed not only by the refractive astigmatism correction, but also by the long-lasting toric lens capsular stability [8,9]. Due to the lens instability, many doctors ceased performing toric lens implantation [4,10]. The most frequent reason for lens rotation after complication-free cataract removal surgery is the capsule’s shrinkage caused by its fibrosis [3,11].
The design of the toric intraocular lens turned out to be highly impracticable for the toric lens stability. Weinand [12] proved perfect rotational stability in case of the AcrySof SA60AT toric intraocular lens. The average post-surgical rotation level was 0.7 degree (range from 0.1 to 1.8 degree) in 17 patients. Since that time, only a few studies of the AcrySof Toric lens have been conducted. Zuberbuhler et al. [4] proved that in a study of 44 AcrySof Toric lens implantation, the post-surgical rotation, checked 3 months after the surgical procedure, ranged 5 degrees in 95% of patients, and in 68% of eyes the rotation ranged 2 degrees. Mendicute [13] analyzed 30 eyes and confirmed the toric intraocular lens displacement was 3.63±3.11 degrees, with the rotation less than 10 degrees in 96.7% of eyes with the AcrySof Toric lens. Most of the intraocular lens rotations were observed in the early post-surgical period. Myung Hun Kim [3] found the average rotational axis was 3.40±3.05; however, in our studies, the rotational axis was 3.24±3.41, after 3 months. The possible factors influencing the toric intraocular lens stability might be capsulorhexis level, as well as the toric intraocular lens’ composition. Ruhswurm et al. [14,15] found a relationship between the toric intraocular lens rotation and the lens capsule’s diameter and the eyeball’s length. Myung Hun Kim et al. found that 93.3% of eyes gained 20/40(0.5) or even better UCVA (uncorrected visual acuity), and in 73.3% of eyes 20/25(0.8) or even better UCVA during the final check-up at 13.3 months. As a comparison, early clinical tests by the US FDA found that 66% of patients after 1-sided toric lens implantation achieved UCVA of 20/25 (0.8) or even better, and 41% of subjects in the control group achieved 1-sided UCVA of 20/25 (0.8) at 6 months [10]. In our study, UCVA equal to 0.6 or better was reported in 92.31% of patients, and in 7.69% of cases the best uncorrected visual acuity reached 0.4–0.6 (Figure 3). In another toric intraocular lens study, without a control group, by Mendicute [13] 66.6% of eyes reached UCVA 20/25 or even better, 93.3% of eyes reached 20/40 or better in by 3 months after the surgical procedure. In the research by Myung Hun Kim [3], astigmatism reduction after AcrySof Toric lens implantation was 85.6%, and in our results it was 84.2%. Mendicute [13] demonstrated 70% astigmatism reduction after AcrySof Toric lens implantation. However, research by Sun [15] showed a 54% astigmatism reduction after Staar TF lens implantation. Till [16] proved higher reduction (81%) after Staar AA4203TF or AA4203TL lens implantation. De Silva and others [17] proved the 65% astigmatism reduction after MicroSil 6116TU toric lens application. The differences among the toric intraocular lens values, as well as the pre-surgical astigmatism values, lead to the percentage results’ variability in case of both the astigmatism reduction and the vision acuity. The choice of the proper toric lens is made after calculation based on the pre-surgical corneal astigmatism value, and is used for calculating the lens’ tensile strength and the axial parameters. Keratometry of the cornea’s cylinder, evaluated by the doctor, is necessary for the estimation of the required toric intraocular lenses cylindrical strength. Therefore, in order to obtain the required effect, toric lens implantation should be carried out with small incisions, and based on the keratometry value. In previous research on the toric intraocular lens implantation, the incision’s size ranged from 2.75 to 3.00 mm. Our research concerned cataract surgery with 2.6 mm cornea incision. The results were satisfactory, similar to results of other studies. There were no post-surgical complications caused by micro-incisions in cataract correction. Therefore, combining the cataract surgery using micro-incisions together with the toric intraocular lenses implantation for stigmatism correction should be considered in treatment of patients with cataracts.
Conclusions
Based on research to date, we found clinically and statistically significant visual acuity improvement in corneal astigmatism patients.
High patient satisfaction is conditioned by proper pre-surgical qualification.
Astigmatism correction during cataract removal surgery is a surgical solution that is both safe and effective. Therefore, improvement in patient quality of life is obtained by not needing to wear glasses. Comparative research in this field should be continued.
AcrySof Toric lenses revealed lack of any significant rotation during a 6-month observation time.
In the future, toric intraocular lens will play a more important role in the surgical correction of cataract and corneal astigmatism.
Footnotes
Source of support: Self-financing
References
- 1.Stankiewicz A. Soczewka toryczna – skuteczna metoda korekcji astygmatyzmu podczas zabiegu usunięcia zaćmy. CX-News. 2008;4:26. [in Polish] [Google Scholar]
- 2.Tsinopoulus I, Tsaousis K, Tsakpinis D, et al. Acrylic toric intraocular lens implantation: a single center experience concerning clinical outcomes and postoperative rotation. Clin Ophthalmol. 2010;4:137–42. doi: 10.2147/opth.s9608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim M, Chung T, Chung E. Long-term Efficacy and Rotational Stability of AcrySof Toric Intraocular Lens Impalntation in Cataract Surgery. Korean J Ophthalmol. 2010;24(4):207–12. doi: 10.3341/kjo.2010.24.4.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zuberbuhler B, Signer T, Gale R, Haefliger E. Rotational stability of the Acrysof SA60TT toric intraocular lenses: A cohort study. BMC Ophthalmol. 2008;8:8. doi: 10.1186/1471-2415-8-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Data on file. Alcon Laboratories, Inc; Fort Worth, Texas: AcrySof® clinical trial. [Google Scholar]
- 6.Grabow HB. Intraocular correction of refractive errors. In: Kershner RM, editor. Refractive keratectomy for cataract surgery and the correction of astigmatism. Thorofare: Slack, Inc; 1994. pp. 79–115. [Google Scholar]
- 7.Novis C. Astigmatism and toric intraocular lenses. Curr Opin Ophthalmol. 2000;11:47–50. doi: 10.1097/00055735-200002000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Hill W, Potvin R. Monte Carlo simulation of expected outcomes with the Acrysof Toric intraocular lens. BMC Ophthalmology. 2008;8:22. doi: 10.1186/1471-2415-8-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Olsen T. Improved accuracy of intraocular lens power calculation with the Zeiss IOLMaster. Acta Ophthalmol Scand. 2007;85(I):84–87. doi: 10.1111/j.1600-0420.2006.00774.x. [DOI] [PubMed] [Google Scholar]
- 10.Horn JD. Status of toric intraocular lenses. Curr Opin Ophthalmol. 2007;18:58–61. doi: 10.1097/ICU.0b013e328011f9bf. [DOI] [PubMed] [Google Scholar]
- 11.Ohmi S. Decentration associated with asymmetric capsular shrinkage and intraocular lens size. J Cataract Refract Surg. 1993;19:640–43. doi: 10.1016/s0886-3350(13)80016-8. [DOI] [PubMed] [Google Scholar]
- 12.Weinand F, Jung A, Stein A, et al. Rotational stability of a single-piece hydrophobic acrylic intraocular lens: new method for high-precision rotation control. J Cataract Refract Surg. 2007;33:800–3. doi: 10.1016/j.jcrs.2007.01.030. [DOI] [PubMed] [Google Scholar]
- 13.Mendicute J, Irigoyen C, Aramberri J, et al. Foldable toric intraocular lens for astigmatism correction in cataract patients. J Cataract Refract Surg. 2008;34:601–7. doi: 10.1016/j.jcrs.2007.11.033. [DOI] [PubMed] [Google Scholar]
- 14.Ruhswurm I, Scholz U, Zahatmayer M, et al. Astigmatism correction with a foldable toric intraocular lens in cataract patients. J Cataract Refract Surg. 2000;26:1022–27. doi: 10.1016/s0886-3350(00)00317-5. [DOI] [PubMed] [Google Scholar]
- 15.Sun XY, Vicary D, Montgomery P, Griffiths M. Toric intraocular lenses for correcting astigmatism in 130 eyes. Ophthalmology. 2000;107:1776–81. doi: 10.1016/s0161-6420(00)00266-9. [DOI] [PubMed] [Google Scholar]
- 16.Till JS, Yoder PR, Jr, Wilcox TK, Spielman JL. Toric intraocular lens implantation: 100 consecutive cases. J Cataract Refract Surg. 2002;28:295–301. doi: 10.1016/s0886-3350(01)01035-5. [DOI] [PubMed] [Google Scholar]
- 17.De Silva DJ, Ramkisson YD, Bloom PA. Evaluation of a toric intraocular lens with a Z-haptic. J Cataract Refract Surg. 2006;32:1492–98. doi: 10.1016/j.jcrs.2006.04.022. [DOI] [PubMed] [Google Scholar]